Published online Jul 27, 2023. doi: 10.4240/wjgs.v15.i7.1286
Peer-review started: January 20, 2023
First decision: March 8, 2023
Revised: March 8, 2023
Accepted: May 5, 2023
Article in press: May 5, 2023
Published online: July 27, 2023
Processing time: 182 Days and 2.5 Hours
Hepatic portal blood flow occlusion is a common technique for reducing hepatic hemorrhage during hepatectomy. We designed a novel Y-Z magnetic hepatic portal blocking band (Y-Z MHPBB) based on the principle of magnetic compression technique.
To introduce the Y-Z MHPBB device and verify the feasibility of this device for hepatic portal blood flow occlusion in dogs.
Ten beagles were randomly divided into the experimental group and control group. The operation time, intraoperative blood loss, the number of portal blood flow occlusions, the total time spent on adjusting the blocking band, and the average time spent on adjusting the blocking band were recorded. The surgeons evaluated the feasibility and flexibility of the two portal occlusion devices.
Laparoscopic hepatectomy was successfully performed in both the experimental group and control group. There was no statistical difference between the two groups in the operation time, intraoperative blood loss, and the number of hepatic portal blood flow occlusions. With respect to the total time spent on adjusting the blocking band and the average time spent on adjusting the blocking band, the experimental group showed significantly better outcomes than the control group, with a statistical difference (P < 0.05). The operators found that the Y-Z MHPBB was superior to the modified T-tube in terms of operational flexibility.
The Y-Z MHPBB seems to be an ingenious design, accurate blood flow occlusion effect, and good flexibility; and it can be used for hepatic portal blood flow occlusion during laparoscopic hepatectomy.
Core Tip: Based on the basic principle of magnetic compression technique, we designed a novel Y-Z magnetic hepatic portal blocking band (Y-Z MHPBB) and compared it with a modified T tube through animal experiments. Mechanical tests and in vitro simulation experiments showed that Y-Z MHPBB has good fluid shielding performance. The animal experiment results showed that the device has good flexibility and convenience under laparoscopy. Y-Z MHPBB seems to have broad application prospects in the clinical field.
- Citation: Zhang MM, Li CG, Xu SQ, Mao JQ, Ren YX, Zhang YH, Ma J, Shi AH, Lyu Y, Yan XP. Primary animal experiment to test the feasibility of a novel Y-Z magnetic hepatic portal blocking band. World J Gastrointest Surg 2023; 15(7): 1286-1293
- URL: https://www.wjgnet.com/1948-9366/full/v15/i7/1286.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i7.1286
Hepatic portal blood flow occlusion is an important technique to effectively reduce hepatic hemorrhage during hepatectomy[1]. At present, during clinical hepatectomy, one end of the cotton tape is often inserted from the left side of the hepatoduodenal ligament and passed through the foramen of Winslow, and the two ends of the cotton tape are passed through the rubber tube. The blood flow into the liver (hepatic artery and portal vein blood flow) can be effectively blocked when the cotton tape is tightened with a rubber tube as a support[2]. The materials used in this method can be easily obtained, and they are low in cost, simple in operation, and reliable in their effect. This method is mainly used in open hepatectomy. However, when used under laparoscopy, its flexibility is greatly reduced, and the existing port needs to be occupied or a new port needs to be established in the abdominal wall. Some surgeons use a rubber tube sheared by scissors from the rim of a surgical glove combined with Hem-o-lok for laparoscopic hepatic portal blood flow occlusion[3]; however, it is effective but not flexible. Thus, there is an urgent clinical need to design a laparoscopic hepatic portal blood flow occlusion device that has good flexibility and does not occupy the abdominal wall port.
Magnetosurgery/Magnetic surgery is a new clinical technique that has developed rapidly in recent years[4]. Magnetic devices designed based on the principle of magnet homopolar repulsion and heteropolar attraction offer great advantages in open surgery, laparoscopic surgery, and endoscopic surgery[5-7]. Magnetic compression technique is the most important clinical application field in the magnetosurgical system. The use of magnetic compression technique can achieve sutureless vascular anastomosis[8-11], digestive tract anastomosis[12-17], therapeutic management of fistula[18] and pathological fistula[19]. Thus, in this study, we aimed to design a novel Y-Z magnetic hepatic portal blocking band (Y-Z MHPBB) for laparoscopic hepatectomy based on the principle of magnetic compression technique, and to test the magnetic parameters and explore the feasibility of its application through animal experiments.
The study protocol and all experimental procedures were carried out strictly in accordance with the Guidelines for Care and Use of Experimental Animals issued by the Xi’an Jiaotong University Medical Center. This experimental study was approved by the Experimental Ethics Committee of Xi’an Jiaotong University (Permit number: 2022-1460). Ten experimental dogs were used as animal models in order to follow the “3R” principle (Reduction, Refinement and Replacement) for animal experiments and reduce the use of experimental animals.
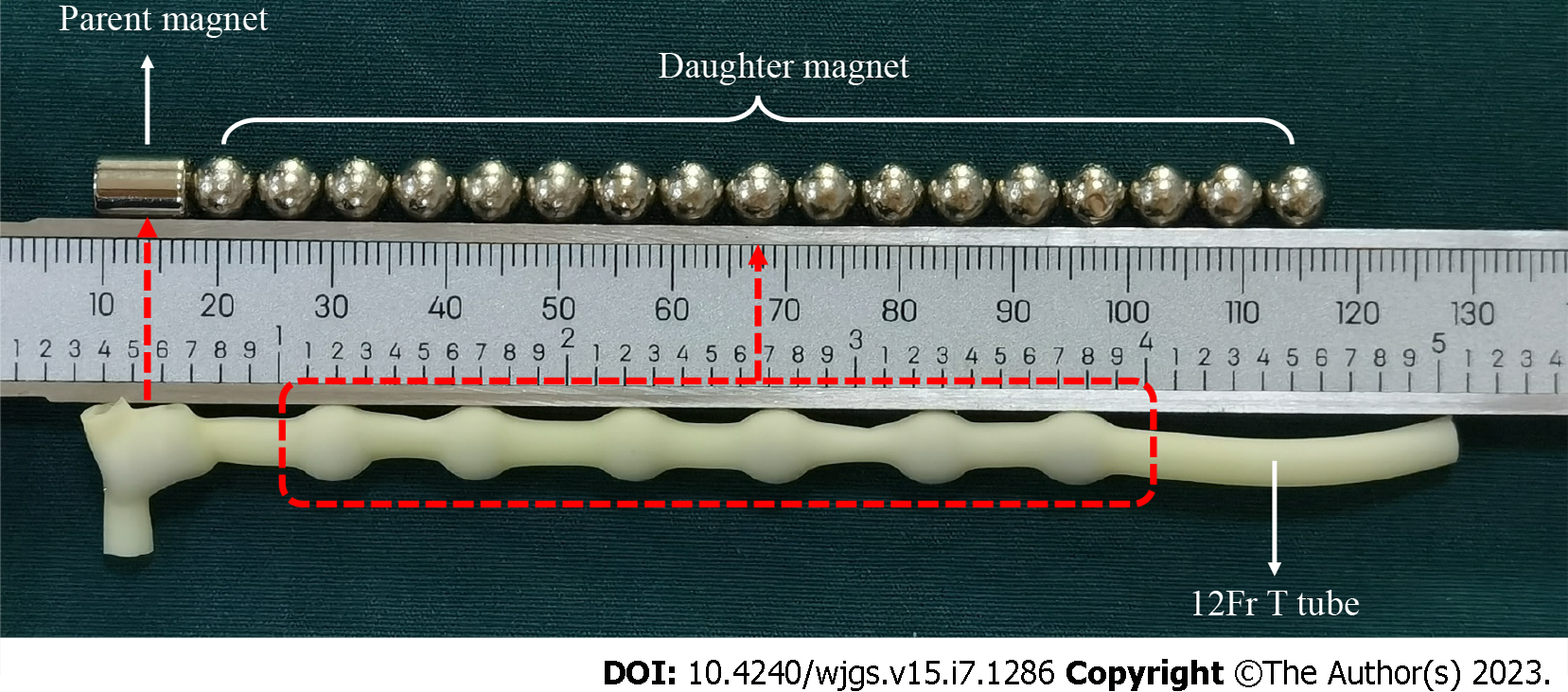
Y-Z MHPBB was prepared by embedding a series of magnets arranged in a specific order and polarity into a rubber tube. A cylindrical parent magnet was placed at the head end, and spherical daughter magnets arranged at intervals were placed along the head end to the tail end. The parent magnet was a cylindrical magnet with a diameter of 6 mm and a height of 8 mm, and the daughter magnet was a spherical magnet with a diameter of 6 mm. Both the daughter and parent magnets were made of N45 sintered NdFeB (29%-32.5% neodymium, 63.95%-68.65% ferrum, 1.1%-1.2% boron); the parent magnet was axially magnetized, and the daughter magnet was magnetized in a single direction. The mass of the parent magnet was 1.70 g, and the magnetic flux density at both ends was 5420 GS (1T = 10000 GS); the mass of the daughter magnet was 0.84 g, and the magnetic flux density at the two poles was 4110 GS. The rubber tube specification was 12Fr. Figure 1 shows the Y-Z MHPBB.
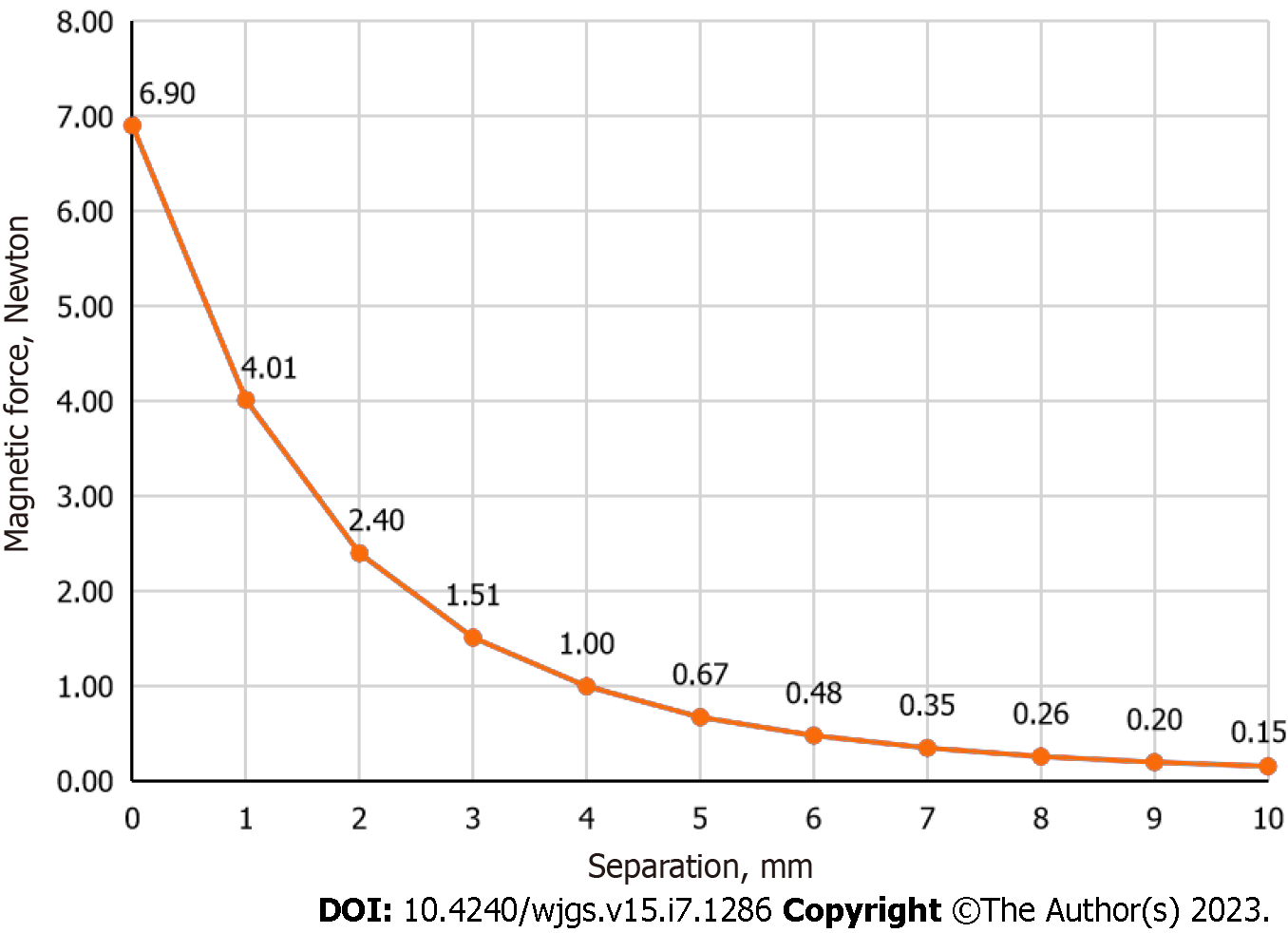
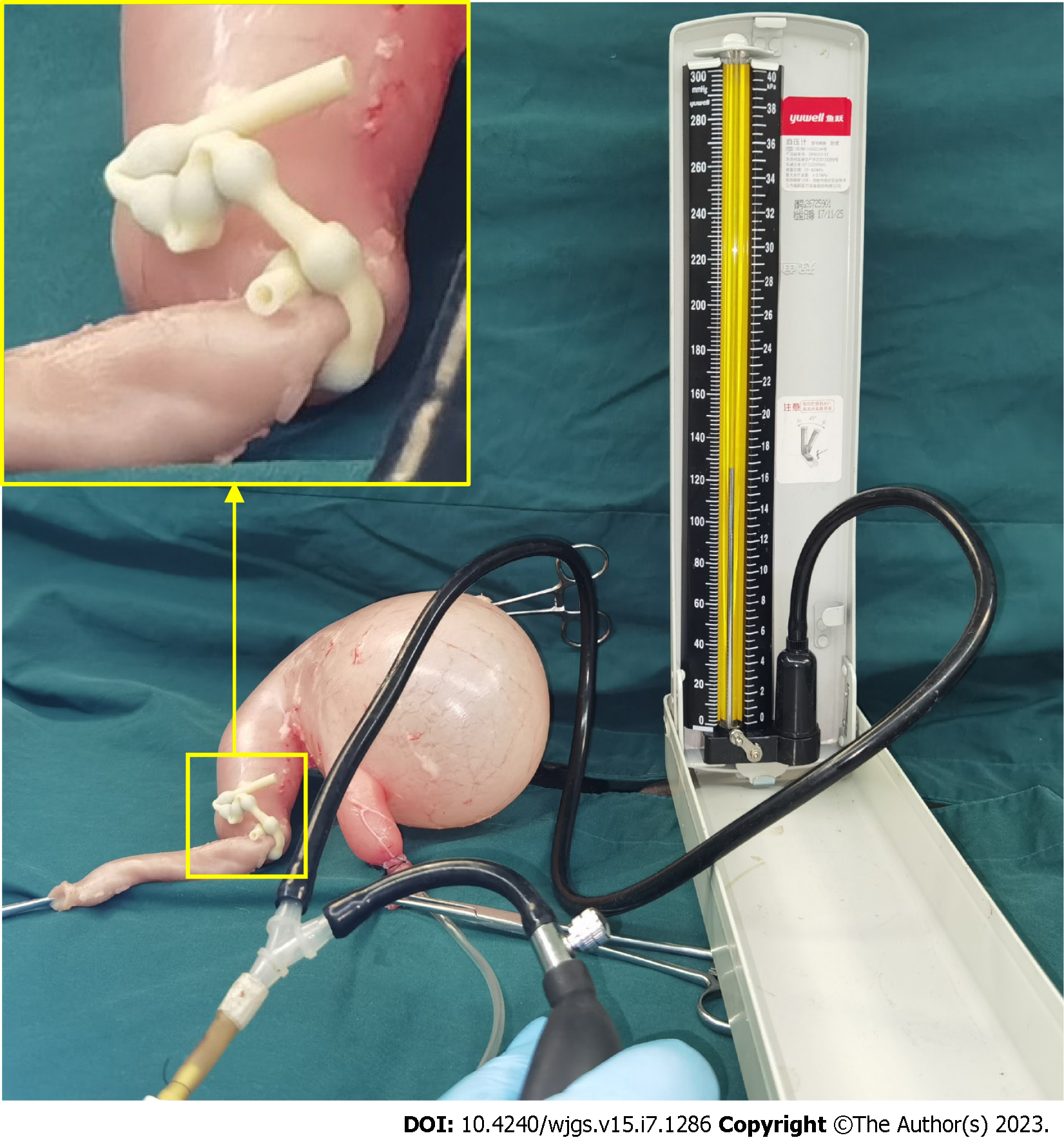
The test results of the electronic universal testing machine showed that the magnetic force of the parent and daughter magnets at zero distance was the largest at 6.90 Newtons. The magnetic force-displacement curve of the parent and daughter magnets is shown in Figure 2. The isolated stomach and duodenum (about 15 cm) of dogs was obtained and fixed on the experimental table, and Y-Z MHPBB was loaded at the junction of the stomach and duodenum. The duodenal side was open, and the esophageal side was connected to a catheter and a pressure measuring device. The catheter was gradually filled with gas to test the occlusion pressure of Y-Z MHPBB. The results showed that the occlusion pressure of the device to gas was 152 mmHg (Figure 3).
Ten beagle dogs (weight, 10-12 kg; male = 5, female = 5) were purchased from the Laboratory Animal Center of Xi'an Jiaotong University (Xi’an China). The animals were acclimatized to laboratory conditions (23 ℃, 12 h/12 h light/dark, 50% humidity, and ad libitum access to food and water) for one week prior to commencing the experiments. The animal protocol was designed to minimize the discomfort to animals. The beagles were randomly divided into the experimental group (n = 5) and control group (n = 5). Five liver surgeons performed laparoscopic hepatectomy. Each expert performed one operation in the experimental group and control group. In the experimental group, Y-Z MHPBB was used for hepatic portal blood flow occlusion; in the control group, a modified T tube was used for hepatic portal blood flow occlusion.
After fasting for 12 h, the beagles were weighed and then anesthetized using intravenous anesthesia by injection of 3% pentobarbital sodium solution (1 mL/kg).
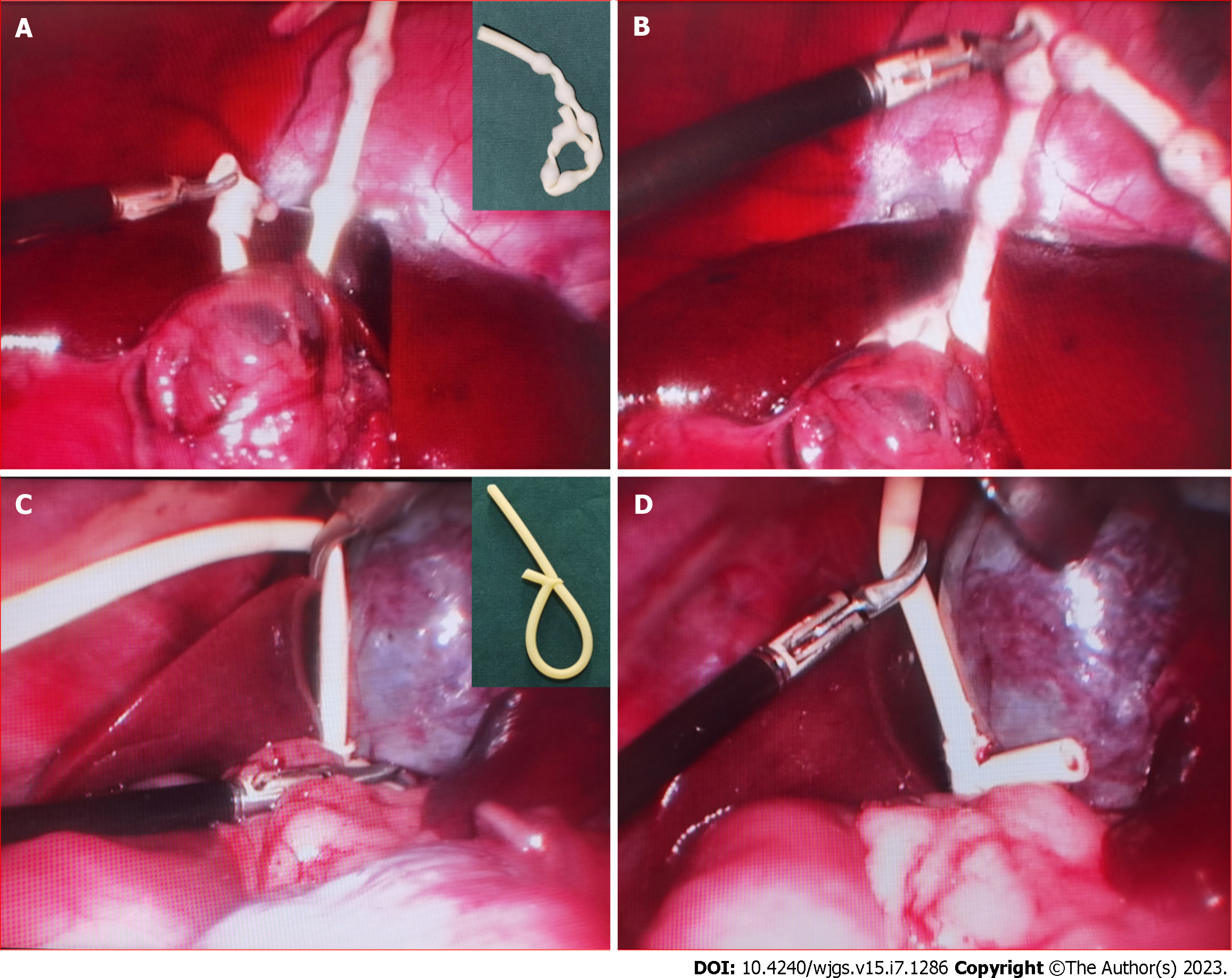
After successful anesthesia, the experimental dogs were fixed in a supine position, and tracheal intubation and ventilator-assisted ventilation were performed. A 10 mm trocar was placed under the umbilicus, and the laparoscopic light source and camera system were introduced. Further, 5 mm and 12 mm ports were placed on the right upper abdomen, and 10 mm and 5 mm ports were placed on the left upper abdomen. Adjustment was made to a slightly higher position on the head and left side to explore the abdominal cavity and liver. The pneumoperitoneum pressure was 12 mmHg. The falciform ligament, left coronary ligament, and left deltoid ligament were disconnected. A non-injured forceps reached the lesser omental mesh through the ventral side of the left hepatoduodenal ligament, the lesser omentum was opened to expose the head end of the non-injured forceps, and the hepatic portal blocking band was placed for use. After marking the incision line with an electric hook, the liver capsule and superficial liver parenchyma were opened with an ultrasonic scalpel. The surgeon could block the portal blood flow at any time, as needed. The smaller branches were clipped with titanium clips and then cut off. The larger branches were clipped with vascular clips, and the left lateral lobe and left median lobe of the liver were successfully and completely removed. Figure 4 shows the hepatic portal blood flow occlusion band during the operation in the experimental group and control group.
The experimental dogs were given drinking water at 6 h after recovery from anesthesia, and they were free to eat after 1 d. During the first 3 d after surgery, intramuscular pethidine (1 mg/kg) was injected every 12 h. The mental state, eating, and activity of each dog were observed daily after the operation, and the observation end point was 2 wk after the operation.
Observation and analysis indicators included the following: Operation time, intraoperative blood loss, the number of portal blood flow occlusions, the total time spent on adjusting the blocking band, and the average time spent on adjusting the blocking band. The surgeon evaluated the feasibility and flexibility of the two hepatic portal blood flow occlusion devices.
SPSS 20.0 software was used for statistical analysis. Measurement data with normal distribution were expressed as mean ± SD, and measurement data with skewed distribution were expressed as median.
All beagles in this study successfully underwent laparoscopic left lateral lobe and left median lobe liver resection. None of the dogs died during the perioperative period. The operation time in the experimental group was slightly shorter than that in the control group (98.2 ± 19.77 min vs 107.4 ± 12.99 min), but there was no statistical difference (P = 0.410). There was no statistical difference in the intraoperative blood loss between the experimental group and control group (42 ± 8.37 mL vs 40 ± 7.91 mL; P = 0.708). Further, there was no significant difference in the number of hepatic portal blood flow occlusions between the experimental group and control group (P = 0.729). There was a statistical difference in the total time spent on adjusting the blocking band between the experimental group and control group (2.5 ± 1.12 min vs 5.9 ± 1.78 min; P = 0.007). Further analysis showed that there was a statistical difference in the average time spent on adjusting the blocking band between the experimental group and control group (1.12 ± 0.16 min vs 2.43 ± 0.31 min; P = 0.008). Detailed results are presented in Table 1.
| Outcomes | Experimental group (n = 5) | Control group (n = 5) | P value |
| Operation time (min) | 98.2 ± 19.77 | 107.4 ± 12.99 | 0.410 |
| Intraoperative blood loss (mL) | 42 ± 8.37 | 40 ± 7.91 | 0.708 |
| Number of hepatic portal blood flow occlusions | 2.2 ± 0.83 | 2.4 ± 0.54 | 0.729 |
| Total time spent on adjusting the blocking band (min) | 2.5 ± 1.12 | 5.9 ± 1.78 | 0.007 |
| Average time spent on adjusting the blocking band (min) | 1.12 ± 0.16 | 2.43 ± 0.31 | 0.008 |
Five senior hepatobiliary surgeons evaluated the two hepatic portal blood flow occlusion devices. Both devices could meet the need of surgery only in terms of reducing hemorrhage in the liver section. However, when operational flexibility was considered, all five experts believed that flexibility of the Y-Z MHPBB was better than that of the modified T tube. It was also observed that when a specialist performed the operation in the control group, the initially modified T tube was not suitable for use and had to be remodified once.
Reasonable control of blood flow into the liver is the key to prevent massive hemorrhage during laparoscopic hepatectomy. Laparoscopic hepatic portal blood flow occlusion methods include intra-abdominal and extra-abdominal occlusion. Extra-abdominal hepatic portal blood flow occlusion offers advantages, such as simple operation, easy control, and accurate occlusion effect[20,21], but it also has a disadvantage as an additional abdominal wall port is required or the existing abdominal wall port is occupied. At the same time, the blocking band occupies the area of the operative field for a long time, which sometimes interferes with laparoscopic surgery. The intra-abdominal occlusion method can effectively avoid the shortcomings of the extra-abdominal occlusion method, but its flexibility is poor and sometimes it may increase the need for medical consumables. In the past, our team modified the T-tube for use in intra-abdominal portal hepatic blood flow occlusion, which can effectively reduce the need for medical consumables. The blood flow occlusion effect is reliable, but the flexibility is insufficient.
In 2013, the New England Journal of Medicine published the research results of Ganz et al[22] regarding the use of magnetic devices for the treatment of gastroesophageal reflux disease[22]. This novel magnetic device can effectively restrain the opening and closing of the lower end of the esophagus, thereby preventing gastric reflux. This is a typical example of flexible use of magnetic surgical techniques. The design concept of Y-Z MHPBB is similar to that of the LINX reflux management system. The Y-Z MHPBB uses elasticity of the rubber tube to constrain the hepatic hilum, and the magnetic force between the parent and daughter magnets to lock and release the rubber tube.
Compared with other intra-abdominal hepatic portal blood flow occlusion devices, Y-Z MHPBB offers the following advantages: (1) It is convenient to obtain the materials, simple to manufacture, has a low cost (about $5) and disposable. Rubber tubes and magnetic balls are common items, and it is only necessary to insert the magnets into the rubber tube in turn, and they can be used clinically after ethylene oxide sterilization; (2) The operational flexibility is good; and the laparoscopic instrument can conveniently achieve attraction and separation of the parent magnet and daughter magnet during use, and shorten the operation time. In the control group, T-tube modification was generally carried out by the surgeon during the operation. In the process of trimming the T-tube, the size of the restraint hole should be appropriate. If the restraint hole is too large, the friction force will be small, which will ultimately affect the blood flow occlusion effect. If the restraint hole is too small, the friction force will be large, which will ultimately reduce the operational flexibility; and (3) Y-Z MHPBB is an intra-abdominal porta hepatis blocking device, which does not occupy the already established port of the abdominal wall and does not require additional puncture holes, thus avoiding increased abdominal wall trauma.
In this study, the five experts gave high recognition to Y-Z MHPBB and considered that this device has clinical application value. However, one of the experts pointed out that the magnets in the Y-Z MHPBB may slightly interfere with the laparoscopic instruments. The other four experts believed that there is a certain attraction between the magnet and the operating instrument, but this effect can be completely eliminated by using a proper surgical technique.
In conclusion, mechanical tests and in vitro simulation experiments showed that the Y-Z MHPBB has good fluid occlusion properties. The results of animal experiments also showed that the device offers excellent flexibility and convenience under laparoscopy. We believe that the Y-Z MHPBB has broad application prospects in the clinical field.
Hepatic portal blood flow occlusion is an important technique to effectively reduce hepatic hemorrhage during hepatectomy, but the existing hepatic portal blocking band has poor operational flexibility in laparoscopic hepatectomy.
The design of a flexible hepatic portal blocking band is helpful for laparoscopic hepatectomy.
To design the magnetic hepatic portal blocking band (MHPBB) and verify the feasibility of this device for hepatic portal blood flow occlusion in laparoscopic hepatectomy.
The feasibility of MHPBB in laparoscopic hepatectomy was verified in experimental dogs.
The study showed that the Y-Z MHPBB was superior to the modified T-tube in terms of operational flexibility.
The Y-Z MHPBB can be used for hepatic portal blood flow occlusion during laparoscopic hepatectomy in clinic.
Animal experiments show that Y-Z MHPBB has a good effect, which can be applied in clinic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Martín Del Olmo JC, Spain; Suda T, Japan S-Editor: Fan JR L-Editor: A P-Editor: Xu ZH
| 1. | Scatton O, Zalinski S, Jegou D, Compagnon P, Lesurtel M, Belghiti J, Boudjema K, Lentschener C, Soubrane O. Randomized clinical trial of ischaemic preconditioning in major liver resection with intermittent Pringle manoeuvre. Br J Surg. 2011;98:1236-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Giordano M, Lopez-Ben S, Codina-Barreras A, Pardina B, Falgueras L, Torres-Bahi S, Albiol M, Castro E, Figueras J. Extra-Glissonian approach in liver resection. HPB (Oxford). 2010;12:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Cai J, Zheng J, Xie Y, Kirih MA, Jiang G, Liang Y, Liang X. A novel simple intra-corporeal Pringle maneuver for laparoscopic hemihepatectomy: how we do it. Surg Endosc. 2020;34:2807-2813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Yan XP, Shang P, Shi AH, Liu WY, Liu YX, Lv Y. [Exploration and establishment of magnetic surgery]. Kexue Tongbao. 2019;64:815-826. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Zhang M, Ji L, Chang K, Wang Y, Lyu Y, Yan X. A novel micromagnetic ring used for biliary-enteric anastomosis in rats. J Pediatr Surg. 2022;57:451-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Rivas H, Robles I, Riquelme F, Vivanco M, Jiménez J, Marinkovic B, Uribe M. Magnetic Surgery: Results From First Prospective Clinical Trial in 50 Patients. Ann Surg. 2018;267:88-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Matsuzaki I, Hattori M, Yamauchi H, Goto N, Iwata Y, Yokoi T, Tsunemi M, Kobayashi M, Yamamura T, Miyahara R. Magnetic anchor-guided endoscopic submucosal dissection for colorectal tumors (with video). Surg Endosc. 2020;34:1012-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Obora Y, Tamaki N, Matsumoto S. Nonsuture microvascular anastomosis using magnet rings: preliminary report. Surg Neurol. 1978;9:117-120. [PubMed] |
| 9. | Filsoufi F, Farivar RS, Aklog L, Anderson CA, Chen RH, Lichtenstein S, Zhang J, Adams DH. Automated distal coronary bypass with a novel magnetic coupler (MVP system). J Thorac Cardiovasc Surg. 2004;127:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Charitou A, Panesar SS, DeL Stanbridge R, Athanasiou T. Novel use of a magnetic coupling device to repair damage of the internal thoracic artery. J Card Surg. 2006;21:89-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Zhang M, Ma J, An Y, Lyu Y, Yan X. Construction of an intrahepatic portosystemic shunt using the magnetic compression technique: preliminary experiments in a canine model. Hepatobiliary Surg Nutr. 2022;11:611-615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Sterlin A, Evans L, Mahler S, Lindner A, Dickmann J, Heimann A, Sahlabadi M, Aribindi V, Harrison MR, Muensterer OJ. An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J Pediatr Surg. 2022;57:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Watanabe R, Barberio M, Kanaji S, Lapergola A, Ashoka AH, Andreiuk B, Guerriero L, Pizzicannella M, Seeliger B, Saida Y, Kaneko H, Worreth M, Saadi A, Marescaux J, Klymchenko AS, Diana M. Hybrid fluorescent magnetic gastrojejunostomy: an experimental feasibility study in the porcine model and human cadaver. Surg Endosc. 2020;34:1393-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Schlottmann F, Ryou M, Lautz D, Thompson CC, Buxhoeveden R. Sutureless Duodeno-Ileal Anastomosis with Self-Assembling Magnets: Safety and Feasibility of a Novel Metabolic Procedure. Obes Surg. 2021;31:4195-4202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Ore AS, Askenasy E, Ryou M, Baldwin T, Thompson CC, Messaris E. Evaluation of sutureless anastomosis after ileostomy takedown using the self-forming magnet anastomosis system in a porcine model. Surg Endosc. 2022;36:7664-7672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 16. | Jang SI, Lee KH, Yoon HJ, Lee DK. Treatment of completely obstructed benign biliary strictures with magnetic compression anastomosis: follow-up results after recanalization. Gastrointest Endosc. 2017;85:1057-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Kamada T, Ohdaira H, Takeuchi H, Takahashi J, Ito E, Suzuki N, Narihiro S, Yoshida M, Yamanouchi E, Suzuki Y. New Technique for Magnetic Compression Anastomosis Without Incision for Gastrointestinal Obstruction. J Am Coll Surg. 2021;232:170-177.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression ostomy as new cystostomy technique in the rat: magnacystostomy. Urology. 2012;79:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Gao Y, Wu RQ, Lv Y, Yan XP. Novel magnetic compression technique for establishment of a canine model of tracheoesophageal fistula. World J Gastroenterol. 2019;25:4213-4221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 20. | Zhang Y, Yang H, Deng X, Chen Y, Zhu S, Kai C. Intermittent Pringle maneuver versus continuous hemihepatic vascular inflow occlusion using extra-glissonian approach in laparoscopic liver resection. Surg Endosc. 2016;30:961-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Rotellar F, Pardo F, Benito A, Martí-Cruchaga P, Zozaya G, Pedano N. A novel extra-glissonian approach for totally laparoscopic left hepatectomy. Surg Endosc. 2012;26:2617-2622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Ganz RA, Peters JH, Horgan S, Bemelman WA, Dunst CM, Edmundowicz SA, Lipham JC, Luketich JD, Melvin WS, Oelschlager BK, Schlack-Haerer SC, Smith CD, Smith CC, Dunn D, Taiganides PA. Esophageal sphincter device for gastroesophageal reflux disease. N Engl J Med. 2013;368:719-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 202] [Article Influence: 16.8] [Reference Citation Analysis (0)] |