Copyright
©2010 Baishideng Publishing Group Co.
World J Radiol. Jul 28, 2010; 2(7): 237-248
Published online Jul 28, 2010. doi: 10.4329/wjr.v2.i7.237
Published online Jul 28, 2010. doi: 10.4329/wjr.v2.i7.237
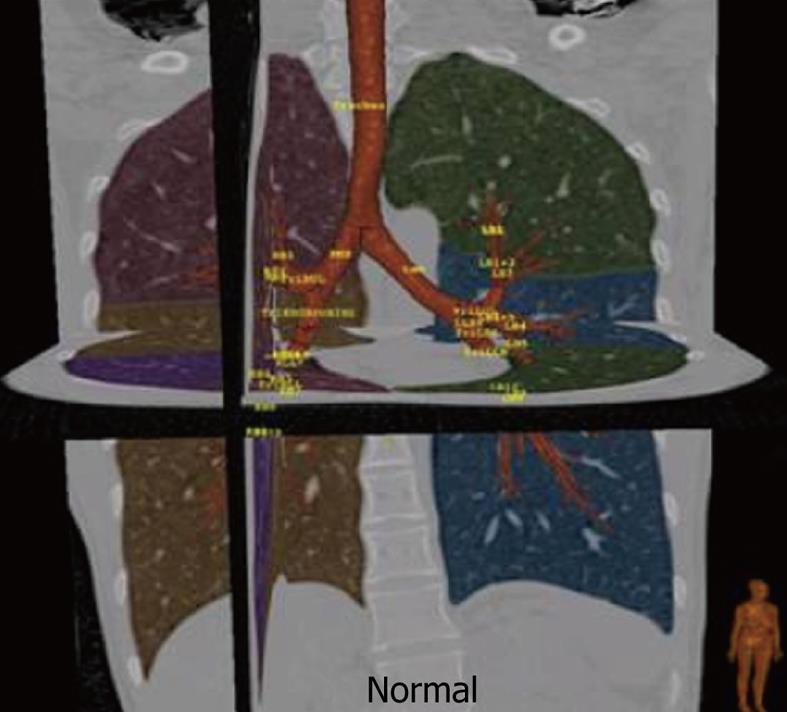
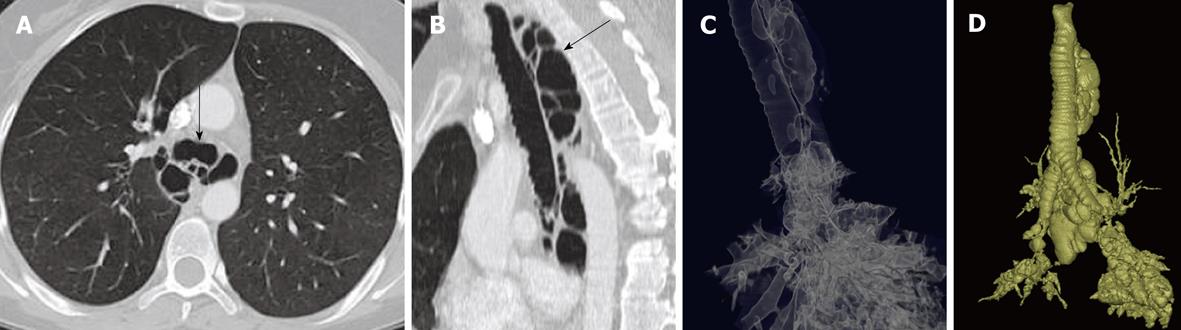
Figure 1 Normal tracheo-bronchial tree with automated lobar segmentation and nomenclature for main airways using dedicated three-dimensional reconstruction software.
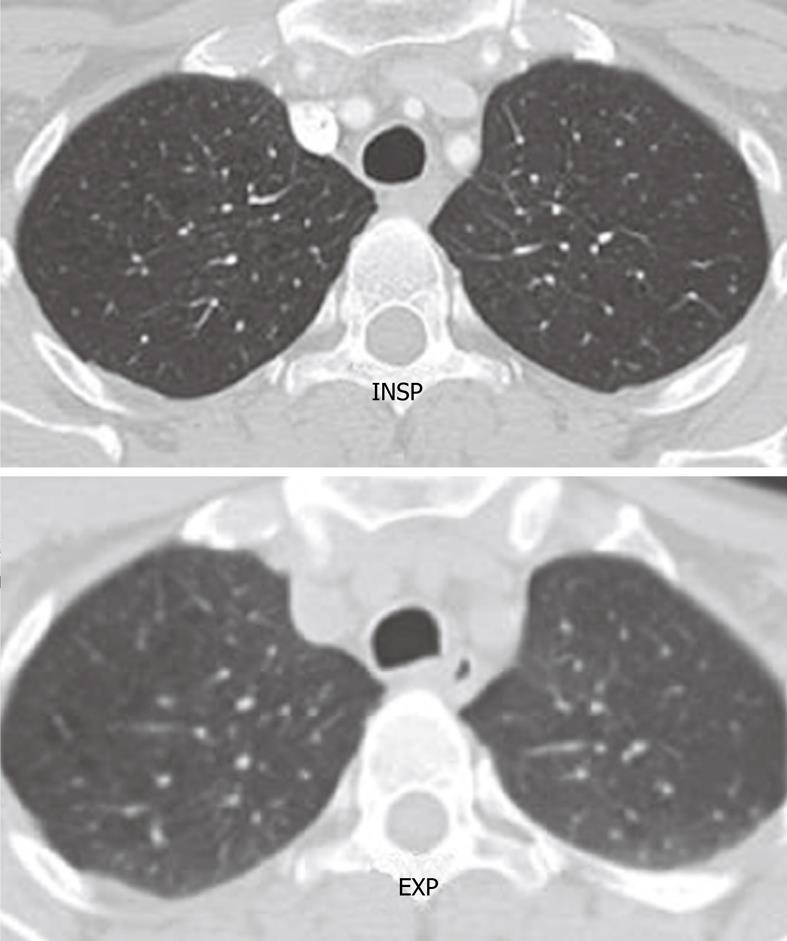
Figure 2 Axial computed tomography image shows the normal rounded configuration of the trachea at the end of inspiration.
Note the normal anterior bowing of the posterior membranous wall of the trachea at the end of expiration.
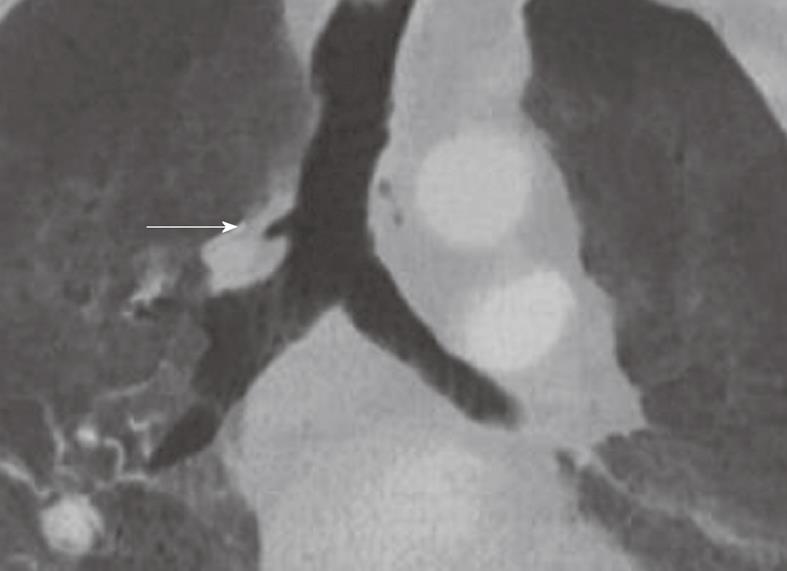
Figure 3 Minimum intensity projection coronal view demonstrating “bronchus suis” (arrow) arising from the right wall of the distal trachea.
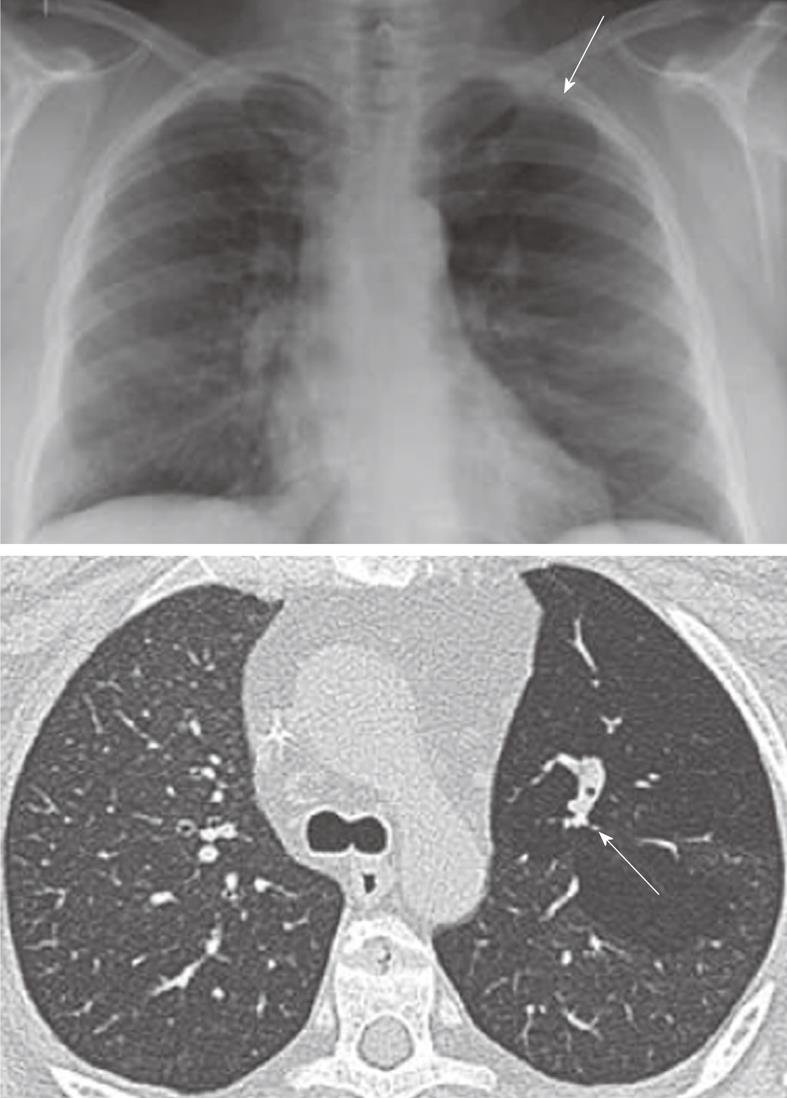
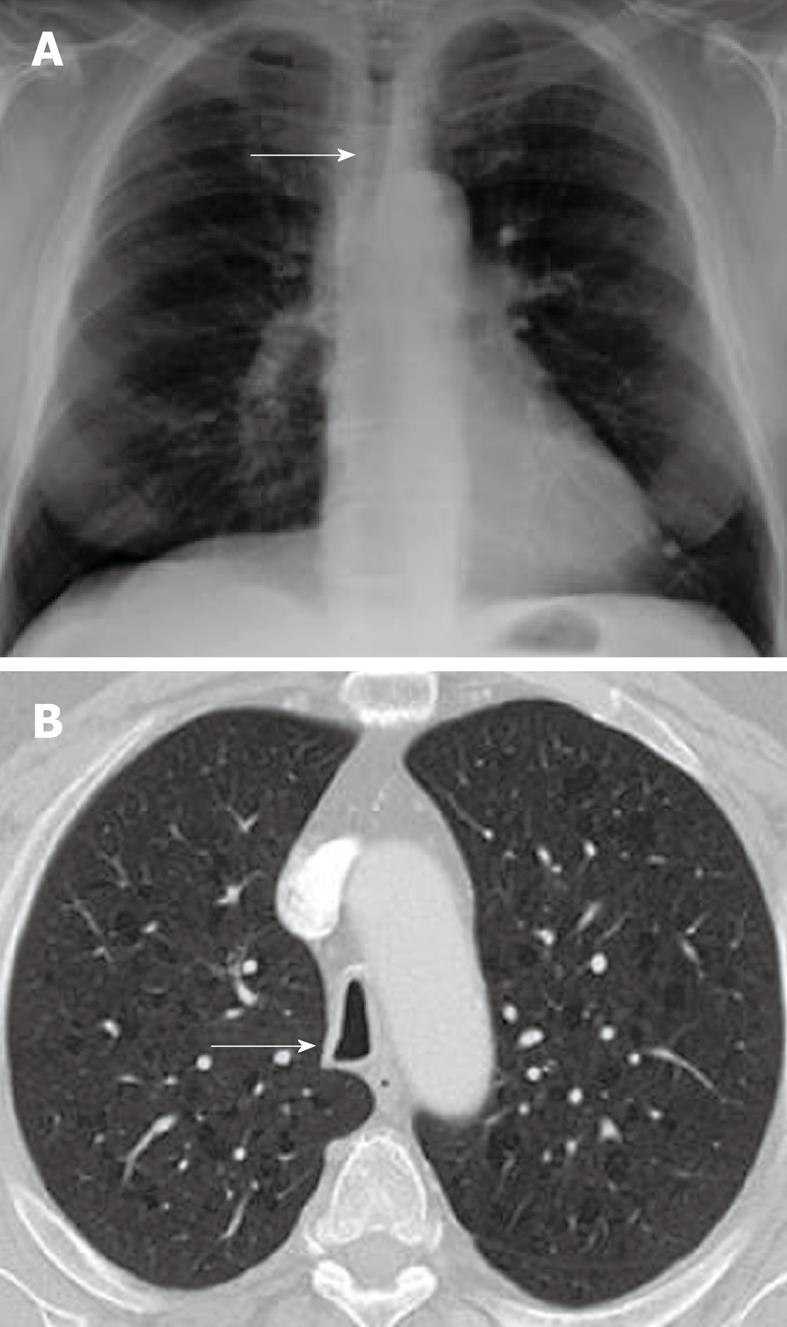
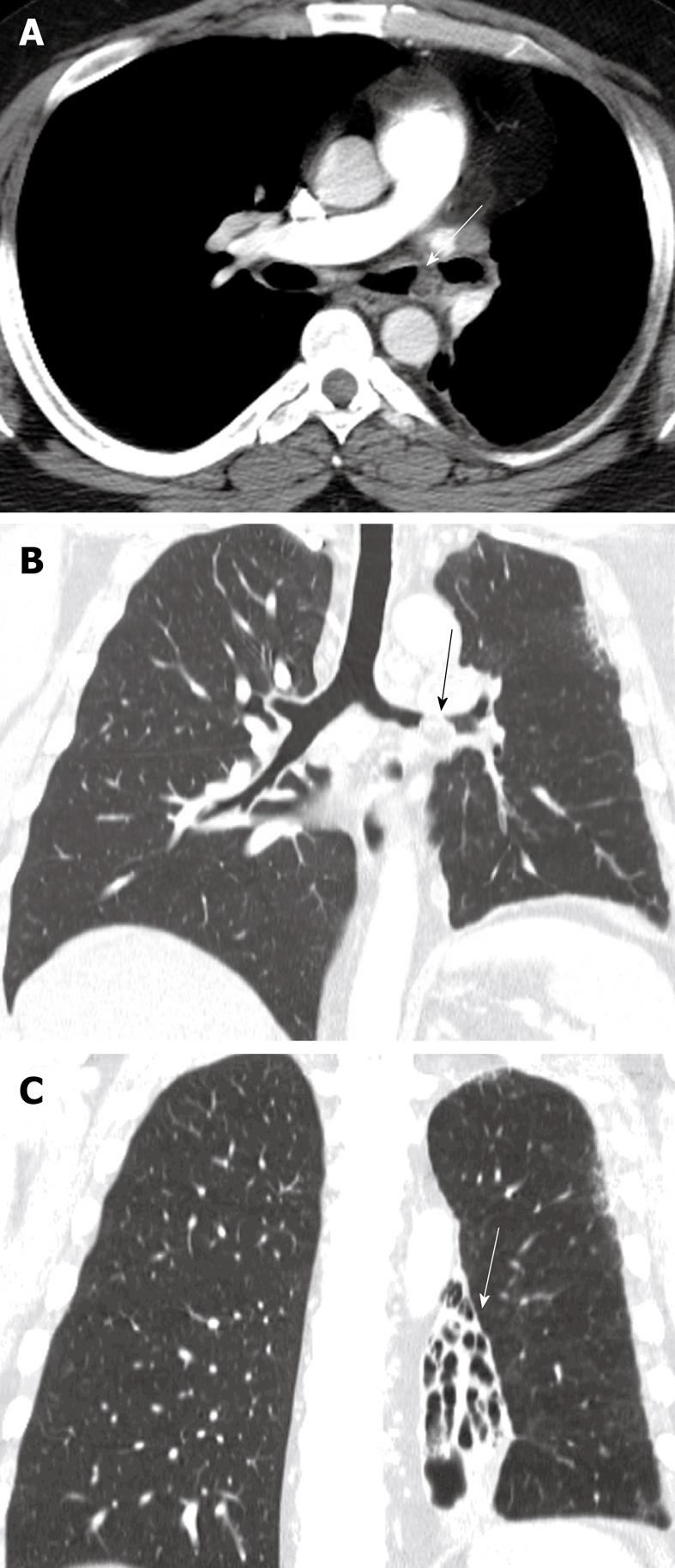
Figure 4 Congenital bronchial atresia.
Chest X-ray showing relative lucency of the left upper lobe (arrows). The axial computed tomography section showing hyperinflation in the left upper with non-enhancing branching tubular structure representing the mucus filled left upper lobe bronchus. This appearance is virtually diagnostic of congenital bronchial atresia.
Figure 5 Mounier Kuhn syndrome (congenital tracheobronchomegaly).
Axial computed tomography (A), multiplanar sagittal (B) and the minimum intensity projection reconstruction (C) show tracheal enlargement with multiple paratracheal and peribronchial diverticule (arrows). The maximum intensity projection reconstruction (D) demonstrates all interconnected airway structures.
Figure 6 Saber sheath trachea.
A: Chest radiograph PA view demonstrating diffuse narrowing of the trachea (arrow); B: Axial computed tomography scan showing inward bowing of the lateral tracheal wall (arrow) with elongated sagittal dimension of the trachea compared to the coronal plane is consistent with the saber sheath configuration.
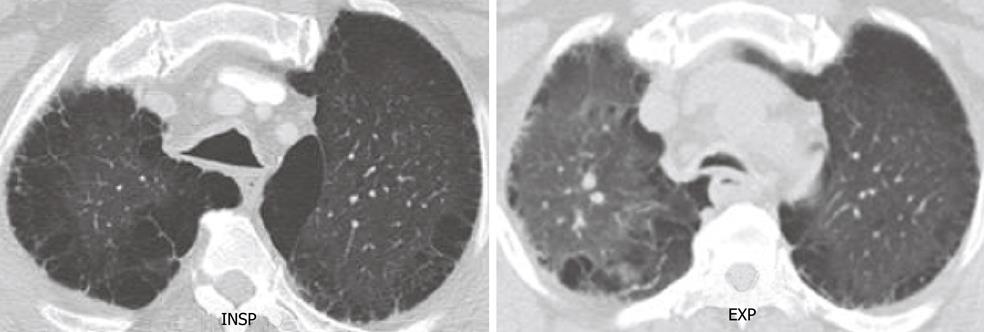
Figure 7 Tracheomalacia.
End inspiratory and end expiratory axial computed tomography scan shows excessive collapse of the posterior wall of the trachea in expiration. Note the extensive changes consistent with emphysema in both lungs.
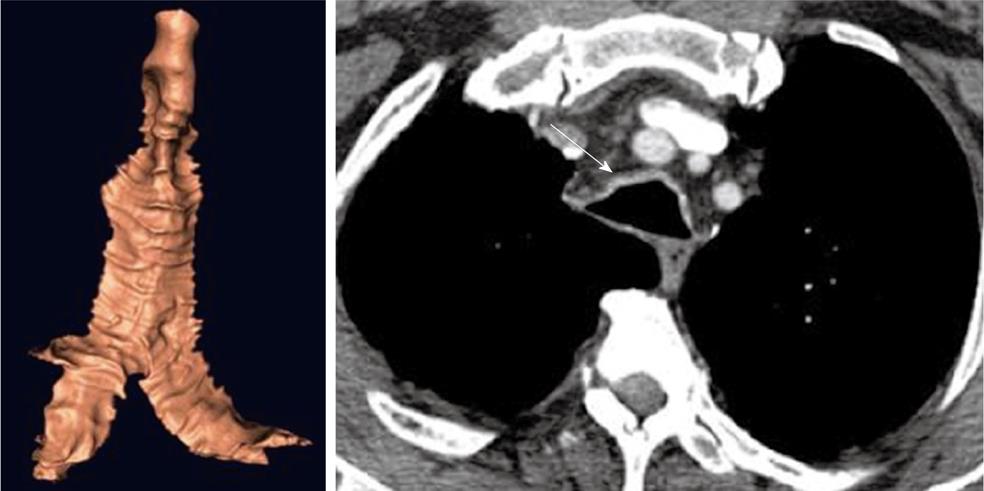
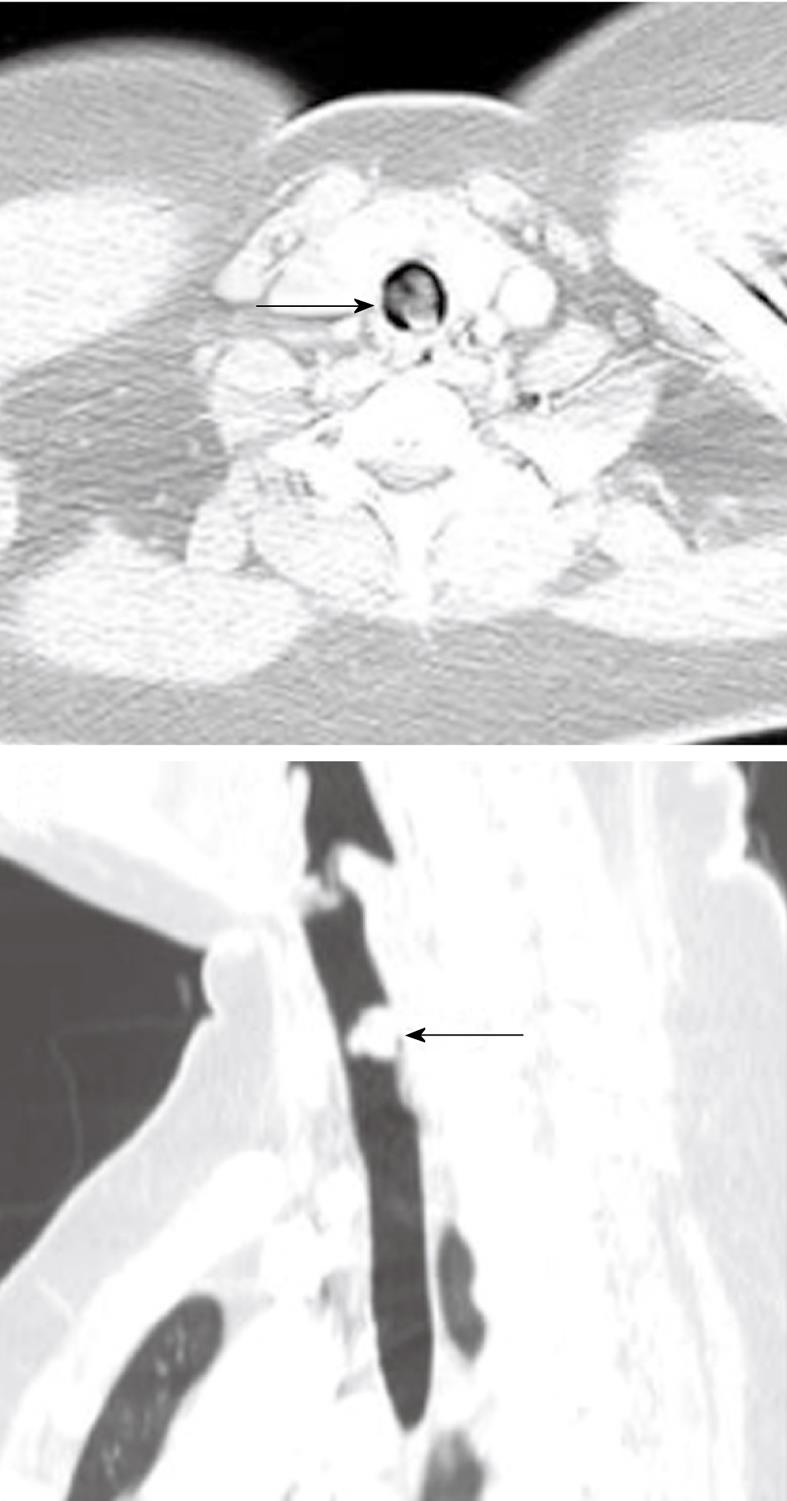
Figure 8 Relapsing polychondritis.
Note the characteristic thickening of the anterior cartilaginous wall of the trachea (arrow). The posterior membranous wall is uninvolved.
Figure 9 Subglottic stenosis.
Three-dimensional (3-D) shaded surface display computed tomography (CT) image shows smooth focal narrowing of the trachea in the subglottic region (arrow). The extent of the stenosis is much better demonstrated on the 3-D images than on axial CT images.
Figure 10 Extrinsic narrowing of the trachea.
Axial computed tomography image in the superior mediastinum demonstrating displacement and narrowing of the proximal trachea (arrow) by a large thyroid mass.
Figure 11 Axial computed tomography image and sagittal multiplanar reconstruction showing invasion of the anterior wall off the carina (arrows) by malignant lymphadenopathy from non-small cell lung cancer.
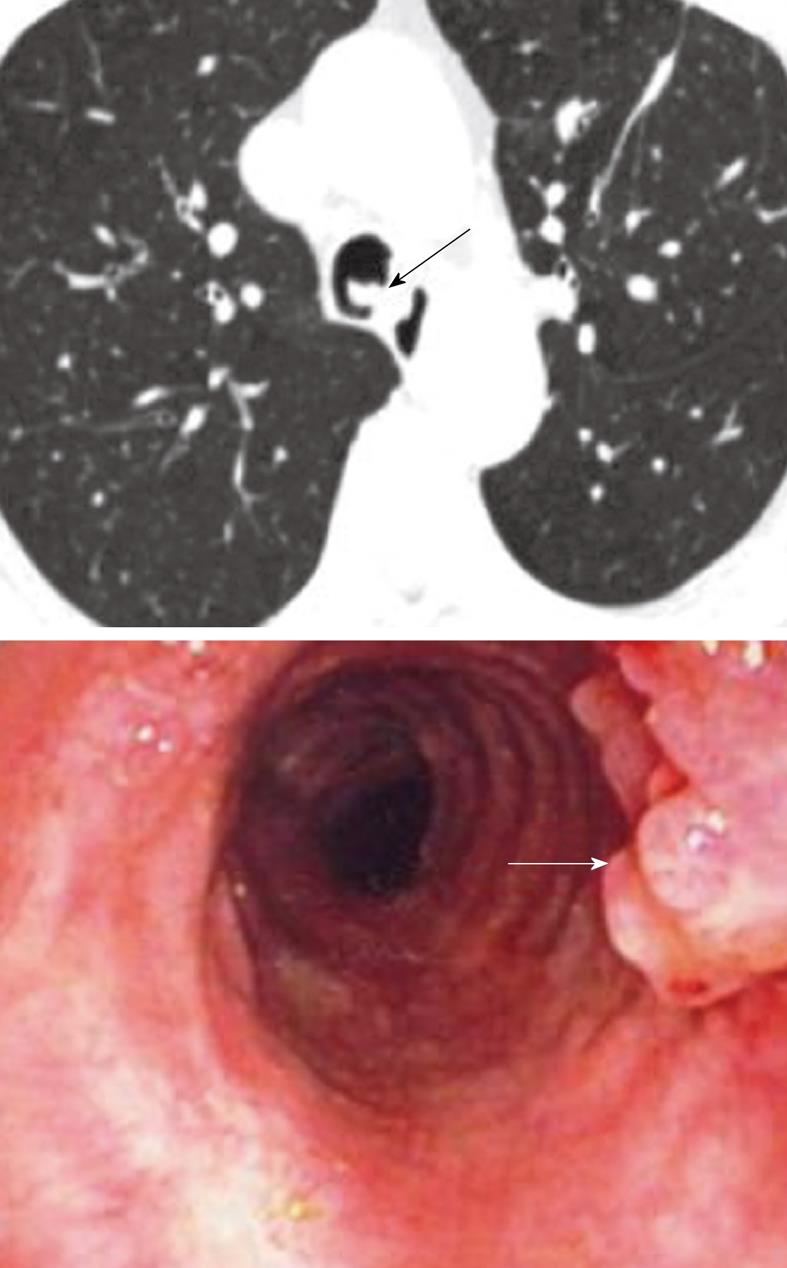
Figure 12 Respiratory papillomatosis.
Endoluminal masses in respiratory papillomatosis seen on the axial computed tomography scan (black arrow) and on bronchoscopy (white arrow).
Figure 13 Coronal multiplanar reconstruction and the virtual bronchoscopic image showing extensive involvement of the distal trachea (arrow) and the right bronchus in a case of recurrent respiratory papillomatosis.
Figure 14 Squamous cell cancer of the trachea (arrow) in a known case of recurrent respiratory papillomatosis.
Note the extensive bilateral cystic lung lesions consistent with pulmonary involvement in respiratory papillomatosis.
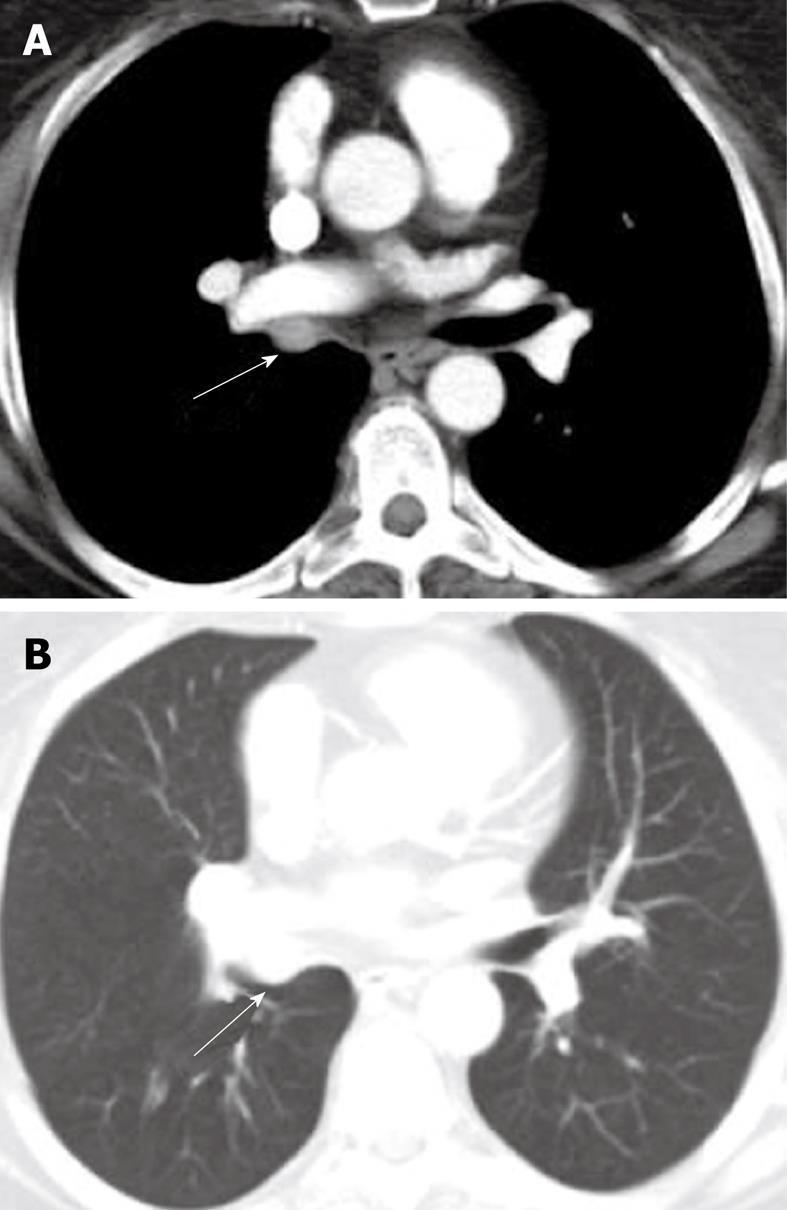
Figure 15 Metastatic melanoma right main bronchus.
Axial computed tomography image-mediastinal (A) and lung windows (B) shows enhancing soft tissue mass occupying the right main bronchus (arrows).
Figure 16 Endobronchial hamartoma.
Axial computed tomography image (A) and the multiplanar reconstruction in the lung window (B and C) shows chronic bronchiectasis in the left lower lobe (arrow) secondary to a long-standing slow-growing obstruction of the left main bronchus and recurrent infections (arrows).
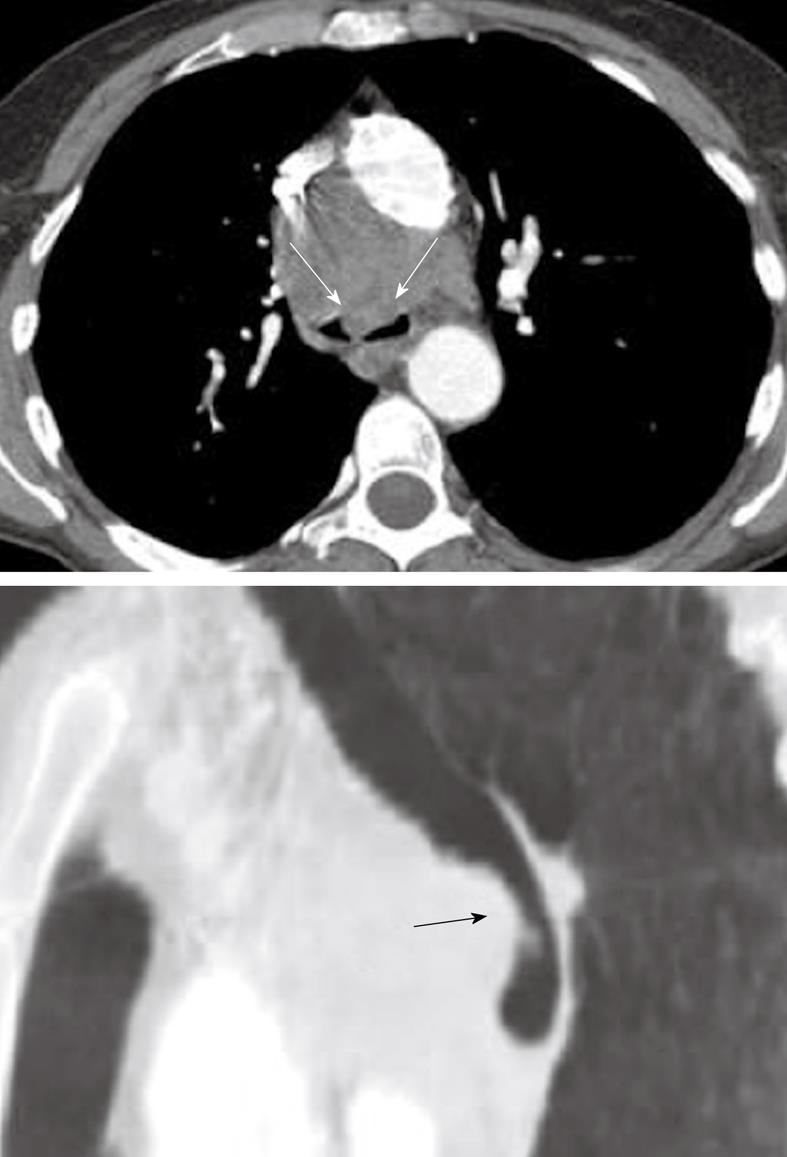
Figure 17 Axial and sagittal reconstruction of the computed tomography scan images demonstrates a fleshy mass within the tracheal lumen (arrows) in a patient presenting with increasing difficulty of breathing.
Histopathology following surgical resection demonstrated a primary sarcoma of the trachea.
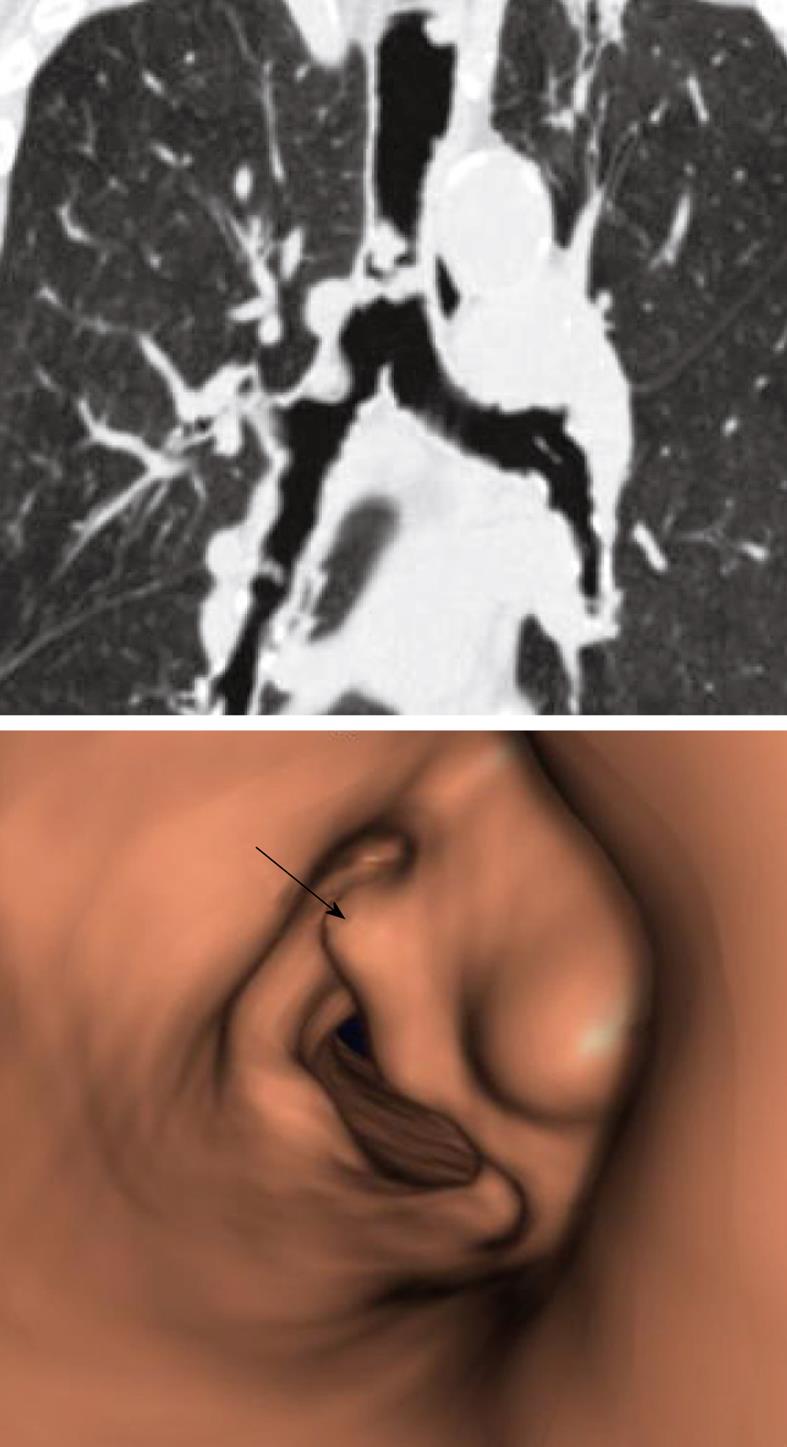
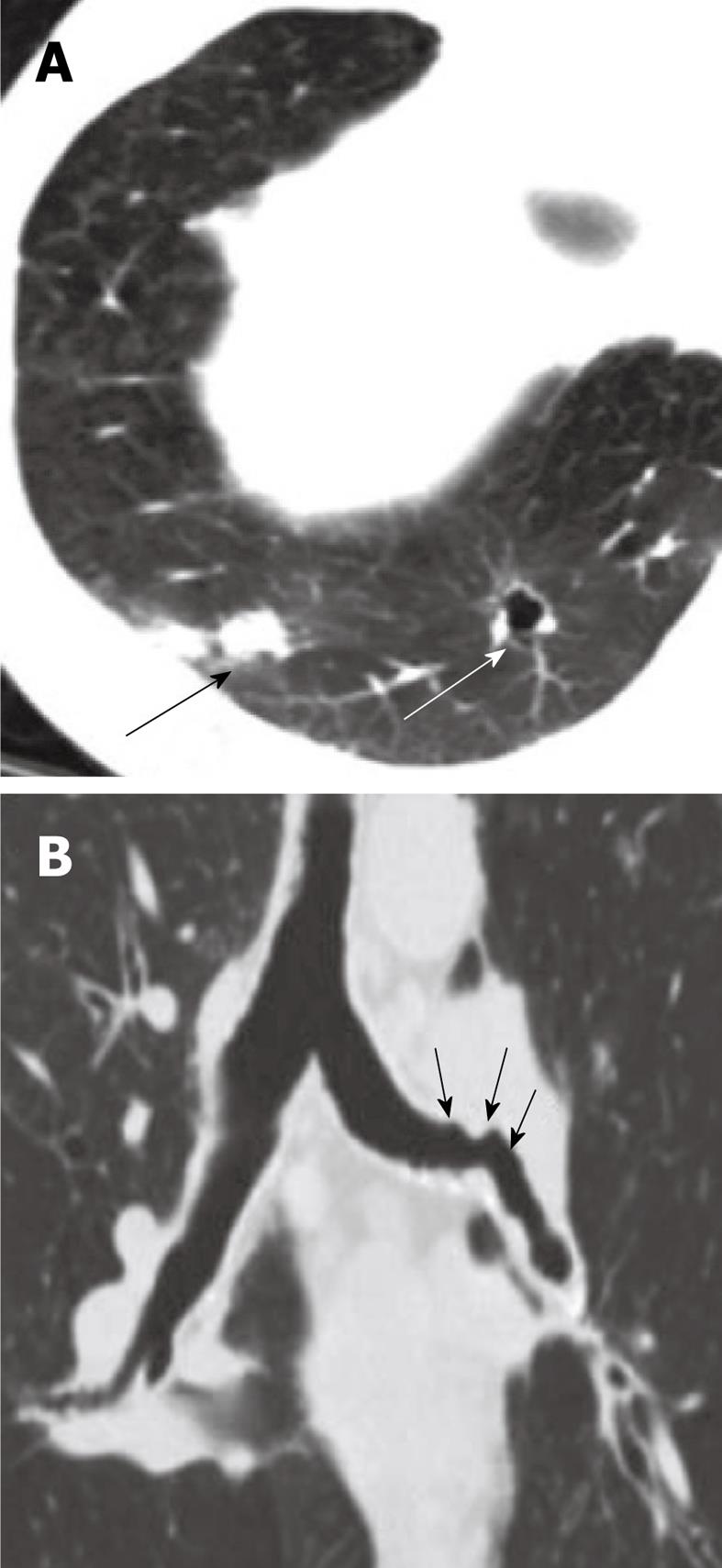
Figure 18 Airway involvement in Wegner’s granulomatosis.
A: Axial computed tomography image shows cavitary lung nodules (large arrows); B: Coronal multiplanar reconstruction in lung window demonstrates irregular narrowing of the left main bronchus (small arrows).
- Citation: Laroia AT, Thompson BH, Laroia ST, Beek EJV. Modern imaging of the tracheo-bronchial tree. World J Radiol 2010; 2(7): 237-248
- URL: https://www.wjgnet.com/1949-8470/full/v2/i7/237.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i7.237