Published online Jun 26, 2025. doi: 10.4330/wjc.v17.i6.102722
Revised: March 11, 2025
Accepted: May 13, 2025
Published online: June 26, 2025
Processing time: 236 Days and 12.4 Hours
Sinus of Valsalva aneurysm (SoVA) is a rare cardiac defect that may be congenital or acquired. It is characterized by abnormal dilatation of the aortic root due to a weakened elastic lamina at the junction of the annulus fibrosus and the aortic media. SoVAs are present in approximately 0.09% of the general population and comprise up to 3.5% of all congenital cardiac defects. It is usually found inci
Core Tip: Sinus of Valsalva aneurysm is a rare cardiac defect defined as an abnormal dilatation of the aortic root. This arises due to a weakened elastic lamina at the junction of the annulus fibrosus and the aortic media. Echocardiography is the first-line imaging of choice for diagnosis. Definitive management includes surgery. However, transcatheter closure is a newer minimally invasive technique that is now increasingly preferred over traditional surgical approaches in the treatment of both ruptured and unruptured aneurysms.
- Citation: English K. Diagnosis and treatment options for sinus of Valsalva aneurysms: A narrative review. World J Cardiol 2025; 17(6): 102722
- URL: https://www.wjgnet.com/1949-8462/full/v17/i6/102722.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i6.102722
Sinus of Valsalva aneurysm (SoVA) is an uncommon cardiac defect characterized by an abnormal dilatation of the aortic root between the sinotubular ridge and the aortic valve annulus[1]. They can be congenital or acquired and are more common among men than women, with a reported incidence of 0.09% in the general population[1,2]. Congenital cases are commonly associated with other cardiac anomalies, such as bicuspid aortic valves (BAVs), pulmonary stenosis (PS), and ventricular septal defects (VSDs)[3,4]. Inherent deficiency of the elastic lamina in the affected aortic sinus is the common underlying mechanism of most SoVA[5]. Over time, this structural abnormality under long-standing pressure leads to progressive aneurysmal dilatation and eventual rupture[5,6].
SoVAs commonly originate from the right coronary sinus in 70% to 90% of cases, followed by the noncoronary sinus (10%-25%) and the left sinus (< 5%)[7]. Patients may present asymptomatic or symptomatic with symptoms suggestive of acute rupture, such as dyspnea, chest pain, cardiac murmurs, and palpitations[7,8]. Unruptured aneurysms are usually clinically silent and are commonly discovered incidentally on echocardiography or cross-sectional imaging performed for other reasons[7-9].
Treatment of SoVA has evolved over the last decade. Although surgical repair remains the definitive management option, transcatheter closure (TCC) is a minimally invasive technique that has emerged in the previous two decades[10]. This procedure treats both ruptured and unruptured aneurysms and has expanded the range of nonsurgical options for patients with SoVA[10,11]. In this article, we provide a narrative review of SoVA and its epidemiology, pathophysiology, diagnosis, and management.
SoVAs are extremely rare, occurring in approximately 0.2% to 0.9% of patients undergoing cardiac surgery[5,12,13]. These aneurysms constitute up to 3.5% of all congenital cardiac anomalies, with an even lower reported incidence of 0.09% in the general population[14-16]. Due to its rarity, many cases of SoVAs remain clinically silent until an adverse event such as rupture occurs[17]. Congenital SoVAs typically occur in younger people and are 4 times more likely in men compared to women, with a higher reported incidence in the Western population[18,19]. This higher incidence in Western groups suggests a genetic predisposition[18-20].
Acquired SoVAs, in contrast, typically occur in older individuals, reflecting the additive effect of atherosclerosis or other risk factors such as infective endocarditis (IE), syphilis, vasculitis diseases, or trauma[21,22]. These aneurysms originate from the right coronary sinus in up to 90 of cases, followed by the noncoronary sinus (10%-25%) and the left sinus (< 5%)[3,23-25]. There is a significant increase in morbidity and mortality if ruptured SoVA occurs and remains untreated, owing to 1-year life expectancy[26].
As mentioned above, SoVAs can be congenital or acquired[27]. Congenital SoVAs develop due to the absence of elastic lamina in the wall of the affected sinus, leading to an enlargement of the aortic root between the sinotubular ridge and the aortic valve annulus[28,29]. These aneurysms are frequently associated with other congenital heart anomalies such as BAV, VSD, and PS[30-32]. In fact, VSDs are present in up to 60% of cases[33]. Other associations include coarctation of the aorta, aortic insufficiency, atrial septal defect (ASD), and other rare coronary artery anomalies[34,35]. Aneurysmal dilatation of the sinus of Valsalva can occur due to connective tissue weakness in disorders such as Marfan syndrome, Ehler-Danlos syndrome, and other connective tissue diseases[36,37].
Acquired SoVAs, in contrast, occur due to several factors that diminish the strength of the aortic wall over time and are similarly associated with connective tissue pathologies[38-40]. Chronic changes of atherosclerosis leading to cystic media necrosis can weaken the intimal layer of the aorta, leading to SoVAs[41]. Infectious etiologies are well-known risk factors for the aneurysm, which include syphilis, tuberculosis, and IE[42]. Additionally, inflammatory conditions that damage the proximal aorta, including inflammatory aortitis and Takayasu arteritis, have been implicated as causes of SoVA[43]. Chest trauma and iatrogenic injury during aortic valve replacement surgery have also been reported as secondary mechanisms of acquired SoVA[43-45].
The pathophysiology of SoVA commonly occurs due to a complex interplay of physiological and anatomical factors, which leads to the creation and potential rupture of the aneurysm[5,46]. SoVAs occur at the three dilated sections of the aortic root area between the aortic valve annulus and the sinotubular junction[47]. These sections are termed the sinuses of Valsalva, which are normally reinforced by elastic lamina, which a thick fenestrated layer of elastin that provides structural integrity to the aortic wall[48]. The lack or defect in the elastic lamina at the sinuses, particularly at the junction of the aortic media and the annulus fibrosus, leads to the formation of SoVAs[49]. In congenital cases, the anomalous development of the bulbus cordis during embryogenesis results in a structurally weakened aortic wall, giving rise to aneurysmal dilatation[50]. Congenital SoVAs are commonly associated with other heart defects such as BAV, VSDs, ASDs, and PS[50,51].
Acquired SoVAs occur due to chronic degenerative changes of the aortic wall[52]. These changes arise due to several factors, including atherosclerosis, connective tissue disorders, and aging, leading to progressive weakness and an increased risk of aneurysmal formation[51-53]. Infectious etiologies such as IE and syphilis lead to inflammation and scarring of the aortic wall, increasing susceptibility to aneurysm formation[54,55]. Similarly, inflammatory conditions such as vasculitis can cause chronic inflammation and structural changes, leading to SoVAs[56]. Complications from cardiac surgeries and trauma can lead to physical damage to the aortic wall, which predisposes to the formation of aneurysms and rupture[57]. The aortic root is predisposed to massive hemodynamic stress due to high-pressure blood flow from the left ventricle. This stress is more pronounced at the sinuses of Valsalva, where the aortic valve cusps attach. The absence of the elastic lamina or prolonged stress in this area significantly increases the risk of aneurysm formation and rupture[58].
