Published online Aug 26, 2025. doi: 10.4330/wjc.v17.i8.109738
Revised: June 13, 2025
Accepted: August 4, 2025
Published online: August 26, 2025
Processing time: 92 Days and 10 Hours
Sex disparities in clinical outcomes following thoracic endovascular aortic repair (TEVAR) for acute complicated type B aortic dissection (TBAD) are not well understood.
To evaluates the impact of sex on primary and secondary outcomes by comparing male and female cohorts undergoing TEVAR.
A systematic search of PubMed, EMBASE, Cochrane Library, and ScienceDirect identified five studies involving 2572 patients (1153 males and 1419 females). The primary outcome was hospital mortality. Secondary outcomes included reintervention rates, acute kidney injury (AKI), ischemic stroke, limb ischemia, and spinal cord ischemia. Odds ratios (OR) with 95% confidence intervals (CI) were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic.
The primary outcome showed no significant difference between males and females for hospital mortality (OR: 1.13, 95%CI: 0.81-1.59, P = 0.47, I2 = 0). Among secondary outcomes, males had a significantly higher risk of AKI (OR: 1.55, 95%CI: 1.21-2.00, P = 0.0006, I² = 0). No differences were observed for reintervention rates, ischemic stroke, limb ischemia, or spinal cord ischemia.
Male patients undergoing TEVAR for complicated TBAD are at increased risk of AKI but show comparable outcomes to females for mortality, ischemic events, reintervention, and other complications. Future research should explore mechanisms and strategies to optimize outcomes.
Core Tip: This meta-analysis demonstrates that while most clinical outcomes following thoracic endovascular aortic repair (TEVAR) for acute complicated type B aortic dissection are comparable between sexes, male patients face a higher risk of postoperative acute kidney injury (AKI). By addressing modifiable risk factors and exploring innovative care models, clinicians can reduce the burden of AKI and enhance care for patients undergoing TEVAR.
- Citation: Khawar M, Shah SA, Komel A, Anfaal Z, Ali U, Mubarik M, Buhadur Ali MK, Muhammad A, Saifullah M, Hadeed Khawar MM, Qadeer A, Rahman SU, Haider M, Mehdi AM. Sex-based outcomes following thoracic endovascular aortic repair for acute complicated type B aortic dissection: A meta-analysis. World J Cardiol 2025; 17(8): 109738
- URL: https://www.wjgnet.com/1949-8462/full/v17/i8/109738.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i8.109738
The life-threatening medical emergency, aortic dissection (AD), which is classified within the family of acute aortic syndromes[1], is believed to impact 3-4 individuals per 100000 annually. Among these, 40% of patients are categorized as having type B AD (TBAD), which originates distal to the left subclavian artery[2].
Depending on initial clinical manifestations of malperfusion and rupture, TBAD can be further subdivided into complicated or uncomplicated TBAD[3]. According to the definition, we must observe the presence of at least one of the following features for acute complicated TBAD (cTBAD): Rapid aortic expansion, aortic rupture, intractable pain, relent
However, following the procedure, there are still various outcomes of great significance for patients. Operative mortality is the primary outcome, while secondary outcomes include acute kidney injury (AKI), spinal cord ischemia, stroke, length of hospital stay, and overall survival[9].
Despite the growing body of literature on TEVAR for cTBAD, the impact of sex on outcomes remains poorly under
To address the gaps in the findings of various outcomes, we have carried out this meta-analysis to identify the most frequent complications in the two sexes. We believe that the emphasis we have placed on the variation in clinical mani
A comprehensive literature search was conducted by the PRISMA guidelines and recommended methodologies. The search was conducted across various databases, including PubMed, EMBASE, Cochrane Library, and ScienceDirect, from inception to December 2024. The search strategy included a combination of MeSH terms and keywords, including “Thoracic Endovascular Aortic Repair,” “TEVAR,” “Type B Aortic Dissection,” “Acute Aortic Dissection,” and “Sex Differences.” Through a manual search of the bibliographies of relevant studies, additional references were identified. The study adhered to the PRISMA guidelines[11]. Detailed Search String is given in the Supplementary material.
Those Studies were included if they were observational studies comparing male and female patients undergoing TEVAR for acute cTBAD. Studies were eligible if they reported quantitative data on at least one primary or secondary outcome of interest.
Studies were excluded if they did not have a Sex-specific outcomes comparison. Also, Case reports, conference abstracts, editorials, or expert opinions were excluded. Those studies were also excluded that were duplicate studies with overlapping patient data (the most comprehensive or recent study was retained).
Two independent reviewers performed the search, assessed full-text articles for eligibility, and screened titles and abstracts. By consulting with a third reviewer, Disagreements were resolved through discussion. Data extraction was conducted independently by the same reviewers and included details on study design, population characteristics, surgical approach, and reported outcomes.
Two independent reviewers used the Newcastle-Ottawa Scale (NOS) to assess the methodological quality of the included studies. While other tools, such as ROBINS-I, also provide more detailed assessments, the NOS was chosen for its efficiency and consistency in evaluating key domains relevant to our study. The NOS evaluates three domains: Selection (4 items), comparability (1 item, up to 2 stars), and outcome assessment (3 items), with a maximum possible score of 9 stars. Discrepancies were resolved through discussion with a third reviewer[12].
All statistical analyses were conducted using Review Manager 5.3 (Cochrane Collaboration)[13]. Since all included outcomes were dichotomous variables, effect estimates were calculated using odds ratios (OR) with 95% confidence intervals (CI). A random-effects model was applied throughout the analysis to account for potential heterogeneity among studies. Due to the limited number of included studies (n = 5), Egger’s regression test and other publication bias assessments were not performed, as recommended for meta-analyses with fewer than 10 studies. According to the Cochrane Handbook (chapter 9), heterogeneity was considered significant if the alpha value of the χ2 test is below 0. In contrast, the interpretation of the I-square test is as follows: 0% to 40% indicates no significant heterogeneity, 30% to 60% indicates moderate heterogeneity, 50% to 90% suggests substantial heterogeneity, and 75% to 100% indicates considerable heterogeneity[14,15]. For each outcome, a forest plot was constructed to analyze the data visually.
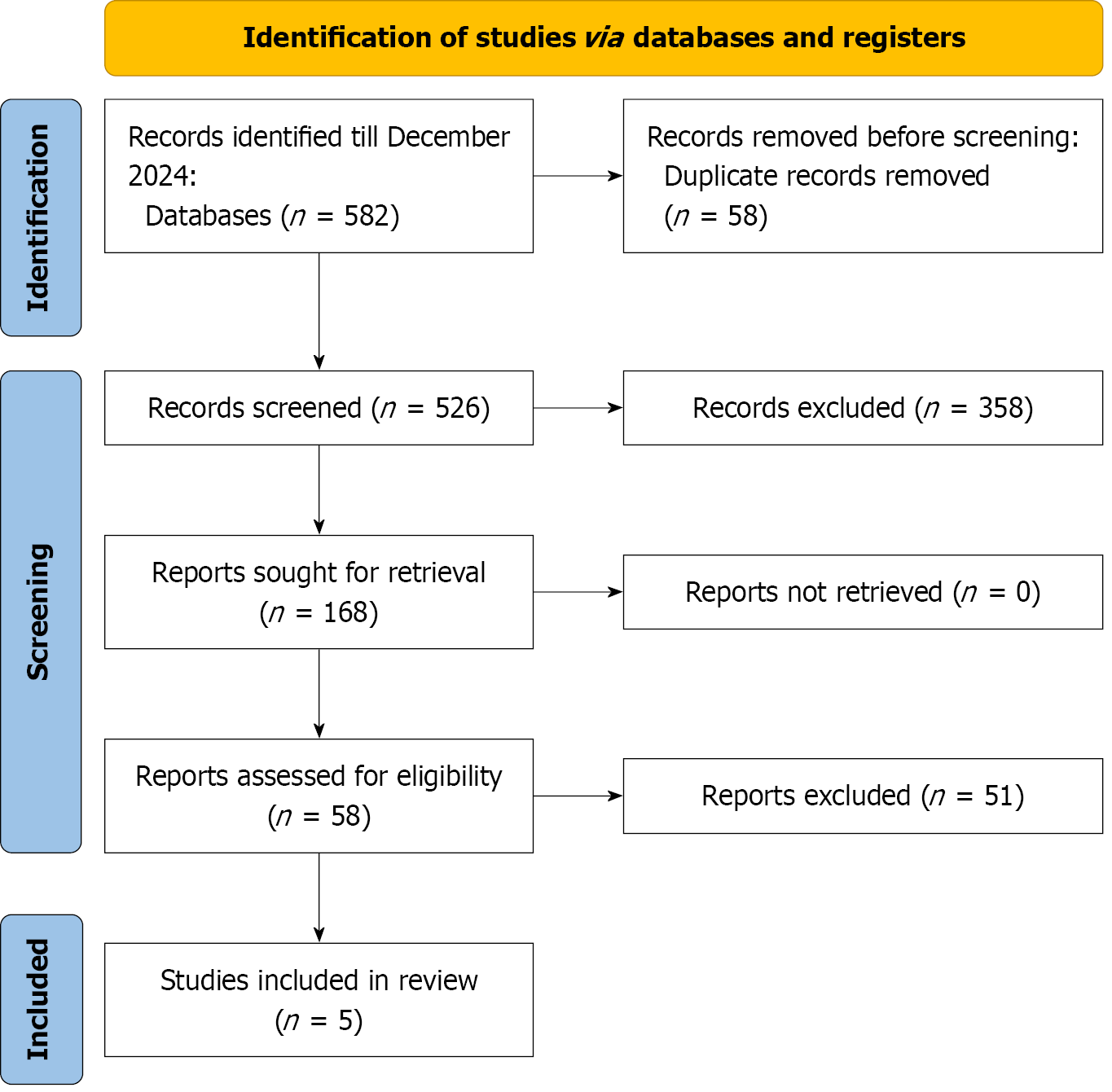
The PRISMA statement flowchart (Figure 1) outlines the literature screening process, study selection, and exclusion criteria. The initial search yielded 582 articles, from which 46 full-text articles were retrieved for assessment. Ultimately, five studies[16-20] met the eligibility criteria and were included in both the qualitative and quantitative meta-analyses.
A total of 2572 patients (1153 males, 1419 females) from five retrospective cohort studies were included in the meta-analysis. The mean age for male patients ranged from 53.84 to 64.67 years (mean: 59.9 ± 12.1 years), while female patients had a mean age between 58.8 and 64.67 years (mean: 62.5 ± 12.1 years).
Regarding comorbidities, hypertension was common in both sexes (male: 84.2%-91.96%, female: 78.3%–94.59%), with slightly higher rates in males in most studies. Smoking was consistently more prevalent in males (38.8%-63%) compared to females (2.5%-59.5%), a difference that may contribute to an increased risk of AKI in male patients, given the estab
These baseline characteristics illustrate notable Sex-based differences in age, comorbidities, and risk factors. Notably, the higher prevalence of smoking and DM in males may predispose them to higher rates of postoperative complications such as AKI. In contrast, the greater burden of COPD in females could influence respiratory outcomes following TEVAR for acute cTBAD (Table 1).
| Ref. | Year | Study design | Max. follow up | Total no. of patients | Age (mean SD) years | Smoker (%) | Hypertension (%) | Diabetes mellitus (%) | COPD (%) | Chronic kidney disease (%) | |||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | ||||
| Bashir et al[17] | 2022 | Retrospective cohort | NA | 41 | 17 | 58.2 ± 13.6 | 58.8 ± 13.3 | NA | NA | 87.8 | 88.2 | 9.7 | 5.9 | NA | NA | NA | NA |
| Filiberto et al[18] | 2022 | Retrospective cohort | 5 years | 121 | 38 | 59.6 ± 14.1 | 62.5 ± 14 | 38.8 | 42.1 | 90.9 | 84.2 | 11.6 | 13.2 | 7.4 | 18.4 | 32.2 | 39.5 |
| Luo et al[16] | 2021 | Retrospective cohort (prospectively maintained single center) | 4 years | 793 | 120 | 53.84 ± 11 | 56.11 ± 10.07 | 55.2 | 2.5 | 85.6 | 78.3 | 5.4 | 13.4 | 1.3 | 0 | 7.9 | 6.7 |
| Summers et al[19] | 2024 | Retrospective cohort | 5 years | 1095 | 531 | 58.67 ± 14.10 | 64.67 ± 15.61 | 63 | 58 | 87 | 88 | 11 | 14.5 | 9.3 | 15 | NA | NA |
| Yammine et al[20] | 2024 | Retrospective cohort | 3 years | 112 | 74 | 60 ± 12.8 | 64.1 ± 14.5 | 42.9 | 59.5 | 91.96 | 94.59 | 16.96 | 16.22 | 15.18 | 27.03 | 27.68 | 21.62 |
The in-hospital outcomes were examined between males and females undergoing TEVAR, including neurological and renal complications, as well as other perioperative parameters.
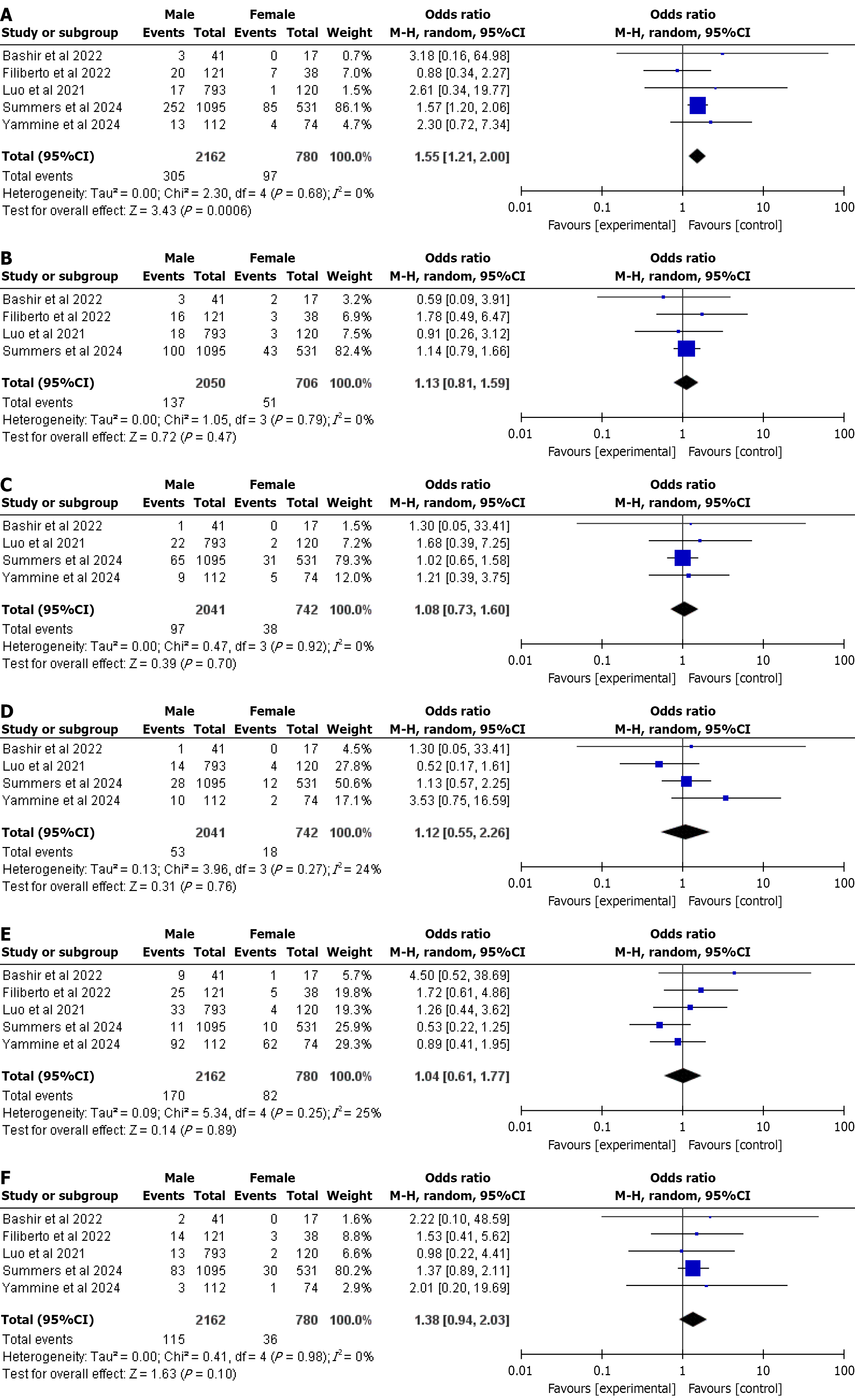
AKI: For patients undergoing TEVAR for TBAD, the male population was significantly at a higher risk for postoperative AKI than females, i.e., (OR 1.55, 95%CI: 1.21-2.00, P = 0.0006). There was no heterogeneity (I2 = 0%) in our pooled analysis. This demonstrated that Sex could influence postoperative complications (Figure 2A).
Hospital mortality: The male population had a higher risk of hospital mortality compared to females, but the findings were statistically insignificant (OR 1.13, 95%CI: 0.81-1.59, P = 0.4747), with no heterogeneity (I2 = 0%). This suggests that Sex had no significant impact on hospital mortality (Figure 2B).
Ischemic stroke: There was no statistically significant difference in ischemic stroke between male and female populations, i.e., (OR 1.08, 95%CI: 0.73-1.60, P = 0.70). There was no observed heterogeneity (I2 = 0%) in our analysis (Figure 2C).
Limb ischemia: The incidence of limb ischemia was also statistically insignificant between the two sexes undergoing TEVAR for TBAD, i.e., (OR 1.12, 95%CI: 0.55-2.26, P = 0.76). Additionally, heterogeneity was relatively low, i.e., (I2 = 24%) (Figure 2D).
Re intervention: There was no statistically significant Sex-based difference in reintervention between the two groups, i.e., (OR 1.04, 95%CI: 0.61-1.77, P = 0.89). There was low heterogeneity in our pooled analysis (I2 = 25%) (Figure 2E).
Spina Cordrd ischemia: There was no statistically significant difference in spinal cord ischemia between the male and female populations (OR 1.38, 95%CI: 0.94-2.0, P = 0.10). No heterogeneity (I2 = 0%) was observed. This demonstrated that Sex had no significant impact on perioperative spinal cord ischemia (Figure 2F).
The NOS evaluation showed that all included studies demonstrated moderate to high methodological quality. Luo et al[16] and Filiberto et al[18] achieved the highest scores (9/9), indicating a high level of methodological rigor. Summers et al[19] and Yammine et al[20] scored 8/9, showing minor limitations in comparability. Bashir et al[17] had the lowest score (7/9) due to lower comparability ratings. Overall, the studies were of high quality, ensuring reliability in the findings (Table 2).
This meta-analysis of 2572 patients (1153 males and 1419 females) from five retrospective cohort studies evaluated sex-based differences in clinical outcomes following TEVAR for acute cTBAD. The results suggest that TEVAR is equally effective for men and women in preventing hospital mortality, ischemic stroke, limb ischemia, reintervention, and spinal cord ischemia. However, male patients experienced a significantly higher incidence of postoperative AKI, highlighting a critical sex-specific disparity that necessitates targeted clinical strategies.
The lack of difference in hospital mortality between sexes aligns with prior research. A large international registry study of 9518 patients across 13 countries reported comparable mortality rates for male and female patients undergoing TEVAR[21]. Similarly, a propensity-score matched analysis of over 10000 patients from the Nationwide Readmissions Database found no sex-based differences in in-hospital mortality[22]. These findings suggest that sex does not indepen
Similarly, outcomes such as ischemic stroke, limb ischemia, reintervention, and spinal cord ischemia showed no significant sex-based differences, suggesting that the procedural risks of TEVAR are consistent across sexes in the early postoperative period. These findings are reassuring, as they indicate that sex alone does not significantly alter the risk profile for these complications, allowing clinicians to focus on other patient-specific factors when planning TEVAR.
The significantly higher incidence of AKI in male patients is a key finding that requires careful consideration. Bio
The higher risk of AKI in males has significant implications for clinical practice. Perioperative strategies to protect renal function should be prioritized, particularly for male patients. These include ensuring adequate hydration, minimizing exposure to contrast agents, and maintaining hemodynamic stability during and after TEVAR. While pharmacological interventions like N-acetylcysteine have shown mixed results in preventing contrast-induced AKI, their use could be considered in high-risk male patients[29]. Additionally, multidisciplinary care models, such as cluster nursing, have demonstrated potential in reducing AKI rates in other surgical contexts by enhancing perioperative monitoring and early intervention, and their application in TEVAR warrants further exploration[30]. Preoperative optimization of modifiable risk factors, such as smoking cessation and aggressive blood pressure control, could further mitigate AKI risk in males, given their higher prevalence of these conditions.
This meta-analysis has several limitations. The inclusion of only five retrospective studies may limit statistical power and introduce selection bias. However, most outcomes showed low heterogeneity (I² = 0 for all except AKI, where I² = 25%). Unmeasured confounding factors, such as differences in comorbidity management between sexes, could influence the results. For example, variations in the preoperative control of hypertension, diabetes, or CKD might differ between male and female patients, affecting their susceptibility to AKI. The lack of individual patient data prevented adjustment for these variables. Variations in AKI definitions, despite the use of standardized criteria, may introduce minor inconsistencies. The analysis did not account for differences in procedural techniques or institutional protocols, which could have impacted the outcomes.
Furthermore, the long-term consequences, quality of life, and sex-specific hormonal impacts were not evaluated, which limits the scope of the conclusions. Future research should employ prospective designs, standardized outcome defini
This meta-analysis demonstrates that while most clinical outcomes following TEVAR for acute cTBAD are comparable between sexes, male patients face a higher risk of postoperative AKI. These findings underscore the need for sex-specific risk stratification and tailored preventive measures to optimize outcomes. By addressing modifiable risk factors and exploring innovative care models, clinicians can reduce the burden of AKI and enhance care for patients undergoing TEVAR.
| 1. | Tsai TT, Nienaber CA, Eagle KA. Acute aortic syndromes. Circulation. 2005;112:3802-3813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 352] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 2. | Dake MD, Thompson M, van Sambeek M, Vermassen F, Morales JP; DEFINE Investigators. DISSECT: a new mnemonic-based approach to the categorization of aortic dissection. Eur J Vasc Endovasc Surg. 2013;46:175-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 118] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Habib SG, Abdul-Malak OM, Madigan M, Salem K, Eslami MH. Trends in Utilization of Completion Imaging after Lower Extremity Bypass and Its Association with Major Adverse Limb Events and Loss of Primary Patency. Ann Vasc Surg. 2023;96:268-275. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Crawford TC, Beaulieu RJ, Ehlert BA, Ratchford EV, Black JH 3rd. Malperfusion syndromes in aortic dissections. Vasc Med. 2016;21:264-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 5. | Afifi RO, Sandhu HK, Leake SS, Boutrous ML, Kumar V 3rd, Azizzadeh A, Charlton-Ouw KM, Saqib NU, Nguyen TC, Miller CC 3rd, Safi HJ, Estrera AL. Outcomes of Patients With Acute Type B (DeBakey III) Aortic Dissection: A 13-Year, Single-Center Experience. Circulation. 2015;132:748-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 117] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Ehrlich MP, Rousseau H, Heijmen R, Piquet P, Beregi JP, Nienaber CA, Sodeck G, Fattori R. Midterm results after endovascular treatment of acute, complicated type B aortic dissection: the Talent Thoracic Registry. J Thorac Cardiovasc Surg. 2013;145:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, von Allmen RS, Vrints CJ; Grupa Robocza Europejskiego Towarzystwa Kardiologicznego (ESC) do spraw rozpoznawania i leczenia chorób aorty. [2014 ESC Guidelines on the diagnosis and treatment of aortic diseases]. Kardiol Pol. 2014;72:1169-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 8. | Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, Mastracci TM, Mell M, Murad MH, Nguyen LL, Oderich GS, Patel MS, Schermerhorn ML, Starnes BW. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67:2-77.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1801] [Article Influence: 257.3] [Reference Citation Analysis (0)] |
| 9. | Pitcher GS, Biggs JH, Dayama A, Newton DH, Tran K, Stoner MC, Smeds MR, Schermerhorn ML, Mix D. A national census for the off-label treatment of complex aortic aneurysms. J Vasc Surg. 2024;80:604-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Summers SP, Meccanici F, Rastogi V, Yadavalli SD, Allievi S, Wang GJ, Patel VI, Wyers M, Verhagen HJM, Schermerhorn ML. The association between sex and outcomes after thoracic endovascular repair for acute type B aortic dissection. J Vasc Surg. 2024;80:1045-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40456] [Article Influence: 10114.0] [Reference Citation Analysis (2)] |
| 12. | Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 1635] [Article Influence: 148.6] [Reference Citation Analysis (0)] |
| 13. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24830] [Article Influence: 1773.6] [Reference Citation Analysis (3)] |
| 14. | Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds.). Cochrane Handbook for Systematic Reviews of Interventions. Cochrane. 2024. Available from: https://training.cochrane.org/handbook. |
| 15. | van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine (Phila Pa 1976). 1997;22:2323-2330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 468] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 16. | 16 Luo S, Zhu Y, Xie E, Ding H, Yang F, Chen L, Liu J, Liu Y, Xue L, Fan R, Luo J, Chen J. Influence of Sex on Outcomes After Thoracic Endovascular Repair for Type B Aortic Dissection. Angiology. 2021;72:556-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Bashir M, Jubouri M, Gwilym BL, Sadeghipour P, Pouraliakbar H, Rabiee P, Mohebbi B, Moosavi J, Babaei M, Afrooghe A, Ghoorchian E, Hosseini S, Mohammed I, Velayudhan B, Bailey DM, Williams IM. Ethnic & Sex Disparities in Type B Aortic Dissection Patients Undergoing Thoracic Endovascular Aortic Repair: An International Perspective. Ann Vasc Surg. 2023;94:68-79. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Filiberto AC, Pruitt EY, Hensley SE, Weaver ML, Shah S, Scali ST, Neal D, Huber TS, Upchurch GR Jr, Cooper M. Sex-based differences in patients undergoing thoracic endovascular aortic repair for acute complicated type B dissection. J Vasc Surg. 2022;76:1198-1204.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 19. | Ulug P, Sweeting MJ, von Allmen RS, Thompson SG, Powell JT; SWAN collaborators. Morphological suitability for endovascular repair, non-intervention rates, and operative mortality in women and men assessed for intact abdominal aortic aneurysm repair: systematic reviews with meta-analysis. Lancet. 2017;389:2482-2491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 142] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 20. | 20 Yammine H, Briggs CS, Frederick JR, Stanley G, Crespo Soto H, Nussbaum T, Madjarov JM, Arko FR 3rd. Disparities in Outcomes Between Sexes in Type B Aortic Dissection Patients Treated with TEVAR. Ann Vasc Surg. 2024;99:223-232. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Geiger J, Iannuzzi J, Stoner M, Doyle A. Minimum Asymptomatic Carotid Endarterectomy Surgeon and Hospital Volume Cutoffs. Ann Vasc Surg. 2023;89:85-86. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Maitusong B, Sun HP, Xielifu D, Mahemuti M, Ma X, Liu F, Xie X, Azhati A, Zhou XR, Ma YT. Sex-Related Differences Between Patients With Symptomatic Acute Aortic Dissection. Medicine (Baltimore). 2016;95:e3100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Zhang Y, Zhang Y, Wang Y, Lai H, Fu W, Wang C, Wang L, Ji Q. Sex-based outcomes after thoracic endovascular aortic repair: A systematic review and meta-analysis. J Vasc Surg. 2024;80:1303-1313.e8. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Hellgren T, Beck AW, Behrendt CA, Becker D, Beiles B, Boyle JR, Jormalainen M, Koncar I, Lopez Espada C, Setacci C, Settembre N, Sutzko DC, Szeberin Z, Thomson I, Venermo M, Mani K. Thoracic Endovascular Aortic Repair Practice in 13 Countries: A Report From VASCUNET and the International Consortium of Vascular Registries. Ann Surg. 2022;276:e598-e604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Yousef S, Brown JA, Aranda-Michel E, Serna-Gallegos D, Wang Y, Ogami T, Sultan I. Sex-Related Differences in Clinical Outcomes After Thoracic Endovascular Aortic Repair. J Am Heart Assoc. 2023;12:e025520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 26. | Yadavalli SD, Wu WW, Rastogi V, Gomez-Mayorga JL, Solomon Y, Jones DW, Scali ST, Verhagen HJM, Schermerhorn ML. Thoracic endovascular aortic repair of metachronous thoracic aortic aneurysms following prior infrarenal abdominal aortic aneurysm repair. J Vasc Surg. 2023;78:614-623. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Maldonado TS, Powell A, Wendorff H, Rowse J, Nagarsheth KH, Dexter DJ, Dietzek AM, Muck PE, Arko FR, Chung J; STRIDE study group. One-year limb salvage and quality of life following mechanical aspiration thrombectomy in patients with acute lower extremity ischemia. J Vasc Surg. 2024;80:1159-1168.e5. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Sorber R, Tsai LL, Hicks CW, Black JH 3rd. Midterm outcomes of isolated thoracic aortic replacement in congenital versus degenerative aortopathy in a 15-year institutional cohort. J Vasc Surg. 2023;77:20-27. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Zambetti BR, Blitzer DN, Nagarsheth K, Toursavadkohi S. Outcomes and Predictors of Morbidity after Carotid Body Tumor Resection. Ann Vasc Surg. 2024;99:442-447. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 30. | Barreto EF, May HP, Schreier DJ, Meade LA, Anderson BK, Rensing ME, Ruud KL, Kattah AG, Rule AD, McCoy RG, Finnie DM, Herges JR, Kashani KB; ACT Study Group. Development and Feasibility of a Multidisciplinary Approach to AKI Survivorship in Care Transitions: Research Letter. Can J Kidney Health Dis. 2022;9:20543581221081258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |