Copyright
©The Author(s) 2021.
World J Cardiol. Aug 26, 2021; 13(8): 254-270
Published online Aug 26, 2021. doi: 10.4330/wjc.v13.i8.254
Published online Aug 26, 2021. doi: 10.4330/wjc.v13.i8.254
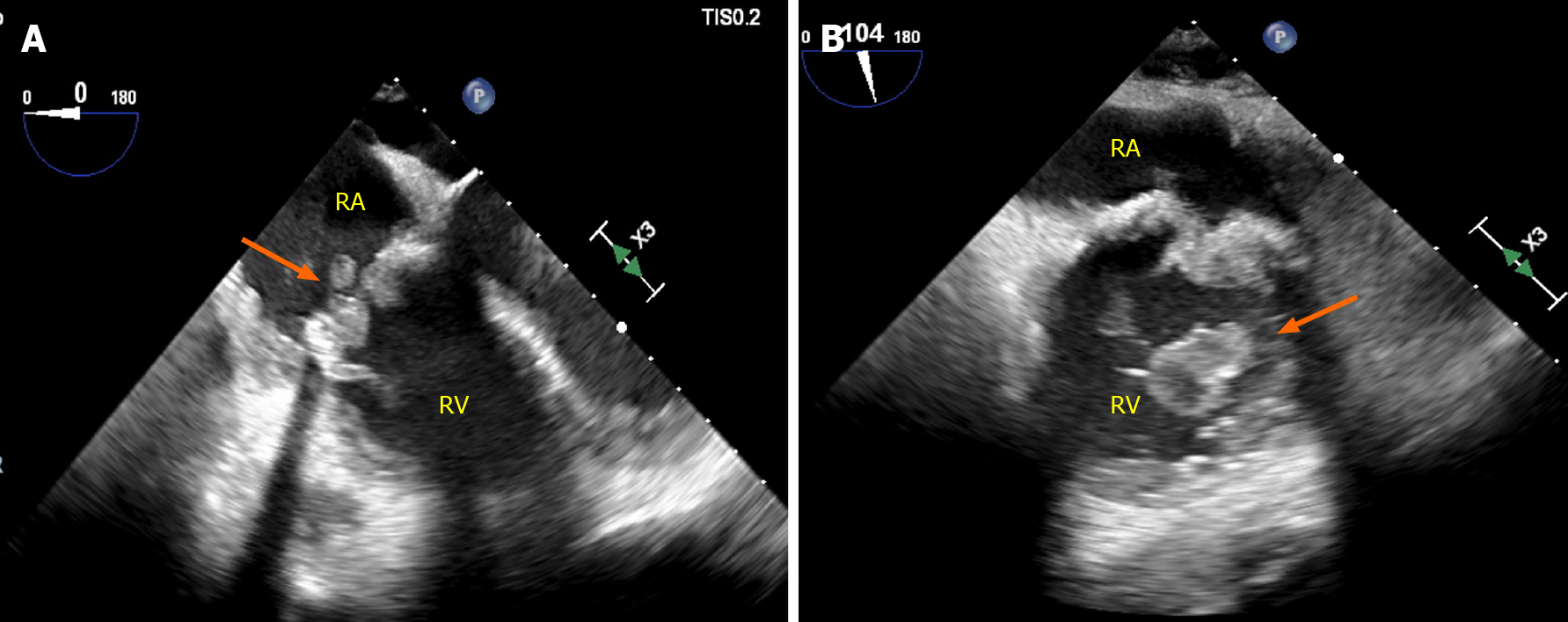
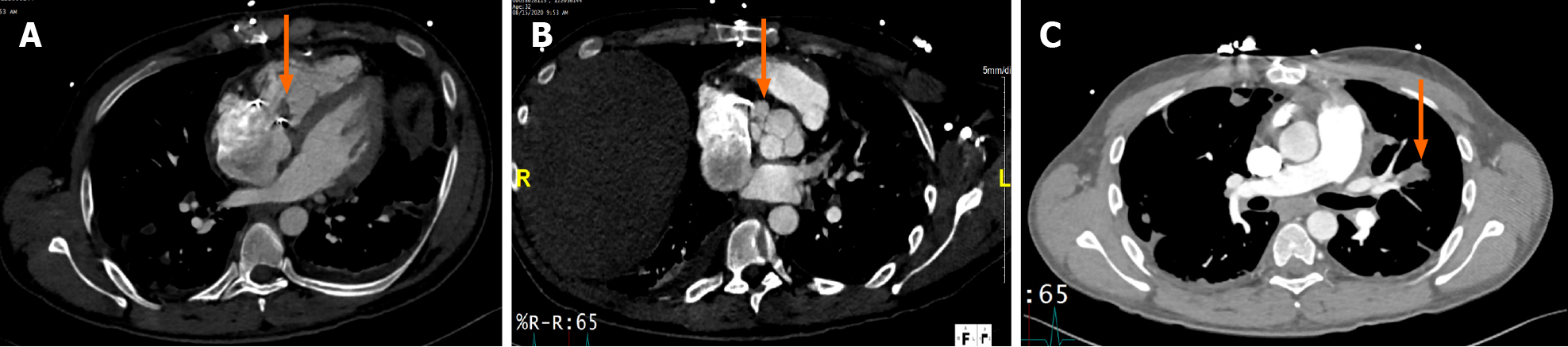
Figure 1 Prosthetic valve endocarditis complicating prior bioprosthetic tricuspid valve replacement secondary to intravenous drug abuse relapse.
Thirty-two year-old male with a history of intravenous drug abuse status post bioprosthetic tricuspid valve replacement presenting with methicillin-sensitive Staphylococcus Aureus prosthetic valve endocarditis due to relapsed drug abuse. Images from Panel A and B demonstrate a tricuspid valve prosthesis at mid esophageal 4 chamber right ventricular focused (A) and modified bicaval views (B) with severe thickening and attached vegetations on both sides of the valve. RA: Right atrium; RV: Right ventricle.
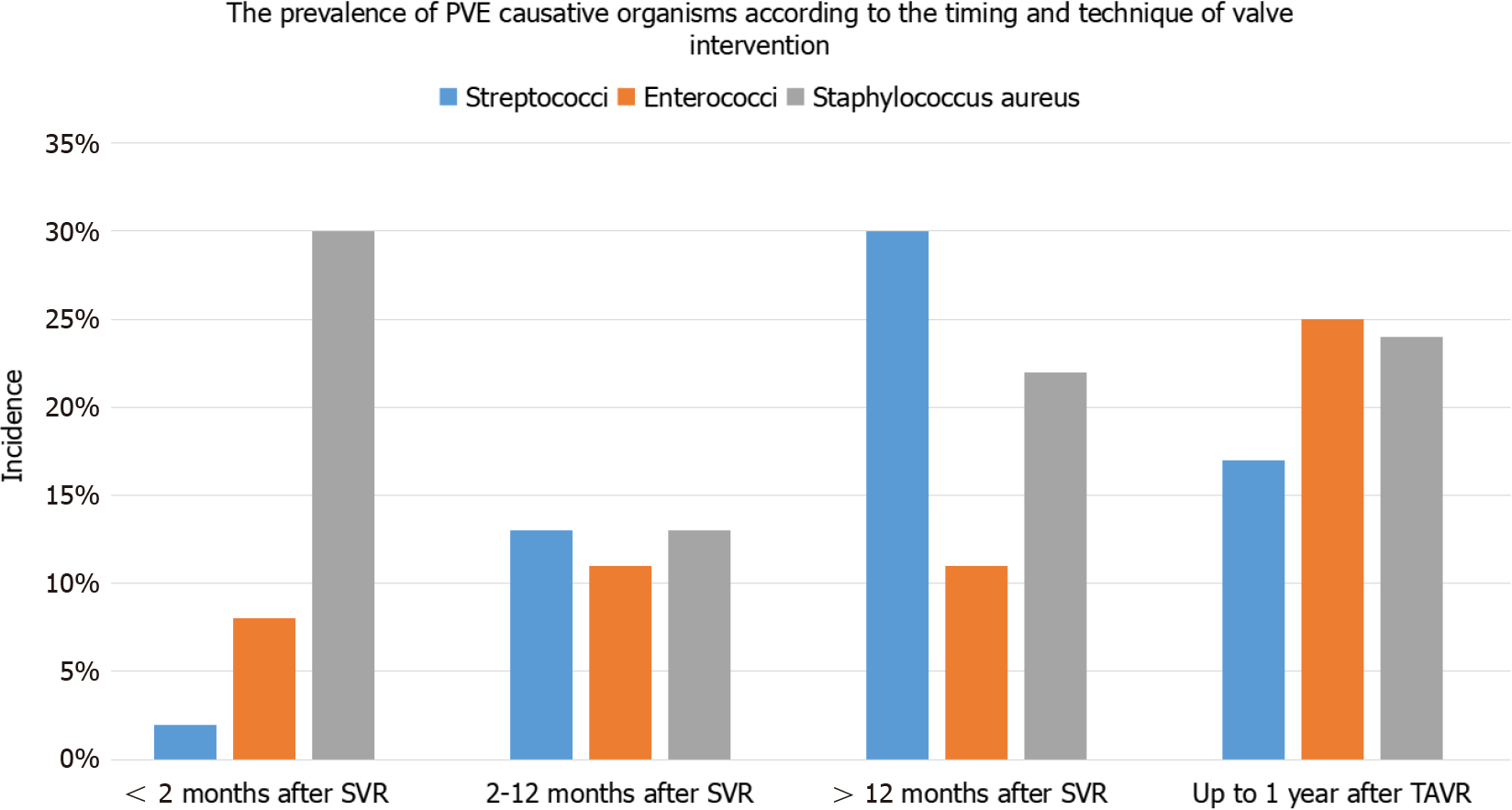
Figure 2 Prevalence of causative organisms according to timing and technique of valve intervention.
The prevalence of causative organisms of prosthetic valve endocaridits in surgical left-sided valve replacement among 579 patients pooled from 5 studies[2,32-34,79] and transcatheter aortic valve replacement among 275 patients from 2 studies[35,36], categorized according to time since the index procedure. PVE: Prosthetic valve endocarditis; SVR: Surgical valve replacement; TAVR: transcatheter aortic valve replacement.
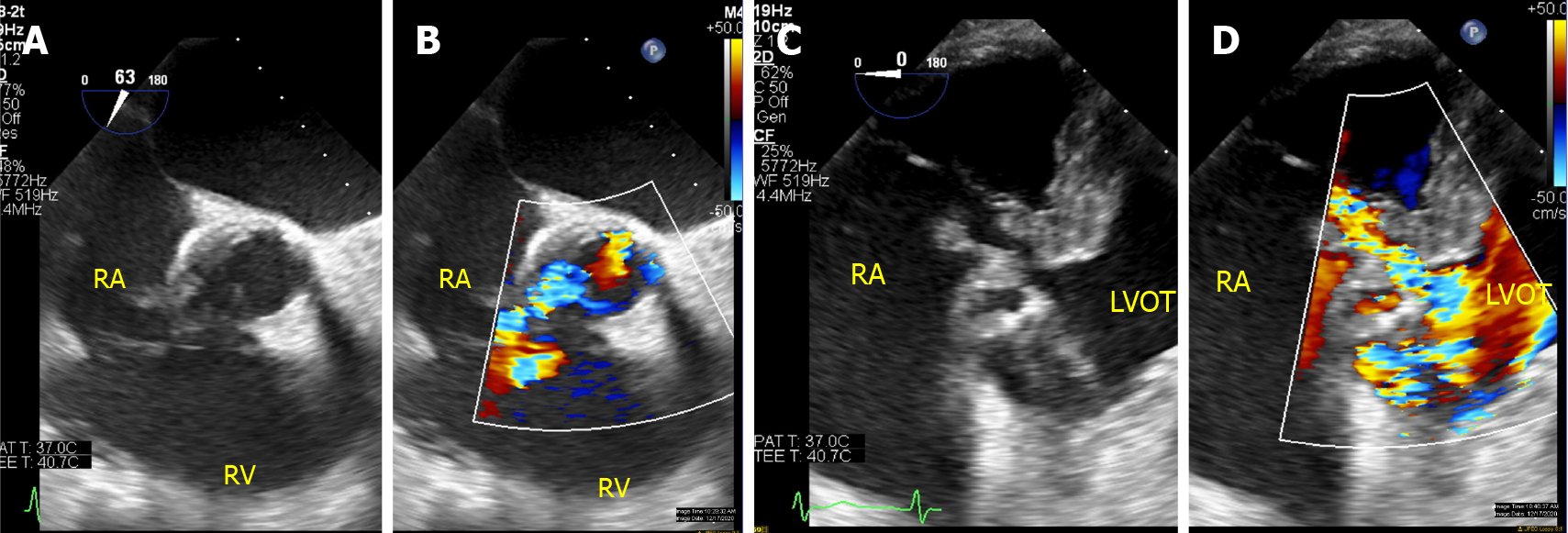
Figure 3 Para-valvular fistula in a patient with complicated endocarditis involving prior stentless aortic valve.
Eighty-two year-old male with a history of coronary artery bypass grafts and stentless aortic valve replacement presenting with Streptococcus Gallolyticus prosthetic valve endocarditis complicated by aortic root abscess and fistulous tract treated with homograft aortic root replacement (25 mm Cryo-Life aortic allograft root), bovine pericardial closure of aortic root to right atrium fistula, right atrium reconstruction with bovine patch and bypass revision. A and B: TEE interrogating the aortic valve replacement with color compare demonstrated thickening of the leaflets and abnormal color flow into the right atrium; C and D: Additional imaging from deep transgastric views with color compare in the left ventricular outflow tract demonstrated a complex fistulous tract (Gerbode-type defect) communicating the left ventricular outflow track, right atrium and aortic root. RA: Right atrium; RV: Right ventricle; LVOT: Left ventricular outflow tract.
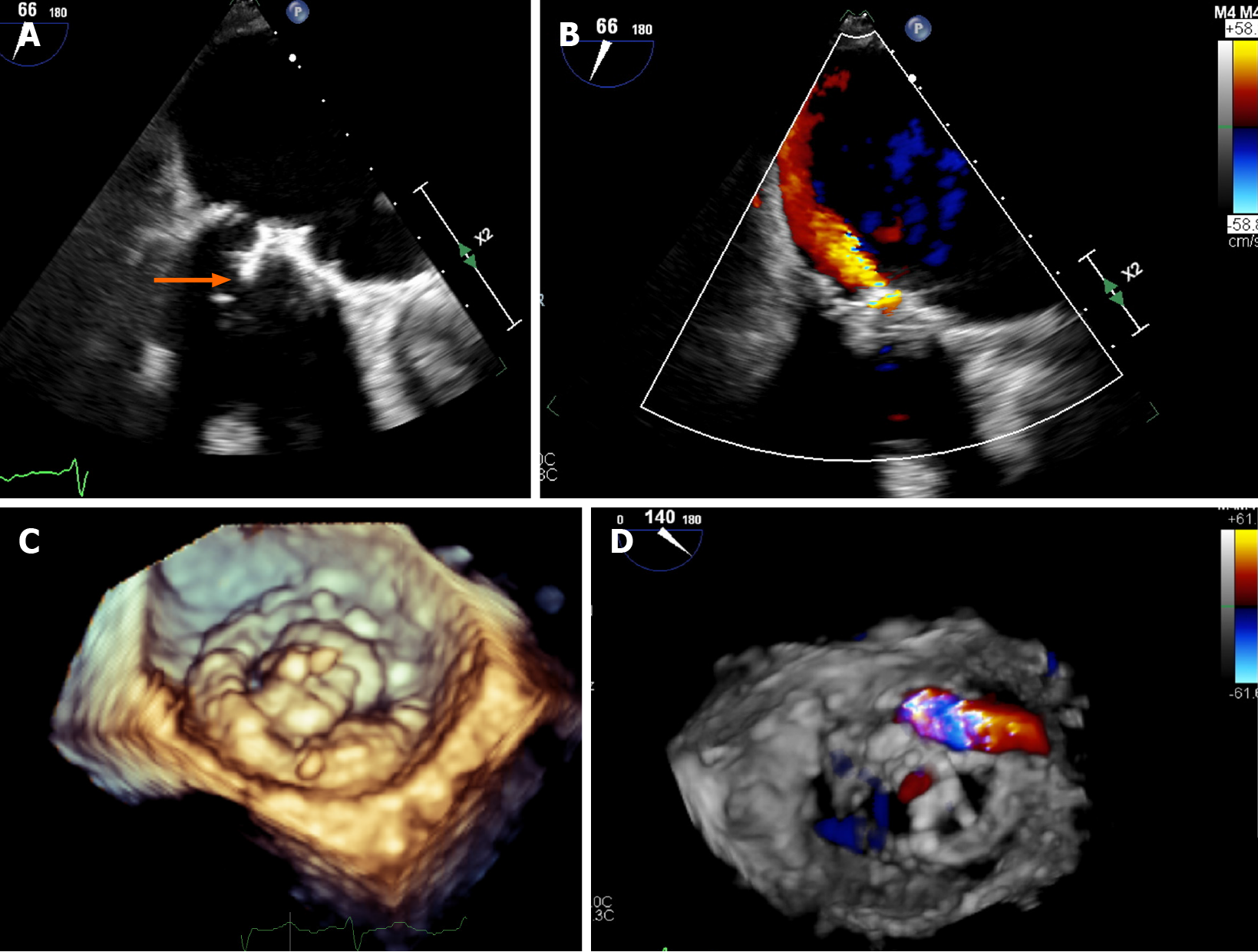
Figure 4 Transesophageal echocardiogram in a patient with mitral valve replacement endocarditis with 3D-reconstruction.
Sixty-six year-old male with a history of coronary artery bypass graft and mitral valve replacement three years before presenting with Enterococcus Faecalis endocarditis. Transesophageal echocardiogram demonstrated severe structural degeneration of the mitral valve replacement with attached vegetation (A: Arrow). Color Doppler analysis demonstrated a large jet arising from the leaflet body consistent with prosthetic leaflet perforation confirmed by 3D-reconstruction (B-D).
Figure 5 Cardiac computed tomography in a patient with tricuspid valve replacement endocarditis with peri-valvular extension.
Thirty-two year-old male with a history of intravenous drug abuse status post bioprosthetic tricuspid valve replacement presenting with methicillin-sensitive Staphylococcus Aureus due to relapsed drug abuse. Cardiac computed tomography demonstrated thickening of the valve leaflets (A: Arrow) and a 2.7 cm × 1.9 cm × 1.4 cm lobulated pocket of free-flowing blood/contrast interposed between the tricuspid annulus and the aortic annulus consistent with abscess/fistula (B: Arrow). Prominent pulmonary septic embolism was also detected (C: Arrow).
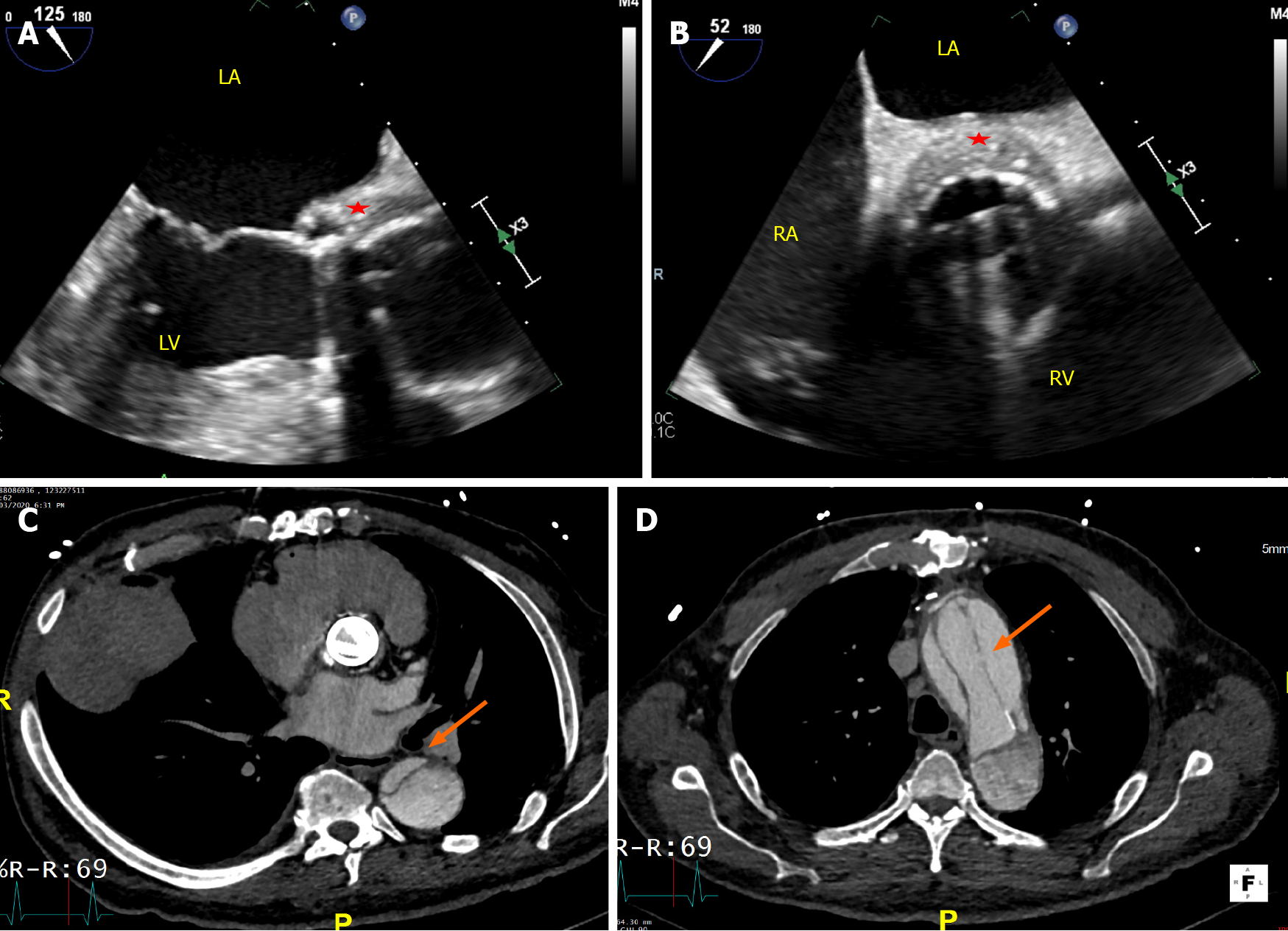
Figure 6 Transesophageal echocardiogram and cardiac computed tomography in a patient with metallic aortic valve replacement endo
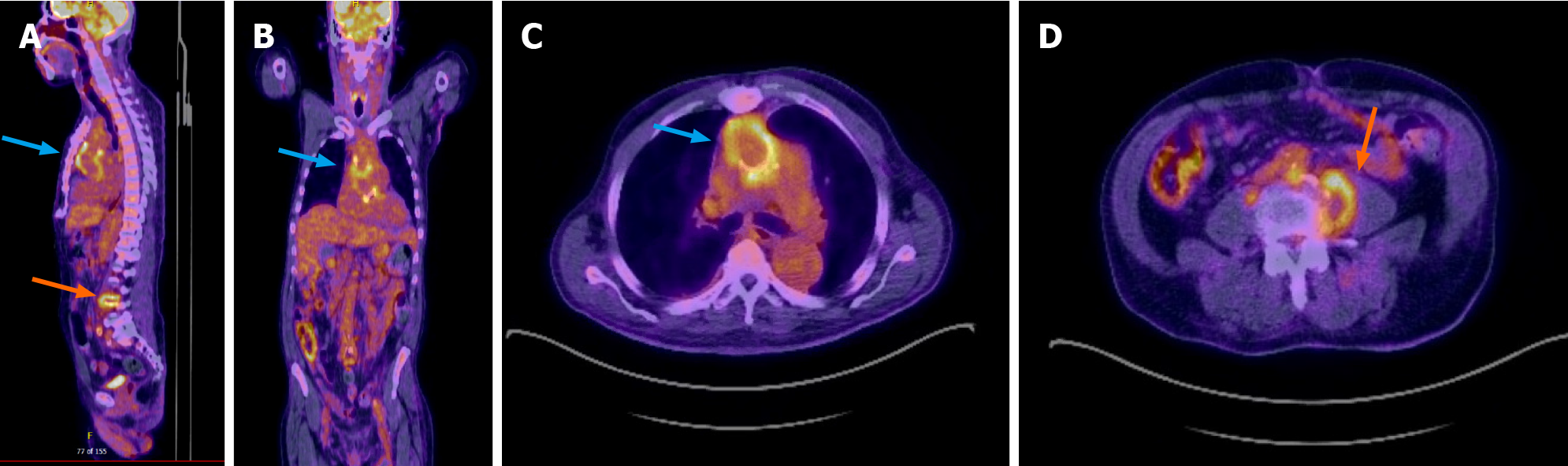
Figure 7 18-fluorodeoxyglucose photon emission tomography/computed tomography in a patient with prosthetic aortic valve endocar
- Citation: Lo Presti S, Elajami TK, Zmaili M, Reyaldeen R, Xu B. Multimodality imaging in the diagnosis and management of prosthetic valve endocarditis: A contemporary narrative review. World J Cardiol 2021; 13(8): 254-270
- URL: https://www.wjgnet.com/1949-8462/full/v13/i8/254.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i8.254