The most feared complication of SoVA is rupture[56-58]. These aneurysms typically enlarge over time, which leads to thin wall rupture, causing blood to spread to the nearby pericardial space or adjacent cardiac chambers, leading to heart failure and hemodynamic instability[59]. Depending on the aneurysm’s physiologic location and function, it can present significant clinical consequences in both the rupture and unruptured state. Rupture of the right and noncoronary sinuses commonly results in communication between the right ventricular outflow tract and the aorta or the right atrium and the aorta[60,61]. This rupture, as a result, is susceptible to creating left-to-right shunts, which can lead to right-sided heart failure and right ventricular overload[60-62]. In contrast, rupture of a left SoVA is clinically less significant. This commonly results in communication to the left ventricular outflow tract and the left atrium[63].
Ruptures commonly occur between 20 and 40 years, with occasional outliers in late adulthood and early infancy[64]. In conjunction with the size and location, the speed at which rupture occurs is the major determinant of prognosis[65]. The right ventricle is the most common location of rupture, followed by the right atrium[66]. Historically, rupture across the interventricular septum has been associated with left ventricular outflow tract obstruction[65-67].
The size of SoVAs also has severe implications on clinical outcomes. Large SoVAs serve as a nest for thrombus formation[68]. Major coronary arteries have been occluded by SoVAs with thrombus formation, leading to ischemic heart disease. SoVAs in both the ruptured and unruptured states can be complicated by aortic regurgitation (AR), resulting in volume overload and heart failure[69]. AR as a complication occurs in up to 50% of patients with SoVAs[8,70]. For this reason, aortic valve replacement is usually done in conjunction with operative repair of the aneurysm at the time of surgery[71,72].
The clinical history of patients with SoVA is highly dependent upon whether the aneurysm is ruptured or unruptured. Patients with unruptured aneurysms are typically asymptomatic. The condition is frequently discovered incidentally in these patients while undergoing imaging for other reasons[73,74]. Symptomatic patients commonly express chest pain, dyspnea, and palpitations[75]. In cases where SoVA has ruptured, the history may include severe symptoms such as sudden onset chest pain, syncope, and severe shortness of breath. Patients may also report a history of syphilis, IE, cardiac surgery, and any other condition that predisposes them to SoVAs[76].
Physical examination is usually clinically unremarkable in asymptomatic patients. Patients with ruptured SoVAs typically have key examination findings such as murmurs. Diastolic murmurs indicate classic AR due to the aneurysm’s effect on the aortic valve[77]. Continuous murmurs can be heard if communication exists between the aorta and the right atrium or ventricle[78]. In cases of acute rupture, additional objective findings may include hypotension, hypoxia, and tachycardia.
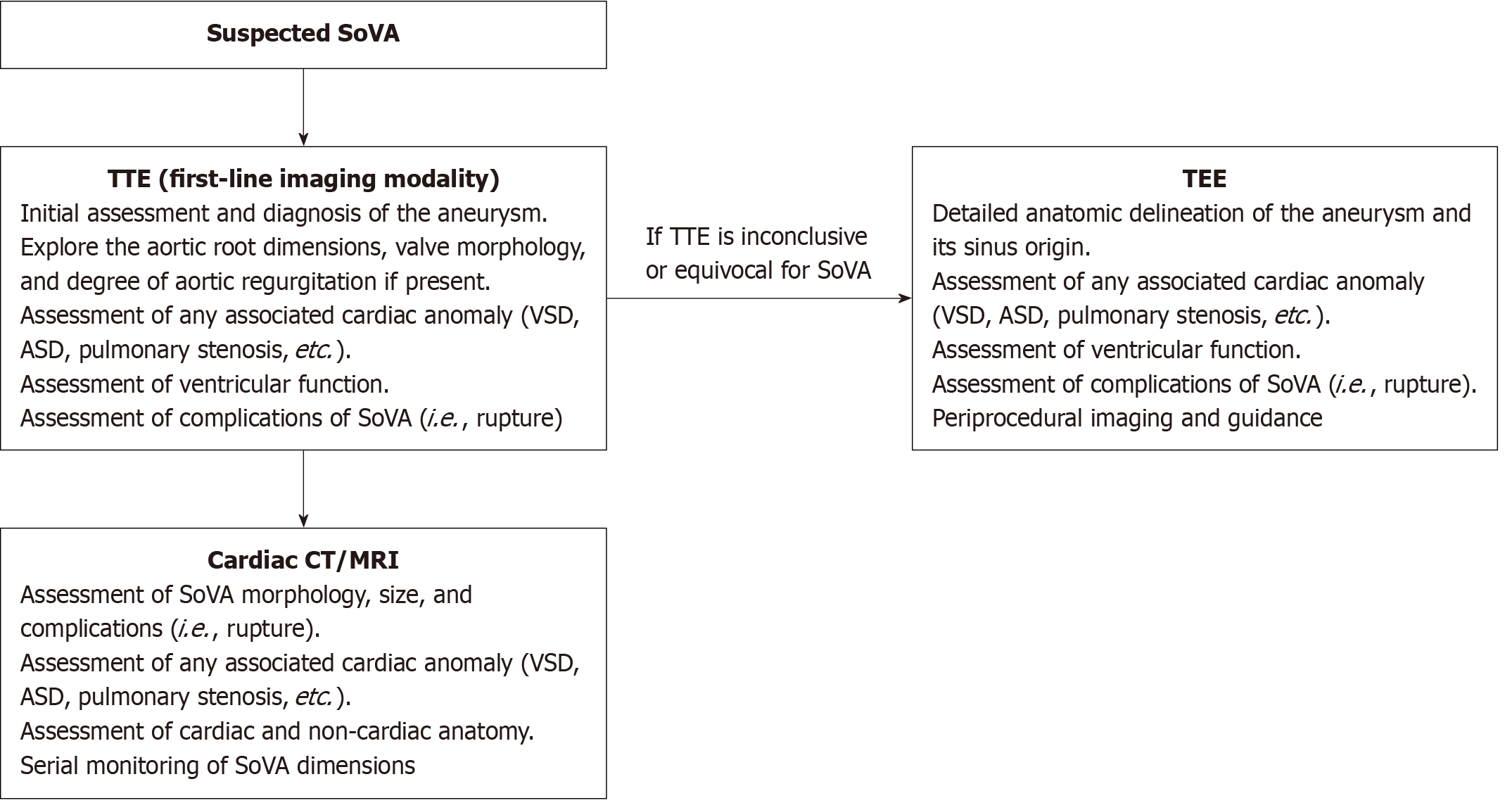
In conjunction with physical examination, the diagnosis (Figure 1) of SoVAs usually requires imaging. These imaging modalities are as follows (Table 1).
| Imaging modalities | General information | Strengths | Limitations |
| TTE | The first imaging modality of choice for diagnosis of SoVA | Possess > 90% accuracy for detecting SoVA. It is additionally safe, cost-effective, portable, and more widely available | Can sometimes incorrectly detect rupture site |
| TEE | Required as additional imaging in up to 25% of cases to further characterize the anatomy of the sinuses and their surrounding structures | Possesses better acoustic window and higher resolution, which facilitates more accurate characterization of the aneurysm and its surrounding structures | Contraindicated in patients with esophageal disease including known stricture, varices, diverticula, or tumors |
| ECG-gated MDCT | An acquisition technique that triggers a scan during a particular portion of the cardiac cycle | Provides high spatial resolution, elimination of motion artifacts, and improved temporal resolution in the nonemergent setting. Additionally, gated CT’s ability to obtain multiplanar reformations provides superior anatomic delineation and can simultaneously assess the coronary arteries | More cost prohibitive. Additionally, retrospective ECG gating is needed to assess ventricular function and valvular motion, which carries a high radiation burden |
| Cardiac MRI | Plays an important role in SoVA assessment and is particularly important in the assessment of biventricular function | Gold standard imaging technique for SoVA due to its lack of ionizing radiation, better temporal resolution, ability to quantify ventricular function and aortic regurgitant fraction, and provides an assessment of wall motion abnormalities | More cost prohibitive |
Echocardiography has been the traditional first-line imaging study to detect SoVAs[79,80]. A transthoracic echocardiogram is routinely performed first in cases of suspected SoVAs, although more commonly obtained for other reasons, such as heart failure exacerbation. This imaging modality can identify the aneurysm, visualize the aortic root, and detect associated anomalies such as an ASD, VSD, or a BAV[81]. For further investigation on transthoracic echocardiogram findings, a transesophageal echocardiogram (TEE) is usually performed, which provides a more detailed anatomical delineation of the aneurysm’s origin, which commonly appears on two-dimensional imaging as a thin-walled mobile structure that is circular in the short axis[82-84]. This structure commonly protrudes from above the plane of the coronary artery origins into an adjacent cardiac chamber, which produces a classical appearance known as a “windsock” deformity with enlargement during systole[84,85].
TEE also allows physicians to observe the filling of the aneurysm with color flow Doppler[86]. The additional use of contrast may help differentiate ruptured vs unruptured aneurysms and aid in visualizing the left-to-right shunt[86,87]. Spectral Doppler allows quantification of flow velocity and direction, where rupture into a cardiac chamber with subsequent shunting commonly yields a constant flow from the aorta to the lower pressure chambers through systole and diastole[88]. It is essential to recognize this pattern as it allows differentiation from other intracardiac shunts, such as VSDs[88,89].
Cardiac computed tomography (CT) offers high-resolution images of the sinuses of Valsalva and provides quality images of the aorta[90]. This modality can delineate the morphology and size of the aneurysm and serve as a valuable tool for assessing cardiac and vascular structures in preparation for surgery[90,91]. Newer cardiac CT imaging, such as electrocardiogram gated angiography CT, can provide high-spatial resolution images of the aortic root[7]. This is an acquisition technique to obtain high-quality scans void of pulsation artifacts[7,92]. Electrocardiographic-gated CT offers several advantages to echocardiography in nonemergent situations. These include gaining an unrestricted field of view and obtaining multiplanar reformations to provide advanced anatomic delineation while assessing the coronary arteries[93,94]. Cardiac CT still possesses lower temporal resolution than magnetic resonance imaging (MRI) and cannot provide flow information, making CT inferior to MRI for valvular assessment[95].
MRI can provide a comprehensive assessment of cardiac morphology and is the gold standard technique for the evaluation of biventricular function[96]. It is considered the imaging study of choice, particularly in patients with infectious etiology, as a cause[96,97]. The saccular aneurysm can often be seen arising from one of the sinuses and protruding into an adjacent cardiac chamber. MRI has a higher temporal resolution than CT and offers excellent soft tissue contrast and anatomical delineation[98]. When used with multiplanar sequencing, it can further evaluate intracardiac shunts in ruptured SoVAs[99]. Although considered the gold standard for diagnosis, it is not required in cases where other imaging studies have already given the pertinent anatomic and physiologic details in conjunction with the diagnosis.
Angiography is not commonly used to diagnose SoVAs; however, it can provide detailed images of the coronary arteries and the aortic root[95]. Catheterization is particularly useful in patients with a planned surgical intervention and may aid the assessment of the hemodynamic impact of the aneurysm[95]. Patients who are at intermediate or high risk for coronary artery disease commonly undergo angiography to assess possible bypass grafting at the time of diagnosis[100,101].
For unruptured SoVAs, medical management is a temporary option for patients until definitive surgical intervention is possible. Medical therapy alone is insufficient as the optimal treatment for unruptured SoVAs. Management includes a serial echocardiogram to assess aneurysm morphology and size. In addition, blood pressure control is essential. Medications such as beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers should be used to lower blood pressure to the normal range and reduce aortic wall stress[102]. Patients should also be advised to limit activities that may increase intrathoracic pressure and precipitate rupture, such as heavy lifting and strenuous exercises[103]. In cases of acute rupture, medical stabilization with intravenous fluids and blood pressure support should be administered while managing heart failure or shock symptoms until surgical repair can be done.
Surgical repair is recommended for both ruptured SoVAs and SoVAs with associated intracardiac abnormalities such as VSD, PS, or significant AR[5,104,105]. Surgical intervention should also be considered for large SoVAs and patients with symptomatic unruptured aneurysms[106]. The main goal of repair is to prevent rupture and restore normal aortic and cardiac function. Although specific guidelines regarding SoVA repair are yet to be established, it is generally accepted to follow the abdominal aortic aneurysm algorithm[107]. According to the 2010 American Guidelines on Thoracic Aortic Disease, surgical repair should be considered in those with aneurysms > 5.5 cm, > 5 cm in patients with BAVs, > 4.5 cm in the setting of connective tissue disease, or a growth rate of more than 0.5 cm per year[108].
All surgical repairs are done with cardiopulmonary bypass and cardioplegic arrest[109]. Several operative approaches are available. However, the choice is determined by the size of the aneurysm, aortic valvular pathology such as aortic insufficiency, the cardiac chamber involved, and the associated intracardiac anomaly such as a VSD[110,111]. The primary operative approaches include through the cardiac chamber where the aneurysm has ruptured, through the aortic root via an aortotomy, or a combination of both, including an aortotomy and an incision into the involved cardiac chamber. Closure techniques include primary and patch closure[112]. Primary closure is commonly used for the repair of small SoVAs, while patch closure is preferred in the repair of larger SoVAs[112,113]. The use of primary closure in large SoVAs can distort the aortic sinus, resulting in valve incompetence or excessive tissue tension at the site of repair, which may increase the risk of recurrent rupture in the future[112-114]. Surgical repair overall has an operative mortality rate of up to 3.6%, with survival rates of close to 90% at 15 years[5,112].
TCC is a newer minimally invasive technique that is used to treat both ruptured and unruptured SoVAs[115]. This is an alternative approach to open heart surgery and is particularly useful in patients who are high-risk surgical candidates, including those who are older and patients with multiple comorbidities[115,116]. Clinical indications for TCC include both symptomatic and asymptomatic unruptured aneurysm and ruptured SoVAs causing heart failure or hemodynamic instability[115-117].
TCC offers several advantages, including avoiding open heart surgery, especially in high-risk surgical candidates. This avoidance reduces surgical risk and shortens hospital length and recovery time[118]. Several studies have demonstrated high success rates for TCC, resulting in effective aneurysm occlusion and relief of symptoms[118,119]. Complications such as residual shunt or embolization and device malposition are relatively low and can be treated with rapid intervention[120,121]. With the advancements in device technology and procedural techniques, TCC is becoming increasingly preferred over the traditional surgical approaches in managing SoVA. A comparison of treatment approaches with their respective advantages and disadvantages can be seen in Table 2.
| Interventions | Recommendations | Advantages | Disadvantages |
| Medical management | Insufficient for definitive treatment. Blood pressure control with antihypertensives such as angiotensin-converting enzyme inhibitors, beta-blockers, or calcium channel blockers to reduce aortic wall stress should be used as a temporary measure until definitive surgical repair or transcatheter closure can be done | Reduces the chances of rupture for cases of unruptured SoVAs | Not definitive treatment |
| Surgical repair | Surgery remains the definitive treatment for SoVAs. Recommended for symptomatic, large, or rapidly progressive aneurysms and all ruptured aneurysms. The 2010 American Guidelines for Thoracic Aortic Disease recommend considering surgical repair for aneurysms greater than 5.5 cm, greater than 5 cm in patients with BAVs, greater than 4.5 cm in the setting of connective tissue disease, or a yearly growth rate that exceeds 0.5 cm | Can address concurrent cardiac issues such as VSDs or aortic valve dysfunction | Higher risk for complications such as bleeding, infection, or heart failure. Additionally, surgical repair prolongs hospital stay and recovery times compared to TCC |
| Transcatheter closure | Emerging minimally invasive technique used to treat both ruptured and unruptured aneurysms | Advantages include reduced surgical risks, avoiding heart surgery, and shortened hospital length and recovery times | Has potential complications such as residual shunt, embolization, or device malposition, which are generally manageable |
Patient selection criteria should be carefully considered prior to intervention for SoVA. Xiao et al[122] consider patients to be candidates for TCC if they meet the following: A bodyweight exceeding 10 kg, if the right or non-coronary sinus is the origin of the defect rupturing into the right atrium or ventricle, if the defect size is < 10 mm, if the ruptured SoVA does not involve the aortic valve has > 7 mm distance from the annulus of the aortic valve, if surgery is needed in the absence of other cardiac defects, and if a gap of > 5 mm exists between the ostium of the right coronary sinus and the ruptured site. Liu et al[123] also suggested that patients with ruptured SoVAs with a European System for Cardiac Operative Risk Evaluation II score greater than 20% would benefit from catheter closure. Overall, indications for TCC vs surgery remain a topic of debate among the medical community. Further studies are needed to validate the inclusion and contraindications for patients with ruptured SoVAs.
Since the initial case of TCC repair of a ruptured SoVA in 1994, evolving evidence, mostly in the form of case series and reports, has indicated the effectiveness of catheter closure as a suitable alternative to surgery[124-126]. TEE is valuable during the intervention because it provides real-time visualization of cardiac structures, particularly the aortic valve[82-88]. A systematic review by Ayati et al[120] revealed a post-interventional mortality of only 0.5% from a cohort of 407 patients who underwent TCC for ruptured SoVAs. In this review, 12% of patients developed complications, most notably from residual shunts (1.7%), new onset aortic insufficiency (1.5%), and rupture recurrence (1.5%). The study ultimately concluded that while TCC is a valuable alternative to surgery, precise patient selection is mandatory as surgery still remains the first-line treatment option for patients with ruptured SoVA and accompanied heart defects, arrhythmias, infections, or outflow tract obstruction. This post-operative mortality is notably lower compared to the surgical mortality mentioned by Sarikaya et al[112] in their retrospective review. However, more systemic reviews and meta-analyses of larger patient cohorts are needed to clarify the mortality benefit between the two treatment approaches.
The diagnosis of SoVA requires a combination of history, physical examination, and imaging. The first line imaging study includes an echocardiogram to visualize the aortic root, identifying the aneurysm and any associated intracardiac abnormality. Additionally, cardiac studies such as CT and MRI can provide more precise information on the anatomic delineation of the aneurysm and its surrounding structures. Definite treatment of SoVAs includes surgery. However, TCC is an emerging technique used in managing both ruptured and unruptured SoVAs and is now increasingly preferred over traditional surgical approaches due to the reduction in surgical risk, shortened hospital course, and decreased recovery time.
Although inclusion criteria for TCC exist regarding the treatment of SoVAs, there are no evidence-based clinical guidelines that provide a census within the medical community. Therefore, clinicians should ultimately decide on treatment based on each clinical scenario. More research is needed to validate the indications and contraindications of TCC in patients with ruptured SoVAs. Larger studies are also needed to further assess mortality, complication rates, and recovery time between TCC and traditional surgery for SoVAs.
| 1. | Bricker AO, Avutu B, Mohammed TL, Williamson EE, Syed IS, Julsrud PR, Schoenhagen P, Kirsch J. Valsalva sinus aneurysms: findings at CT and MR imaging. Radiographics. 2010;30:99-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Zhang T, Juan C, Yuan GD, Zhang HZ. Giant Unruptured Sinus of Valsalva Aneurysm: A Rare One Arise From Left Sinus. Circ Cardiovasc Imaging. 2019;12:e009850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Feldman DN, Gade CL, Roman MJ. Ruptured aneurysm of the right sinus of valsalva associated with a ventricular septal defect and an anomalous coronary artery. Tex Heart Inst J. 2005;32:555-559. [PubMed] |
| 4. | Liau CS, Chu IT, Ho FM. Unruptured congenital aneurysm of the sinus of Valsalva presenting with pulmonary stenosis. Catheter Cardiovasc Interv. 1999;46:210-213. [PubMed] [DOI] [Full Text] |
| 5. | Weinreich M, Yu PJ, Trost B. Sinus of valsalva aneurysms: review of the literature and an update on management. Clin Cardiol. 2015;38:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 127] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 6. | Takach TJ, Reul GJ, Duncan JM, Cooley DA, Livesay JJ, Ott DA, Frazier OH. Sinus of Valsalva aneurysm or fistula: management and outcome. Ann Thorac Surg. 1999;68:1573-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 208] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Hanna MF, Malguria N, Saboo SS, Jordan KG, Landay M, Ghoshhajra BB, Abbara S. Cross-sectional imaging of sinus of Valsalva aneurysms: lessons learned. Diagn Interv Radiol. 2017;23:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Sarhan HHT, Shawky AH, Anilkumar S, Elmaghraby A, Sivadasan PC, Omar AS, Al-Mulla AW. Association of ruptured sinus of Valsalva aneurysm and congenital ventricular septal defect: a case series. Eur Heart J Case Rep. 2021;5:ytab233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Mookadam F, Haley J, Mendrick E. Rare cause of right heart failure: contained rupture of a sinus of Valsalva aneurysm associated intraventricular septal aneurysm. Eur J Echocardiogr. 2005;6:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Nguyen Q, Vervoort D, Phan K, Luc JGY. Surgical management for unruptured sinus of Valsalva aneurysms: a narrative review of the literature. J Thorac Dis. 2021;13:1833-1850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Sivadasanpillai H, Valaparambil A, Sivasubramonian S, Mahadevan KK, Sasidharan B, Namboodiri N, Thomas T, Jaganmohan T. Percutaneous closure of ruptured sinus of Valsalva aneurysms: intermediate term follow-up results. EuroIntervention. 2010;6:214-219. [PubMed] |
| 12. | Goldberg N, Krasnow N. Sinus of Valsalva aneurysms. Clin Cardiol. 1990;13:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 81] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Vural KM, Sener E, Taşdemir O, Bayazit K. Approach to sinus of Valsalva aneurysms: a review of 53 cases. Eur J Cardiothorac Surg. 2001;20:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Chigurupati K, Kumaresan B, Gadhinglajkar S, Sreedhar R. Multiple unruptured aortic sinus of Valsalva aneurysms: A rare presentation. Echocardiography. 2017;34:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Luo Y, Fang Z, Meng W. A giant aneurysm of noncoronary sinus of Valsalva concomitant with aortic regurgitation and mitral regurgitation. Echocardiography. 2017;34:796-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Omeh DJ, Makaryus AN. Unruptured Multiple Sinus of Valsalva Aneurysms. Case Rep Radiol. 2020;2020:5046095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Smer A, Elsallabi O, Ayan M, Buaisha H, Rayes H, Alshebani Y, Tantoush H, Salih M. Sinus of Valsalva Aneurysm: A Rare Cause of Dyspnea. Case Rep Med. 2015;2015:467935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Chaturvedi H, Chaurasia AK, Makkar JS. Transcatheter closure of ruptured sinus of Valsalva type IV with misleading severe aortic regurgitation. J Cardiol Cases. 2024;29:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Sari NMAW, Dewangga MSY, Wibhuti IBR, Suastika LOS, Badung IDGSM, de Liyis BG, Kosasih AM, Prana Jagannatha GN. Ruptured sinus of Valsalva aneurysm coexisted with congenital ventricular septal defect: a case series. Egypt Heart J. 2023;75:90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Wang ZJ, Zou CW, Li DC, Li HX, Wang AB, Yuan GD, Fan QX. Surgical repair of sinus of Valsalva aneurysm in Asian patients. Ann Thorac Surg. 2007;84:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Debakey ME, Lawrie GM. Aneurysm of sinus of Valsalva with coronary atherosclerosis: successful surgical correction. Ann Surg. 1979;189:303-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Patra KP, Vanchiere JA, Bocchini JA Jr, Wu AC, Jackson RD, Kiel EA, Mello D. Endocarditis with ruptured sinus of Valsalva aneurysm caused by nonvaccine Streptococcus pneumoniae serotype 21. Tex Heart Inst J. 2012;39:277-280. [PubMed] |
| 23. | Moustafa S, Mookadam F, Connelly MS. Reticent uneventful rupture of right coronary sinus of valsalva aneurysm into right ventricle. Heart Lung Circ. 2013;22:390-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Del Campo C, Weinberg DM. Sinus of valsalva aneurysm of the non-coronary cusp: repaired in the adult with a Freestyle bioprosthesis. Tex Heart Inst J. 2003;30:202-204. [PubMed] |
| 25. | Miranda D, Peter AA, Osorion J, Ferreira AC. Ruptured aneurysm of the noncoronary sinus of valsalva. Tex Heart Inst J. 2005;32:586-588. [PubMed] |
| 26. | Asmarats L, Bethencourt A, Rodríguez A, Noris M, Maristany J, Grau A, Gómez-Jaume A, Peral V. Ruptured sinus of Valsalva aneurysm: A reversible cause of suprasystemic pulmonary hypertension. Rev Port Cardiol. 2022;41:177.e1-177.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Al-Sabeq B, De S, Davey R. A case of ruptured sinus of Valsalva aneurysm and reversible flow-induced pulmonary hypertension. Pulm Circ. 2018;8:2045894018760656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Carrel T. Sinus of Valsalva Aneurysm: Different Modes of Presentation and Techniques of Repair. J Cardiovasc Dev Dis. 2024;11:100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Sharma S, Shah J, Charaniya R, Dash R. Dissecting aneurysm of sinus of Valsalva into interventricular septum and rupturing into left ventricle through multiple sinuses: a rare case report. Eur Heart J Case Rep. 2024;8:ytae417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Bhutia E, Kumar D, Shankar B, Das SP, Kishore S. Bicuspid Aortic Valve: An Unusual Cause of Aneurysm of Left Coronary Sinus of Valsalva. Iran J Med Sci. 2017;42:310-313. [PubMed] |
| 31. | Vora K, Surana U, Ranjan A. Sinus of Valsalva Rupture or VSD Shunt: Mystery Solved by Cardiac CT. Indian J Radiol Imaging. 2021;31:748-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Bulkley BH, Hutchins GM, Ross RS. Aortic sinus of Valsalva aneurysms simulating primary right-sided valvular heart disease. Circulation. 1975;52:696-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Arora H, Kumar PA. Ruptured Sinus of Valsalva Aneurysms: Does Transesophageal Echocardiography Have a Role in the Era of Sophisticated Cardiac Imaging? J Cardiothorac Vasc Anesth. 2020;34:3382-3384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 34. | Deore RA, Hiremath MS. Transcatheter intervention for ruptured sinus of Valsalva aneurysm and coarctation of aorta with bicuspid aortic valve. IHJ Cardiovascular Case Rep. 2022;6:80-82. [DOI] [Full Text] |
| 35. | Mittal K, Dadhania D, Dey AK, Gadewar R, Hira P. Unruptured Noncoronary Sinus of Valsalva Aneurysm Associated with Atrial Septal Defect (ASD). J Clin Diagn Res. 2015;9:TD01-TD02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 36. | Tucker DH, Miller DE, Jacoby WJ Jr. Ehlers-Danlos syndrome with a sinus of Valsalva aneurysm and aortic insufficiency simulating rheumatic heart disease. Am J Med. 1963;35:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Farì G, Pennacchia I, Stigliano E, Oliva A, Carbone A, Arena V. Right sinus of Valsalva aneurysm. Cardiovasc Pathol. 2020;47:107209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Park SH, Seol SH, Seo GW, Song PS, Kim DK, Kim KH, Kim DI. Acquired Large Calcified Unruptured Sinus of Valsalva Aneurysm. Heart Lung Circ. 2015;24:e197-e199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Ning F, Tang M, Wang M, Muhlestein JB, Day JD, Li G, Yan Y. Case Report: Extrinsic Compression of the Left Main Coronary Artery by a Giant Sinus of Valsalva Aneurysm. Front Cardiovasc Med. 2021;8:753154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Ruzieh M, Shafiq Q, Murphy L, Bonnell M, Khouri S. Embolic Stroke Due to Sinus of Valsalva Aneurysm Thrombus. Am J Med Sci. 2016;352:333-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 41. | Tousek P, Krupicka J, Línková H, Straka Z, Koldová L, Widimský P. [Huge sinus of Valsalva aneurysm in patient with cystic medial necrosis of the aorta]. Vnitr Lek. 2004;50:939-942. [PubMed] |
| 42. | Ott DA. Aneurysm of the sinus of valsalva. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2006;165-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 43. | Narumi T, Watanabe T, Iwayama T, Ichikawa K, Wanezaki M, Nishiyama S, Sadahiro M, Kubota I. Ruptured Right Sinus of Valsalva Aneurysm Caused by Suspected Takayasu's Arteritis. Intern Med. 2016;55:1305-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 44. | Gharzuddine WS, Sawaya JI, Kazma HK, Obeid MY. Traumatic pseudoaneurysm of the left sinus of Valsalva: a case report. J Am Soc Echocardiogr. 1997;10:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Wingo M, de Angelis P, Worku BM, Leonard JR, Khan FM, Hameed I, Lau C, Gaudino M, Girardi LN. Sinus of Valsalva aneurysm repairs: Operative technique and lessons learned. J Card Surg. 2019;34:400-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 46. | Marroush TS, Boshara AR, Botros B, Vendittelli P, Ahmed Z, Dawood L, Rosman HS. Rupture of sinus of Valsalva aneurysm: Two case reports and a concise review of the literature. Heart Lung. 2018;47:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 47. | Schoenhoff FS, Loupatatzis C, Immer FF, Stoupis C, Carrel TP, Eckstein FS. The role of the sinuses of Valsalva in aortic root flow dynamics and aortic root surgery: evaluation by magnetic resonance imaging. J Heart Valve Dis. 2009;18:380-385. [PubMed] |
| 48. | Annabathula RV, Zhou L, Kincaid EH, Stacey RB, Vasu S, Upadhya B. An Unusual Cause of Acute Abdominal Pain and Unexplained Dyspnea in a Young Man: A Sinus of Valsalva Aneurysm. CASE (Phila). 2022;6:167-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 49. | Yarnoz MD, Weber DO, Richman A, Del Mastro P. Repair of sinus of Valsalva aneurysm associated with aortoventricular discontinuity. Ann Thorac Surg. 1982;33:290-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 50. | Lin TT, Tsai HE, Lin L, Chen TY, Lee CP, Wu CC. Very late recurrence of sinus of Valsalva aneurysm rupture after patch repair. BMC Surg. 2014;14:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Sakakibara S, Konno S. Congenital aneurysm of the sinus of Valsalva. Anatomy and classification. Am Heart J. 1962;63:405-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 169] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 52. | Ramachandran P, Garg N, Devasia T, Kansal N. Acquired aneurysm of the left sinus of Valsalva and coexistence of coronary artery disease with hypereosinophilia in a young menstruating woman: a case report. Int J Angiol. 2008;17:99-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 53. | Isilak Z, Deveci OS, Yalçin M, Incedayi M. An adult patient with ruptured sinus of Valsalva aneurysm to the right ventricle. BMJ Case Rep. 2013;2013:bcr2012008184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 54. | Deng Z, Liu Q, Liu H, Yuan J, Li J. Right sinus of Valsalva aneurysm rupture into the right ventricle in a rare cardiovascular case of syphilis. Arch Med Sci. 2023;19:1920-1922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 55. | Mukhopadhyay M, Mukherjee A, Basu S, Chaturvedi A, Sharma RK. Ruptured sinus of Valsalva aneurysm due to Infective Endocarditis managed by device closure - a case report. J Cardiol Cases. 2022;25:292-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 56. | Deshpande AA, Malhi AS, Nandi D, Bansal R, Kumar S. Unruptured sinus of valsalva aneurysm in a case of large vessel vasculitis: A diagnostic dilemma. J Card Surg. 2021;36:3874-3876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 57. | Seki H, Borger M, Mohr F, Misfeld M. Traumatic sinus of valsalva aneurysm repaired by partial david operation. Thorac Cardiovasc Surg Rep. 2014;3:13-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 58. | El Mathari S, van der Bom T, Bouma B, Driessen A, Kluin J. Sinus Valsalva Aneurysm of the non-coronary cusp initially diagnosed as right ventricular thrombus: A case report. Radiol Case Rep. 2022;17:306-309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 59. | Kalil R, Spitz J, Sciria C, Kim J, Narula N, Karas M, Horn E, Singh H. Ruptured Sinus of Valsalva Aneurysm: An Unusual Cause of Heart Failure in a Young Woman. CASE (Phila). 2022;6:27-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 60. | Kubišová K, Škňouřil L, Branny M. Rupture of the right Valsalva sinus with significant left-to-right shunt: A case report. Cor Vasa. 2017;59:e177-e180. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 61. | Nabati M, Ghaffari R, Ghaemian A. Rupture of a noncoronary sinus of Valsalva aneurysm into the left atrium: a rare cause of acute pulmonary edema. Echocardiography. 2013;30:E315-E318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 62. | Sánchez ME, García-Palmieri MR, Quintana CS, Kareh J. Heart failure in rupture of a sinus of valsalva aneurysm. Am J Med Sci. 2006;331:100-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 63. | Vadivelu R, Rohit MK, Yadav M. Ruptured sinus of Valsalva aneurysm from left coronary sinus into right atrium: a rare anomaly with an odd presentation. BMJ Case Rep. 2013;2013:bcr2012007855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 64. | Doost A, Craig JA, Soh SY. Acute rupture of a sinus of Valsalva aneurysm into the right atrium: a case report and a narrative review. BMC Cardiovasc Disord. 2020;20:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 65. | Yi SY, Zhou C, Feng J, Zhan WS, Zhou Z, Yang Y. Rupture of the right sinus of Valsalva aneurysm and formation of ventricular septal dissection and third-degree atrioventricular block: A case report. SAGE Open Med Case Rep. 2022;10:2050313X221140658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 66. | Ali Z, Asif T, Sheehy JP, Jacob D, Baweja P. Ruptured Sinus of Valsalva Aneurysm Causing Aorto-Atrial Fistula and Acute Heart Failure: A Rare Encounter. Eur J Case Rep Intern Med. 2020;7:001499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 67. | Kumar GA, Parimala PS, Jayaranganath M, Jagadeesh AM. Three-dimensional transesophageal echocardiography-guided transcathetar closure of ruptured noncoronary sinus of valsalva aneurysm. Ann Card Anaesth. 2017;20:S73-S75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 68. | Ravishankar M, Ghergherehchi A, Liu J, Jimenez E, Khalid U. Large Sinus of Valsalva Aneurysm Complicated by Thrombus Formation. Methodist Debakey Cardiovasc J. 2020;16:e8-e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 69. | Moshman RA, Ricketti DA, Mazzarelli JK. Severe Aortic Regurgitation From Sinus of Valsalva Aneurysm Prolapse. CASE (Phila). 2023;7:481-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 70. | Qiu J, Xie E, Wang Y, Wang W, Yu C, Luo X. Surgical Interventions Are Effective for Treating Unruptured Sinus of Valsalva Aneurysms. Front Cardiovasc Med. 2021;8:707147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 71. | Nakamura Y, Burkhart HM. Sinus of Valsalva aneurysm: Defining the optimal approach. J Card Surg. 2022;37:4456-4458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 72. | Au WK, Chiu SW, Mok CK, Lee WT, Cheung D, He GW. Repair of ruptured sinus of valsalva aneurysm: determinants of long-term survival. Ann Thorac Surg. 1998;66:1604-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 73. | Shaw M, Sharma A, Kumar S. Sinus of Valsalva Aneurysms: Basic Concepts and Imaging Evaluation Using Multidetector Computed Tomography. J Thorac Imaging. 2020;35:W30-W38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 74. | Marco LD, Comentale G, Bruno M, Lanzillotti V, Colletta M, Russo V, Pacini D, Casella G. To Treat or Not to Treat? This Is the Question… About the Incidental Finding of Double Sinus of Valsalva Aneurysm in A 91-Year-Old Woman. Braz J Cardiovasc Surg. 2022;37:268-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 75. | Mirdamadi A, Mirmohammadsadeghi M, Marashinia F, Nourbakhsh M. Sinus of Valsalva aneurysm: An uncommon presentation. ARYA Atheroscler. 2012;8:164-166. [PubMed] |
| 76. | Moustafa S, Mookadam F, Cooper L, Adam G, Zehr K, Stulak J, Holmes D. Sinus of Valsalva aneurysms--47 years of a single center experience and systematic overview of published reports. Am J Cardiol. 2007;99:1159-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 188] [Article Influence: 10.4] [Reference Citation Analysis (1)] |
| 77. | Banerjee S, Jagasia DH. Unruptured sinus of Valsalva aneurysm in an asymptomatic patient. J Am Soc Echocardiogr. 2002;15:668-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Topi B, John J, Agarwal A, Nerella N, Shetty V, Sadiq A, Shani J. An uncommon cause of a continuous murmur. Exp Clin Cardiol. 2012;17:148-149. [PubMed] |
| 79. | Wong BY, Bogart DB, Dunn MI. Echocardiographic features of an aneurysm of the left sinus of Valsalva. Chest. 1978;73:105-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 80. | Yang Y, Zhang L, Wang X, Lü Q, He L, Wang J, Wang B, Li L, Yuan L, Liu J, Ge S, Xie M. Echocardiographic diagnosis of rare pathological patterns of sinus of Valsalva aneurysm. PLoS One. 2017;12:e0173122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 81. | Dhawan I, Malik V, Sharma KP, Makhija N, Pangasa N. Transthoracic echocardiography versus transesophageal echocardiography for rupture sinus of Valsalva aneurysm. Ann Card Anaesth. 2017;20:245-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 82. | Tosun V, Korucuk N, Guntekin U. Rupture of Sinus of Valsalva Aneurysm into Left Atrium in a Patient who is a Candidate for Hepatic Transplantation. J Cardiovasc Echogr. 2018;28:130-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 83. | Hirapur I, Veeranna RM, Agrawal N. Classical windsock deformity of ruptured sinus of Valsalva: an unusual appearance on transthoracic echocardiography. BMJ Case Rep. 2014;2014:bcr2014204493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 84. | Gandhi S, Asija A, Chahal A, Singh K, Malhotra N, Lohchab SS. Classical windsock deformity of ruptured sinus of valsalva seen in transesophageal echocardiography. World J Pediatr Congenit Heart Surg. 2012;3:273-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 85. | Chigurupati K, Senniappan K, Gadhinglajkar S, Sreedhar R, Mathew T. Windsock deformity of interatrial septum. Ann Card Anaesth. 2016;19:722-723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 86. | Abdelkhirane C, Roudaut R, Dallocchio M. Diagnosis of ruptured sinus of Valsalva aneurysms: potential value of transesophageal echocardiography. Echocardiography. 1990;7:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 87. | Baur LH, Vliegen HW, van der Wall EE, Hazekamp M, Bootsma M, de Roos A, Bruschke AV. Imaging of an aneurysm of the sinus of Valsalva with transesophageal echocardiography, contrast angiography and MRI. Int J Card Imaging. 2000;16:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 88. | Dadana S, Kondapalli A, Madhwani V. A Case of Sinus of Valsalva Aneurysm Rupture Causing Cardiogenic Shock. Cureus. 2023;15:e44210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 89. | McGregor PC, Temtanakitpaisan Y, Hiltbolt A, Aragam JR. A spectrum of sinus of Valsalva aneurysm-From the young to the old. Echocardiography. 2017;34:1524-1530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 90. | Troupis JM, Nasis A, Pasricha S, Patel M, Ellims AH, Seneviratne S. Sinus valsalva aneurysm on cardiac CT angiography: assessment and detection. J Med Imaging Radiat Oncol. 2013;57:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 91. | Pampapati P, Rao HT, Radhesh S, Anand HK, Praveen LS. Multislice CT imaging of ruptured left sinus of Valsalva aneurysm with fistulous track between left sinus and right atrium. J Radiol Case Rep. 2011;5:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 92. | Liang T, Wang P. Imaging unruptured giant aneurysm of right sinus of Valsalva by 320-row dynamic volume computed tomography (CT): a case report. Int J Cardiovasc Imaging. 2015;31:1075-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 93. | Jain A, Achuthan G. Rupture of Sinus of Valsalva Aneurysm into Interventricular Septum: Role of Cardiac CT. Cureus. 2019;11:e5589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 94. | Xu B, Kocyigit D, Godoy-Rivas C, Betancor J, Rodriguez LL, Menon V, Jaber W, Grimm R, Flamm SD, Schoenhagen P, Svensson LG, Griffin BP. Outcomes of contemporary imaging-guided management of sinus of Valsalva aneurysms. Cardiovasc Diagn Ther. 2021;11:770-780. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 95. | Fathala A. Depiction of ruptured sinus of Valsalva aneurysms by cardiac computed tomography angiography. Exp Clin Cardiol. 2012;17:152-154. [PubMed] |
| 96. | Li Looi J, Kerr AJ. Sinus of Valsalva aneurysm and bicuspid aortic valve: detection and mechanism by cardiac magnetic resonance imaging. Clin Pract. 2011;1:e72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 97. | Breatnach CR, Walsh KP. Ruptured Sinus of Valsalva Aneurysm and Gerbode Defects: Patient and Procedural Selection: the Key to Optimising Outcomes. Curr Cardiol Rep. 2018;20:90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 98. | Moguillansky N, Bleiweis M, Reid J, Jacobs JP, Moguillansky D. Ruptured Sinus of Valsalva Aneurysm: Three Case Reports and Literature Review. Cureus. 2024;16:e59220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 99. | Hoey ET, Kanagasingam A, Sivananthan MU. Sinus of valsalva aneurysms: assessment with cardiovascular MRI. AJR Am J Roentgenol. 2010;194:W495-W504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 100. | Dev V, Goswami KC, Shrivastava S, Bahl VK, Saxena A. Echocardiographic diagnosis of aneurysm of the sinus of Valsalva. Am Heart J. 1993;126:930-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 101. | Lukács L, Bartek I, Haán A, Hankóczy J, Arvay A. Ruptured aneurysms of the sinus of Valsalva. Eur J Cardiothorac Surg. 1992;6:15-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 102. | Dayco JS, Dsouza A, Baciewicz F, Cardozo S. A rare variant of a ruptured sinus of valsalva aneurysm forming an aorto-atrial fistula: a case report and review of literature. Eur Heart J Case Rep. 2023;7:ytad018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 103. | Yagoub H, Srinivas BP, McCarthy J, Kiernan TJ. Gigantic unruptured sinus of Valsalva aneurysm presenting as an incidental murmur. BMJ Case Rep. 2012;2012:bcr2012006824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 104. | Regeer MV, van der Zwaan HB, Schoof PH, van Aarnhem EEHL. Surgical Repair of a Sinus of Valsalva Aneurysm. World J Pediatr Congenit Heart Surg. 2022;13:807-809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 105. | Jaswal V, Kumar V, Thingnam SKS, Puri GD. Surgical repair of ruptured sinus of Valsalva aneurysm: 13-year single center experience. J Card Surg. 2021;36:1264-1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 106. | van Son JA, Danielson GK, Schaff HV, Orszulak TA, Edwards WD, Seward JB. Long-term outcome of surgical repair of ruptured sinus of Valsalva aneurysm. Circulation. 1994;90:II20-II29. [PubMed] |
| 107. | Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, Mastracci TM, Mell M, Murad MH, Nguyen LL, Oderich GS, Patel MS, Schermerhorn ML, Starnes BW. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67:2-77.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1794] [Article Influence: 256.3] [Reference Citation Analysis (0)] |
| 108. | Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121:e266-e369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 952] [Cited by in RCA: 1208] [Article Influence: 80.5] [Reference Citation Analysis (0)] |
| 109. | Joshi AS, Aironi BD, Kotkar NS, Kulkarni DV, Jadhav UE, Nagare KM. Ruptured sinus of Valsalva aneurysms - our surgical experience of 7 years. Kardiochir Torakochirurgia Pol. 2021;18:100-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 110. | Ozkara A, Cetin G, Mert M, Erdem CC, Okcün B, Günay I. Sinus of Valsalva aneurysm: surgical approaches to complicated cases. ANZ J Surg. 2005;75:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 111. | Zikri MA, Stewart RW, Cosgrove DM. Surgical correction for sinus of Valsalva aneurysm. J Cardiovasc Surg (Torino). 1999;40:787-791. [PubMed] |
| 112. | Sarikaya S, Adademir T, Elibol A, Büyükbayrak F, Onk A, Kirali K. Surgery for ruptured sinus of Valsalva aneurysm: 25-year experience with 55 patients. Eur J Cardiothorac Surg. 2013;43:591-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 113. | Azakie A, David TE, Peniston CM, Rao V, Williams WG. Ruptured sinus of valsalva aneurysm: early recurrence and fate of the aortic valve. Ann Thorac Surg. 2000;70:1466-70; discussion 1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 114. | Gurbuz A, Iscan S, Gokalp O, Karaagac E, Girgin S, Aksun M. Surgical Management of Left Sinus of Valsalva Aneurysm Presenting with Exertional Chest Pain. Braz J Cardiovasc Surg. 2020;35:573-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 115. | Kerkar PG, Lanjewar CP, Mishra N, Nyayadhish P, Mammen I. Transcatheter closure of ruptured sinus of Valsalva aneurysm using the Amplatzer duct occluder: immediate results and mid-term follow-up. Eur Heart J. 2010;31:2881-2887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 116. | Chang CW, Chiu SN, Wu ET, Tsai SK, Wu MH, Wang JK. Transcatheter closure of a ruptured sinus of valsalva aneurysm. Circ J. 2006;70:1043-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 117. | Mumtaz ZA, Sagar P, Rajendran M, Sivakumar K. Transcatheter Versus Surgical Closure of Acute Ruptured Sinus of Valsalva Aneurysms with Associated Ventricular Septal Defects. Pediatr Cardiol. 2022;43:1494-1501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 118. | Fang ZF, Huang YY, Tang L, Hu XQ, Shen XQ, Tang JJ, Zhou SH. Long-term outcomes of transcatheter closure of ruptured sinus valsalva aneurysms using patent ductus arteriosus occluders. Circ J. 2014;78:2197-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 119. | Srivastava A, Radha AS. Transcatheter closure of ruptured sinus of valsalva aneurysm into the left ventricle: a retrograde approach. Pediatr Cardiol. 2012;33:347-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 120. | Ayati A, Toofaninejad N, Hosseinsabet A, Mohammadi F, Hosseini K. Transcatheter closure of a ruptured sinus of valsalva: a systematic review of the literature. Front Cardiovasc Med. 2023;10:1227761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 121. | Arora R, Trehan V, Rangasetty UM, Mukhopadhyay S, Thakur AK, Kalra GS. Transcatheter closure of ruptured sinus of valsalva aneurysm. J Interv Cardiol. 2004;17:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 122. | Xiao JW, Wang QG, Zhang DZ, Cui CS, Han X, Zhang P, Hou C, Zhu XY. Clinical outcomes of percutaneous or surgical closure of ruptured sinus of Valsalva aneurysm. Congenit Heart Dis. 2018;13:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 123. | Liu S, Xu X, Zhao X, Chen F, Bai Y, Li W, Zhang Y, Wang C, Xiang J, Wu G, Chen X, Qin Y. Percutaneous closure of ruptured sinus of Valsalva aneurysm: results from a multicentre experience. EuroIntervention. 2014;10:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 124. | Agrawal G, Agarwal M, Chintala K. Transcatheter closure of ruptured sinus of Valsalva aneurysm in a pregnant woman. J Cardiol Cases. 2015;12:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 125. | Vamsidhar A, Rajasekhar D, Vanajakshamma V. Transcatheter device closure of multiple defects in ruptured sinus of Valsalva aneurysm. Indian Heart J. 2015;67 Suppl 3:S74-S77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 126. | Ayati A, Toofaninejad N, Hosseinsabet A, Hosseini K, Hajizeinali A. Transcatheter closure of ruptured sinus of Valsalva: A report of first five cases in Tehran Heart Center, Iran. Clin Case Rep. 2023;11:e7036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |