Published online Sep 27, 2023. doi: 10.4240/wjgs.v15.i9.1941
Peer-review started: May 19, 2023
First decision: June 1, 2023
Revised: June 21, 2023
Accepted: July 18, 2023
Article in press: July 18, 2023
Published online: September 27, 2023
Processing time: 126 Days and 3.6 Hours
Mortality rates after pancreaticoduodenectomy (PD) have significantly decreased in specialized centers. However, postoperative morbidity, particularly delayed gastric emptying (DGE), remains the most frequent complication following PD.
To identify risk factors associated with DGE after the PD procedure.
In this retrospective, cross-sectional study, clinical data were collected from 114 patients who underwent PD between January 2015 and June 2018. Demographic factors, pre- and perioperative characteristics, and surgical complications were assessed. Univariate and multivariate analyses were performed to identify risk factors for post-PD DGE.
The study included 66 males (57.9%) and 48 females (42.1%), aged 33-83 years (mean: 62.5), with a male-to-female ratio of approximately 1.4:1. There were 63 cases (55.3%) of PD and 51 cases (44.7%) of pylorus-preserving pancreatoduodenectomy. Among the 114 patients who underwent PD, 33 (28.9%) developed postoperative DGE. Univariate analysis revealed significant differences in four of the 14 clinical indexes observed: pylorus preservation, retrocolonic anastomosis, postoperative abdominal complications, and early postoperative albumin (ALB). Logistic regression analysis further identified postoperative abdominal complications [odds ratio (OR) = 4.768, P = 0.002], preoperative systemic diseases (OR = 2.516, P = 0.049), and early postoperative ALB (OR = 1.195, P = 0.003) as significant risk factors.
Postoperative severe abdominal complications, preoperative systemic diseases, and early postoperative ALB are identified as risk factors for post-PD DGE.
Core Tip: This study enrolled 114 patients with pancreaticoduodenectomy (PD) over a recent 5-year period at a single center with a short time span and detailed and reliable data. To investigate the risk factors for delayed gastric emptying after PD. We have draw the conclusion that postoperative severe abdominal complications, preoperative systemic diseases and early postoperative albumin are risk factors for post-PD delayed gastric emptying.
- Citation: Xie FL, Ren LJ, Xu WD, Xu TL, Ge XQ, Li W, Ge XM, Zhou WK, Li K, Zhang YH, Wang Z. Preoperative and postoperative complications as risk factors for delayed gastric emptying following pancreaticoduodenectomy: A single-center retrospective study. World J Gastrointest Surg 2023; 15(9): 1941-1949
- URL: https://www.wjgnet.com/1948-9366/full/v15/i9/1941.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i9.1941
Pancreaticoduodenectomy (PD) is a commonly performed surgical procedure for treating tumors in the head of the pancreas, the lower part of the common bile duct, and the ampullary region of the duodenum. It involves the resection of the pancreatic head, lower portion of the common bile duct, gallbladder, distal stomach, duodenum, and part of the jejunum[1]. With medico-technological advancements, PD has become a standardized surgical approach for treating pancreatic head cancer and periampullary benign and malignant tumors[2], decreasing serious postoperative complications such as severe pancreatic leakage, bile leakage, and massive hemorrhage[3]. However, the underlying mechanism of delayed gastric emptying (DGE), one of its complications, remains unknown, presenting a challenge for clinicians in its treatment[4]. Despite advancements in surgical techniques and perioperative management, which have reduced the occurrence of severe postoperative complications such as severe pancreatic leakage, bile leakage, and massive hemorrhage, some complications, particularly DGE, continue to be prevalent among those who underwent PD, with no known cause or effective treatment[5].
DGE is a syndrome characterized by a gastric motility disorder and gastric emptying disturbances, primarily caused by non-mechanical obstruction factors resulting from abdominal surgery[6]. The cause of DGE has remained unknown, resulting in poor treatment outcomes and prolonged hospital stays, posing challenges for clinicians. Evidence indicates that DGE is a functional gastric emptying disorder without organic lesions[7]. The incidence of DGE has been consistently high for many decades, with a study conducted by the International Study Group of Pancreatic Surgery (ISGPS) in 2007 reporting an incidence ranging from 19% to 57% following pancreatic surgery[5]. A recent foreign research review discovered that the incidence of DGE ranges from 3.2% to 59%, with 3234 (27.7%) out of 11669 patients experiencing post-PD DGE[8]. In recent years, numerous pancreas centers worldwide have conducted extensive studies and discussions on the factors inducing DGE after PD[9]; however, a definite and convincing conclusion is yet to be reached. Determining whether the cause lies in surgical techniques, perioperative management issues, or other factors is crucial in guiding treatment decisions.
Regarding treatment, the specific pathogenesis of DGE remains uncharacterized[5] without an established treatment plan for DGE, resulting in undesirable effects with various treatment approaches. Consequently, comprehensive measures have been generically adopted. For patients with postoperative DGE, the routine treatment plan of our team is to correct hypoproteinemia (HP) and electrolyte imbalances, maintain stable blood sugar levels, and utilize methods such as intramuscular metoclopramide, acupuncture, gastroscope-guided jejunal nutrition tube placement, and occasional intravenous erythromycin infusions[10-12]. However, past treatment attempts using these approaches have failed to improve gastric motility significantly or indicate the exact timing at which gastric function recovers in patients.
Therefore, this study aims to thoroughly investigate the risk factors associated with DGE and introduce a novel treatment approach, as detailed below.
The clinical data of 114 patients who underwent PD between January 2015 and June 2018 at The First People's Hospital of Lianyungang were collected. Inclusion criteria: (1) Patients who underwent PD; (2) Patients who met the diagnostic criteria for DGE following PD; (3) Patients without cerebrovascular diseases who could tolerate surgery; (4) Patients with no history of abdominal surgery; and (5) Patients with complete clinical data. Exclusion criteria: (1) Patients with incomplete clinical data; (2) Patients with pre-existing gastrointestinal obstructive diseases; (3) Patients with Grade A DGE; (4) Patients with postoperative pulmonary infection; and (5) Patients undergoing re-operation due to postoperative complications.
All the included patients underwent either PD or pylorus-preserving pancreatoduodenectomy (PPPD) under general anesthesia. The tumor was resected through a median abdominal incision, and lymph nodes were dissected from the pancreatic head, the lower part of the common bile duct, the gallbladder, the upper jejunum, the duodenum, and portions of the distal stomach. All digestive tract reconstructions were performed using the Child procedure. Anastomosis was performed as follows: Firstly, pancreaticojejunostomy was performed using a modified pancreatic duct-jejunal mucosa-to-mucosa one-layer anastomosis or pancreas-jejunal invagination anastomosis; secondly, the gastrointestinal anastomosis was performed by a full-thickness continuous absorbable suture with absorbable threads; finally, end-to-side gastrojejunostomy (for PD) or duodenal-jejunal end-to-side anastomosis (for PPPD) was adopted for gastrointestinal anastomosis. The gastrointestinal anastomosis stoma was located either in the anterior or posterior colon. The stomach and some jejunal feeding tubes were routinely placed during the operation, and two abdominal drainage tubes were inserted postoperatively.
The current diagnosis of DGE after pancreatic surgery follows the requirements recommended by the ISGPS in 2007. Gastroparesis (GP) can be diagnosed if the following conditions are met: (1) Continuous gastrointestinal decompression with a daily drainage volume of > 500 mL for > 3 d after pancreatic surgery; (2) Inability to consume solid food within 7 days after the operation; (3) Vomiting or bloating; and (4) Requirement for gastrointestinal excitomotors. When considering these symptoms, it is essential to rule out mechanical obstruction of the gastrointestinal outflow tract. ISGPS classifies DGE after pancreatic surgery into grades A, B, and C based on the severity. Grade A refers to the retention of the gastric tube for 4-7 d after the operation or the inability to consume solid food on the 7th postoperative day; grade B refers to the retention of gastric tubes for 8-14 d after the operation, or the inability to consume a solid diet on the 14th postoperative day; grade C corresponds to the postoperative gastric tube retention for > 14 d, significantly impacting patient recovery, or the inability to consume a solid diet even after 21 postoperative days. Patients with grades B and C, which have a significant impact on postoperative recovery, were included in the study[5].
According to the Consensus on the Diagnosis, Treatment, and Prevention of Common Complications in Pancreatic Surgery (2017)[13], formulated by the Pancreatic Surgery Group of the Chinese Medical Association, postoperative complications such as pancreatic fistula, biliary fistula, postoperative bleeding, and chylous fistula were assessed. A pancreatic fistula is an abnormal channel between the pancreatic ductal epithelium and other epithelial surfaces, resulting in the flow of enzyme-rich fluid from the pancreas. The diagnostic criteria for pancreatic fistula are as follows: The amylase concentration in the drainage fluid, measured at least 3 d after the operation, exceeds three times the upper limit of the normal serum amylase concentration, alongside corresponding clinical manifestations. A biliary fistula is an abnormal passage through which bile flows out of the biliary system into the abdominal cavity or outside the body through a breach (or the cholangio-jejunal anastomotic stoma) of the biliary system. Postoperative bleeding is defined as bleeding that occurs after pancreatic surgery, typically indicated by bloody fluid in the abdominal drainage or gastrointestinal decompression tube or hematochezia. Simultaneous changes in vital signs, such as the heart rate and decreased hemoglobin (Hb) concentration, were observed. Chylous fistula is diagnosed when chylous fluid is drained from a drainage tube, orifice, or wound at ≥ 3 d after the operation, regardless of the amount of drainage, provided the concentration of triglycerides is > 1100 mg/L. Intra-abdominal infection is defined by symptoms such as chills, high fever, abdominal distension, and intestinal paralysis, occurring 3 d after the operation and persisting for > 24 h. Laboratory tests showing significantly elevated white blood cell count, with or without HP and anemia, and imaging evidence of intra-abdominal fluid accumulation contribute to the diagnosis of intra-abdominal infection. The diagnosis can be confirmed if the puncture extract is purulent or if bacteria are detected.
Postoperative indicators were considered primary outcome measures, while general information and surgical factors were secondary.
General information: Gender, age, preoperative systemic diseases, preoperative nutritional status.
Surgical factors: Pylorus preservation status, lymph node dissection, operation time (min), intraoperative blood loss (mL).
Postoperative indicators: Pancreatic fistula, abdominal complications, early enteral nutrition treatment (within 4 d), and Hb and albumin (ALB) levels on postoperative days 1, 4, and 7.
All data were statistically analyzed using SPSS 23.0. Enumeration data were expressed as proportions and compared using the Chi-square test or Fisher exact probability method. Measurement data were expressed as medians ± SD and analyzed using the t-test. Variables with a test value of P < 0.10 in the univariate analysis were included in the multivariate analysis to identify independent risk factors associated with DGE using logistic regression. The estimated odds ratio with 95% confidence intervals was used to describe the relative risk. Statistical significance was indicated by P < 0.05.
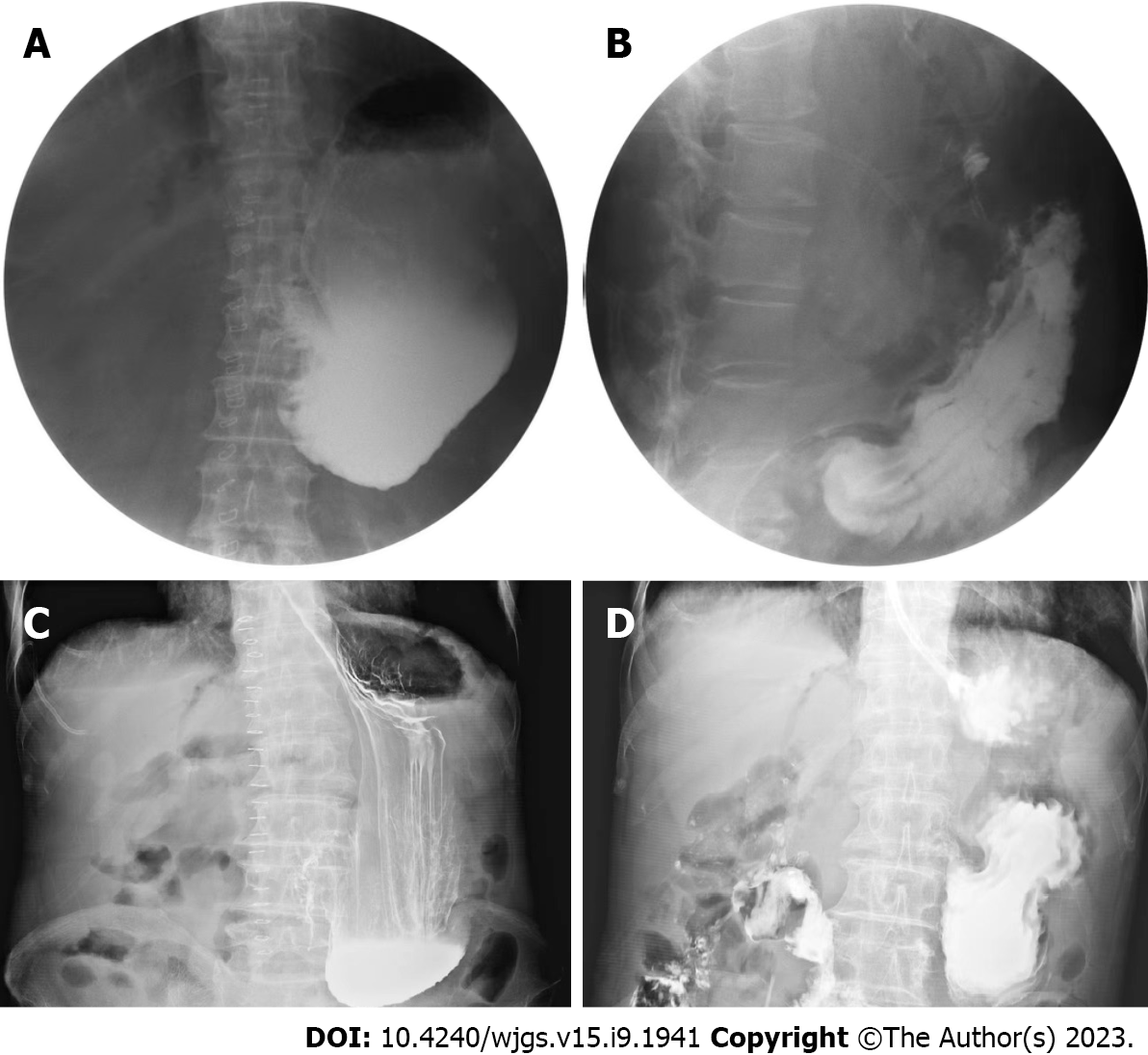
The study included 66 males (57.9%) and 48 females (42.1%) (male-to-female ratio is approximately 1.4:1), with a mean age of 62.5 years (range: 33-83 years). Sixty-three cases (55.3%) underwent PD, while 51 (44.7%) received PPPD. The primary diseases diagnosed were pancreatic cancer, cholangiocarcinoma, ampullary carcinoma, solid pseudopapillary tumor of the pancreas, intraductal papillary mucinous neoplasms, chronic pancreatitis, duodenal stromal tumor, and duodenal papillary adenomyoma, with 46, 32, 23, 3, 3, 3, 2, and 2 cases, respectively. DGE occurred in 33 patients, with an incidence of 28.9%. The angiography results are shown in Figure 1.
Univariate analysis of postoperative DGE showed that pylorus preservation, gastrointestinal anastomosis mode, postoperative abdominal complications, and ALB on a postoperative day 4 were significant risk factors for post-PD DGE (P < 0.05), as shown in Table 1.
| Clinical indexes | n | Postoperative delayed gastric emptying | χ2/t | P value | |
| Yes | No | ||||
| Sex | 0.002 | 0.965 | |||
| Male | 66 | 19 | 47 | ||
| Female | 48 | 14 | 34 | ||
| Age (yr) | 62.00 ± 9.47 | 62.63 ± 9.72 | 0.316 | 0.752 | |
| Preoperative systemic disease | 3.271 | 0.071 | |||
| With | 44 | 17 | 27 | ||
| Without | 70 | 16 | 54 | ||
| Preoperative nutritional status | 0.729 | 0.393 | |||
| Good | 92 | 25 | 67 | ||
| Poor | 22 | 8 | 14 | ||
| Pylorus preservation | 4.731 | 0.03 | |||
| Yes | 51 | 20 | 31 | ||
| No | 63 | 13 | 50 | ||
| Lymph node dissection | 2.451 | 0.117 | |||
| Yes | 58 | 13 | 45 | ||
| No | 56 | 20 | 36 | ||
| Operation time (min) | 216.54 ± 63.23 | 233.56 ± 66.35 | 1.259 | 0.211 | |
| Gastrointestinal anastomosis mode | 4.731 | 0.03 | |||
| Antecolic anastomosis | 63 | 13 | 50 | ||
| Retrocolic anastomosis | 51 | 20 | 31 | ||
| Intraoperative hemorrhage (mL) | 327.27 ± 185.86 | 367.28 ± 273.54 | 0.77 | 0.443 | |
| Postoperative pancreatic fistula | 0.277 | 0.871 | |||
| Without | 61 | 17 | 44 | ||
| Mild | 41 | 13 | 28 | ||
| Severe | 12 | 3 | 9 | ||
| Postoperative abdominal complications | 8.551 | 0.003 | |||
| With | 62 | 25 | 37 | ||
| Without | 52 | 8 | 44 | ||
| Early enteral nutrition | 0.215 | 0.643 | |||
| With | 9 | 2 | 7 | ||
| Without | 105 | 31 | 74 | ||
| Hb on postoperative day 1 | 117.23 ± 16.21 | 115.45 ± 18.23 | 0.488 | 0.627 | |
| Hb on postoperative day 4 | 113.12 ± 13.45 | 108.23 ± 14.32 | 1.682 | 0.095 | |
| Hb on postoperative day 7 | 109.64 ± 14.42 | 109.87 ± 14.23 | 0.078 | 0.938 | |
| ALB on postoperative day 1 | 30.93 ± 4.05 | 30.52 ± 3.73 | 0.519 | 0.605 | |
| ALB on postoperative day 4 | 34.85 ± 4.01 | 32.20 ± 5.22 | 2.616 | 0.01 | |
| ALB on postoperative day 7 | 34.52 ± 5.16 | 33.62 ± 4.27 | 0.959 | 0.339 | |
The six observation indexes (preoperative systemic disease, pylorus preservation, gastrointestinal anastomosis mode, postoperative abdominal complications, Hb and ALB on postoperative day 4), which were identified with P < 0.10 in the univariate analysis, were subjected to logistic regression analysis. The results are presented in Table 2.
| Clinical indexes | n | Postoperative delayed gastric emptying | χ2/t | P value | |
| Yes | No | ||||
| Preoperative systemic diseases | 3.271 | 0.071 | |||
| With | 44 | 17 | 27 | ||
| Without | 70 | 16 | 54 | ||
| Pylorus preservation | 4.731 | 0.03 | |||
| Yes | 51 | 20 | 31 | ||
| No | 63 | 13 | 50 | ||
| Gastrointestinal anastomosis mode | 4.731 | 0.03 | |||
| Antecolic anastomosis | 63 | 13 | 50 | ||
| Retrocolic anastomosis | 51 | 20 | 31 | ||
| Postoperative abdominal complications | 8.551 | 0.003 | |||
| With | 62 | 25 | 37 | ||
| Without | 52 | 8 | 44 | ||
| Hb on postoperative day 4 | 113.12 ± 13.45 | 109.43 ± 14.32 | 1.269 | 0.207 | |
| ALB on postoperative day 4 | 34.85 ± 4.01 | 32.20 ± 5.07 | 2.616 | 0.01 | |
Finally, the regression equation included postoperative abdominal complications, preoperative systemic diseases, and ALB on postoperative day 4 as factors influencing the occurrence of DGE after PD, as shown in Table 3.
| Related factors | Regression coefficients | OR | OR (95%CI) | P value |
| Postoperative abdominal complications | 1.562 | 4.768 | 1.748-13.005 | 0.002 |
| Preoperative systemic diseases | 0.923 | 2.516 | 1.004-6.304 | 0.049 |
| ALB on postoperative day 4 | 0.178 | 1.195 | 1.062-1.344 | 0.003 |
This study enrolled 114 patients who underwent PD within a recent 5-year period at a single center, ensuring a brief timeframe and providing comprehensive and reliable data. Severe DGE grades of B and C were observed in 33 of the 114 patients after PD, resulting in an incidence rate of 28.9%, consistent with findings from other reports. We further investigated the potential impact of pyloric preservation on the risk of DGE, which has been controversial. A randomized controlled trial (RCT) study conducted by Japanese scholars[14] on 130 patients who underwent PD reported a significantly higher incidence of DGE in patients with pylorus preservation compared to those without pylorus preservation (17.2% vs 4.5%, P = 0.02). However, another RCT study conducted by German scholars on 188 patients undergoing PD by German scholars[15] found no significant difference in the incidence of DGE in 95 patients with pylorus preservation and 93 patients without pylorus preservation (25.3% vs 31.2%, P = 0.208). In the clinical setting, we have consistently observed patients undergoing PPPD to have a higher possibility of developing DGE. The univariate analysis of this study also showed a higher incidence of DGE in patients who underwent PPPD (P = 0.03), with 20 (39.2%) among the 51 patients developing DGE, compared to 13 (20.6%) among the 63 patients who underwent PD, which suggesting that PPPD patients have a high incidence of DGE in patients who have undergone PPPD. However, the multivariate analysis did not reveal a significant correlation between pylorus preservation and DGE. A further in-depth study found that patients with pylorus preservation experienced earlier and milder cases of DGE. If there were no other associated risk factors, the faster patient recovery would not compromise the safety of the procedure or the occurrence of postoperative abdominal complications.
Many studies have indicated postoperative abdominal complications as risk factors for DGE[14,16]. In this research, the univariate analysis revealed that postoperative abdominal complications are independent risk factors (P = 0.003) for DGE. Multivariate analysis identified postoperative abdominal complications as the most significant risk factors for DGE (OR = 4.768). Serious postoperative abdominal complications, such as abdominal infection, hemorrhage, chylous fistula, and anastomotic leakage, primarily occur due to pancreatic fistula and biliary fistula with infection. Although postoperative pancreatic leakage was considered an observation index in this study, both univariate and multivariate analyses showed no significant association with postoperative DGE. This finding could be attributed to the adequate abdominal drainage of a simple pancreatic fistula and the absence of local infection in the abdominal cavity, reducing the likelihood of developing postoperative DGE.
Some scholars have suggested[16] that local inflammation or infection foci caused by pancreatic fistula may contribute to DGE. Therefore, measures such as improving the operation quality and implementing early postoperative interventions to promote intestinal peristalsis could lower the incidence of postoperative pancreatic fistula; this ensures unobstructed drainage after the occurrence of pancreatic fistula. The prompt puncture and drainage of the fistula could prevent the accumulation of corrosive fluids, thereby lowering the risk of postoperative DGE. Furthermore, this study identified two other significant risk factors: early postoperative ALB and preoperative systemic diseases. Postoperative ALB, in the presence of systemic diseases, leads to anastomotic edema; suture cutting causes a significant increase in the incidence of anastomotic leakage, which can easily result in abdominal infection, bleeding, and other complications, resulting in postoperative DGE.
A study has investigated the use of neostigmine in treating GP following abdominal surgery[17]; it has shown encouraging results, particularly in the treatment of post-PD DGE. In this study, neostigmine was administered to a 73-year-old male patient with refractory GP after distal gastrectomy, demonstrating a certain degree of safety and clinical efficacy, suggesting that neostigmine is a safe and effective treatment in GP. Previous studies have reported[18-20] the presence of receptor pathways for spinal and sympathetic nerves in the skin and the clinical effectiveness of intradermal administration in treating conditions such as herpes zoster neuralgia and visceral pain[21,22]. Our study demonstrated the unique effects of neostigmine administered via the transdermal receptor pathway, which cannot be replicated through other routes of administration. Investigating the target of neostigmine in the receptor pathway is also a future research direction for our team.
Based on the results of this study, the following recommendations can be made for the prevention of DGE after PD: (1) Effective communication with patients and their families before the operation is crucial; this allows them to fully comprehend the potential postoperative complications, management strategies, and past experiences in handling complications, helping alleviate their anxiety; (2) Patients with systemic diseases such as hypertension and diabetes should receive careful perioperative treatment to maintain hemodynamic stability and a stable internal environment; (3) Standardizing and improving the procedure is essential to minimize postoperative pancreatic and bile leakage; and (4) Timely initiation of preoperative nutritional support therapy and postoperative ALB supplementation is essential to prevent tissue edema and maintain water-electrolyte balance. Continuous postoperative gastrointestinal decompression, and using patent gastric and abdominal cavity drainage tubes could help reduce the likelihood of abdominal complications.
However, this study has some limitations. As a single-center retrospective study, the potential biases in the data collection and analysis processes could have moderately influenced the final study results. Moreover, no specific analysis was performed during DGE treatment, and a larger sample size with more extensive data is needed to verify the therapeutic effect of neostigmine. Therefore, well-designed, multi-center studies with larger sample sizes are necessary for validation.
Mortality after pancreaticoduodenectomy (PD) has decreased to very low levels in specialized centers. However, postoperative morbidity remains high. Delayed gastric emptying (DGE) still remains the most frequent complication following pancreatoduodenectomy (PD).
When it comes to treatment, the specific pathogenesis of DGE remains uncharacterized, nor is there a specific treatment plan for DGE, resulting in unsatisfactory effects of various treatment approaches. The purpose of this study is to thoroughly explore the risk factors of the disease and introduce a new treatment method.
This study aims to identify related risk factors for DGE after the PD procedure.
In this retrospective, cross-sectional study, clinical data were collected from 114 patients who underwent PD from January 2015 to June 2018. They were analyzed regarding demographic factors, pre- and perioperative characteristics, and surgical complications. Univariate and multivariate analyses were performed to identify the risk factors for post-PD DGE.
The study included 66 males (57.9%) and 48 females (42.1%), aged 33-83 years (mean: 62.5), with a male-to-female ratio of approximately 1.4:1. There were 63 cases (55.3%) of PD and 51 cases (44.7%) of pylorus-preserving pancreatoduodenectomy (PPPD). Among the 114 patients who underwent PD, 33 (28.9%) developed postoperative DGE. Univariate analysis revealed significant differences in four of the 14 clinical indexes observed: Pylorus preservation, retrocolonic anastomosis, postoperative abdominal complications, and early postoperative albumin (ALB). Logistic regression analysis further identified postoperative abdominal complications [odds ratio (OR) = 4.768, P = 0.002], preoperative systemic diseases (OR = 2.516, P = 0.049), and early postoperative ALB (OR = 1.195, P = 0.003) as significant risk factors.
Postoperative severe abdominal complications, preoperative systemic disease and early postoperative ALB are risk factors for post-PD DGE.
The research perspective of this study is to thoroughly explore the risk factors for post-PD DGE.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rastogi A, India; Yoshikawa K, Japan S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Xiang Y, Wu J, Lin C, Yang Y, Zhang D, Xie Y, Yao X, Zhang X. Pancreatic reconstruction techniques after pancreaticoduodenectomy: a review of the literature. Expert Rev Gastroenterol Hepatol. 2019;13:797-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Peng YC, Wu CH, Tien YW, Lu TP, Wang YH, Chen BB. Preoperative sarcopenia is associated with poor overall survival in pancreatic cancer patients following pancreaticoduodenectomy. Eur Radiol. 2021;31:2472-2481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 3. | Schorn S, Demir IE, Vogel T, Schirren R, Reim D, Wilhelm D, Friess H, Ceyhan GO. Mortality and postoperative complications after different types of surgical reconstruction following pancreaticoduodenectomy-a systematic review with meta-analysis. Langenbecks Arch Surg. 2019;404:141-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Wang TH, Lin AY, Mentor K, O'Grady G, Pandanaboyana S. Delayed Gastric Emptying and Gastric Remnant Function After Pancreaticoduodenectomy: A Systematic Review of Objective Assessment Modalities. World J Surg. 2023;47:236-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Simon R. Complications After Pancreaticoduodenectomy. Surg Clin North Am. 2021;101:865-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 58] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 6. | Kurahara H, Shinchi H, Maemura K, Mataki Y, Iino S, Sakoda M, Ueno S, Takao S, Natsugoe S. Delayed gastric emptying after pancreatoduodenectomy. J Surg Res. 2011;171:e187-e192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Cogliandro RF, Rizzoli G, Bellacosa L, De Giorgio R, Cremon C, Barbara G, Stanghellini V. Is gastroparesis a gastric disease? Neurogastroenterol Motil. 2019;31:e13562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Panwar R, Pal S. The International Study Group of Pancreatic Surgery definition of delayed gastric emptying and the effects of various surgical modifications on the occurrence of delayed gastric emptying after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int. 2017;16:353-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Mao SH, Shyr BS, Chen SC, Wang SE, Shyr YM, Shyr BU. Risk factors for delayed gastric emptying in pancreaticoduodenectomy. Sci Rep. 2022;12:22270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Navas CM, Wadas ED, Zbib NH, Crowell MD, Lacy BE. Gastroparesis and Severity of Delayed Gastric Emptying: Comparison of Patient Characteristics, Treatments and Medication Adverse Events. Dig Dis Sci. 2021;66:526-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Tewari M, Mahendran R, Kiran T, Verma A, Dixit VK, Shukla S, Shukla HS. Outcome of 150 Consecutive Blumgart's Pancreaticojejunostomy After Pancreaticoduodenectomy. Indian J Surg Oncol. 2019;10:65-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Luttikhold J, de Ruijter FM, van Norren K, Diamant M, Witkamp RF, van Leeuwen PA, Vermeulen MA. Review article: the role of gastrointestinal hormones in the treatment of delayed gastric emptying in critically ill patients. Aliment Pharmacol Ther. 2013;38:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Study Group of Pancreatic Surgery in Chinese Society of Surgery of Chinese Medical Association; Pancreatic Disease Committee of Chinese Research Hospital Association; Editorial Board of Chinese Journal of Surgery. [A consensus statement on the diagnosis, treatment, and prevention of common complications after pancreatic surgery (2017)]. Zhonghua Wai Ke Za Zhi. 2017;55:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, Uchiyama K, Yamaue H. Pylorus ring resection reduces delayed gastric emptying in patients undergoing pancreatoduodenectomy: a prospective, randomized, controlled trial of pylorus-resecting versus pylorus-preserving pancreatoduodenectomy. Ann Surg. 2011;253:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 147] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 15. | Matsumoto I, Shinzeki M, Asari S, Goto T, Shirakawa S, Ajiki T, Fukumoto T, Suzuki Y, Ku Y. A prospective randomized comparison between pylorus- and subtotal stomach-preserving pancreatoduodenectomy on postoperative delayed gastric emptying occurrence and long-term nutritional status. J Surg Oncol. 2014;109:690-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Qu H, Sun GR, Zhou SQ, He QS. Clinical risk factors of delayed gastric emptying in patients after pancreaticoduodenectomy: a systematic review and meta-analysis. Eur J Surg Oncol. 2013;39:213-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 17. | Jayarajah U, Yapa K, Ranaweera K, Rahuman A, Perera P, Weerasekara D. Successful use of neostigmine for resistant gastroparesis following distal gastrectomy: A case report. Int J Surg Case Rep. 2023;106:108166. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Orihara M, Takazawa T, Horiuchi T, Sakamoto S, Nagumo K, Tomita Y, Tomioka A, Yoshida N, Yokohama A, Saito S. Comparison of incidence of anaphylaxis between sugammadex and neostigmine: a retrospective multicentre observational study. Br J Anaesth. 2020;124:154-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 19. | Dagnino APA, Campos MM. Chronic Pain in the Elderly: Mechanisms and Perspectives. Front Hum Neurosci. 2022;16:736688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 82] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 20. | Rzhevskiy A, Popov A, Pavlov C, Anissimov Y, Zvyagin A, Levin Y, Kochba E. Intradermal injection of lidocaine with a microneedle device to provide rapid local anaesthesia for peripheral intravenous cannulation: A randomised open-label placebo-controlled clinical trial. PLoS One. 2022;17:e0261641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Wang YL, Zhu HY, Lv XQ, Ren XY, Peng YC, Qu JY, Shen XF, Sun R, Xiao ML, Zhang H, Chen ZH, Cong P. Electroacupuncture Zusanli (ST36) Relieves Somatic Pain in Colitis Rats by Inhibiting Dorsal Root Ganglion Sympathetic-Sensory Coupling and Neurogenic Inflammation. Neural Plast. 2023;2023:9303419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 22. | Yang XN, Geng ZS, Zhang XL, Zhang YH, Wang XL, Zhang XB, Cui JZ. Single intracutaneous injection of local anesthetics and steroids alleviates acute nonspecific neck pain: A CONSORT-perspective, randomized, controlled clinical trial. Medicine (Baltimore). 2018;97:e11285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |