Published online Dec 26, 2023. doi: 10.4330/wjc.v15.i12.642
Peer-review started: August 1, 2023
First decision: October 24, 2023
Revised: November 13, 2023
Accepted: December 11, 2023
Article in press: December 11, 2023
Published online: December 26, 2023
Processing time: 146 Days and 9.5 Hours
Tetralogy of Fallot (TOF) is one of the most common congenital heart defects, and surgery is the primary treatment. There are no precise guidelines on the treatment protocol for tricuspid regurgitation (TR) as a common complication of TOF repair. The timing for treatment in patients presenting with valve regurgitation after TOF repair is often difficult to determine. Here, we report the first case of sequential treatment of pulmonary and TR using interventional therapy.
We present the case of a 52-year-old female patient, who had a history of TOF repair at a young age. A few years later, the patient presented with pulmonary and tricuspid regurgitation. The symptoms persisted and TR worsened following percutaneous pulmonary valve implantation. Preoperative testing revealed that the patient’s disease had advanced to an intermediate to advanced stage and that her general health was precarious. Because open-heart surgery was not an option for the patient, transcatheter tricuspid valve replacement was suggested. This procedure was successful, and the patient recovered fully without any adverse effects. This case report may serve as a useful resource for planning future treatments.
Treatment of both valves should be considered in patients with tricuspid and pulmonary regurgitations following TOF repair. The interventional strategy could be an alternative for patients with poor general health.
Core Tip: Tetralogy of Fallot (TOF) is a common congenital heart disease. Complications following TOF repair, including pulmonary regurgitation, tricuspid regurgitation (TR), and cardiac arrhythmia, can have a negative impact on the prognosis. In this case, the patient had been treated with percutaneous pulmonary valve implantation after TOF repair, but developed TR progression and was treated with transcatheter tricuspid valve replacement. No standardized treatment guidelines for similar patients exist, and the timing and modalities of treatment remain controversial. Therefore, whether patients who develop both types of valve regurgitation after TOF repair should be treated simultaneously or sequentially is important. A treatment plan should be developed based on the patient’s overall condition, with interventional techniques being the optimal option for patients with poor baseline conditions.
- Citation: Cao JY, Ning XP, Zhou GW, Li BL, Qiao F, Han L, Xu ZY, Lu FL. Pulmonary and tricuspid regurgitation after Tetralogy of Fallot repair: A case report. World J Cardiol 2023; 15(12): 642-648
- URL: https://www.wjgnet.com/1949-8462/full/v15/i12/642.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i12.642
Tetralogy of Fallot (TOF) is one of the most common cyanotic congenital heart diseases accounting for 7%-10% of all congenital heart diseases[1]. Four distinct anatomical features characterized it: Ventricular septal defect, pulmonary outflow tract obstruction, overriding aortic root, and right ventricular hypertrophy. Surgery is the primary treatment with a 30-year survival rate of patients after surgery of approximately 90%[2-4]. However, the outcomes after TOF are strongly affected by postoperative complications, including pulmonary regurgitation (PR), tricuspid regurgitation (TR), heart failure, and arrhythmias, which are closely linked to death[5,6]. These patients often undergo multiple surgeries, and percutaneous intervention is an attractive option because the procedure can be complicated by multiple sternotomies[7,8]. Challa et al[9] described a case of successful percutaneous insertion of a transcatheter 29 mm Edwards Sapien XT valve into the tricuspid valve in a patient who underwent TOF repair[9]. Seckeler et al[10] reported the case of a high-risk patient with complex adult congenital heart disease who underwent successful percutaneous tricuspid valve-in-ring placement with a SAPIEN 3 valve. Roberts et al[11] described 15 patients with congenital heart disease who had successful percutaneous tricuspid valve replacement with Melody valves, one of whom had TOF. Although numerous publications have described the percutaneous insertion of bioprosthetic tricuspid valves in patients with congenital heart disease, this is the first case described involving a LuX-Valve used in a patient after TOF repair and percutaneous pulmonary valve implantation (PPVI).
A 52-year-old female patient was admitted because of poor cardiac function and massive pleural and abdominal effusions.
Two years prior, she underwent PPVI with a Venus P valve device[12] at another hospital because of severe PR and TR. The patient improved immediately after treatment but soon developed recurrent right heart failure with severe TR, pulmonary hypertension, and extensive pleural effusion and ascites. In the previous year, she had been hospitalized multiple times for recurrent ascites with early cirrhotic changes on liver ultrasonography. The symptoms keep getting worse, presenting with progressive shortness of breath on exertion, orthopnea, paroxysmal nocturnal dyspnea, and bilateral lower limb swelling. The symptoms were severe enough to make conversation difficult and limited her activities of daily life.
She was admitted with a 20-year TOF repair history and a 2-year history of PPVI. The patient was diagnosed with TOF at an early age and did not undergo corrective surgery until she was an adult because of her poor financial status. Postoperative complications, such as PR, TR, and right heart failure, had progressively worsened in recent years. Cardiac ultrasonography showed ventricular septum repair, despite the patient’s inability to recall details of the procedure.
The patient did not have a family history of congenital heart disease, heart failure, or respiratory illness.
A physical examination revealed reduced bilateral breathing sounds with slight tremor. Dilatation of the jugular vein and pitted edema of the lower extremities. From a cardiac perspective, the New York Heart Association functional class was IV. Comprehensive preoperative evaluation included the 6-minute walking distance of 221 meters; a Kansas City Cardiomyopathy Questionnaire result of 58 for quality of life assessment; and an The Society of Thoracic Surgeons score of 15.57% for surgical risk evaluation.
Laboratory examinations revealed varying degrees of reduction in peripheral blood cytopenia, liver and kidney function impairment, and a significant increase in B-type natriuretic peptide (517.2 pg/mL) and N-terminal pro B-type natriuretic peptide (1490 pg/mL).
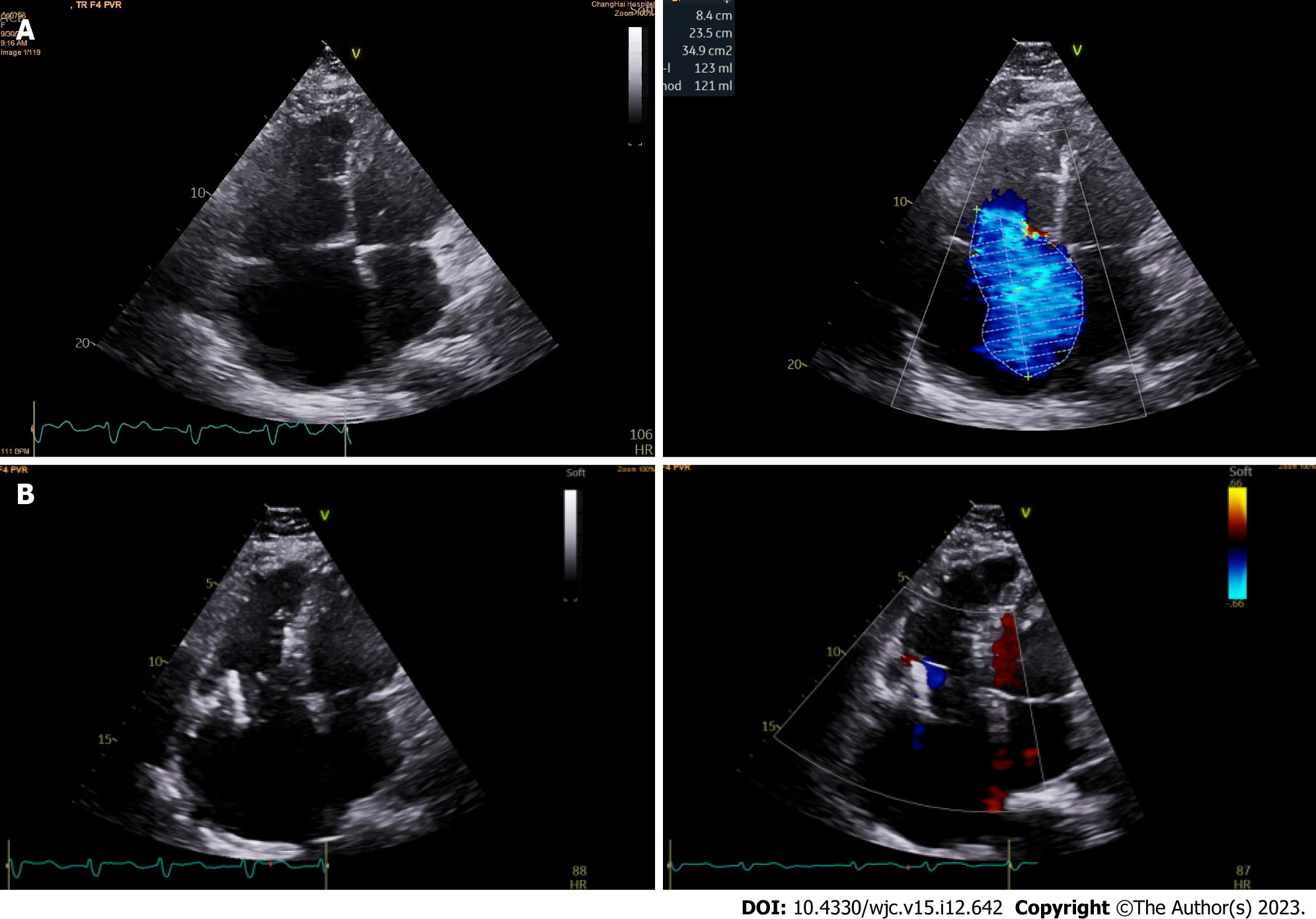
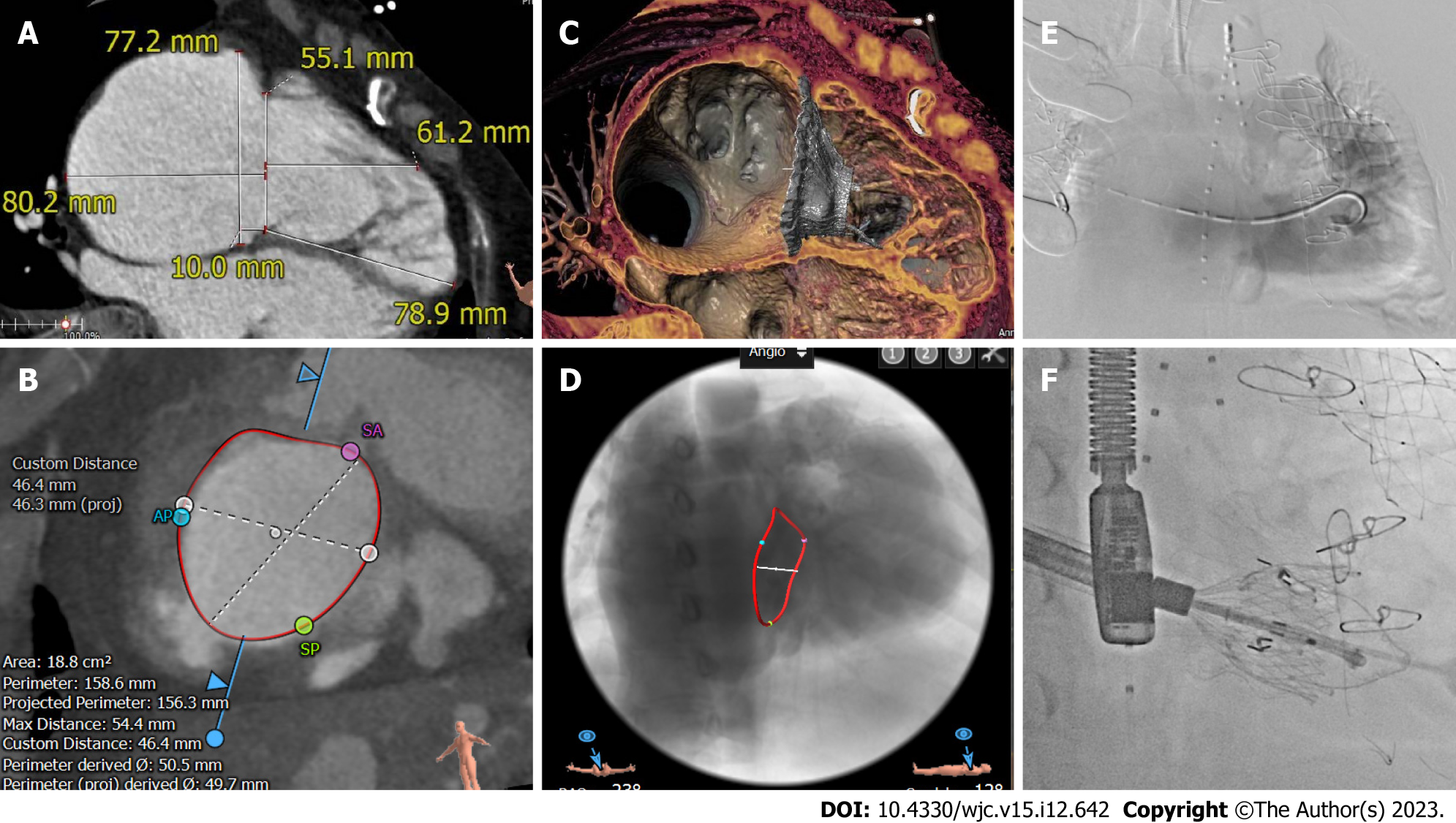
Transthoracic echocardiography (Figure 1A) indicated torrential TR (121 mL), a dilated right heart, and a preserved left ventricular ejection fraction (LVEF) of 56%. The tricuspid annular plane systolic excursion (TAPSE) was 11 mm, and the fractional area change (FAC) was 49%. Preoperative computed tomography (CT) (Figure 2A and B) showed an enlarged right heart and a widened inferior vena cava.
The final diagnosis was severe TR.
Owing to massive pleural and abdominal effusions, the patient was admitted to the hospital and underwent closed drainage of the thorax and abdomen. Torasemide (10 mg twice daily) and sacubitril valsartan (25 mg twice daily) were administered. After one month of medication adjustment, the patient underwent transcatheter tricuspid valve intervention and replacement.
After evaluation by a multidisciplinary team, the patient was deemed unsuitable for a second surgery because of her poor physical condition and inability to withstand the trauma of traditional surgery. Based on the patient’s anatomy and condition, we decided to use the LuX-Valve developed by the team for transcatheter tricuspid valve replacement (TTVR), and a size of 30-55 was chosen (Figure 2C and D). The Institutional Review Board of Changhai Hospital approved the study protocol and data publication (No. CHEC2018-136).
The procedure was performed in the digital subtraction angiography operating room under transesophageal echocardiography and X-ray fluoroscopy guidance. We chose a minimally invasive right-fifth intercostal thoracotomy to create the delivery channel. Following angiography to determine the TR volume, the delivery system was sent to the right heart until it reached the tricuspid valve. The valve delivery system was gently retracted, and the prosthesis was released to capture the anterior leaflet. The delivery system was adjusted to ensure the graspers were in good contact with the valve leaflet and released into the right atrial disc. Finally, the anchor was secured to the ventricular septum until the valve was adjusted to minimize perivalvular leakage. The delivery system was removed, and angiography showed satisfactory valve function with no regurgitation or paravalvular leakage (Figure 2E and F). The pressure in the right atrium immediately decreased from 41 mmHg to 34 mmHg (Videos 1 and 2).
Transthoracic echocardiography 1 mo after the operation showed that the valve was in position with no obvious regurgitation or paravalvular leakage, with an LVEF of 57% (Figure 1B), and the enlargement of the right atrium was significantly improved (from 327 mL to 253 mL). The TAPSE and FAC became 13mm and 38%, respectively. The mean abdominal circumference reduced from 916.51 mm to 810 mm.
PR, a common complication of TOF repair, is a major cause of distant cardiac insufficiency and death[7]. Up to 36% of patients who undergo early TOF repair require pulmonary valve replacement within 30 years of surgery[13]. Compensatory cardiac mechanisms can maintain early homeostasis after TOF repair. However, with disease progression, prolonged exposure to PR and chronic right heart volume overload can lead to right heart dysfunction, progressive right ventricular dilatation, an enlarged tricuspid annulus, and worsening TR[14,15]. The incidence of moderate-to-severe TR after TOF repair is 32%[16]. Owing to delayed treatment for PR, although patients with combined TR improve immediately after pulmonary valve replacement, TR worsens and even leads to arrhythmias and sudden death in more than 15% of patients during long-term follow-up[17]. Numerous studies have discussed the type of treatment that is more beneficial for patients who have undergone TOF repair and subsequently develop pulmonary and tricuspid valve lesions. Most authors believe that tricuspid valve repair should be performed concurrently with pulmonary valve replacement in patients with combined moderate-to-severe TR. In the first multicenter study, the Surgical Correction of Tricuspid Insufficiency in Adult Congenital Patients requiring Pulmonary Valve Replacement (SCOTIA-PVR) and concurrent tricuspid valve intervention was shown to be safe and to improve early tricuspid valve function more than pulmonary valve replacement alone in patients with significant TR after TOF[18]. However, some studies concluded that the long-term results of pulmonary valve replacement with simultaneous tricuspid valve repair are controversial. Studies have shown no statistical difference at 6 mo between patients who underwent concurrent tricuspid valve repair and those who underwent pulmonary valve replacement alone[19]. Our patient underwent PPVI after TOF repair when she developed PR and TR. However, the patient’s symptoms did not improve significantly, and right heart failure continued to progress after treatment. The reasons are as follows: (1) Although we could not obtain information about her past treatment, we speculated that the repair resulted in adhesion between the tricuspid valve and the ventricular patch. Therefore, treatment with PR does not make any sense for TR; (2) As described previously, pulmonary valve replacement alone may not improve TR, and treatment is still required. This finding indicates that both PR and TR should be considered after TOF repair; and (3) Infective endocarditis. Several studies have reported endocarditis after valve placement. Patel et al[20] described 4 cases of endocarditis after transcatheter pulmonary valve replacement. This may have been caused by the eccentric turbulence and thrombogenesis. Butera et al[21] also reported 2 cases of endocarditis following valve placement. Valve implantation is a risk factor for the development of infective endocarditis, making early monitoring and anti-infective therapy after the interventions indispensable[22].
Lesions after TOF repair are often amenable to transcatheter intervention. In selected cases, PR can be treated with transcatheter valve insertion[23]. Regarding sequential or concurrent therapy that should be used in managing PR and TR, ongoing monitoring of RV function is an important part of clinical assessment. Meanwhile, multicenter large-scale clinical studies or randomized controlled studies may help clarify whether concurrent tricuspid valve repair can improve patient prognosis.
The LuX-Valve is a novel radial-force-independent TTVR device that we previously designed. Its skirt-shaped, self-expandable, nitinol-valved stent can adapt well to an enlarged annulus and effectively prevent perivalvular leakage. The radial force-independent anchoring concept can minimize damage to the conduction bundle and reduce the occurrence of an atrioventricular block. Pre-clinical and early clinical trials[24-26] have shown that the LuX-Valve is a relatively safe and effective treatment for patients with severe TR via right atrial access. Patients who reach an advanced stage of the disease are in poor general condition and cannot tolerate conventional open heart surgery. Based on our experience, interventional treatment may be a preferable option and should be considered when managing patients with TOF with advanced disease and a challenging clinical status.
Attention should be paid to the treatment of patients with postoperative complications of TOF. Multiple clinical studies are meaningful, and the formulation of relevant guidelines is helpful for the diagnosis and treatment of the disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lakusic N, Croatia; Sef D, United Kingdom S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY
| 1. | Starr JP. Tetralogy of fallot: yesterday and today. World J Surg. 2010;34:658-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Chiu SN, Wang JK, Chen HC, Lin MT, Wu ET, Chen CA, Huang SC, Chang CI, Chen YS, Chiu IS, Chen CL, Wu MH. Long-term survival and unnatural deaths of patients with repaired tetralogy of Fallot in an Asian cohort. Circ Cardiovasc Qual Outcomes. 2012;5:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Murphy JG, Gersh BJ, Mair DD, Fuster V, McGoon MD, Ilstrup DM, McGoon DC, Kirklin JW, Danielson GK. Long-term outcome in patients undergoing surgical repair of tetralogy of Fallot. N Engl J Med. 1993;329:593-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 653] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 4. | Nollert G, Fischlein T, Bouterwek S, Böhmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of Fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol. 1997;30:1374-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 481] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 5. | Gatzoulis MA, Till JA, Somerville J, Redington AN. Mechanoelectrical interaction in tetralogy of Fallot. QRS prolongation relates to right ventricular size and predicts malignant ventricular arrhythmias and sudden death. Circulation. 1995;92:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 469] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 6. | Ghai A, Silversides C, Harris L, Webb GD, Siu SC, Therrien J. Left ventricular dysfunction is a risk factor for sudden cardiac death in adults late after repair of tetralogy of Fallot. J Am Coll Cardiol. 2002;40:1675-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 311] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 7. | Faries CM, Sengupta A, Alexis SL, Tadros RO, Octeau D, Barnes HJ, Tang GHL. Transcatheter Tricuspid and Pulmonary Valve Repair and Replacement. Surg Technol Int. 2020;36:217-223. [PubMed] |
| 8. | Filsoufi F, Anyanwu AC, Salzberg SP, Frankel T, Cohn LH, Adams DH. Long-term outcomes of tricuspid valve replacement in the current era. Ann Thorac Surg. 2005;80:845-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 165] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Challa A, Markham R, Walters D. Percutaneous valve in valve in the tricuspid position in a patient with Tetralogy of Fallot. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Seckeler MD, White SC, Jenkins J, Klewer SE. Treatment of tricuspid regurgitation and para-ring leak in tetralogy of Fallot with oversized SAPIEN 3 valve-in-ring implantation. J Card Surg. 2018;33:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Roberts PA, Boudjemline Y, Cheatham JP, Eicken A, Ewert P, McElhinney DB, Hill SL, Berger F, Khan D, Schranz D, Hess J, Ezekowitz MD, Celermajer D, Zahn E. Percutaneous tricuspid valve replacement in congenital and acquired heart disease. J Am Coll Cardiol. 2011;58:117-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 12. | Cao QL, Kenny D, Zhou D, Pan W, Guan L, Ge J, Hijazi ZM. Early clinical experience with a novel self-expanding percutaneous stent-valve in the native right ventricular outflow tract. Catheter Cardiovasc Interv. 2014;84:1131-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Frigiola A, Hughes M, Turner M, Taylor A, Marek J, Giardini A, Hsia TY, Bull K. Physiological and phenotypic characteristics of late survivors of tetralogy of fallot repair who are free from pulmonary valve replacement. Circulation. 2013;128:1861-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Hickey EJ, Veldtman G, Bradley TJ, Gengsakul A, Webb G, Williams WG, Manlhiot C, McCrindle BW. Functional health status in adult survivors of operative repair of tetralogy of fallot. Am J Cardiol. 2012;109:873-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Oechslin EN, Harrison DA, Harris L, Downar E, Webb GD, Siu SS, Williams WG. Reoperation in adults with repair of tetralogy of fallot: indications and outcomes. J Thorac Cardiovasc Surg. 1999;118:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 172] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Mahle WT, Parks WJ, Fyfe DA, Sallee D. Tricuspid regurgitation in patients with repaired Tetralogy of Fallot and its relation to right ventricular dilatation. Am J Cardiol. 2003;92:643-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Kobayashi J, Kawashima Y, Matsuda H, Nakano S, Miura T, Tokuan Y, Arisawa J. Prevalence and risk factors of tricuspid regurgitation after correction of tetralogy of Fallot. J Thorac Cardiovasc Surg. 1991;102:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Deshaies C, Trottier H, Khairy P, Al-Aklabi M, Beauchesne L, Bernier PL, Dhillon S, Gandhi SK, Haller C, Hancock Friesen CL, Hickey EJ, Horne D, Jacques F, Kiess MC, Perron J, Rodriguez M, Poirier NC; Canadian Congenital Cardiac Collaborative (4C). Tricuspid Intervention Following Pulmonary Valve Replacement in Adults With Congenital Heart Disease. J Am Coll Cardiol. 2020;75:1033-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Cramer JW, Ginde S, Hill GD, Cohen SB, Bartz PJ, Tweddell JS, Earing MG. Tricuspid repair at pulmonary valve replacement does not alter outcomes in tetralogy of Fallot. Ann Thorac Surg. 2015;99:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Patel M, Iserin L, Bonnet D, Boudjemline Y. Atypical malignant late infective endocarditis of Melody valve. J Thorac Cardiovasc Surg. 2012;143:e32-e35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Butera G, Milanesi O, Spadoni I, Piazza L, Donti A, Ricci C, Agnoletti G, Pangrazi A, Chessa M, Carminati M. Melody transcatheter pulmonary valve implantation. Results from the registry of the Italian Society of Pediatric Cardiology. Catheter Cardiovasc Interv. 2013;81:310-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 22. | Verzelloni Sef A, Jaggar SI, Trkulja V, Alonso-Gonzalez R, Sef D, Turina MI. Factors associated with long-term outcomes in adult congenital heart disease patients with infective endocarditis: a 16-year tertiary single-centre experience. Eur J Cardiothorac Surg. 2023;63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Villafañe J, Feinstein JA, Jenkins KJ, Vincent RN, Walsh EP, Dubin AM, Geva T, Towbin JA, Cohen MS, Fraser C, Dearani J, Rosenthal D, Kaufman B, Graham TP Jr; Adult Congenital and Pediatric Cardiology Section, American College of Cardiology. Hot topics in tetralogy of Fallot. J Am Coll Cardiol. 2013;62:2155-2166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 140] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 24. | Lu F, Qiao F, Lv Y, An Z, Liu X, Cao P, Song Z, Xu Z. A radial force-independent bioprosthesis for transcatheter tricuspid valve implantation in a preclinical model. Int J Cardiol. 2020;319:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Lu FL, Ma Y, An Z, Cai CL, Li BL, Song ZG, Han L, Wang J, Qiao F, Xu ZY. First-in-Man Experience of Transcatheter Tricuspid Valve Replacement With LuX-Valve in High-Risk Tricuspid Regurgitation Patients. JACC Cardiovasc Interv. 2020;13:1614-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 26. | Lu FL, An Z, Ma Y, Song ZG, Cai CL, Li BL, Zhou GW, Han L, Wang J, Bai YF, Liu XH, Wang JF, Meng X, Zhang HB, Yang J, Dong NG, Hu SS, Pan XB, Cheung A, Qiao F, Xu ZY. Transcatheter tricuspid valve replacement in patients with severe tricuspid regurgitation. Heart. 2021;107:1664-1670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |