Published online Nov 27, 2022. doi: 10.4331/wjbc.v13.i5.83
Peer-review started: August 22, 2022
First decision: September 26, 2022
Revised: September 30, 2022
Accepted: November 23, 2022
Article in press: November 23, 2022
Published online: November 27, 2022
Processing time: 94 Days and 20.6 Hours
The excessive concentration of leptin has negative effects on all aspects of female reproduction. Despite this established relationship, the exact role of leptin in women’s fertility is not clear enough and needs more clarification.
To evaluate the serum leptin levels in Sudanese women and to ascertain the relationship between serum leptin levels and unexplained infertility (UI).
A matched (age and body mass index) case-control study was conducted from March 2021 to February 2022. The study samples were 210 women with UI and 190 fertile women of reproductive age who were attending the maternity hospitals and fertility clinics in Khartoum state Sudan. The serum concentration of leptin and other serum biomarkers were determined using enzyme-linked immunosorbent assays.
The results showed that there was a highly statistically significant difference between the two groups (P < 0.001) for all examined eight biomarkers. Whereby, leptin, luteinizing hormone (LH)/follicular stimulating hormone (FSH) ratio, prolactin hormone (PRL) and testosterone (T) were significantly higher in the UI group compared with the control group. In contrast, FSH and estradiol (E2)/T ratio were significantly lower in the UI group than in the control group and the effect size test for the difference between the two groups was very large (effect size > 0.80), for leptin level, LH/FSH ratio, PRL level, and E2/T ratio, and large (effect size 0.50- ≤ 0.80) for FSH and T.
This study reveals that leptin could be a potential biomarker for UI in Sudanese women and it may be useful for identifying women with a high risk of infertility.
Core Tip: A matched (age and body mass index) case-control study was conducted to find the serum leptin levels in Sudanese women and to ascertain the relationship between serum leptin levels and unexplained infertility (UI). A total of 400 women of reproductive age were recruited for this study (210 with UI and 190 fertile women). Leptin, luteinizing hormone/follicular stimulating hormone (FSH) ratio, prolactin hormone and testosterone (T) were significantly higher in the UI group compared with the control group. In contrast, FSH and estradiol/T ratio were significantly lower in the UI group than in the control group. Thus, this study reveals that leptin could be a potential biomarker for UI in Sudanese women and it may be useful for identifying women with a high risk of infertility.
- Citation: Abdulslam Abdullah A, Ahmed M, Oladokun A, Ibrahim NA, Adam SN. Serum leptin level in Sudanese women with unexplained infertility and its relationship with some reproductive hormones. World J Biol Chem 2022; 13(5): 83-94
- URL: https://www.wjgnet.com/1949-8454/full/v13/i5/83.htm
- DOI: https://dx.doi.org/10.4331/wjbc.v13.i5.83
According to the World Health Organization, infertility is the inability of sexually active couples within 1 year who aren’t under any contraceptive methods, to achieve clinically recognizable pregnancy[1]. Infertility can be due to male factors, female factors, combined factors or unknown (unexplained) factors[2,3]. Despite the discoveries and improvements in reproduction medicine, infertility prevalence seems to increase over time[4], where it is found to affect 10% of couples worldwide[1]. Nevertheless, the current knowledge and practices in infertility treatment proved a suitable treatment for almost all infertility types and their etiologies, except for unexplained infertility (UI), which is when standard-approved infertility tests have not found a clear cause for the couple’s inability to achieve pregnancy[5]. Consequently, for such couples with UI, it may be very frustrating[6].
Studies from all around the world reported different prevalence’s of UI (10%-37%)[1,3,7,8], whereby the highest prevalence was reported in low and middle-income countries (LMICs)[3,8]. In addition, women were reported to be responsible for at least 50% of all UI cases[1,8]. For all the above-mentioned reasons, UI has been identified as a public health priority, especially in LMICs like Sudan, which creates an urgent necessity to search and identify the unknown causes of infertility. Therefore, to achieve this goal, the reproductive system in women has been studied massively to find clear causes of UI. Studies proposed many possible causes of female UI, however, the diagnostic evidence for these proposed causes is still weak[9,10] and can’t be counted on in infertility diagnosis.
Adipokines such as leptin were found to have a positive relationship with UI in females and they can be used as reliable predictive biomarkers for UI in women[11-13]. Leptin is a peptide hormone encoded in the LEP gene on chromosome 7q32.1[14]. Leptin is mainly produced by white adipocytes cells and when it is secreted in the plasma, it bonds with many binding proteins such as immunoglobulin superfamily members siglec-6 and binds to the leptin receptor in the brain. This reaction activates the downstream signaling pathway of feeding inhibition and promotes energy expenditure, hence, it plays a key role in regulating basal metabolism, food consumption, energy expenditure and body weight[15-17].
Besides, leptin plays an important role in the physiological regulation of several neuroendocrine axes, such as hypothalamic-pituitary-gonadal, -thyroid, -growth hormone and -adrenal axes[15,16]. In particular, the effect of leptin has been studied on the hypothalamic-pituitary-ovarian (HPO) axis in females and its relationship with reproduction. These studies revealed that leptin and leptin receptors were extensively expressed in the HPO axis and this can be a strong argument about the effect of leptin on the reproduction process[18-20].
Leptin was found to have direct regulatory effects (inhibitory and stimulatory depending on its concentration) on all parts of the HPO axis[15,16]. In line with this conclusion, experimental evidence shows that the excessive concentration of leptin was found to have negative effects on all aspects of reproduction; ovarian steroidogenesis, folliculogenesis, oogenesis, and HPO axis hormones secretion [gonadotrophin-releasing hormone (GnRH), follicular stimulating hormone (FSH), luteinizing hormone (LH), prolactin hormone (PRL), anti-Mullerian hormone (AMH), estradiol (E2) as well as progesterone and testosterone (T)][16,21-23]. In addition, mice treated with anti-leptin drugs had a higher number of Graafian follicles in their ovaries compared with the non-treated group and this indicates that peripheral leptin may act as an inhibitor of ovarian follicle development and also on the HPO axis hormones[24].
Despite the established relationship between leptin and female reproduction, the exact role of leptin in women’s infertility is not clear enough and a reasonable conclusion is that “we need further investigations to fill this diagnostic gap”. Whereby, some studies, reported high levels of serum leptin in infertile women[25-27], other studies reported increased leptin levels in both fertile and infertile women, thus, high serum leptin levels in these patients were not a contributing factor for infertility[28]. The available findings of the role of leptin in female infertility are still contradicted, unexplained and need more clarification[29-34]. However, a meta-analysis of six studies which were conducted to find the relationship between leptin level and UI found that leptin level was higher in women with UI compared with fertile women, hence the study concludes that leptin can be used as an early predictive serum marker for UI in women[12]. Despite the many difficulties in diagnosis and treating UI, this early detection may improve pregnancy possibilities and reduce the treatment cost through increased clinical surveillance and clinical intervention for UI patients. Thus, the aim of this study was to evaluate the serum leptin levels in Sudanese women and to ascertain the relationship between serum leptin levels, UI and selected serum biomarkers between UI and fertile women.
This matched [age and body mass index (BMI)] case-control study was conducted in Khartoum state-central Sudan during the period from March 2021 to February 2022. Study participants were recruited using the systematic random sampling technique from the largest health care facilities providing assisted conception services and modern antenatal care in the state and Sudan. In general, these hospitals and centers were purposefully selected, namely; Prof. El-Sir Abo Elhassan Fertility Center, Omdurman Maternity Hospital, Nile Fertility Center, Antenatal Care Hospital in Khartoum for Fertility, Khartoum Reproductive Health Care Center, Sudan Assisted Reproductive Clinic, University of Khartoum Fertility Center, Saad Abualila Teaching Hospital, Banoun Fertility Center and Hawwa Center for Fertility.
The required sample size of the current study (sample size to compare two means) was calculated using Open Epi software version 3.01. Based on the given inputs; 5% significance level and 80% power of the study with a mean difference of serum leptin levels of 0.97 between UI and fertile women[12], and a standard deviation of 4.29 for UI group and 2.11 for the fertile group, the minimum required sample size for the significant result was 382 (with 1:1 case-control ratio), however, to consider the non-response and attrition rates throughout the study period, a 5% have been added (5% attrition -38%). Therefore, a total of 420 Sudanese women were recruited for the study (210 infertile women with UI and 210 fertile women).
The current study targeted 420 Sudanese women between the age of 18 years to 44 years. The case group consisted of 210 women with UI and these cases were chosen from patients who had tried but were unable to conceive for at least a 1 year of regular unprotected sexual intercourse. In addition, they had regular menstruation, open uterine tubes, a normal size and shape of the uterine cavity according to the hysterosalpingography and no ovarian abnormalities such as fibroids and ovarian cysts according to transvaginal ultrasonography[2]. Also, of note, normal fertility tests of the woman, the male partner had a normal spermiogram “with a concentration of at least 15 million per milliliter of sperm, a motility value over 70 % and morphology of more than 4 % with normal forms”[2]. The control group consisted of 210 fertile and non-pregnant women who had at least one healthy 2-year-old child (end of lactation).
Furthermore, study participants (cases and controls) were excluded from this study if they had any of the following illnesses; any sexual transmitted diseases, hypertension, diabetes, endocrine disorders, autoimmune/immunocompromised conditions, a history of genetic disease or severely obese (BMI of 35 kg/m2 or more). In addition to that, women were also excluded if they were undergoing the effect of any aromatase inhibitors and/or anti-inflammatory medicines or if they were under the effects of hormonal contraception within the last 6 mo. Finally, any women who refused to sign the informed consent or withdrew during the study were excluded.
All study participants were examined by the primary investigator after obtaining written informed consent, obtaining their height (in meters) and weight (in kilograms) to find the BMI. Meanwhile, the hip measured at the level of the greater trochanter (in meter) and waist circumference measured at the level of the umbilicus (in meter) to determine the waist/hip ratio (WHR).
During the laboratory visits which occurred between 09:00 and 10:30 am for the women in the follicular phase of the cycle (on day 3 of the menstrual cycle) who were overnight fasting, a 5 mL sample of their peripheral blood was collected by venipuncture in a plain test tube and then the fresh blood was allowed to clot to get sera. Following the blood draw, the serum was separated by centrifuge at 3000 rpm for 5 min and immediately stored in a deep freezer at a temperature of -20 °C for subsequent analysis.
Serum levels of leptin hormone, FSH, LH, PRL, AMH, E2 and T were measured using the enzyme-linked immunosorbent assay (ELISA) method and the ELISA kits of the DRG diagnostics labs (DRG Diagnostics, Marburg Germany). All measurements were carried out in duplicate to ensure the quality of the results.
All data from this study were sorted and recorded in Microsoft Excel version 2016, cleaned, and then transferred to STATA software, version 16.0 (Stata Corp LLC, 77845 Texas, United States) for analysis. The data were presented as mean ± SD with a 95% confidence interval (CI), also tables and figures were used for data presentation. The normal distribution test of the study variables (Univariate, pairwise and multivariate[35]) was performed using the Shapiro Wilk test and data were considered as normally distributed if the P value is more than 0.05. The mean differences of the study variables (age, BMI, WHR, leptin serum level, FSH, LH, LH/FSH ratio, PRL, AMH, E2, T and E2/T ratio) between the two study groups were assessed using a two-tailed independent t-test for normally distributed variables (leptin serum level, LH/FSH ratio, PRL and T) and Mann-Whitney U-test for non-normally distributed variables (age, BMI, WHR, FSH, LH, AMH, E2 and E2/T ratio). Moreover, to magnitude the difference between the two groups we used effect sizes index for the difference between the two groups (Cohen’s D for normally distributed data and rank biserial correlation for non-normally distributed data), and the threshold for interpreting these effect sizes were as follows: Small ≤ 0.20; medium ≤ 0.05; large ≤ 0.80; and very large > 0.80[36].
To better understand the study data, the association between leptin serum level and the other study variables, a correlation test was performed using Pearson’s correlation for normally distributed data and Spearman’s rank correlation for non-normally distributed data. Finally, to predict the serum leptin levels in Sudanese women, a multiple linear regression test was performed using the best-fit model after verifying all test assumptions. In addition, the collinearity was checked using the variance inflation factor. For all of the above-mentioned statistical tests, the threshold of significance was P value of < 0.05.
The current study recruited 420 Sudanese women (210 cases and 210 controls), of whom 20 women from the control group were removed due to the loss of the samples and the follow-up, giving a response rate of 95.2%. Finally, the study included a total of 400 women (210 women with UI as case subjects and 190 fertile women as control subjects). The study’s two groups were matched by age and BMI, whereby the mean age (in years) was 28.59 and 28.44 for the case group and control group, respectively, and the mean BMI value was 24.67 and 24.41 for the case group and control group, respectively. The two groups had almost a similar mean value of WHR (0.844 for the UI group and 0.837 for the fertile group) (Table 1).
| Variable | Unexplained infertility group, n = 210 | Fertile group, n = 190 | Effect size | P value | ||
| mean ± SD | 95%CI | mean ± SD | 95%CI | |||
| Age in yr | 28.59 ± 5.22 | 27.87-29.3 | 28.44 ± 4.95 | 27.73-29.15 | 0.0202 | 0.7314 |
| BMI in kg/m2 | 24.67 ± 4.08 | 24.11-25.22 | 24.41 ± 4.38 | 23.78-25.03 | 0.0462 | 0.4244 |
| WHR | 0.844 ± 0.108 | 0.829-0.859 | 0.837 ± 0.114 | 0.821-0.854 | 0.0322 | 0.5754 |
| Leptin in ng/mL | 30.05 ± 5.22 | 29.34-30.76 | 22.89 ± 6.48 | 21.96-23.81 | 1.2251 | < 0.0013 |
| FSH in IU/L | 6.42 ± 2.82 | 6.04-6.81 | 9.52 ± 2.79 | 9.12-9.92 | 0.5582 | < 0.0014 |
| LH in IU/L | 10.32 ± 3.37 | 9.86-10.78 | 7.78 ± 2.19 | 7.46-8.09 | 0.4232 | < 0.0014 |
| LH/FSH ratio | 1.7 ± 0.339 | 1.65-1.75 | 0.82 ± 0.075 | 0.81-0.83 | 3.5021 | < 0.0013 |
| PRL in μg/L | 17.48 ± 3.434 | 17.01-17.95 | 12.52 ± 3.736 | 11.99-13.06 | 1.3851 | < 0.0013 |
| AMH in ng/mL | 2.07 ± 0.418 | 2.01-2.13 | 2.43 ± 0.624 | 2.34-2.52 | 0.3452 | < 0.0014 |
| E2 in nmol/L | 121.61 ± 30.54 | 117.46-125.77 | 154.86 ± 47.83 | 148.01-161.7 | 0.4282 | < 0.0014 |
| T in nmol/L | 2.43 ± 0.52 | 2.36-2.51 | 2.12 ± 0.62 | 2.04-2.21 | 0.5431 | < 0.0013 |
| E2/T ratio | 49.59 ± 3.97 | 49.05-50.13 | 72.69 ± 5.52 | 71.9-73.48 | 0.9872 | < 0.0014 |
Table 1 displayed the serum biomarkers investigated in this study; leptin, FSH, LH, LH/FSH ratio, PRL, AMH, E2, T and E2/T ratio. The results showed that there was a highly statistically significant difference between the two studied groups (P < 0.001) for all the above biomarkers. However, this statistical difference cannot be explained alone without weighting, therefore, to quantify this difference, an effect size test for the difference between the two groups was performed and the result found that the difference between the two groups was very large (effect size > 0.80) for leptin level, LH/FSH ratio, PRL level, and E2/T ratio, and large (effect size 0.50- ≤ 0.80) for FSH and T. To summarize the above-mentioned differences in the examined biomarkers, leptin, LH/FSH ratio, PRL and T were significantly higher in the UI group compared with the control group. In contrast, FSH, and E2/T ratio were significantly lower in the UI group than in the control group.
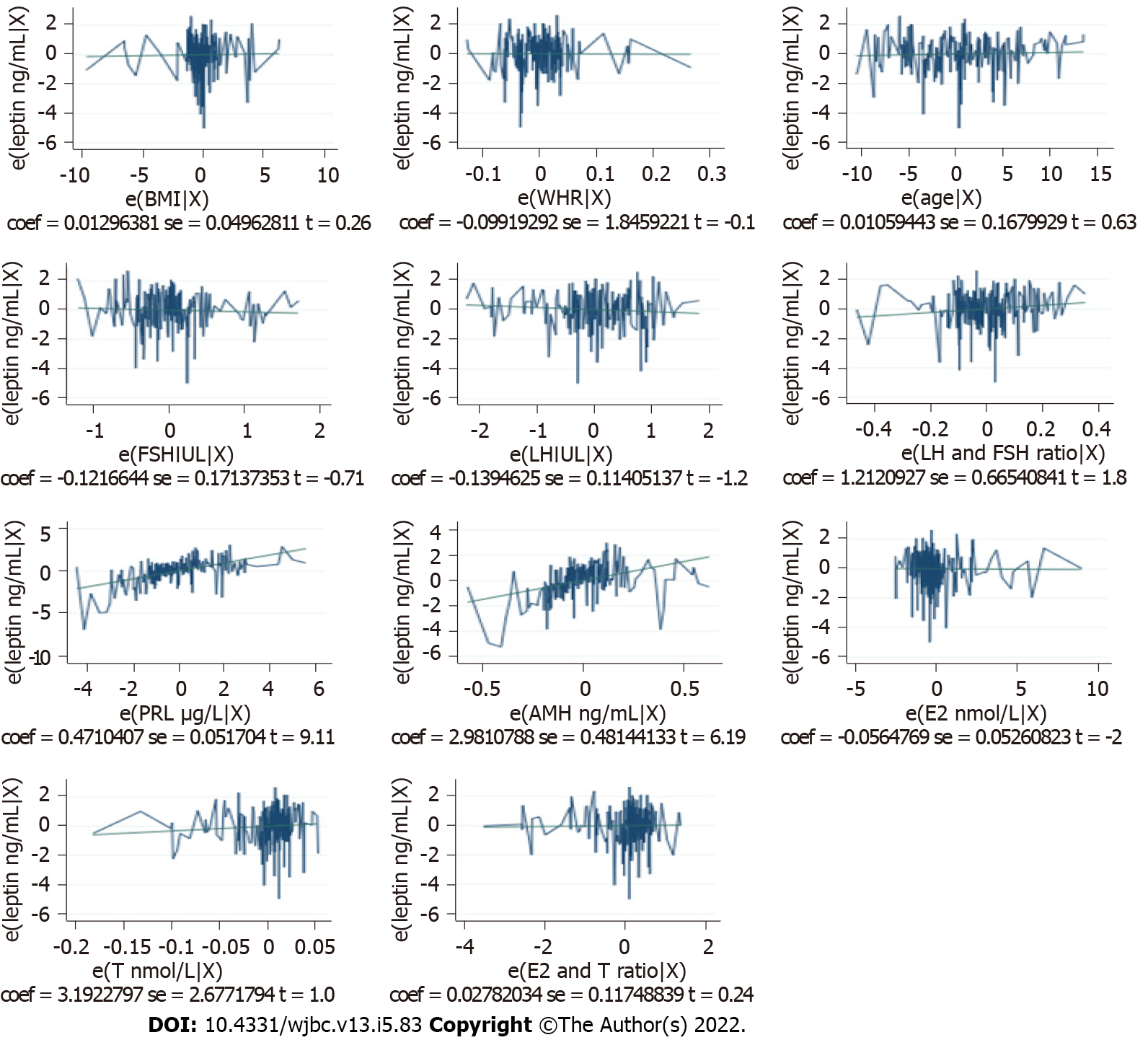
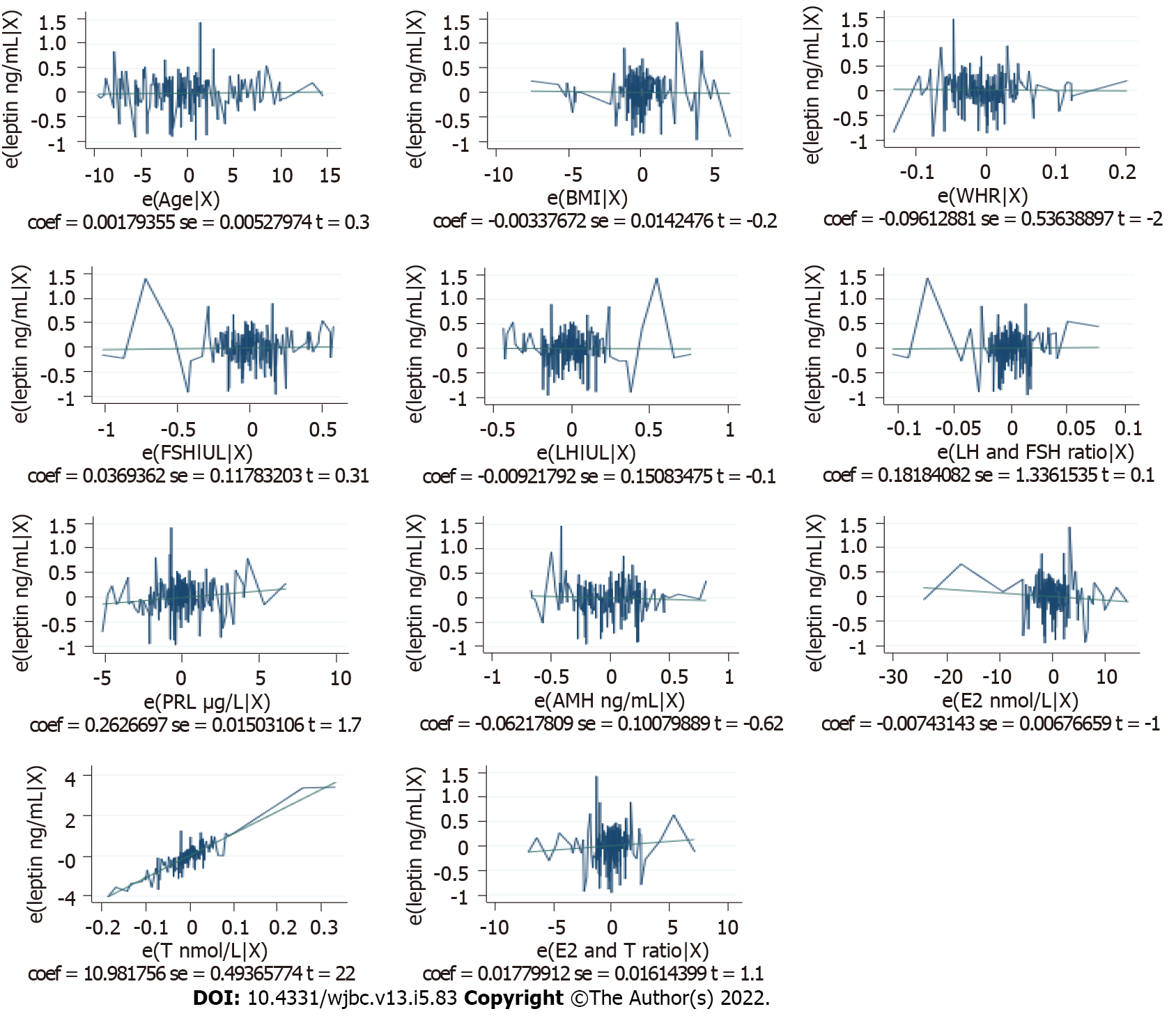
The association between leptin and other study variables in both the cases and control groups was shown in Table 2. The study results found a highly significant negative correlation between leptin levels and FSH and LH in both fertile and infertile women. On the other hand, leptin levels had a highly significant positive correlation with LH/FSH ratio, PRL, AMH, E2 and T in the two groups. However, the associations between leptin levels and E2/T ratio were positive in the two groups but statistically significant only in the UI group. This noticeable high association between leptin and other study variables requires further investigations so a multiple linear regression was performed to identify the independent predictors of serum leptin levels and the final model reveals that only PRL and AMH levels can be independent predictors (P < 0.05) of serum leptin level in Sudanese women with UI. The fully detailed prediction models were shown in Table 3 and Figures 1 and 2 below.
| Variable | Unexplained Infertility group | Fertile group | ||
| r value | P value | r value | P value | |
| Age in yr | -0.0441 | 0.524 | -0.1072 | 0.142 |
| BMI in kg/m2 | 0.1582 | 0.022 | 0.3982 | < 0.001b |
| WHR | 0.1411 | 0.041 | 0.3891 | < 0.001b |
| FSH in IU/L | -0.8542 | < 0.001b | -0.7231 | < 0.001b |
| LH in IU/L | -0.7272 | < 0.001b | -0.6831 | < 0.001b |
| LH/FSH | 0.7142 | < 0.001b | 0.2312 | < 0.001a |
| PRL in μg/L | 0.8882 | < 0.001b | 0.8882 | < 0.001b |
| AMH in ng/mL | 0.9282 | < 0.001b | 0.9172 | < 0.001b |
| E2 in nmol/L | 0.9162 | < 0.001b | 0.9672 | < 0.001b |
| T in nmol/L | 0.9322 | < 0.001b | 0.3592 | 0.033 |
| E2/T ratio | 0.4782 | < 0.001b | 0.1382 | 0.057 |
| Independent variable | Model, leptin ng mL | Coefficients | P value | Beta, 95%CI | |
| Lower | Upper | ||||
| Constant | Unexplained infertility | 6.812 | 0.274 | -5.436 | 19.060 |
| Fertile | -1.076 | 0.527 | -4.426 | 2.274 | |
| Age | Unexplained infertility | 0.011 | 0.529 | -0.023 | 0.044 |
| Fertile | 0.002 | 0.734 | -0.009 | 0.012 | |
| BMI | Unexplained infertility | 0.013 | 0.794 | -0.085 | 0.111 |
| Fertile | -0.003 | 0.813 | -0.031 | 0.025 | |
| WHR | Unexplained infertility | -0.099 | 0.957 | -3.739 | 3.541 |
| Fertile | -0.096 | 0.858 | -1.155 | 0.962 | |
| FSH in IU/L | Unexplained infertility | -0.122 | 0.479 | -0.460 | 0.216 |
| Fertile | -0.037 | 0.754 | -0.196 | 0.269 | |
| LH in IU/L | Unexplained infertility | -0.139 | 0.223 | -0.364 | 0.085 |
| Fertile | 0.009 | 0.951 | -0.307 | 0.288 | |
| LH/FSH | Unexplained infertility | 1.212 | 0.070 | -0.100 | 2.524 |
| Fertile | 0.182 | 0.892 | -2.455 | 2.819 | |
| PRL in μg/L | Unexplained infertility | 0.471 | < 0.001a | 0.369 | 0.573 |
| Fertile | 0.026 | 0.082 | -0.003 | 0.056 | |
| AMH in ng/mL | Unexplained infertility | 2.981 | < 0.001a | 2.032 | 3.930 |
| Fertile | -0.062 | 0.538 | -0.261 | 0.137 | |
| E2 in nmol/L | Unexplained infertility | -0.006 | 0.915 | -0.109 | 0.098 |
| Fertile | -0.007 | 0.274 | -0.021 | 0.006 | |
| T in nmol/L | Unexplained infertility | 3.192 | 0.235 | -2.087 | 8.472 |
| Fertile | 10.982 | < 0.001a | 10.008 | 11.956 | |
| E2/T ratio | Unexplained infertility | 0.028 | 0.813 | -0.204 | 0.260 |
| Fertile | 0.018 | 0.272 | -0.014 | 0.050 | |
Leptin plays an important role in the function of the HPO axis by affecting the release of GnRH, gonadotrophins and aromatase enzymes from the hypothalamus, pituitary gland, and ovaries, respectively. Hence, it has a significant role in the reproductive process and reproductive hormone levels[16]. Studies on the possible relationship between leptin levels and UI showed that leptin was one of the most accurate serum biomarkers to detect UI in women[12,13,30], therefore, this study was conducted to find the serum leptin levels in UI Sudanese women and their relationship with 4 gonadotropin biomarkers and 4 ovarian biomarkers after eliminating the effect of all possible confounding factors (age, BMI and WHR).
The current study revealed that the leptin serum level was significantly higher in women with UI compared with fertile women, 30.05 (95%CI: 29.34-30.76) and 22.89 (95%CI: 21.96-23.81), respectively, with a very large effect size of 1.225. This result is in line with the findings reported from Turkey[29], India[30], Iran[31] and Iraq[32,37], and in contrast with findings reported from Pakistan[33] and Iran[34]. The difference between the current findings reported from Sudan and other findings reported from other countries (which all were non-African countries), could be due to the difference in genetic makeup, sample sizes, age and BMI.
In this study, the four examined gonadotrophins biomarkers (LH, FSH, LH/FSH ratio and PRL) were significantly different between the two groups, whereby LH, LH/FSH ratio and PRL were significantly higher in the UI group than in the fertile group. Meanwhile, FSH was significantly lower in the UI group than in a fertile group. Furthermore, the high leptin serum level was strongly associated with the low level of FSH and LH (negative association) and the high level of LH/FSH ratio and PRL in UI women (positive association). These findings are consistent with the previous findings from Turkey[29], Iraq[32,37] and Iran[31]. However, the reported change in these biomarkers (high PRL, low LH and FSH) can be related to female infertility due to the fact that low FSH and LH levels together with the high level of PRL in females can induce ovulatory dysfunction, implantation defects and abnormal ovarian steroidogenesis[13,38]. In addition, from the examined ovarian biomarkers; AMH, E2, and E2/T ratio were significantly lower in the UI group compared with the fertile group. This low level of AMH, E2, and E2/T ratio in the UI group may affect the follicular growth and maturation[38-40]. This is in agreement with the findings of Demir et al[29] in Turkey, Tafvizi and Masomi[31] in Iran, Baig et al[33] in Pakistan and Abduljalal et al[37] in Iraq.
Meanwhile, similar to the results of Demir et al[29] in Turkey and Abduljalal et al[37] in Iraq, our study found that T was significantly higher in the UI group compared with the fertile group and this high T level can signal a potential female fertility problem that is mainly related to ovulatory dys
Despite the above, leptin was positively associated with AMH, T, and E2/T ratio and negatively associated with E2 in UI women. These results were supported by experimental findings which found that the high leptin level decreases the gene expression of the steroidogenic enzymes which leads to high T levels, low E2 and AMH levels[44]. An interesting finding in our study was that from all examined biomarkers, the strongest independent predictors of serum leptin levels in women with UI were only PRL and AMH levels, thus we can propose that leptins effect on female fertility by its cleared effect on two of the most important fertility hormones. The strength of this study was its control of all possible confounding factors and the relatively large sample size. Yet, limitations observed include that the study should have compared serum and follicular leptin levels.
The results of this study found that leptin, LH/FSH ratio, PRL, and T were significantly higher in the UI group compared with the control group. In contrast, FSH and E2/T ratio were significantly lower in the UI group than in the control group. Furthermore, this study reveals that leptin could be a potential biomarker for UI in Sudanese women and it may be useful for identifying women with a high risk of infertility. Thus, we recommend that the measuring of the leptin test should be introduced and become one of the routine fertility tests, especially for UI cases. Finally, we recommend that further studies be carried out to clarify the exact association between leptin levels and UI in women.
The current knowledge and practices in infertility treatment proved suitable for almost all infertility types and their etiologies, except for unexplained infertility (UI) which is when standard-approved infertility tests have not found a clear cause for the couple’s inability to achieve pregnancy. Adipokines such as leptin were found to have a positive relationship with UI in females and they can be used as reliable predictive biomarkers for UI in women.
Despite the established relationship between leptin and female reproduction, the exact role of leptin in women’s infertility is not clear enough and the reasonable conclusion is that “we need further investigations to fill this diagnostic gap”. Where some studies reported high levels of serum leptin in infertile women, other studies reported increased leptin levels in both fertile and infertile women, thus, high serum leptin levels in these patients were not a contributing factor to infertility.
The objective of this study was to evaluate the serum leptin levels in Sudanese women and to ascertain the relationship between serum leptin levels and UI.
A matched (age and body mass index) case-control study was conducted from March 2021 to February 2022. The study samples were 210 women with UI and 190 fertile women of reproductive age who were attending the maternity hospitals and fertility clinics in Khartoum state Sudan. The serum concentration of leptin and other serum biomarkers were determined using enzyme-linked immunosorbent assays.
The results showed that there was a highly statistically significant difference between the two groups (P < 0.001) for all examined eight biomarkers. Whereby, leptin, luteinizing hormone/follicular stimulating hormone (FSH) ratio, prolactin hormone and testosterone (T) were significantly higher in the UI group compared with the control group, in contrast, FSH and estradiol/T ratio were significantly lower in the UI group than in the control group.
This study reveals that leptin could be a potential biomarker for UI in Sudanese women and it may be useful for identifying women with a high risk of infertility.
Further studies need to be carried out to clarify the exact association between leptin levels and UI in women.
The authors would like to thank the Pan African University of Life and Earth Sciences Institute, the African Union for financial support, and the University of Ibadan for hosting this PhD program. Our appreciation also goes to data collectors and supervisors for their diligence during data collection to obtain necessary information. Our special thanks also go to participants who generously shared their thoughts and feelings despite other commitments. In addition, our thanks go to the federal ministry of health and administrators of all healthcare facilities included in this study for giving us the necessary background information to conduct this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Biochemistry and molecular biology
Country/Territory of origin: Sudan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Merigo F, Italy; Zhou FT, China S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | World Health Organization. Infertility. [cited 12 March 2022]. Available from: https://www.who.int/news-room/fact-sheets/detail/infertility. |
| 2. | Mableson HE, Okello A, Picozzi K, Welburn SC. Neglected zoonotic diseases-the long and winding road to advocacy. PLoS Negl Trop Dis. 2014;8:e2800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Abdullah AA, Ahmed M, Oladokun A. Prevalence of infertility in Sudan: A systematic review and meta-analysis. Qatar Med J. 2021;2021:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (3)] |
| 4. | Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990-2017: results from a global burden of disease study, 2017. Aging (Albany NY). 2019;11:10952-10991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 354] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 5. | Mol BW, Tjon-Kon-Fat R, Kamphuis E, van Wely M. Unexplained infertility: Is it over-diagnosed and over-treated? Best Pract Res Clin Obstet Gynaecol. 2018;53:20-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Kiani Z, Simbar M, Hajian S, Zayeri F, Shahidi M, Saei Ghare Naz M, Ghasemi V. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertil Res Pract. 2020;6:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Abebe MS, Afework M, Abaynew Y. Primary and secondary infertility in Africa: systematic review with meta-analysis. Fertil Res Pract. 2020;6:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (1)] |
| 8. | Abdelazim IA, Purohit P, Farag RH, Zhurabekova G. Unexplained infertility: prevalence, possible causes and treatment options. A review of the literature. J Obstet Gynecol Investigat. 2018;1:17-22. [DOI] [Full Text] |
| 9. | Ray A, Shah A, Gudi A, Homburg R. Unexplained infertility: an update and review of practice. Reprod Biomed Online. 2012;24:591-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 10. | Schattman GL, Esteves S, Agarwal A. Unexplained infertility: Pathophysiology, evaluation treatment. New York: Springer, 2015. |
| 11. | Reverchon M, Ramé C, Bertoldo M, Dupont J. Adipokines and the female reproductive tract. Int J Endocrinol. 2014;2014:232454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Abdullah AA, Ahmed M, Oladokun A. Leptin levels in women with unexplained infertility: A systematic review and meta-analysis. World J Meta-Anal. 2022;10:37-45. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (5)] |
| 13. | Qu T, Yan M, Shen WJ, Li L, Zhu P, Li Z, Huang J, Han T, Hu W, Zhou R, Li P, Xu L, Huang T, Zhong Y, Gu J. Predictive serum markers for unexplained infertility in child-bearing aged women. Am J Reprod Immunol. 2020;83:e13194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | LEP leptin [Homo sapiens (human)]. [cited 13 March 2022]. Available from: https://www.ncbi.nlm.nih.gov/gene/3952. |
| 15. | Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, Hamnvik OP, Koniaris A. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab. 2011;301:E567-E584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 407] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 16. | Khan SM, Hamnvik OP, Brinkoetter M, Mantzoros CS. Leptin as a modulator of neuroendocrine function in humans. Yonsei Med J. 2012;53:671-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Mitchell M, Armstrong DT, Robker RL, Norman RJ. Adipokines: implications for female fertility and obesity. Reproduction. 2005;130:583-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 179] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 18. | Herrid M, Palanisamy SK, Ciller UA, Fan R, Moens P, Smart NA, McFarlane JR. An updated view of leptin on implantation and pregnancy: a review. Physiol Res. 2014;63:543-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Siawrys G, Smolinska N. In vitro effects of luteinizing hormone, progesterone and oestradiol-17β on leptin gene expression and leptin secretion by porcine luteal cells obtained in early pregnancy. J Physiol Pharmacol. 2013;64:513-520. [PubMed] |
| 20. | Maleszka A, Smolinska N, Nitkiewicz A, Kiezun M, Chojnowska K, Dobrzyn K, Szwaczek H, Kaminski T. Adiponectin Expression in the Porcine Ovary during the Oestrous Cycle and Its Effect on Ovarian Steroidogenesis. Int J Endocrinol. 2014;2014:957076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Fornari MC, Sarto A, Berardi VE, Martínez MA, Rocha MG, Pasqualini S, Diez RA. Effect of ovaric hyper-stimulation on blood lymphocyte subpopulations, cytokines, leptin and nitrite among patients with unexplained infertility. Am J Reprod Immunol. 2002;48:394-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Hausman GJ, Barb CR, Lents CA. Leptin and reproductive function. Biochimie. 2012;94:2075-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Avelino-Cruz JE, Flores A, Cebada J, Mellon PL, Felix R, Monjaraz E. Leptin increases L-type Ca2+ channel expression and GnRH-stimulated LH release in LbetaT2 gonadotropes. Mol Cell Endocrinol. 2009;298:57-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Panwar S, Herrid M, Kauter KG, McFarlane JR. Effect of passive immunization against leptin on ovarian follicular development in prepubertal mice. J Reprod Immunol. 2012;96:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Barcz E, Milewski L, Radomski D, Dziunycz P, Kamiński P, Roszkowski PI, Malejczyk J. A relationship between increased peritoneal leptin levels and infertility in endometriosis. Gynecol Endocrinol. 2008;24:526-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Dayer D, Nikbakht R, Kadkhodai Elyaderani M. Comparison of leptin concentrations between infertile women with polycystic ovary syndrome and fertile women. Iran J Reprod Med. 2013;11:1033-1034. [PubMed] |
| 27. | Kucera R, Babuska V, Ulcova-Gallova Z, Kulda V, Topolcan O. Follicular fluid levels of anti-Müllerian hormone, insulin-like growth factor 1 and leptin in women with fertility disorders. Syst Biol Reprod Med. 2018;64:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Wertel I, Gogacz M, Polak G, Jakowicki J, Kotarski J. Leptin is not involved in the pathophysiology of endometriosis-related infertility. Eur J Obstet Gynecol Reprod Biol. 2005;119:206-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Demir B, Guven S, Guven ES, Atamer Y, Gunalp GS, Gul T. Serum leptin level in women with unexplained infertility. J Reprod Immunol. 2007;75:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Kumari P, Jaiswar SP, Shankhwar P, Deo S, Ahmad K, Iqbal B, Mahdi AA. Leptin as a Predictive Marker in Unexplained Infertility in North Indian Population. J Clin Diagn Res. 2017;11:QC28-QC31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Tafvizi F, Masomi M. Comparison of Serum Leptin Level in Women with Unexplained Infertility and Fertile Women in Iran. J Obstet Gynaecol India. 2016;66:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Al-Fartosy AJM, Awad NA, Mahmood RA. A comparative study of leptin, oxidant/antioxidant status and some trace elements in women of healthy control and unexplained infertility in Basrah-Iraq. Indone Biomed J. 2019;11:327-337. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Baig M, Azhar A, Rehman R, Syed H, Tariq S, Gazzaz ZJ. Relationship of Serum Leptin and Reproductive Hormones in Unexplained Infertile and Fertile Females. Cureus. 2019;11:e6524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Kamyabi Z, Gholamalizade T. A Comparative Study of Serum and Follicular Fluid Leptin Concentrations among Explained Infertile, Unexplained Infertile and Fertile Women. Int J Fertil Steril. 2015;9:150-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 35. | Keselman HJ, Othman AR, Wilcox RR. Preliminary testing for normality: Is this a good practice? J Modern Appl Statist Methods. 2013;12:1-19. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Sullivan GM, Feinn R. Using Effect Size-or Why the P Value Is Not Enough. J Grad Med Educ. 2012;4:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2471] [Cited by in RCA: 2845] [Article Influence: 218.8] [Reference Citation Analysis (0)] |
| 37. | Abduljalal MH, Chilmeran SK, Ali Z, Salih SA. Evaluation of serum leptin level, lipid profile and sex hormones in infertile females of unknown cause. Biochem Cell Arch. 2021;21:4473-4477. |
| 38. | Murto T, Bjuresten K, Landgren BM, Stavreus-Evers A. Predictive value of hormonal parameters for live birth in women with unexplained infertility and male infertility. Reprod Biol Endocrinol. 2013;11:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | Grynnerup AG, Lindhard A, Sørensen S. Anti-Müllerian hormone levels in salpingectomized compared with nonsalpingectomized women with tubal factor infertility and women with unexplained infertility. Acta Obstet Gynecol Scand. 2013;92:1297-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 40. | Seckin B, Tokmak A, Yumusak OH. The role of anti-Müllerian hormone in prediction of pregnancy in young and older women with unexplained infertility undergoing intrauterine insemination. J Chin Med Assoc. 2019;82:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 41. | Barbieri RL, Sluss PM, Powers RD, McShane PM, Vitonis A, Ginsburg E, Cramer DC. Association of body mass index, age, and cigarette smoking with serum testosterone levels in cycling women undergoing in vitro fertilization. Fertil Steril. 2005;83:302-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 42. | Olooto WE, Amballi AA, Banjo TA. A review of Female Infertility; important etiological factors and management. J Microbiol Biotech Res. 2017;2:379-385. |
| 43. | Rashid BM, Mahmoud TJ, Nore BF. Hormonal study of primary infertile women. J Zankoy Sulaimani-Part A. 2013;. [DOI] [Full Text] |
| 44. | Masarwi M, Shamir R, Phillip M, Gat-Yablonski G. Leptin stimulates aromatase in the growth plate: limiting catch-up growth efficiency. J Endocrinol. 2018;237:229-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |