Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1652
Peer-review started: April 28, 2023
First decision: May 16, 2023
Revised: May 30, 2023
Accepted: June 21, 2023
Article in press: June 21, 2023
Published online: August 27, 2023
Processing time: 119 Days and 10.9 Hours
Few studies have addressed the question of which drain types are more beneficial for patients with pancreatic trauma (PT).
To investigate whether sustained low negative pressure irrigation (NPI) suction drainage is superior to closed passive gravity (PG) drainage in PT patients.
PT patients who underwent pancreatic surgery were enrolled consecutively at a referral trauma center from January 2009 to October 2021. The primary outcome was defined as the occurrence of severe complications (Clavien-Dindo grade ≥
In this study, 146 patients underwent initial PG drainage, and 50 underwent initial NPI suction drainage. In the entire cohort, a multivariable logistic regression model showed that the adjusted risk for severe complications was decreased with NPI suction drainage [14/50 (28.0%) vs 66/146 (45.2%); odds ratio (OR), 0.437; 95% confidence interval (CI): 0.203-0.940]. After 1:1 PSM, 44 matched pairs were identified. The proportion of each operative procedure performed for pancreatic injury-related and other intra-abdominal organ injury-related cases was comparable in the matched cohort. NPI suction drainage still showed a lower risk for severe complications [11/44 (25.0%) vs 21/44 (47.7%); OR, 0.365; 95%CI: 0.148-0.901]. A forest plot revealed that NPI suction drainage was associated with a lower risk of Clavien-Dindo severity in most subgroups.
This study, based on one of the largest PT populations in a single high-volume center, revealed that initial NPI suction drainage could be recommended as a safe and effective alternative for managing complex PT patients.
Core Tip: Few studies have addressed the question of which drain types are more beneficial for patients with pancreatic trauma (PT). A total of 196 PT patients were selected from 2009 to 2021, of whom 146 underwent closed passive gravity (PG) drainage, and 50 underwent low negative pressure irrigation (NPI) suction drainage. In the entire cohort, multivariate analysis showed that the risk for severe complications (Clavien-Dindo grade ≥ Ⅲb) was decreased with NPI suction drainage. After 1:1 propensity score matching between the PG and NPI groups, the results were consistent with multivariate analysis.
- Citation: Li KW, Wang K, Hu YP, Yang C, Deng YX, Wang XY, Liu YX, Li WQ, Ding WW. Initial suction drainage decreases severe postoperative complications after pancreatic trauma: A cohort study. World J Gastrointest Surg 2023; 15(8): 1652-1662
- URL: https://www.wjgnet.com/1948-9366/full/v15/i8/1652.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i8.1652
Pancreatic trauma (PT) is relatively rare; however, injury to the pancreas can be challenging for even the most experienced trauma surgeon[1-3]. Significant morbidity and mortality are usually related to the cumulative effect of all injured organs[4]. Surgical management is nearly always adopted for PT in the emergency setting of abdominal trauma[5,6].
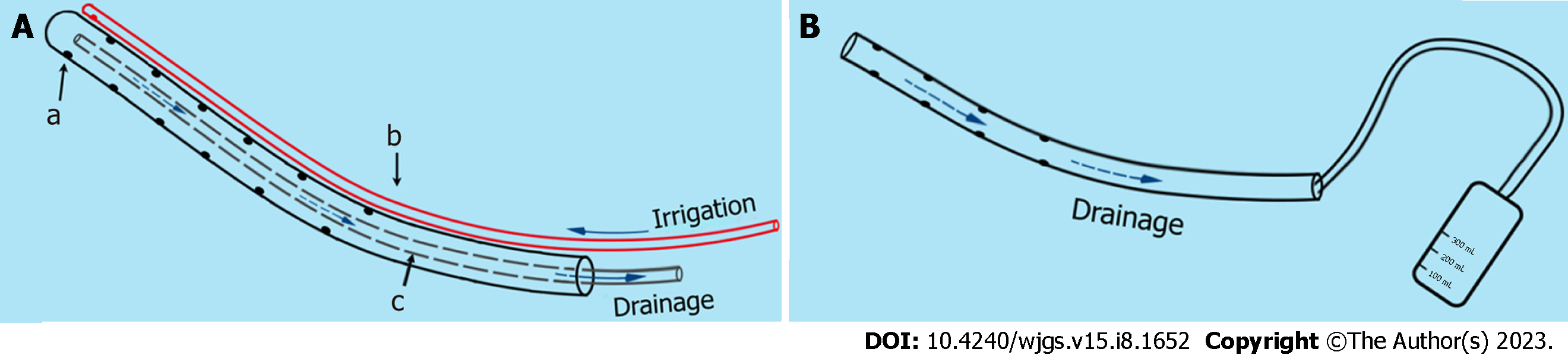
Consensus regarding the need for drainage has been formulated in many management strategies for PT[7-9]. The rationale is to evacuate intra-abdominal exudate, pancreatic juice or blood that can accumulate after surgery and serve as an early warning sign of possible pancreatic fistula, anastomotic fistula and associated hemorrhage[8-10]. Moreover, peripancreatic drainage alone is an important therapeutic measure[11,12]. The following two drain types are mainly placed for pancreatic surgery: Closed passive gravity (PG) drainage and sustained low negative pressure irrigation (NPI) suction drainage. PG drainage applies no pressure, evacuating fluid by gravity alone with intra-abdominal pressure[13]. NPI suction drainage actively flushes the abdominal cavity with normal saline under low negative pressure[14,15]. In fact, high-level evidence has not yet been provided to support the choice of drain type for PT[16].
Several issues related to drainage are considered counterproductive, leading to constant evaluation of the roles of these methods[16,17]. First, the drains can serve as portals of entry for bacteria[18]. Second, fistula, hemorrhage, or hollow-organ perforation can be caused by mechanical pressure, suction or erosion around the anastomosis and fragile tissue[19]. It is of paramount importance to understand the extent to which drains influence the development and severity of complications. Therefore, based on one of the largest PT populations in our high-volume center, we performed a retrospective study to investigate whether NPI is superior to PG drainage.
We performed a retrospective cohort study of consecutive patients who underwent pancreatic surgery at a tertiary trauma referral center between January 2009 and October 2021 in our PT database. The study was approved by the Institutional Review Board (IRB) of Jinling Hospital (Approval No. 2021DZGZR-YBB-009). Informed consent was waived by the IRB because of the retrospective nature of the study. This study was conducted in accordance with the principles of the Declaration of Helsinki. The exclusion criteria were as follows: Early death (< 48 h) after admission; Glasgow Coma Scale score ≤ 8; Abbreviated Injury Scale score = 6 for any area of the body; nonoperative treatment; pregnancy status; and previous history of malignancy, immune system or hematological diseases.
Pancreatic injuries are classified into 5 grades (Ⅰ-Ⅴ) according to the Organ Injury Scale, proposed by the American Association for the Surgery of Trauma in 1990. For low-grade PT (Ⅰ-Ⅱ), drainage alone was performed after complete exposure of the pancreas. For high-grade PT (Ⅲ-Ⅴ), distal pancreatectomy with or without splenectomy was usually adopted for grade III injury; debridement/resection of the area of injury, closure of the proximal stump and distal Roux-en-Y pancreaticojejunostomy or drainage alone was implemented for grade IV injury; and one-stage damage control drainage and subsequent definitive operative or pancreaticoduodenectomy was utilized for grade Ⅴ injury.
After distal pancreatectomy, a drain was inserted via the left flank and was placed near the pancreatic remnant; the other drain was placed in the left subphrenic area, but only when splenectomy was performed. Similarly, a drain was inserted via the left flank and was placed between the pancreaticojejunostomy and pancreatic remnant after middle pancreatectomy. After pancreatoduodenectomy, a drain was inserted via the right flank and placed posterior to the biliary anastomosis, extending to the proximal margin of the pancreatic remnant. The other drain was inserted via the left flank and was placed posterior to the stomach, extending to the posterior surface of the pancreatic anastomosis in proximity to the contralateral drain. In addition, individualized operative management was performed, and drains were placed as appropriate after careful assessment of the other intra-abdominal organs.
The two drain types adopted are shown in Figure 1. The decision regarding which drain type to place was made on a case-by-case basis and according to the surgeon's preference. Drains were routinely kept in situ for at least postoperative days (POD) 7 to 10. Computed tomography (CT) scans were performed every other week postoperatively. Once pancreatic fistula grade B/C or gastrointestinal fistula was confirmed by fistulography, the duration of drain placement was prolonged. For these patients, PG drainage was replaced by NPI suction drainage through the sinus tract for irrigation to minimize erosion of the surrounding tissue by the digestive juice. A controlled pancreaticocutaneous fistula or enterocutaneous fistula was created by retaining the catheter in situ until the fistula healed spontaneously. When necessary, a CT-guided percutaneous drainage procedure was performed in patients with local pancreatic complications after failed initial drainage and/or new-onset gastrointestinal fistula and localized intra-abdominal abscess requiring source control, and the PG drain was then replaced with NPI suction drainage following the guidewire.
We regularly replaced the catheter to maximize the effect of sustained irrigation drainage and reduce the size of the tube by degrees as appropriate. Two replacement strategies are employed for the management of NPI suction drainage in clinical practice: (1) Planned replacement for prophylactic drainage; and (2) On-demand replacement for therapeutic drainage. If patients do not develop pancreatic fistula grade B/C or gastrointestinal fistula and the volume of drainage fluid is decreasing, prophylactic NPI suction drainage is planned to be replaced every 3 d. For patients with pancreatic fistula grade B/C or gastrointestinal fistula, on-demand replacement is adopted because the role of NPI has been converted to therapeutic drainage. The catheter was retained in situ to create a controlled pancreaticocutaneous fistula or enterocutaneous fistula when there was a large volume of drainage fluid. In addition, the nature of the drainage fluid and the irrigation and drainage fluid in and out volume per unit of time were used to judge whether catheter blockage occurred. If blockage occurred, it was replaced promptly. Moreover, in the presence of a decreasing volumes of drainage fluid and no evidence of intra-abdominal infection, we switched the NPI suction drainage from on demand to planned replacement.
We adhered to the following drain removal policy: Lack of infection-induced systemic inflammatory response syndrome; pancreatic fistula defined by the International Study Group of Pancreatic Fistula was absent or grade A; the evidence provided by CT excluded intra-abdominal abscess or undrained fluid collections; drained fluid was less than 20 mL per day and turned clear; and lack of any gastrointestinal fistula. Additional management methods included the administration of antibiotics, supplemental parenteral or enteral nutrition, reinterventions (reoperation, endoscopic or interventional radiological procedures), and organ function support.
Data analyzed included demographics, vital signs, injury parameters, operative procedures, types and locations of drains, complications, reinterventions, bacterial culture information about drainage fluid samples, mortality and length of stay (LOS). The primary outcome was the occurrence of severe complications defined as Clavien-Dindo grade Ⅲb-Ⅴ during hospitalization. Further details on the definitions of outcome variables are provided in Supplementary Table 1.
Student’s t test and Wilcoxon’s rank sum test were used to compare normal or nonnormal continuous variables, respectively. The chi-square test and Fisher’s exact test were used to compare categorical variables. A multivariate logistic regression model was applied to evaluate the associations between the primary outcome and different drain types. Variables with P < 0.2 in the univariate test were included in the multivariate analysis.
To study effect modification by different drainage methods and to adjust for confounding factors, we performed sensitivity analysis based on propensity score matching (PSM). The PG group was matched 1:1 with the NPI group using their propensity scores with the nearest neighbor matching algorithm without replacement (the caliper was set at 0.2). A standardized mean difference (SMD) of less than 10% indicates appropriate balance. A univariable logistic regression model was adopted to estimate the odds ratio (OR) and corresponding 95% confidence interval (CI) for the primary outcome. Prespecified subgroup analyses were performed in the matched cohort to determine whether the effect of drainage varied across stratification factors of covariates. R software, version 4.0.3, was used for statistical analysis.
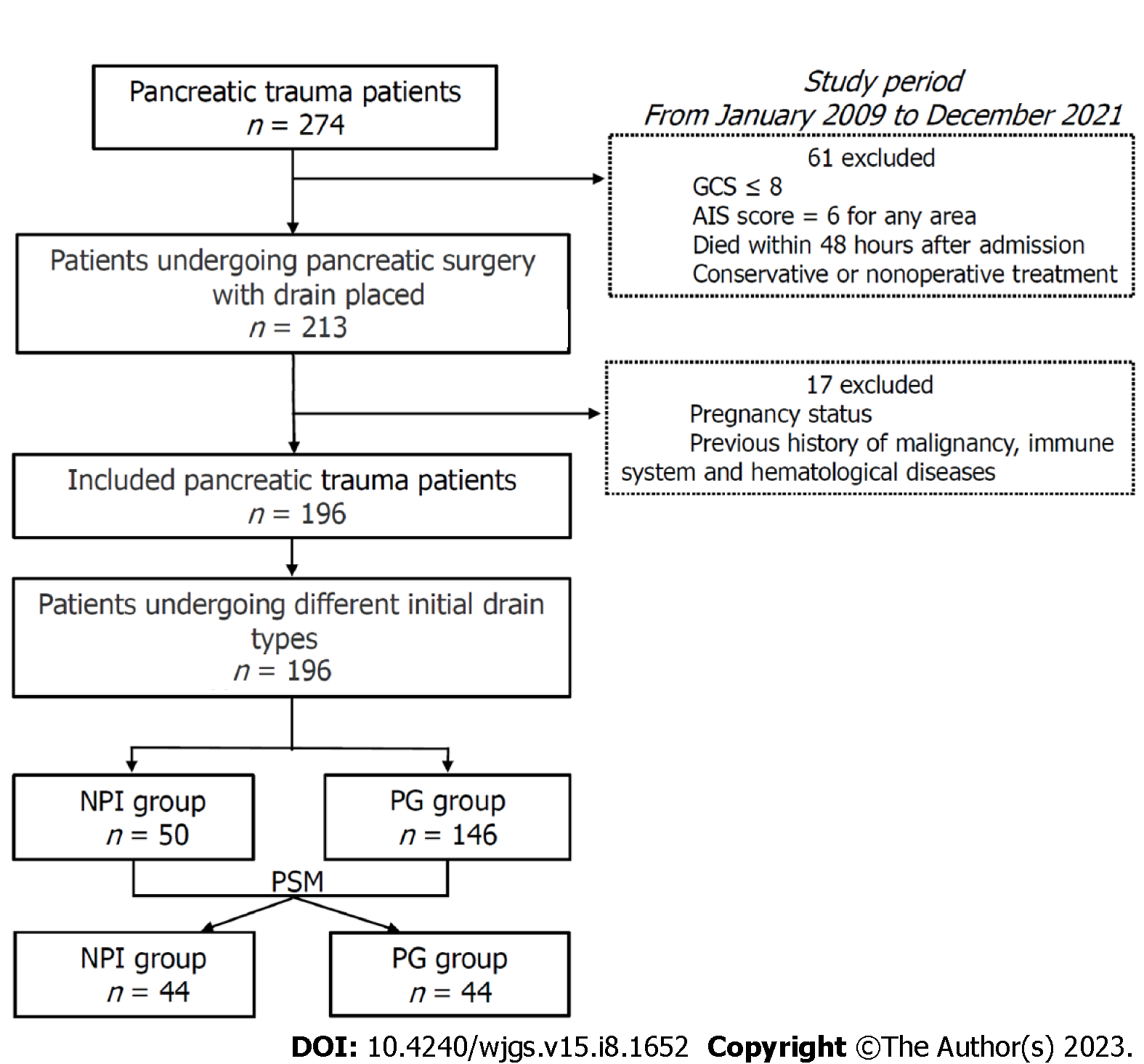
Two hundred thirteen PT patients were managed by operative management with drain placement during the study period. Of these patients, 196 met the inclusion criteria: 146 (74.5%) in the PG group vs 50 (25.5%) in the NPI group. The screening process is shown in Figure 2. The patients’ preoperative demographics, clinical characteristics and injury parameters are summarized in Table 1. In the entire cohort, the NPI group had less duodenum injury and more concomitant vascular injury (P < 0.05). Regarding the time from trauma to operation, delayed operative treatment (24 h) occurred more frequently in the NPI group (46.0% vs 20.5%, P = 0.001).
| Characteristics | Before matching | After matching | ||||||
| PG (n = 146) | NPI (n = 50) | P value | PG (n = 44) | NPI (n = 44) | P value | |||
| Male sex, n (%) | 137 (93.8) | 43 (86.0) | 0.148 | 41 (93.2) | 39 (88.6) | 0.518 | ||
| Age, median (IQR) | 40 (30.75-48.25) | 44.5 (26.25-52.25) | 0.058 | 39 (30.25-47.00) | 44.5 (27-51) | 0.843 | ||
| BMI, mean ± SD | 23.04 (3.68) | 23.46 (3.62) | 0.477 | 23.59 (4.48) | 23.36 (3.57) | 0.787 | ||
| Blunt injury, n (%) | 137 (93.8) | 48 (96.0) | 0.733 | 42 (95.5) | 42 (95.5) | 1.000 | ||
| ISS, median (IQR) | 17 (9-21) | 16 (9-20) | 0.183 | 16 (9-20) | 16 (9-20) | 0.936 | ||
| Abdominal AIS, median (IQR) | 3 (3-4) | 3 (3-4) | 0.146 | 3 (3-4) | 3 (3-4) | 0.985 | ||
| Pancreatic injury grade, n (%) | 0.090 | 0.829 | ||||||
| Ⅰ + Ⅱ | 45 (30.8) | 22 (44.0) | 19 (43.2) | 18 (40.9) | ||||
| Ⅲ + Ⅳ + Ⅴ | 101 (69.2) | 28 (56.0) | 25 (56.8) | 26 (59.1) | ||||
| Isolated pancreatic injury, n (%) | 0.489 | 1.000 | ||||||
| No | 123 (84.2) | 40 (80.0) | 35 (79.5) | 35 (79.5) | ||||
| Yes | 23 (15.8) | 10 (20.0) | 9 (20.5) | 9 (20.5) | ||||
| Duodenum injury, n (%) | 0.043 | 1.000 | ||||||
| No | 116 (79.5) | 46 (92.0) | 39 (88.6) | 40 (90.9) | ||||
| Yes | 30 (20.5) | 4 (8.0) | 5 (11.4) | 4 (9.1) | ||||
| Vascular injury, n (%) | 0.032 | 0.787 | ||||||
| No | 127 (87.0) | 37 (74.0) | 35 (79.5) | 36 (81.8) | ||||
| Yes | 19 (13.0) | 13 (26.0) | 9 (20.5) | 8 (18.2) | ||||
| Parenchyma organ injury, n (%) | 0.242 | 0.831 | ||||||
| No | 62 (42.5) | 26 (52.0) | 22 (50.0) | 23 (52.3) | ||||
| Yes | 84 (57.5) | 24 (48.0) | 22 (50.0) | 21 (47.7) | ||||
| Hollow organ injury, n (%) | 0.144 | 1.000 | ||||||
| No | 53 (36.3) | 24 (48.0) | 20 (45.5) | 20 (45.5) | ||||
| Yes | 93 (63.7) | 26 (52.0) | 24 (54.5) | 24 (54.5) | ||||
| Shock on admission, n (%) | 0.597 | 0.777 | ||||||
| No | 127 (87.0) | 42 (84.0) | 36 (81.8) | 37 (84.1) | ||||
| Yes | 19 (13.0) | 8 (16.0) | 8 (18.2) | 7 (15.9) | ||||
| Number of abdominal organ injuries, n (%) | 0.093 | 0.631 | ||||||
| 2 | 49 (33.6) | 22 (44.0) | 18 (40.9) | 20 (45.4) | ||||
| ≥ 3 | 74 (50.7) | 18 (36.0) | 17 (38.6) | 15 (34.1) | ||||
| Time to operation, n (%) | 0.001 | 1.000 | ||||||
| < 24 h | 116 (79.5) | 27 (54.0) | 27 (61.4) | 27 (61.4) | ||||
| ≥ 24 h | 30 (20.5) | 23 (46.0) | 17 (38.6) | 17 (38.6) | ||||
PSM with a 1:1 ratio resulted in 88 patients (PG 44, NPI 44). Before PSM, 13 of 15 baseline characteristics were unequally distributed between the two groups; following PSM, all of the variables reached an SMD < 0.10 (Supple
| Operative procedure | Before matching | After matching | ||||
| PG (n = 146) | NPI (n = 50) | P value | PG (n = 44) | NPI (n = 44) | P value | |
| Pancreas injury-related, n (%) | ||||||
| Peripancreatic drainage alone | 61 (41.8) | 22 (44.0) | 0.784 | 19 (43.2) | 19 (43.2) | 1.000 |
| Distal pancreatectomy | 37 (25.3) | 10 (20.0) | 0.445 | 10 (22.7) | 8 (18.2) | 0.597 |
| Distal pancreatectomy + splenectomy | 22 (15.1) | 9 (18.0) | 0.624 | 6 (13.6) | 8 (18.2) | 0.560 |
| Pancreaticojejunostomy | 21 (14.4) | 7 (14.0) | 0.947 | 8 (18.2) | 7 (15.9) | 0.777 |
| Whipple | 5 (3.4) | 2 (4.0) | 0.850 | 1 (2.3) | 2 (4.5) | 1.000 |
| Other intra-abdominal organ injury-related, n (%) | ||||||
| Gastric or duodenal | 38 (26.0) | 6 (12.0) | 0.040 | 5 (11.4) | 5 (11.4) | 1.000 |
| Jejunal or ileal | 25 (17.1) | 9 (18.0) | 0.888 | 9 (20.5) | 9 (20.5) | 1.000 |
| Colorectal | 30 (20.5) | 11 (22.0) | 0.828 | 10 (22.7) | 10 (22.7) | 1.000 |
| Parenchymal organ | 58 (39.7) | 12 (24.0) | 0.045 | 11 (25.0) | 10 (22.7) | 0.803 |
| Vascular | 19 (13.0) | 13 (26.0) | 0.032 | 9 (20.5) | 8 (18.2) | 0.787 |
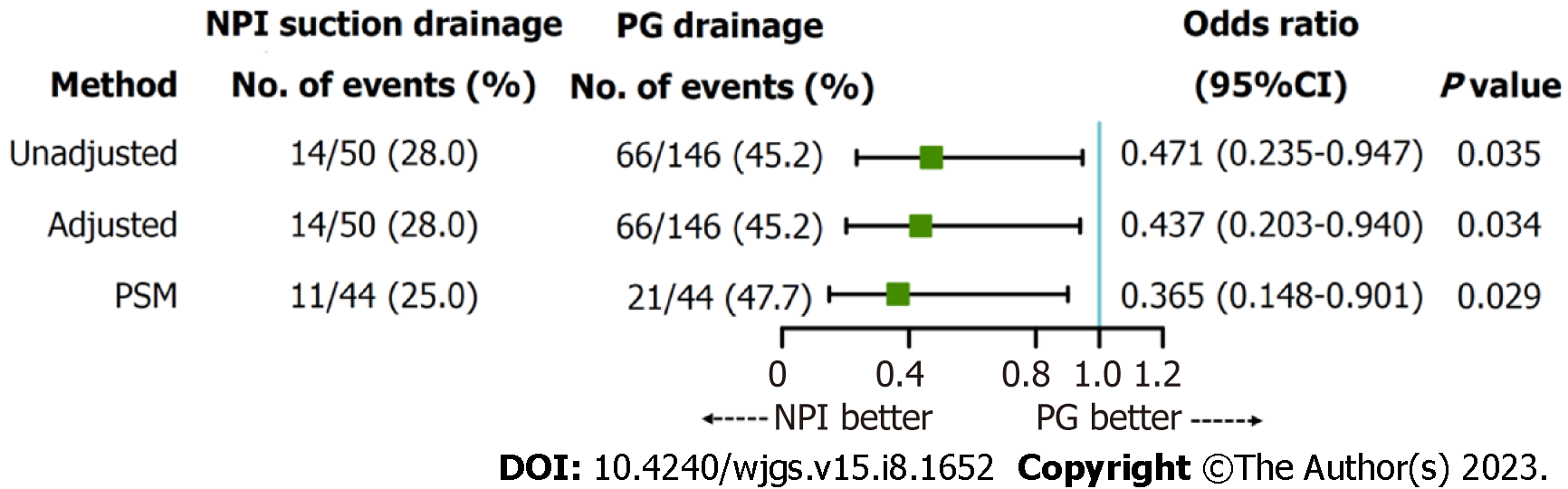
In the entire cohort, the incidence of severe complications in the NPI group was significantly lower than that in the PG group [14/50 (28.0%) vs 66/146 (45.2%), P = 0.033] (Table 3). In univariate logistic regression analysis, injury severity score, abdominal abbreviated injury scale, isolated pancreatic injury, and different drain types were associated with severe complications (P < 0.05) (Supplementary Table 2). Notably, the NPI group was significantly less likely to develop severe complications (OR: 0.471; 95%CI: 0.235-0.947; P = 0.035). In multivariate analysis, the adjusted risk for severe complications was decreased in the NPI group (OR: 0.437; 95%CI: 0.203-0.940; P = 0.034) (Figure 3). After PSM, the results of the sensitivity analysis were consistent with those of the multivariate analysis (OR: 0.365; 95%CI: 0.148-0.901; P = 0.029) (Figure 3).
| Outcomes | Before matching | After matching | ||||
| PG (n = 146) | NPI (n = 50) | P value | PG (n = 44) | NPI (n = 44) | P value | |
| Clavien-Dindo grade ≥ Ⅲb, n (%) | 66 (45.2) | 14 (28.0) | 0.033 | 21 (47.7) | 11 (25.0) | 0.045 |
| Pancreas-related, n (%) | 70 (47.9) | 15 (30.0) | 0.027 | 23 (52.3) | 13 (29.5) | 0.050 |
| Pancreatic fistula grade B/C | 62 (42.5) | 13 (26.0) | 0.039 | 22 (50.0) | 11 (25.0) | 0.027 |
| Pancreatic pseudocyst | 2 (1.4) | 2 (4.0) | 0.269 | 0 | 2 (4.5) | 0.494 |
| Peripancreatic abscess | 6 (4.1) | 0 | 0.341 | 1 (2.3) | 0 | 1.000 |
| Organ failure, n (%) | 37 (25.3) | 9 (18.0) | 0.290 | 6 (13.6) | 3 (6.8) | 0.484 |
| Circulatory failure | 23 (15.8) | 6 (12.0) | 0.519 | 4 (9.1) | 2 (4.5) | 0.676 |
| Respiratory failure | 20 (13.7) | 5 (10.0) | 0.499 | 4 (9.1) | 1 (2.3) | 0.360 |
| Renal failure | 24 (16.4) | 7 (14.0) | 0.683 | 5 (11.4) | 3 (6.8) | 0.713 |
| Gastrointestinal fistulas, n (%) | 50 (34.2) | 10 (20.0) | 0.059 | 17 (38.6) | 7 (15.9) | 0.030 |
| Hemorrhage grade B/C, n (%) | 34 (23.3) | 7 (14.0) | 0.163 | 12 (27.3) | 6 (13.6) | 0.080 |
| Intra-abdominal abscess, n (%) | 20 (13.7) | 8 (16.0) | 0.688 | 7 (15.9) | 5 (11.4) | 0.534 |
| Sepsis, n (%) | 27 (18.5) | 7 (14.0) | 0.469 | 4 (9.1) | 3 (6.8) | 1.000 |
| In-hospital mortality, n (%) | 16 (11.0) | 3 (6.0) | 0.412 | 3 (6.8) | 2 (4.5) | 1.000 |
| Reoperation, n (%) | 55 (38.2) | 11 (22.0) | 0.037 | 16 (36.4) | 7 (15.9) | 0.029 |
| CT-drainage, n (%) | 47 (32.2) | 9 (18.0) | 0.038 | 15 (34.1) | 7 (15.9) | 0.042 |
| Drainage period, median (IQR) | 47.0 (30.0-75.25) | 37.0 (20.0-54.25) | 0.002 | 47.0 (30.0-68.0) | 35.0 (20.0-54.75) | 0.009 |
| LOS, median (IQR) | 65.5 (47.75-97.0) | 43.5 (30.5-69.25) | 0.002 | 62.5 (43.75-97.0) | 44.0 (33.0-69.75) | 0.047 |
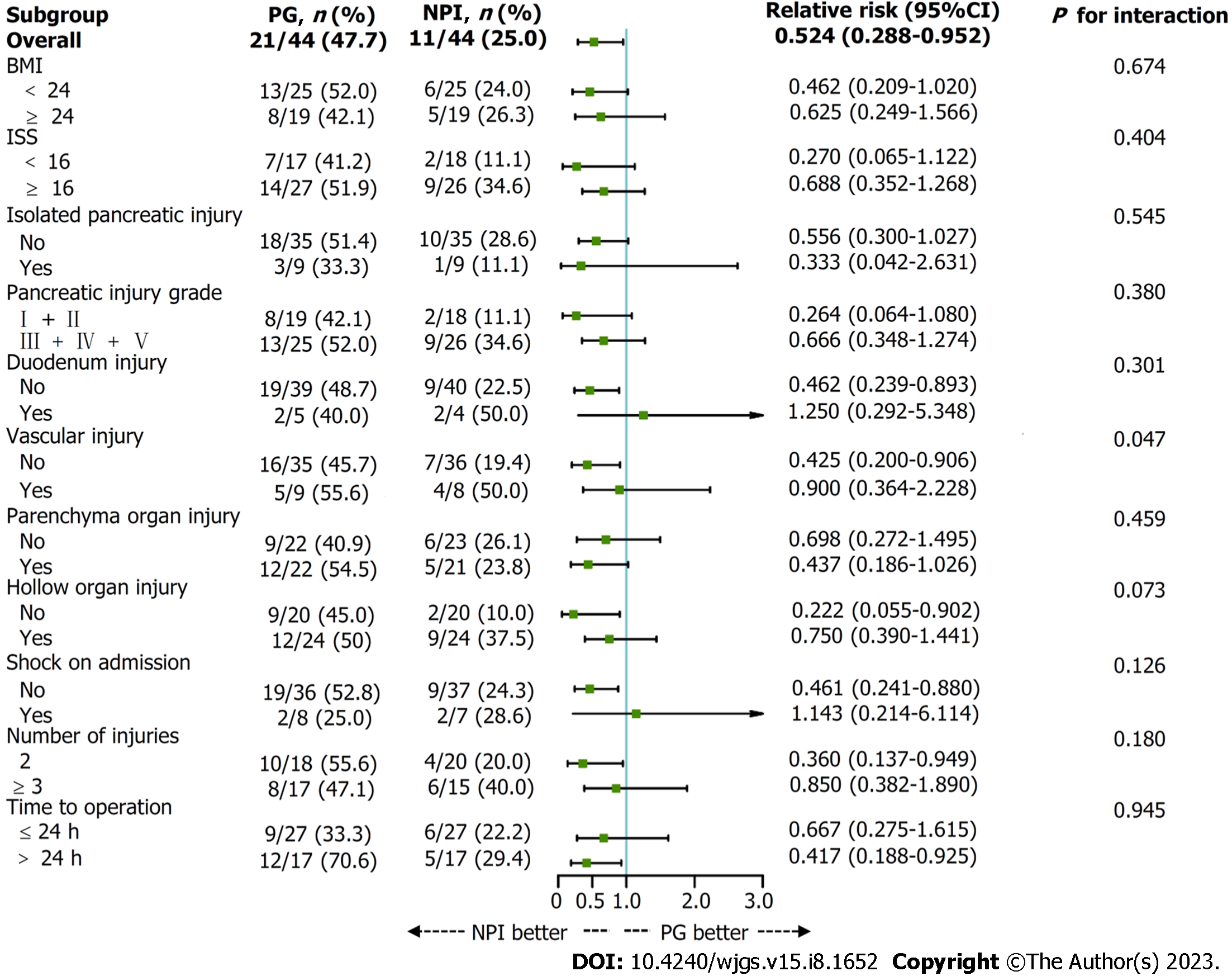
Among the matched cohort, no significant difference in in-hospital mortality was observed between the two groups. The drainage period in the NPI group was shorter than that in the PG group [median (inter-quartile range), 35.0 (20.0-54.75) vs 47.0 (30.0-68.0) d; P = 0.009]. The proportion of patients who underwent CT drainage in the NPI group was still significantly lower (15.9% vs 34.1%, P = 0.042). Moreover, the NPI group was associated with a lower incidence of pancreatic fistula grade B/C, a lower incidence of gastrointestinal fistulas, a lower reoperation rate, and a shorter LOS (P < 0.05) (Table 3). The POD 7 infection rate of drainage fluid in the NPI group was significantly lower [11/36 (30.6%) vs 27/43 (62.8%), P = 0.004] (Supplementary Table 3). With regard to the qualitative microbiological analysis, the incidence of G+ bacterial infection was higher in the NPI group [7/11 (63.6%) vs 5/27 (18.5%), P = 0.017] (Supplementary Table 4). In this prespecified subgroup analysis, the difference in the rate of the primary outcome between the PG and the NPI group was greater among patients without concomitant vascular injury (Figure 4). We detected no significant interactions of treatment with the other baseline factors P > 0.10 for all comparisons.
Few comparative studies have focused on the potential differences in the postoperative outcomes related to drain types for PT patients. Most western countries recommend closed suction drainage, but conclusive evidence is lacking[7-9,20]. The Memphis group found that closed suction drainage reduced septic complications, while sump drainage caused retrograde infections via catheters[21]. However, it is difficult to derive robust results from this study due to the heterogeneity of study participants, injury parameters, and operative procedures. In this study, we evaluated the severity of complications for different drain types after PT and found that NPI suction drainage is superior to PG drainage.
The reduced Clavien-Dindo severity for NPI suction drainage can be attributed to several factors. First, NPI suction drainage can effectively remove residual infection within intra-abdominal or between intestinal loops through continuous and active irrigation with sterile normal saline, thereby reducing the incidence of abscess, systemic inflammation or sepsis[22]. Second, NPI suction drainage can rapidly drain collected pancreatic juice by a low negative pressure system to reduce accumulation and diffusion, and it can dilute the accumulated fluid collection by irrigating sterile normal saline to minimize erosion and impairment to other tissues, thus preventing mild pancreatic leakage from developing into a serious pancreatic fistula and avoiding hemorrhage and the formation of gastrointestinal fistulas. Jiang et al[15] verified that pancreatic fistula grade C in patients with NPI suction drainage was significantly less common than in patients with passive drainage after pancreaticoduodenectomy. Under dual effects, NPI suction drainage could achieve significant clinical benefits for patients. PG drainage generally relies on the pressure difference and gravity, which might not obtain adequate drainage and predispose patients to catheter blockage. In this study, the incidence of catheter blockage was 9.6% (14/146) in the PG group, whereas it did not occur in the NPI group.
More importantly, postoperative digestive tract fistulas often contribute to various other complications, such as hemorrhage, sepsis, multisystem organ failure, and even death. These complications require reinterventions, such as percutaneous drainage or reoperation[23]. Nevertheless, resection and anastomoses should not be considered suitable procedures due to the edematous and friable nature of and adhesions adjacent to the fistula site. Fistulography is performed to evaluate the possibility of conservative treatment. For patients able to be treated conservatively, we uniformly adopted NPI suction drainage. The outer cannula can prevent both aspiration damage to surrounding tissues and blockage of the inner suction cannula. The patency provided by NPI suction drainage is a fundamental principle in the formation of a stable and controlled pancreaticocutaneous or enterocutaneous fistula, which is beneficial for facilitating the formation of the fistula tract[24].
In the matched cohort, the incidence of gastrointestinal fistulas and the reoperation rate were higher in the PG group. Sixteen patients required reoperation for one or more intra-abdominal complications: Intra-abdominal hemorrhage grade B/C in 10 patients, small intestinal fistulas in 3, colonic fistulas in 5, pancreatic fistula grade C in 2, and infectious pancreatic necrosis in 2. Correspondingly, 7 patients required reoperation in the NPI group, due to intra-abdominal hemorrhage grade B/C in 1 patient, gastric fistula in 1, colonic fistulas in 3, and pancreatic fistula grade C in 3. For patients who underwent CT-guided percutaneous drainage, the proportion in the NPI group was significantly smaller than that in the PG group. From the above, it can be determined that patients in the NPI group could undergo fewer invasive reinterventions. Our previous study also found that 74 of 88 gastric and small intestinal fistulas (84.1%) and 21 of 72 colonic fistulas (29.2%) caused by acute pancreatitis could be cured by NPI suction drainage[25]. Some studies have shown that negative pressure contributes by causing local tissue and vascular damage in the area near the drain[26]. However, Čečka et al[17] found that the rates of pancreatic fistula, hemorrhage and overall morbidity were not different between closed suction and PG drainage after pancreatic resection. According to the results of our study, low negative pressure did not raise the above concerns.
The overall mortality rate was 9.6% (19/196): 18 patients died of sepsis and related multiple organ failure. Similarly, the Western Trauma Association Multicenter Trials Group on Pancreatic Injuries found that the mortality was 9.1% (79/872) in PT patients who underwent surgery[11,12]. In our matched cohort, no significant differences in mortality were observed. These patients might benefit from good control of the infected source, and most digestive tract fistulas usually heal spontaneously over time[27]. In addition, the improvement of care capacity for severe trauma, parenteral and enteral nutritional support, and effective anti-infection treatment also played important roles.
The POD 7 infection rate of drainage fluid in the NPI suction drainage group was significantly lower; however, the incidence of infectious complications (abscess and sepsis) was not significantly different between the two drain types. This finding could be attributed to antibiotic administration and the application of percutaneous drainage. We speculate that the higher incidence of G+ bacterial infection with NPI suction drainage might be related to the open nature of the drain or retrograde migration of bacteria. Although subgroup analyses were prespecified, this study was not adequately powered to assess the benefit of treatment. Patients without concomitant vascular injury appeared to benefit more from NPI suction drainage than those with vascular injury. Nevertheless, with the limitations of a relatively small sample size and retrospective nature, caution should be exercised in the interpretation of these results.
Our study has several limitations. First, as an observational study, the analyses are subject to selection bias, and residual unmeasured confounding might persist despite adjustment for a variety of known patient variables using PSM to approximate randomization. Second, conducting the study at a single high-volume center limits its generalizability. Third, the volume, microbiology, amylase concentrations of drainage fluid, trends over time and drainage catheter removal time were not included in our data; however, they might also reflect the potential differences between the two drain types.
In conclusion, we compared the incidence of severe postoperative complications between the PG and NPI groups and found that NPI suction drainage was associated with decreased Clavien-Dindo severity. These findings suggest that initial NPI suction drainage could be recommended as a safe and effective alternative for managing complex PT patients. Further randomized, controlled trials are warranted to validate these results.
Consensus regarding the necessity for drainage has been formulated in the many management strategies for pancreatic trauma (PT).
Few studies have addressed the question of which drain types are more beneficial for PT patients.
To investigate whether sustained low negative pressure irrigation (NPI) suction drainage is superior to closed passive gravity (PG) drainage in PT patients.
We performed a retrospective cohort study of consecutive patients who underwent pancreatic surgery at a tertiary trauma referral center between January 2009 and October 2021 in our PT database. The primary outcome was defined as the occurrence of severe complications (Clavien-Dindo grade ≥ Ⅲb). Multivariable logistic regression was used to model the primary outcome, and propensity score matching (PSM) was included in the regression-based sensitivity analysis.
In this study, 146 patients underwent initial PG drainage, and 50 underwent initial NPI suction drainage. In the entire cohort, a multivariable logistic regression model showed that the adjusted risk for severe complications was decreased with NPI suction drainage [14/50 (28.0%) vs 66/146 (45.2%); odds ratio (OR), 0.437; 95% confidence interval (CI): 0.203-0.940]. After 1:1 PSM, 44 matched pairs were identified. The proportion of each operative procedure performed for pancreatic injury-related and other intra-abdominal organ injury-related cases was comparable in the matched cohort. NPI suction drainage still showed a lower risk for severe complications [11/44 (25.0%) vs 21/44 (47.7%); OR: 0.365; 95%CI: 0.148-0.901].
Initial NPI suction drainage could be recommended as a safe and effective alternative for managing complex PT patients.
Further randomized, controlled trials are warranted to validate these results.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kitamura K, Japan; Valek V, Czech Republic S-Editor: Lin C L-Editor: A P-Editor: Zhang YL
| 1. | Asensio JA, Petrone P, Ogun OA, Perez-Alonso AJ, Wagner M, Bertellotti R, Phillips BJ, Udekwu AO. Laparotomy: The conquering of the abdomen and the historical journey of pancreatic and duodenal injuries. J Trauma Acute Care Surg. 2016;80:1023-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Ayoob AR, Lee JT, Herr K, LeBedis CA, Jain A, Soto JA, Lim J, Joshi G, Graves J, Hoff C, Hanna TN. Pancreatic Trauma: Imaging Review and Management Update. Radiographics. 2021;41:58-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Wiik-Larsen J, Thorsen K, Sandve KO, Søreide K. Incidence and characteristics of pancreatic injuries among trauma patients admitted to a Norwegian trauma centre: a population-based cohort study. Scand J Gastroenterol. 2020;55:1347-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Linsenmaier U, Wirth S, Reiser M, Körner M. Diagnosis and classification of pancreatic and duodenal injuries in emergency radiology. Radiographics. 2008;28:1591-1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Ho VP, Patel NJ, Bokhari F, Madbak FG, Hambley JE, Yon JR, Robinson BR, Nagy K, Armen SB, Kingsley S, Gupta S, Starr FL, Moore HR 3rd, Oliphant UJ, Haut ER, Como JJ. Management of adult pancreatic injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82:185-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 107] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 6. | Yang C, Wang X, Wu C, Wang Y, Wang K, Ding W. A case-control study of risk factors for survival after laparotomy in patients with pancreatic trauma. Asian J Surg. 2022;45:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Uchida K, Hagawa N, Miyashita M, Maeda T, Kaga S, Noda T, Nishimura T, Yamamoto H, Mizobata Y. How to deploy a uniform and simplified acute-phase management strategy for traumatic pancreatic injury in any situation. Acute Med Surg. 2020;7:e502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Biffl WL, Moore EE, Croce M, Davis JW, Coimbra R, Karmy-Jones R, McIntyre RC Jr, Moore FA, Sperry J, Malhotra A, Feliciano D. Western Trauma Association critical decisions in trauma: management of pancreatic injuries. J Trauma Acute Care Surg. 2013;75:941-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Sharpe JP, Magnotti LJ, Weinberg JA, Zarzaur BL, Stickley SM, Scott SE, Fabian TC, Croce MA. Impact of a defined management algorithm on outcome after traumatic pancreatic injury. J Trauma Acute Care Surg. 2012;72:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Büchler MW, Friess H. Evidence forward, drainage on retreat: still we ignore and drain!? Ann Surg. 2006;244:8-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Biffl WL, Ball CG, Moore EE, Lees J, Todd SR, Wydo S, Privette A, Weaver JL, Koenig SM, Meagher A, Dultz L, Udekwu PO, Harrell K, Chen AK, Callcut R, Kornblith L, Jurkovich GJ, Castelo M, Schaffer KB; WTA Multicenter Trials Group on Pancreatic Injuries. Don't mess with the pancreas! A multicenter analysis of the management of low-grade pancreatic injuries. J Trauma Acute Care Surg. 2021;91:820-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Biffl WL, Zhao FZ, Morse B, McNutt M, Lees J, Byerly S, Weaver J, Callcut R, Ball CG, Nahmias J, West M, Jurkovich GJ, Todd SR, Bala M, Spalding C, Kornblith L, Castelo M, Schaffer KB, Moore EE; WTA Multicenter Trials Group on Pancreatic Injuries. A multicenter trial of current trends in the diagnosis and management of high-grade pancreatic injuries. J Trauma Acute Care Surg. 2021;90:776-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Gachabayov M, Gogna S, Latifi R, Dong XD. Passive drainage to gravity and closed-suction drainage following pancreatoduodenectomy lead to similar grade B and C postoperative pancreatic fistula rates. A meta-analysis. Int J Surg. 2019;67:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Tong Z, Ke L, Li B, Li G, Zhou J, Shen X, Li W, Li N, Li J. Negative pressure irrigation and endoscopic necrosectomy through man-made sinus tract in infected necrotizing pancreatitis: a technical report. BMC Surg. 2016;16:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Jiang H, Liu N, Zhang M, Lu L, Dou R, Qu L. A Randomized Trial on the Efficacy of Prophylactic Active Drainage in Prevention of Complications after Pancreaticoduodenectomy. Scand J Surg. 2016;105:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | He S, Xia J, Zhang W, Lai M, Cheng N, Liu Z, Cheng Y. Prophylactic abdominal drainage for pancreatic surgery. Cochrane Database Syst Rev. 2021;12:CD010583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Čečka F, Jon B, Skalický P, Čermáková E, Neoral Č, Loveček M. Results of a randomized controlled trial comparing closed-suction drains vs passive gravity drains after pancreatic resection. Surgery. 2018;164:1057-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Correa-Gallego C, Brennan MF, Dʼangelica M, Fong Y, Dematteo RP, Kingham TP, Jarnagin WR, Allen PJ. Operative drainage following pancreatic resection: analysis of 1122 patients resected over 5 years at a single institution. Ann Surg. 2013;258:1051-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 19. | Čečka F, Loveček M, Jon B, Skalický P, Šubrt Z, Neoral Č, Ferko A. Intra-abdominal drainage following pancreatic resection: A systematic review. World J Gastroenterol. 2015;21:11458-11468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (2)] |
| 20. | Iacono C, Zicari M, Conci S, Valdegamberi A, De Angelis M, Pedrazzani C, Ruzzenente A, Guglielmi A. Management of pancreatic trauma: A pancreatic surgeon's point of view. Pancreatology. 2016;16:302-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Fabian TC, Kudsk KA, Croce MA, Payne LW, Mangiante EC, Voeller GR, Britt LG. Superiority of closed suction drainage for pancreatic trauma. A randomized, prospective study. Ann Surg. 1990;211:724-8; discussion 728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Li J, Ren J, Zhu W, Yin L, Han J. Management of enterocutaneous fistulas: 30-year clinical experience. Chin Med J (Engl). 2003;116:171-175. [PubMed] |
| 23. | Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, Vollmer C, Velanovich V, Riall T, Muscarella P, Trevino J, Nakeeb A, Schmidt CM, Behrns K, Ellison EC, Barakat O, Perry KA, Drebin J, House M, Abdel-Misih S, Silberfein EJ, Goldin S, Brown K, Mohammed S, Hodges SE, McElhany A, Issazadeh M, Jo E, Mo Q, Fisher WE. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 2014;259:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 273] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 24. | Kong X, Cao Y, Yang D, Zhang X. Continuous irrigation and suction with a triple-cavity drainage tube in combination with sequential somatostatin-somatotropin administration for the management of postoperative high-output enterocutaneous fistulas: Three case reports and literature review. Medicine (Baltimore). 2019;98:e18010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Jiang W, Tong Z, Yang D, Ke L, Shen X, Zhou J, Li G, Li W, Li J. Gastrointestinal Fistulas in Acute Pancreatitis With Infected Pancreatic or Peripancreatic Necrosis: A 4-Year Single-Center Experience. Medicine (Baltimore). 2016;95:e3318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 26. | Grobmyer SR, Graham D, Brennan MF, Coit D. High-pressure gradients generated by closed-suction surgical drainage systems. Surg Infect (Larchmt). 2002;3:245-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Hua Z, Su Y, Huang X, Zhang K, Yin Z, Wang X, Liu P. Analysis of risk factors related to gastrointestinal fistula in patients with severe acute pancreatitis: a retrospective study of 344 cases in a single Chinese center. BMC Gastroenterol. 2017;17:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Li Y, Li PY, Sun SJ, Yao YZ, Li ZF, Liu T, Yang F, Zhang LY, Bai XJ, Huo JS, He WB, Ouyang J, Peng L, Hu P, Zhu YA, Jin P, Shao QF, Wang YF, Dai RW, Hu PY, Chen HM, Wang GF, Wang YG, Jin HX, Zhu CJ, Zhang QY, Shao B, Sang XG, Yin CL. Chinese Trauma Surgeon Association for management guidelines of vacuum sealing drainage application in abdominal surgeries-Update and systematic review. Chin J Traumatol. 2019;22:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |