Published online Aug 27, 2013. doi: 10.4240/wjgs.v5.i8.245
Revised: July 12, 2013
Accepted: July 17, 2013
Published online: August 27, 2013
Processing time: 94 Days and 14.5 Hours
AIM: To compare the open and laparoscopic Hartmann’s reversal in patients first treated for complicated diverticulitis.
METHODS: Forty-six consecutive patients with diverticular disease were included in this retrospective, single-center study of a prospectively maintained colorectal surgery database. All patients underwent conventional Hartmann’s procedures for acute complicated diverticulitis. Other indications for Hartmann’s procedures were excluded. Patients underwent open (OHR) or laparoscopic Hartmann’s reversal (LHR) between 2000 and 2010, and received the same pre- and post-operative protocols of cares. Operative variables, length of stay, short- (at 1 mo) and long-term (at 1 and 3 years) post-operative complications, and surgery-related costs were compared between groups.
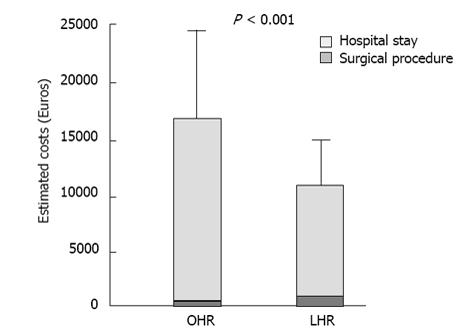
RESULTS: The OHR group consisted of 18 patients (13 males, mean age ± SD, 61.4 ± 12.8 years), and the LHR group comprised 28 patients (16 males, mean age 54.9 ± 14.4 years). The mean operative time and the estimated blood loss were higher in the OHR group (235.8 ± 43.6 min vs 171.1 ± 27.4 min; and 301.1 ± 54.6 mL vs 225 ± 38.6 mL respectively, P = 0.001). Bowel function returned in an average of 4.3 ± 1.7 d in the OHR group, and 3 ± 1.3 d in the LHR group (P = 0.01). The length of hospital stay was significantly longer in the OHR group (11.2 ± 5.3 d vs 6.7 ± 1.9 d, P < 0.001). The 1 mo complication rate was 33.3% in the OHR (6 wound infections) and 3.6% in the LHR group (1 hemorrhage) (P = 0.004). At 12 mo, the complication rate remained significantly higher in the OHR group (27.8% vs 10.7%, P = 0.03). The anastomotic leak and mortality rates were nil. At 3 years, no patient required re-intervention for surgical complications. The OHR procedure had significantly higher costs (+56%) compared to the LHR procedure, when combining the surgery-related costs and the length of hospital stay.
CONCLUSION: LHR appears to be a safe and feasible procedure that is associated with reduced hospitality stays, complication rates, and costs compared to OHR.
Core tip: The present study examined the intra-operative and post-operative clinical outcomes of open vs laparoscopic Hartmann’s reversal in patients first treated for diverticulitis, one of the most common gastrointestinal diseases. By selecting a homogeneous sample of patients, we are able to describe the advantages of laparoscopy in this specific population. The laparoscopic reversal of Hartmann’s procedure appeared to be safe and feasible, with advantages in reduced hospitality stays, complication rates, and heath-related costs compared to the open approach.
- Citation: de’Angelis N, Brunetti F, Memeo R, Batista da Costa J, Schneck AS, Carra MC, Azoulay D. Comparison between open and laparoscopic reversal of Hartmann’s procedure for diverticulitis. World J Gastrointest Surg 2013; 5(8): 245-251
- URL: https://www.wjgnet.com/1948-9366/full/v5/i8/245.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i8.245
Diverticular disease is common in developed countries. The prevalence is largely age-dependent; it is uncommon (approximately 5%) in patients younger than 40 years and drastically increases to 65% in patients aged 65 years and up to 80% in those aged 80 years and older[1-3]. Differences are observed among countries, with a higher prevalence in the United States than in Europe and a low prevalence in African nations[4,5].
Diverticular disease occurs as a result of herniation of the mucosa and submucosa through the muscular layer of the colonic wall. Diverticulosis refers to the presence of one or more diverticula, and the disease has a clinical spectrum from asymptomatic to symptomatic disease with potentially lethal complications. Particularly, diverticulitis, which can affect 20%-30% of individuals with diverticulosis, is one of the most common causes of hospitalization related to gastrointestinal disease[6]. Approximately 15% of patients who have had at least 1 episode of complicated diverticulitis could benefit from surgical management[7].
Currently, in cases of complicated diverticulitis associated with perforation and subsequent purulent or fecal abdominal contamination (i.e., Hinchey classification III or IV), 2-stage surgical management is widely performed[8]. This approach comprises a segmental resection of the involved colon and a diverting proximal stoma (Hartmann’s Procedure, HP)[9], and, subsequently, a colostomy reversal and restoration of bowel continuity in a second operation[6,10]. HP, as the first step of such 2-stage interventions, is the most commonly performed surgery in the emergency setting for perforated sigmoid diverticulitis[9].
HP was described for the first time in 1921[11] for the resection of left-sided colonic carcinoma. The omission of a primary intestinal anastomosis was intended to reduce the morbidity and mortality related to anastomotic dehiscence. It remains unclear whether Hartmann originally intended the colostomy to be reversible. Currently, reestablishing continuity after HP (i.e., Hartmann’s reversal, HR) is usually performed after 3-6 mo, to allow a complete resolution of the pelvic inflammation. HR remains a technically challenging operation that can be performed in only 1/3 of cases[7,12]. HR is associated with a serious risk of surgical morbidity (up to 60% of cases), including a high rate of anastomotic leakage (up to 16%), and a considerable mortality risk (range, 4% to 10%)[7,12-14].
The published results on HR are difficult to interpret because they are based on heterogeneous pathologies (e.g., diverticulitis, sigmoid volvulus, and carcinomas) among different patient groups. Moreover, with the introduction of the circular stapling devices and the development of modern laparoscopic techniques, the restorative procedure has achieved important improvements in patient outcomes, with shorter hospital stays and reduced anastomotic leakage. Since the first use of laparoscopy for HR in 1993[15], the few studies that have examined the role of laparoscopy in performing HR have been primarily small case series, multicenter studies, or retrospective analyses of heterogeneous samples of patients[16-21].
The present study aimed to examine the intra-operative and post-operative clinical outcomes of laparoscopic HR (LHR) compared to open HR (OHR) in patients first treated for complicated diverticulitis.
This is a retrospective, single-center study on a prospectively maintained colorectal surgery database. Data on patients with complicated diverticulitis who underwent conventional HP in the General Surgery Unit of the Henri-Mondor Hospital, Créteil, France, were identified and retrieved after obtaining approval from the Henri-Mondor Hospital Institutional Review Board. The OHR procedures were performed between January 2000 and January 2005, whereas the LHR procedures were performed between January 2005 and January 2010. This temporal disparity occurred because of the hospital unit tended to perform, from 2005 on, HR surgeries using a laparoscopic approach. In total, the study sample includes 46 consecutive patients who underwent OHR (n = 18) or LHR (n = 28) between 2000 and 2010. All patients underwent HP for diverticulitis, as confirmed by histopathological examinations of the surgical specimens. Only Hinchey scores III and IV were included in the analysis. Other indications for HP (e.g., carcinoma, trauma, and ischemia) were excluded from this analysis.
In the pre-operative assessment, both groups underwent an anatomical evaluation (e.g., barium enema or endoscopy) of the remaining proximal colon and rectal stump. All patients underwent bowel preparation (including enemata to empty the rectal stump) approximately 24 h before surgery. They all received perioperative broad-spectrum parenteral antibiotics and subcutaneous low-molecular-weight heparin.
After inducing general anesthesia, the OHR was performed through an abdominal midline vertical incision. The dissection of the peritoneal attachments and rectal stump was achieved using monopolar and/or bipolar electrosurgery devices. Colorectal anastomosis was performed mechanically without stoma protection. In the LHR surgeries, the patients were placed in a modified lithotomy position with the lower limbs slightly flexed on stirrups. A 3-5 trocars technique was used, depending on the level of operative difficulty encountered. The first surgical step was always the excision of the colostomy and the mobilization of the bowel out of the abdomen. Then, the stapler anvil was introduced into the proximal colon by purse string suturing, as previously described[22]. The bowel was returned to the abdominal cavity after having dissected any existing adhesions. Adhesiolysis was achieved with the Harmonic Scalpel (Ultracision®, Ethicon Endo-Surgery, Johnson and Johnson, United States). Colorectal anastomosis was performed mechanically without stoma diversion. In both surgical procedures, the rectal mobilization was systematically performed to ensure the feasibility of the end-to-end anastomosis and to avoid bladder injury. In all cases, the colostomy wall defect was closed using 3 layers of interrupted non-absorbable sutures.
The OHR procedures were performed by 2 experienced general surgeons, 1 (Brunetti F) of whom performed all LHR surgeries.
The OHR and the LHR groups were compared for demographic, operative, and post-operative variables. The main outcomes were the short-term (i.e., 30 d) and long-term (i.e., at 1 year and 3 years) complication rates (including mortality and morbidity). Additionally, the mean invoiced costs per OHR and LHR patient (including surgical materials and hospitality stay) for the French Public Health System (Assistance Publique Hopitaux de Paris) were calculated.
Statistical analysis was performed with SPSS (IBM, SPSS Statistics, Version 20 for Macintosh, Chicago, Illinois, United States). The groups were compared using the Chi-squared or Fisher’s Exact Test for the categorical variables and the T-test for the continuous variables. The following variables were analyzed: age, gender, presence and type of comorbidity, ASA score, Hinchey score, number of episodes of diverticulitis before HP, time between HP and its reversal, extent of colon mobilization, operation time, estimated blood loss, time to flatus, time to resumption of diet, hospital stay, and complication rates. A P value < 0.05 was considered significant.
The demographic characteristics of the OHR and LHR patients are shown in Table 1. The two groups showed no differences in terms of the mean age, gender distribution, body mass index, ASA scores, presence of comorbidities, Hinchey scores, number of episodes of diverticulitis before HP, and d between HP and its reversal. Averaged between both groups, the HR was performed 134.8 ± 63.3 d after the primary resection.
| OHR(n = 18) | LHR(n = 28) | P value | |
| Age (yr) | 61.4 ± 12.8 | 54.9 ± 15.4 | 0.1 |
| Male/female ratio | 5/13 | 12/16 | 0.3 |
| Body masse index (kg/m2) | 24.8 ± 2.9 | 24.1 ± 3.1 | 0.4 |
| ASA score | 0.06 | ||
| I | 4 (22.2) | 16 (57.1) | |
| II | 12 (66.7) | 10 (35.7) | |
| III | 2 (11.1) | 2 (7.1) | |
| Comorbidity | 10 (55.6) | 10 (35.7) | 0.2 |
| Diabetes | 2 (11.1) | 3 (10.7) | |
| Cardiovascular disease | 9 (50) | 9 (32.1) | |
| Pulmonary disease | 4 (22.2) | 2 (7.1) | |
| Hinchey Score at HP | 0.5 | ||
| III | 14 (77.7) | 20 (71.4) | |
| IV | 4 (22.3) | 8 (28.6) | |
| Episodes of acute diverticulitis | 0.2 | ||
| before HP | |||
| None | 13 (72.2) | 16 (57.1) | |
| One | 5 (27.8) | 8 (28.6) | |
| Two or more | 0 (0) | 4 (14.3) | |
| Mean time from HP to reversal (d) | 143.7 ± 64.8 | 129.1 ± 62.8 | 0.4 |
In both groups, all anastomoses were mechanical supra-peritoneal end-to-end anastomoses without stoma diversion. In the majority of the cases, a splenic flexure mobilization was performed to ensure a free-tension anastomosis. The n° 29 stapler was most frequently used in both procedures. No conversion to open surgery occurred in the LHR group. The mean operative time and the amount of estimated blood loss were significantly superior in the OHR compared to the LHR group (Table 2).
| OHR (n = 18) | LHR (n = 28) | P value | |
| Extent of mobilization | 0.5 | ||
| Splenic flexure | 16 (88.9) | 27 (96.4) | |
| Transverse | 2 (11.1) | 1 (3.6) | |
| Stapled end-to-end anastomosis N° (mm) | 0.07 | ||
| N° 28 | 0 (0) | 2 (7.1) | |
| N° 29 | 18 (100) | 21 (75) | |
| N° 31 | 0 (0) | 5 (17.9) | |
| Operation time (min) | 235.8 ± 43.6 | 171.1 ± 27.4 | 0.001 |
| Estimated blood loss (mL) | 301.1 ± 54.6 | 225 ± 38.6 | 0.001 |
Concerning the post-operative variables, the LHR group showed a significantly lower time to flatus, time to resumption to regular diet, and hospital stay (Table 3). The short-term complication rate (1 mo) was also lower in the LHR group compared to the OHR group. No anastomotic leaks occurred. All observed complications were medically managed, except for 1 case of hemorrhage of the inferior epigastric vessel, which required hemostatic laparoscopic surgery, at postoperative day 1 in the LHR group. Regardless of the surgical procedure, the early post-operative complication rate was 15.2%, including mainly wound infections and one case of hemorrhage. Patients with and without complications had similar demographic and operative characteristics. The only variable that was significantly associated with post-operative complications was the length of hospital stay
| OHR (n = 18) | LHR (n = 28) | P value | |
| Time to Flatus (d) | 4.3 ± 1.7 | 3 ± 1.3 | 0.006 |
| Time to Resumption to regular diet (d) | 5.5 ± 1.7 | 3.9 ± 1.2 | 0.001 |
| Length of hospital stay (d) | 11.2 ± 5.1 | 6.7 ± 1.9 | <0.001 |
| 1 mo complication rate | 6 (33.3) | 1 (3.6) | 0.004 |
| Wound infection | 6 (33.3) | 0 | |
| Hemorrhage | 0 | 1 (3.6) | |
| 12 mo complication rate | 5 (27.8) | 3 (10.7) | 0.03 |
| Midline incisional hernia | 4 (22.2) | 0 | |
| Incisional hernia of the previous colostomy | 1 (5.6) | 3 (10.7) |
(P < 0.001).
At 12 mo, the complication rate remained significantly higher in the OHR group (Table 3), including midline incisional hernias and incisional hernia of the previous colostomy, which were electively surgically managed. The overall mortality rate was nil. At 3 years, no patient required re-intervention for surgical complications.
The OHR procedure had significantly higher costs (average +56%) compared to the LHR procedure, when combining the surgery-related costs and the length of hospital stay (Figure 1).
The present study described the clinical outcomes of two surgical approaches (i.e., open vs laparoscopic) to perform HR in a homogeneous sample of patients first treated for complicated diverticulitis (Hinchey scores III or IV). In accordance with the previous literature, our study demonstrated that LHR is safe and feasible, with reduced operative time and more rapid post-operative recovery.
HP, originally described for distal colon cancer complicated with bowel obstruction, has evolved over the years, finding its current main indication in benign pathologies, such as diverticulitis[11,23]. This finding may be particularly true in developed regions, such as North American and Europe, in which the introduction of widespread screening programs for colorectal cancers and advanced endoscopic techniques, such as the placement of endoluminal stents, has relegated the HP primarily to emergency interventions for inflammatory diseases or iatrogenic perforations[24-26]. However, HP remains a rarely performed procedure because of its infrequent indication and the availability of other treatment options, such as antibiotic therapies, laparoscopic lavage, and drainage, or primary resection with immediate anastomosis[17,27,28]. Moreover, HR is not possible in all patients, with reversal rates ranging between 21% and 85% of patients[12,19,25].
For this reason, the current literature on HP and HR is characterized by studies of samples that include all possible indications, thus grouping together patients with diverticulitis, inflammatory bowel diseases, cancers, or trauma. However, this grouping may bias the interpretation of results and influence the risk of underestimating or overestimating the clinical outcomes of HR, with either the open or laparoscopic approach, in relation to specific pathologies.
A recent review showed that LHR offers several advantages over OHR, including more rapid post-operative recovery, less post-operative pain, earlier restoration of bowel function, more rapid return to normal diet, and reduced morbidity[23]. However, the reduced surgical invasivity and the clinical advantages of the laparoscopic approach does not seem to have increased the number of patients candidate to undergo HR, which might have been expected.
In contrast with previous studies[17-21,29], we analyzed a homogeneous sample of consecutive patients diagnosed with diverticulitis who underwent surgery in the same hospital unit with the same laparoscopic technique, to report the data related to a specific subset of patients representing those most often seen in clinical practice.
In our study, the majority of patients (58.7%) with diverticular disease underwent HP at the first episode of acute diverticulitis, in accordance with the disease evolution, which can present with perforation at the first attack[8]. On average, the OHR and LHR were performed 4.5 mo from the HP, which is less than the 7.5 mo reported in other published studies[23]. Moreover, in contrast with other reports[17], the time interval between HP and its reversal did not influence the overall morbidity or complication rates in either the OHR or the LHR group in our study. The reduced time interval between HP and its reversal was justified by the overall optimal status of the patients (e.g., nutritional status), which is also related to the underlying benign pathology and is supported by the low incidence of impossible adhesiolysis (i.e., no conversion was needed), although all patients were classified with a Hinchey score III or IV.
The operative time was significantly lower when the HR was performed laparoscopically, as was expected[17,23]. In the literature, many different laparoscopic procedures are described[19,25,30]. The technique used in the present study, starting with the mobilization of the stoma and the primary preparation of the afferent loop before the placement of the trocars, may contribute to the time saving[22]. Although the ideal laparoscopic technique and the advantages of one over the others is still a matter of debate, it remains an important risk factor for post-operative morbidity[31,32]. In our study, we had no mortality and no anastomotic leaks, in contrast with previous literature[7,13,14,22]. In all interventions, whether OHR or LHR, a tension-free anastomosis was systematically obtained, frequently by the complete mobilization of the splenic flexure, and this process may have favored the anastomotic healing, although there is controversial literature on this topic[19,21,32].
The LHR was associated with a shorter recovery time and a lower incidence of post-operative complications. In particular, the LHR, characterized by minimal invasiveness and surgical trauma, was associated with a reduced time to flatus and resumption of normal diet, which surely contributed to the shortened hospital stays. However, note that we had no intra-operative complications in either group and no conversions from the laparoscopic to the open technique. This finding may be related to the experience of the surgeon operating in a high volume surgical center, which may play an important role regarding this technically challenging intervention[33]. The early complications observed were abdominal wound infections in the OHR group and one case of hemorrhage in the LHR group, with an overall complication rate of 15.2%. The delayed post-operative complications (at 1 year) included midline incisional hernias and incisional hernia of the previous colostomy, for an overall incidence of 17.4%. No further surgical complications were observed within 3 years of follow-up. The complication rates in our studies are within the ranges reported in other recent case series[16,17,22].
In addition to the clear clinical advantages of LHR for the patients, a more rapid recovery time has a great influence on the overall costs of the surgery and hospitalization. Indeed, LHR may have a higher intra-operative cost for surgical materials; however, this cost is overbalanced by lower expenses in the post-operative period because of reduced hospital stays and incidences of complications. This aspect cannot be underestimated because it influences healthcare system policy makers. Moreover, as the population ages, diverticular disease appears to be increasing, thereby representing a significant risk to health with subsequent indications for healthcare expenditures in the elderly population. In the French healthcare system, the major determinant of cost is the length of hospital stay, which is estimated at 1500 euros/d per patient in our department. Thus, although the differences among healthcare systems across European countries and the lack of updated data preclude a precise estimate of diverticulitis-related healthcare costs, a considerable financial burden is expected[2].
The main limitations of this study are the non-randomized study design and the small sample size. However, a single-center randomized controlled trial with an adequate sample size comparing OHR vs LHR appears to be unfeasible because this procedure represents less than 1% of laparoscopically performed colorectal surgeries in a high volume surgical center[17]. This limitation may be counterbalanced by the fact that in the present single center study, we compared OHR to LHR in a homogenous patient sample, with the same indication for HP (i.e., complicated diverticulitis).
In conclusion, in accordance with the previous literature, LHR appears to be a safe and feasible procedure for patients first treated for complicated diverticulitis and offers the advantages of reduced length of hospital stays, lower complication rates, and reduced costs compared to OHR. Although the available evidence supporting the superiority of LHR is mainly based on non-randomized small studies, the laparoscopic approach may now be considered the gold standard technique for HR in high volume colorectal surgical centers.
This study is the subject of a poster presentation at the 21st International Congress of the EAES (European Association for Endoscopic Surgery), Vienna, Austria (June 19-22, 2013)
In cases of diverticulitis Hinchey classification III or IV, the Hartmann’s procedure is the most frequently performed. The reversal of Hartmann’s procedure is associated with high risks of surgical morbidity and mortality, and only a third of the patients can beneficiate of it.
Laparoscopic Hartmann’s reversal is investigated as the surgical technique to achieve better surgical and clinical outcomes.
Most of the previously published studies have examined the laparoscopic Hartmann’s reversal in heterogeneous sample of patients operated for various indications. This may bias the interpretation of the clinical results in relation to the specific pathology. The study assessed the advantages of laparoscopy over open approach in patients with diverticular disease only.
The results of the study provide relevant evidence for the application of laparoscopy for Hartmann’s reversal, in order to have lower morbidity, shorter hospital stay, and reduced costs for the Healthcare System.
The Hartmann’s procedure is the surgical resection of the rectosigmoid colon with closure of the rectal stump and formation of an end colostomy. The Hartmann’s reversal is the restoration of bowel continuity by the closure of the colostomy.
This retrospective cohort study compares the open to laparoscopic reversal of Hartmann’s procedure in a homogenous population with complicated diverticulitis. It is the first to isolate diverticulitis as indication. The results are very interesting and in accordance with previous results, underlining the minimal invasiveness of laparoscopic surgery and the same (or better) security profile.
P- Reviewers Faria GR, Ribas Y, Shabanzadeh DM S- Editor Wen LL L- Editor A E- Editor Lu YJ
| 1. | Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterol. 1975;4:53-69. [PubMed] |
| 2. | Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther. 2003;18 Suppl 3:71-74. [PubMed] |
| 3. | Munson KD, Hensien MA, Jacob LN, Robinson AM, Liston WA. Diverticulitis. A comprehensive follow-up. Dis Colon Rectum. 1996;39:318-322. [PubMed] |
| 4. | Delvaux M, Demoustier-Champagne S. Immobilisation of glucose oxidase within metallic nanotubes arrays for application to enzyme biosensors. Biosens Bioelectron. 2003;18:943-951. [PubMed] |
| 5. | Wong WD, Wexner SD, Lowry A, Vernava A, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G. Practice parameters for the treatment of sigmoid diverticulitis--supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290-297. [PubMed] |
| 6. | Salem L, Flum DR. Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum. 2004;47:1953-1964. [PubMed] |
| 7. | Wigmore SJ, Duthie GS, Young IE, Spalding EM, Rainey JB. Restoration of intestinal continuity following Hartmann’s procedure: the Lothian experience 1987-1992. Br J Surg. 1995;82:27-30. [PubMed] |
| 8. | Klarenbeek BR, Samuels M, van der Wal MA, van der Peet DL, Meijerink WJ, Cuesta MA. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Zeitoun G, Laurent A, Rouffet F, Hay J, Fingerhut A, Paquet J, Peillon C, Research TF. Multicentre, randomized clinical trial of primary versus secondary sigmoid resection in generalized peritonitis complicating sigmoid diverticulitis. Br J Surg. 2000;87:1366-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 119] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Hartmann H. New procedure for the removal of cancers of the terminal part of the pelvic colon. Paris: Secretariat of the Association 1921; 411-413. |
| 12. | Pearce NW, Scott SD, Karran SJ. Timing and method of reversal of Hartmann’s procedure. Br J Surg. 1992;79:839-841. [PubMed] |
| 13. | Vermeulen J, Coene PP, Van Hout NM, van der Harst E, Gosselink MP, Mannaerts GH, Weidema WF, Lange JF. Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Colorectal Dis. 2009;11:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Bell C, Asolati M, Hamilton E, Fleming J, Nwariaku F, Sarosi G, Anthony T. A comparison of complications associated with colostomy reversal versus ileostomy reversal. Am J Surg. 2005;190:717-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Gorey TF, O’Connell PR, Waldron D, Cronin K, Kerin M, Fitzpatrick JM. Laparoscopically assisted reversal of Hartmann’s procedure. Br J Surg. 1993;80:109. [PubMed] |
| 16. | Faure JP, Doucet C, Essique D, Badra Y, Carretier M, Richer JP, Scépi M. Comparison of conventional and laparoscopic Hartmann’s procedure reversal. Surg Laparosc Endosc Percutan Tech. 2007;17:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Haughn C, Ju B, Uchal M, Arnaud JP, Reed JF, Bergamaschi R. Complication rates after Hartmann’s reversal: open vs. laparoscopic approach. Dis Colon Rectum. 2008;51:1232-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Huynh H, Trottier DC, Soto CM, Moloo H, Poulin EC, Mamazza J, Boushey RP. Laparoscopic colostomy reversal after a Hartmann procedure: a prospective series, literature review and an argument against laparotomy as the primary approach. Can J Surg. 2011;54:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Leroy J, Costantino F, Cahill RA, D’Agostino J, Wu WH, Mutter D, Marescaux J. Technical aspects and outcome of a standardized full laparoscopic approach to the reversal of Hartmann’s procedure in a teaching centre. Colorectal Dis. 2011;13:1058-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Petersen M, Köckerling F, Lippert H, Scheidbach H. Laparoscopically assisted reversal of Hartmann procedure. Surg Laparosc Endosc Percutan Tech. 2009;19:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Rosen MJ, Cobb WS, Kercher KW, Sing RF, Heniford BT. Laparoscopic restoration of intestinal continuity after Hartmann’s procedure. Am J Surg. 2005;189:670-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Carus T, Bollmann S, Lienhard H. Laparoscopic reversal of Hartmann’s procedure: technique and results. Surg Laparosc Endosc Percutan Tech. 2008;18:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | van de Wall BJ, Draaisma WA, Schouten ES, Broeders IA, Consten EC. Conventional and laparoscopic reversal of the Hartmann procedure: a review of literature. J Gastrointest Surg. 2010;14:743-752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 24. | Desai DC, Brennan EJ, Reilly JF, Smink RD. The utility of the Hartmann procedure. Am J Surg. 1998;175:152-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 77] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Dumont F, Vibert E, Duval H, Manaouil D, Sredic A, Alfahel N, Mauvais F, De Fresnoy H, Rudant J, Katsahian S. [Morbi-mortality after Hartmann procedure for peritonitis complicating sigmoid diverticulitis. A retrospective analysis of 85 cases]. Ann Chir. 2005;130:391-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Vemulapalli R, Lara LF, Sreenarasimhaiah J, Harford WV, Siddiqui AA. A comparison of palliative stenting or emergent surgery for obstructing incurable colon cancer. Dig Dis Sci. 2010;55:1732-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 27. | Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha S, Remzi FH, Fazio VW, Aydin N, Darzi A, Senapati A. Primary resection with anastomosis vs. Hartmann’s procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Dis Colon Rectum. 2006;49:966-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 158] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 28. | Liang S, Russek K, Franklin ME. Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: laparoscopic lavage and drainage vs. laparoscopic Hartmann‘s procedure. Surg Endosc. 2012;26:2835-2842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 29. | Khaikin M, Zmora O, Rosin D, Bar-Zakai B, Goldes Y, Shabtai M, Ayalon A, Munz Y. Laparoscopically assisted reversal of Hartmann’s procedure. Surg Endosc. 2006;20:1883-1886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Regadas FS, Siebra JA, Rodrigues LV, Nicodemo AM, Reis Neto JA. Laparoscopically assisted colorectal anastomose post-Hartmann’s procedure. Surg Laparosc Endosc. 1996;6:1-4. [PubMed] |
| 31. | Vermeulen J, Vrijland W, Mannaerts GH. Reversal of Hartmann’s procedure through the stomal side: a new even more minimal invasive technique. Surg Endosc. 2008;22:2319-2322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Holland JC, Winter DC, Richardson D. Laparoscopically assisted reversal of Hartmann’s procedure revisited. Surg Laparosc Endosc Percutan Tech. 2002;12:291-294. [PubMed] |
| 33. | Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008;143:762-767; discussion 768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 254] [Article Influence: 14.9] [Reference Citation Analysis (0)] |