Published online Sep 27, 2021. doi: 10.4240/wjgs.v13.i9.988
Peer-review started: March 22, 2021
First decision: May 13, 2021
Revised: May 17, 2021
Accepted: August 10, 2021
Article in press: August 10, 2021
Published online: September 27, 2021
Processing time: 180 Days and 6.5 Hours
Enteric anastomotic (EA) bleeding is a potentially life-threatening surgical complication associated with enteric anastomosis during simultaneous pancreas and kidney transplantation (SPKT).
To investigate whether suture ligation (SL) for submucosal hemostasis during hand-sewn enteric anastomosis could decrease the morbidity of early EA bleeding in SPKT.
We compared the outcomes of 134 patients classified into SL (n = 44) and no SL (NSL) groups (n = 90). This study adheres to the declarations of Istanbul and Helsinki and all donors were neither paid nor coerced.
During the first postoperative week, the EA bleeding rate in the SL group was lower than that in the NSL group (2.27% vs 15.56%; P = 0.021); no relationship was found between EA bleeding and donor age, mean pancreatic cold ischemia time, platelet count, prothrombin time international normalized rate, activated partial thromboplastin time, and thrombin time. Anastomotic leakage was observed in one case in the SL group at postoperative day (POD) 14 and in one case at POD 16 in the NSL group (P = 0.754). No significant difference was found between the two groups in the patient survival, pancreas graft survival, or kidney graft survival.
SL for submucosal hemostasis during hand-sewn enteric anastomosis in SPKT can decrease the morbidity of early EA bleeding without increasing the anastomotic leakage rate.
Core Tip: Enteric anastomotic (EA) bleeding is a potentially life-threatening complication of simultaneous pancreas and kidney transplantation (SPKT) and can result in graft loss; therefore, it is essential to lower the incidence of EA bleeding. This study aimed to investigate whether suture ligation for submucosal hemostasis during enteric anastomosis could decrease the morbidity of early EA bleeding in SPKT. By comparing the outcomes of patients of suture ligation and no suture ligation groups, we found that suture ligation for submucosal hemostasis during enteric anastomosis in SPKT can decrease the morbidity of early EA bleeding without concurrently increasing the anastomotic leakage rate.
- Citation: Wang H, Fu YX, Song WL, Mo CB, Feng G, Zhao J, Pei GH, Shi XF, Wang Z, Cao Y, Nian YQ, Shen ZY. Suture ligation for submucosal hemostasis during hand-sewn side-to-side duodeno-ileostomy in simultaneous pancreas and kidney transplantation. World J Gastrointest Surg 2021; 13(9): 988-999
- URL: https://www.wjgnet.com/1948-9366/full/v13/i9/988.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i9.988
Pancreas transplantation is the treatment of choice for patients with type 1 insulin-dependent diabetes mellitus; recently, more patients with type 2 diabetes mellitus have undergone pancreas transplantation[1]. In the United States, simultaneous pancreas and kidney transplantation (SPKT) was the most common type of pancreas transplantation in 2018[1]. More than 80% of pancreas transplantations are performed with enteric drainage (ED), and systemic venous drainage is used for more than 90% of pancreas transplantations[2]. The site of enteric anastomosis can range from the stomach to the distal ileum of the recipient[3-6]; most often, the site of anastomosis is at the jejunum[2]. Direct side-to-side anastomosis between the transplanted duodenal segment and the recipient small bowel is the most common technique. Gastrointestinal (GI) bleeding and anastomotic leak are the most common surgical complications associated with enteric anastomosis[7]. GI bleeding may occur early and late after transplantation, and the morbidity of GI bleeding could be as high as approximately 11% according to previous reports[5,8]; it can result in graft loss and can be a life-threatening condition[7,9]. The sites of GI bleeding are mainly at the level of the enteric anastomosis[8,9]. Suture ligation (SL) techniques have been used during hemostasis for larger blood vessels throughout gastrectomy. The intestinal wall has abundant microvessels. For ordinary small intestinal anastomosis, sufficient suture pitch and the adequate strength of knotting can ensure adequate hemostasis during the anastomosis between the small intestine, and an SL technique is not needed usually. Enteric anastomosis during SPKT is different from ordinary small intestinal anastomosis: The transplanted duodenal segment is edematous after blood reperfusion, and the anastomotic stoma is corroded by constant exocrine outputs of the pancreas graft. There have been no reports on whether the SL technique is beneficial for submucosal hemostasis during hand-sewn enteric anastomosis in pancreas transplantation. To investigate the advantages and disadvantages of this novel technique on early EA bleeding and anastomotic leakage, we retrospectively analyzed the clinical data of patients who underwent SPKT at our center. This study adheres to the declarations of Istanbul and Helsinki, and none of the organs used were from executed prisoners. All donors were neither paid nor coerced.
From January 2016 to December 2019, 138 SKPT were performed in our center, and 134 patients were included in this study. All graft organs came from deceased donors, including 9 cases of anoxia, 45 cases of cerebrovascular accident/stroke, 73 cases of head trauma, 4 cases of central nervous system tumor, and 3 cases of organophosphorus poisoning. The indications for transplantation were type 1 or type 2 diabetes with end-stage renal disease. During the transplant evaluation process, all patients underwent gastroscopy and colonoscopy. Exploration of all the small intestines during operation was performed for every patient. Patients with one or more of the below diseases were excluded from the study: Gastroduodenal ulcer, severe gastritis and duodenitis, colitis, digestive tract tumor, diverticulum, digestive tract polyp, and GI bleeding history. Patients with graft pancreasectomy due to thrombosis or severe infection within the first postoperative week were excluded from the study. According the above criteria, two patients with graft pancreasectomy due to thrombosis within the first postoperative week were excluded from the study. One patient diagnosed with ascending colonic diverticulum by colonoscope before transplantation and experienced hemorrhage of diverticulum after SPKT was excluded. Another patient was excluded from the study because of a history of duodenal ulcer bleeding. Cytomegalovirus (CMV) DNA tests performed before SPKT were negative for all included patients. The characteristics of the recipients and donors included in the study are shown in Table 1.
| Characteristics | SL group (n = 44) | NSL group (n = 90) | P value |
| Donor age, yr | 34.00 ± 8.82 | 32.32 ± 10.65 | 0.367 |
| Donor gender (male/female, n) | 36/8 | 75/15 | 0.827 |
| Recipient age, yr | 46.52 ± 9.50 | 47.41 ± 10.79 | 0.643 |
| Recipient gender (male/female, n) | 37/7 | 75/15 | 0.911 |
| Duration of diabetes, yr | 16.73 ± 6.2 | 15.88 ± 5.9 | 0.449 |
| Diabetes type (1/2) | 7/37 | 18/72 | 0.568 |
| BMI | 24.66 ± 3.68 | 23.60 ± 3.18 | 0.089 |
| Blood type, n | |||
| A+/B+/AB+/O+ | 10/10/4/20 | 17/35/10/28 | 0.169 |
| Duration of dialysis, months, median (IQR) | 12.00 (6.25, 36.00) | 10.00 (5.00, 20.75) | 0.037 |
| Pancreas ischemia time, minutes | 446.71 ± 104.11 | 400.94 ± 89.79 | 0.010 |
| HLA-A, -B, -DR mismatch | |||
| 0-3 | 8 (18.18) | 19 (21.11) | 0.691 |
| 4-6 | 36 (81.82) | 71 (78.89) | 0.691 |
| Maintenance Immunosupression | |||
| TAC | 40 (90.91) | 72 (80.00) | 0.109 |
| CsA | 4 (9.09) | 18 (20.00) | 0.109 |
| DIC indicators | |||
| PT-INR | 1.50 ± 0.37 | 1.55 ± 0.35 | 0.463 |
| APTT (s) | 60.15 ± 35.18 | 56.35 ± 38.39 | 0.582 |
| TT (s) | 60.07 ± 37.90 | 66.34 ± 37.03 | 0.362 |
| PLT (109/L) | 106.41 ± 45.35 | 108.94 ± 50.87 | 0.780 |
The liver, pancreas, and kidney were recovered using an en bloc technique for organ procurement. For the duodenal decontamination, lavage technique via the nasogastric tube was performed routinely with normal saline (500 mL), and then metronidazole solution (200 mL) was instilled during pancreas procurement. The proximal gastroduodenal artery (GDA) and distal common hepatic artery were distributed to the liver, leaving the aortic patch with the superior mesenteric artery and celiac trunk for the pancreas. Subsequently, the distal splenic artery and vein were ligated, and the spleen was removed. After the proximal and distal donor duodenum were closed using a linear cutting stapler, the stump was strengthened by interrupted seromuscular sutures. As reported in the literature[10], we reconstructed the GDA by end-to-end anastomosis with the common hepatic artery or left gastric artery and interposed a donor mesentery artery, if necessary.
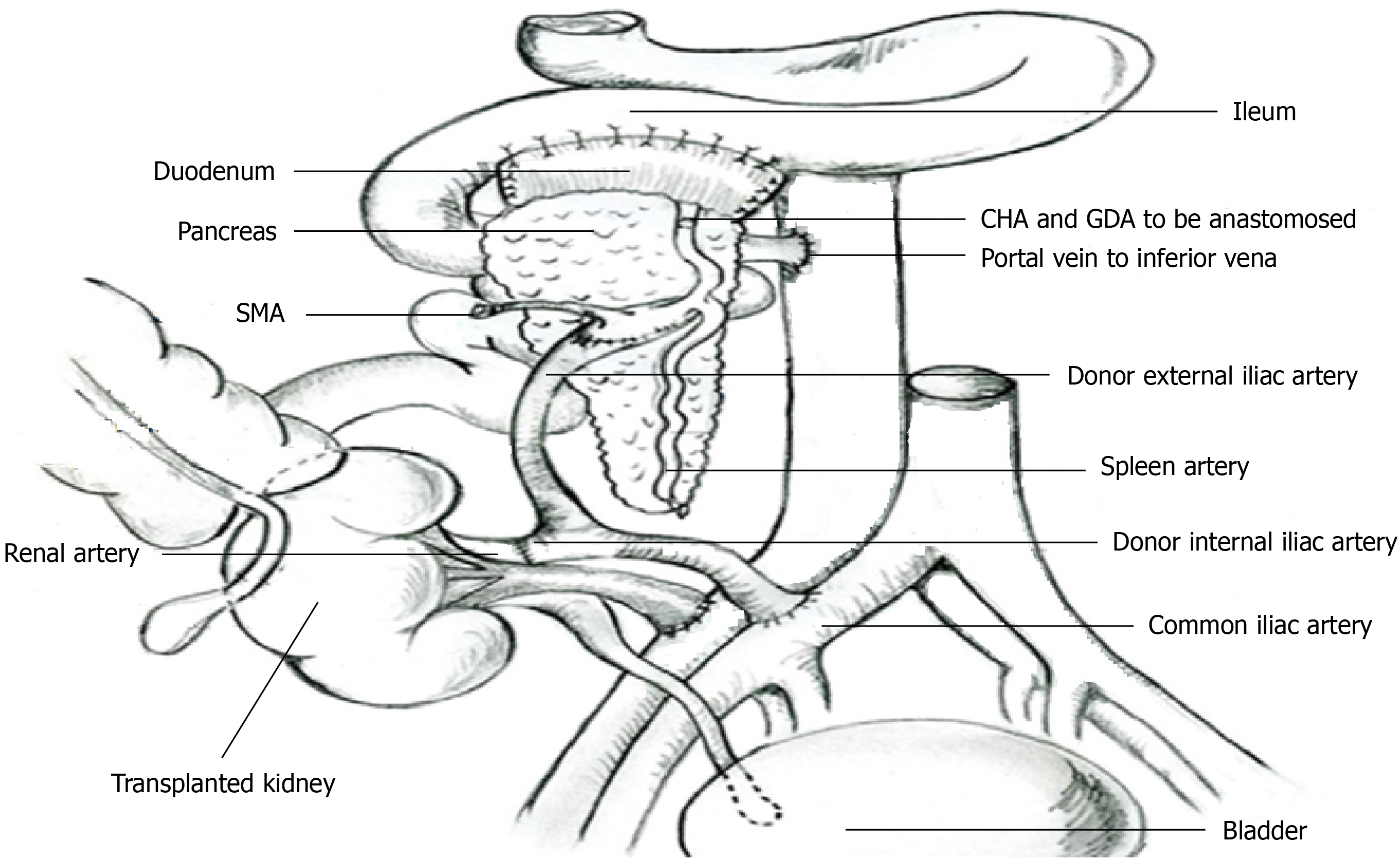
Both kidney and pancreas transplantations were performed using a single right incision through the rectus abdominis. As reported by Tso[11], we anastomosed the renal artery to the internal iliac artery limb of the donor conduit and anastomosed the aortic patch of the graft to the external iliac artery limb of the donor conduit and the common iliac artery of the donor conduit to the right external iliac artery of the recipient in an end-to-side fashion, so both organs could be vascularized by utilizing a single Y arterial conduit (Figure 1). Both organs were transplanted on the right side of the patient’s abdominal cavity. The renal vein was anastomosed to the right external iliac vein. The venous outflow of the pancreas graft was arranged via the systemic venous system by anastomosing the portal vein end-to-side to the distal vena cava. The head of the pancreas and duodenum were oriented superiorly, and the donor duodenal segment was anastomosed side-to-side to the distal ileum. The distance from the anastomotic stoma to the ileocecal valve was 60 cm. The operation process is illustrated in Figure 1.
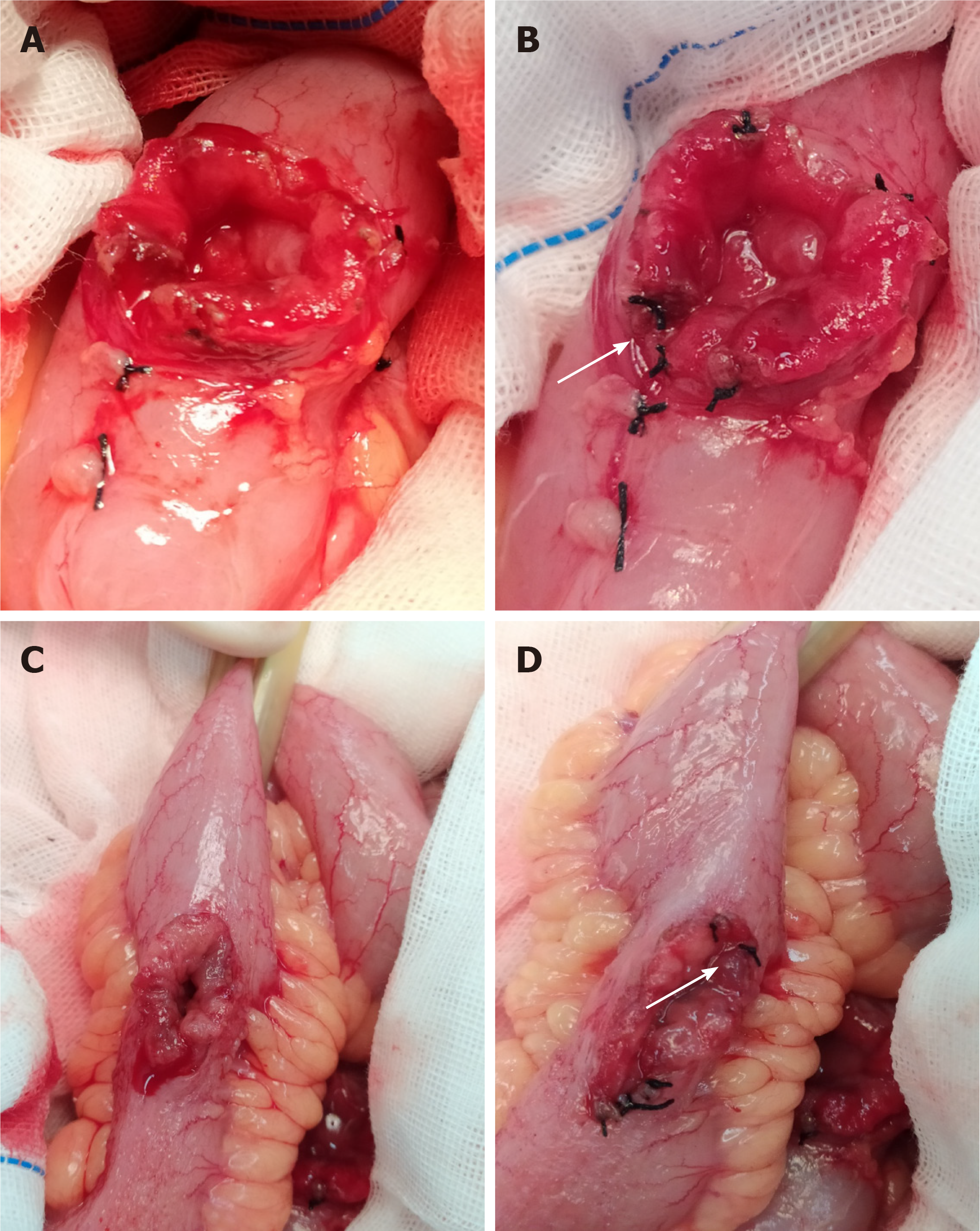
According to the pattern of enteric anastomosis, patients were divided into two groups: SL or no SL (NSL) groups. From the first outpatient visit, during preoperative evaluation, operation, and follow-up after SPKT, a patient will be under constant supervision by the same doctor in our center. If a patient was supervised by the doctor who is the corresponding author of this paper, then the patient was allocated into the SL group. If a patient was not supervised by the doctor who is the corresponding author of this paper, then the patient was allocated into the NSL group. There were no other criteria for grouping. A total of 44 and 90 patients were classified into the SL group and NSL group, respectively. The transplanted duodenal segment and the distal ileum of the recipient were incised 3-4 cm longitudinally at the site of the anastomotic stoma by using a scalpel after pancreas graft blood reperfusion. Then, mucosal aneriodine cotton balls were used for decontamination of the duodenal segment and the distal ileum. In the SL group, bleeding spots at the cut edge of the bowel (ileum of the recipient and duodenum of the transplanted organ) were staunched by transmural figure-of-eight SL at the mucosal points of the bleeding with a silk thread (Figure 2). A penetration of all layers from the serosa to the lumen was made, and the needle position on the serosa and mucosa was 1-2 mm apart from the cut edge. In the NSL group, SL was not performed, and electric coagulation using an argon knife was performed if necessary. After submucosal hemostasis, side-to-side duodeno-ileostomy was performed using a two-layer hand-sewn running anastomosis: A running unabsorbable suture for the transmural inner layer and an outer inverted seromu
Anti-thymocyte globulin was administered for induction at 1.5 mg/kg during surgery and 1.5 mg/kg per day for 3 d after transplantation. The maintenance immunosuppression regimen included tacrolimus or cyclosporine, mycophenolate mofetil, and prednisolone (Table 1). The target trough level of tacrolimus was 8-12 ng/mL within 3 mo of transplantation, the target trough level of cyclosporine was 150-200 ng/mL, and the target level of cyclosporine 2 h after administering the medicine was 800-1200 ng/mL.
To prevent pancreatic graft thrombosis, low-molecular-weight heparin was administered for 6 d (50 IU/kg/d) by subcutaneous injection for all patients, followed by the oral administration of aspirin (100 mg/d) for 3 mo. If GI bleeding occurred, prophylactic anticoagulation therapy was withdrawn. Patients of the two groups received the same anticoagulation prophylaxis. Routine monitoring of the platelet count and disseminated intravascular coagulation (DIC) indicators was performed during anticoagulation therapy.
The diagnostic criteria of EA bleeding were as follows: (1) Patient experienced melena or hematochezia with obvious hemoglobin decline, and anastomotic bleeding was identified by angiography or relaparotomy; and (2) If the patient experienced melena or hematochezia with obvious hemoglobin decline, but relaparotomy was not performed and angiography results was negative and could not show the site of GI bleeding, then the following criteria must be met: No blood fluid was drained from nasogastric tubes and colonoscopy revealed that the end ileal lumen next to the ileocecal valve contained blood fluid. Anastomotic leak was diagnosed based on clinical symptoms, imaging study results, laboratory findings, or a combination thereof, as previously reported[12].
The results of CMV DNA blood tests of all EA bleeding recipients at the time of EA bleeding were collected.
Continuous variables were reported as mean ± SD or medians [interquartile range (IQR)] depending on the distribution of the data. If data were normally distributed and had variance homogeneity, an analysis of variance was used for comparisons between groups. If the distribution was not normal, a Kruskal-Wallis rank-sum test was used for comparisons between groups. Categorical variables were analyzed using a chi-square test. Cumulative graft and patient survival rates were computed by a Kaplan-Meier survival analysis. Data analyses were performed using R 3.6.2 statistical software. The study was reviewed by our expert biomedical statistician Cao Y, MD.
The characteristics of the donors and recipients in the SL and NSL groups are displayed in Table 1. There were 44 and 90 patients in the SL group and NSL group, respectively. The two groups were matched for the following: Age of the donor; donor sex; age of the recipient; diabetes duration; diabetes type; body mass index; blood type; human leukocyte antigen (HLA) -A, HLA-B, and HLA-DR mismatch; immunosuppression; DIC indicators; and platelet count. The duration of dialysis was slightly longer in the SL group than in the NSL group [12.00 mo (IQR, 6.25, 36.00) vs 10.00 mo (IQR, 5.00, 20.75); P = 0.037]. The pancreas ischemia time was longer in the SL group than in the NSL group (446.71 ± 104.11 min vs 400.94 ± 89.79 min; P = 0.010).
In the first postoperative week, the EA bleeding rate was less in the SL group (1/44; 2.27%) than in the NSL group (14/90; 15.56%; P = 0.021) (Table 2), respectively. Patients from both groups received immediate anticoagulant treatment. The transfusion rate for EA bleeding in the first postoperative week was lower in the SL group than in the NSL group [2.27% (1/44) vs 14.44% (13/90); P = 0.035].
| Characteristics | SL group (n = 44) | NSL group (n = 90) | P value |
| EA bleeding | 1 (2.27) | 14 (15.56) | 0.021 |
| Transfusion rates due to EA bleeding | 1 (2.27) | 13 (14.44) | 0.035 |
| Relaparotomy due to EA bleeding | 0 (0.00) | 3 (3.33) | 0.551 |
| Anastomotic leakage | 1 (2.27) | 1 (1.11) | 0.754 |
If medical treatment exceeded more than 48 h and hematochezia was not relieved and was accompanied by unstable blood pressure, relaparotomy was considered. Owing to the failure of conservative therapy, three patients in the NSL group underwent relaparotomy (Tables 2 and 3), and EA bleeding was identified, and the reconstruction of the anastomosis was performed in these three patients. There were no pancreas graft loss and no recurrence of GI bleeding after relaparotomy. The rate of relaparotomy due to EA bleeding was lower in the SL group than in the NSL group; however, no differences were found between the two groups [0% (0/44) vs 3.33% (3/90); P = 0.551].
| Case | Age | Sex | Transplant time | Bleeding start time1 |
| 1 | 47 | M | October 2016 | 5 |
| 2 | 29 | M | October 2016 | 7 |
| 3 | 40 | M | October 2017 | 6 |
Anastomotic leakage was observed in 1 (2.27%) of 44 patients in the SL group at postoperative day (POD) 14 and was healed by conservative treatment. One patient in the NSL group (1/90; 1.11%) experienced anastomotic leakage at POD 16; subsequently, the pancreas graft was lost.
CMV DNA blood testing was performed for all EA bleeding patients within 1 wk post-operation, and results were all negative. Three patients in the NSL group underwent relaparotomy; unfortunately, the biopsy of the transplanted duodenal segment was not performed during relaparotomy. Therefore, the results of the immunohistochemistry staining of the transplanted duodenal segment for CMV were not available.
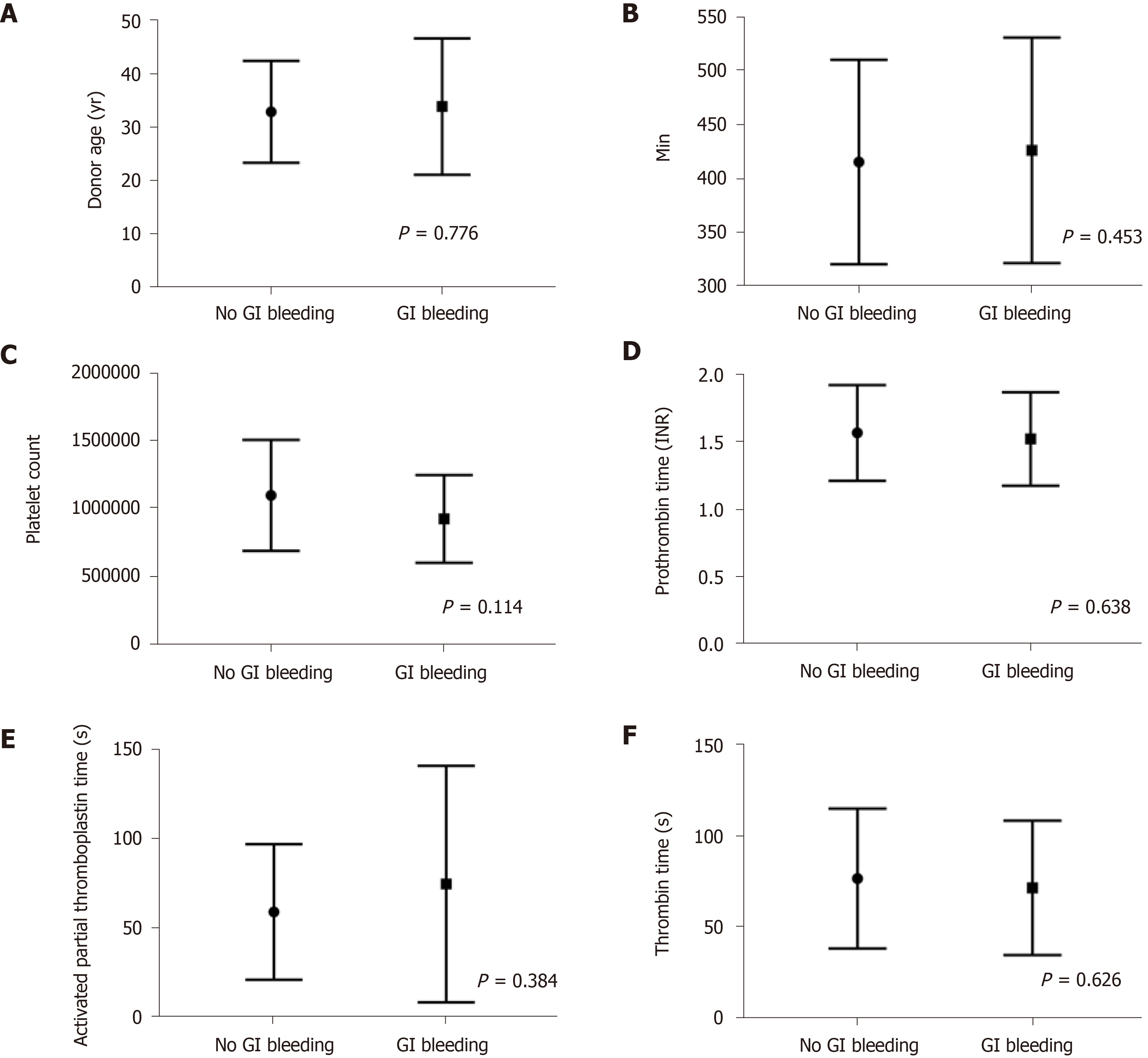
A comparison of patients with EA bleeding (n = 15) and those without EA bleeding (n = 119) within the first week after transplantation showed no differences in donor age (Figure 3A), mean pancreatic cold ischemia time (Figure 3B), platelet count (Figure 3C), prothrombin time international normalized rate (Figure 3D), activated partial thromboplastin time (Figure 3E), and thrombin time (Figure 3F).
The median follow-up durations were 2.11 years and 2.12 years for patients of the SL group and NSL group, respectively. The Kaplan–Meier curves plotted for comparisons between the SL and NSL groups after transplantation are shown in Figure 4. No significant difference was found between the two groups in terms of the survival curves for patients, pancreas graft, and kidney graft. The study was reviewed by our expert Biostatistic Cao Y, MD.
In 1967, the first SPKT was performed by Kelly et al[13] at the University of Minnesota. Since then, several pancreas transplantation techniques have been developed. From the mid-1970s to the mid-1980s, segmental pancreas transplantation was the prevalent technique. Subsequently, whole pancreaticoduodenal graft transplantation with ED became the gold standard for SPKT[6]. In the majority of cases involving ED, systemic venous drainage was used[14]. Inferior vena cava drainage and duodeno-ileostomy without a Roux-en-Y loop have been used in our center.
ED can be justified based on physiological conditions; however, the complications associated with a simultaneously transplanted duodenum, such as GI bleeding and anastomotic leakage, may be potentially life-threatening. The accurate morbidity rate associated with GI bleeding after ED pancreas transplantation is unknown. In the literature, the data on GI bleeding following pancreas transplantation are under-reported. Large case series reports are insufficient and the criteria for GI bleeding were not elucidated from these reports. Orsenigo et al[8] reported that 11% (7/61) of recipients experienced GI bleeding complications during the first postoperative week, and six patients (85.71%) required relaparotomy and EA bleeding was identified in five patients. In a study of 11 cases, one patient required endoscopy for the luminal bleeding of the duodenal anastomosis site[4]. A report in Austria showed that in 379 pancreas transplants, GI bleeding occurred in 28 (7.38%) patients, of which 23 (82.14%) patients experienced GI bleeding at the level of the enteric anastomosis, and surgery was required in 25% of GI bleeding cases[9]. In our study, 20.0% (3/15) of the patients with EA bleeding underwent relaparotomy.
With the dramatic improvements in staplers, stapled anastomoses are being used for digestive tract reconstruction in ordinary small intestinal surgery and for pancreas transplantation[15,16]. When using a linear cutting stapler for enteric anastomosis, bleeding along the staple line could be controlled by interrupted sutures[16]. Because the transplanted duodenal segment is usually edematous after blood reperfusion, stapled anastomoses may be unsuitable for the intestinal tract in severe edematous cases. Besides, stapled anastomoses are more expensive than hand-sewn technique especially in developing countries[17]. Compared with duodeno-duodenostomy, duodeno-ileostomy combined with postcava drainage in our study could decrease the surgical difficulty significantly but made it difficult to perform hemostasis by endoscopy in cases of EA bleeding. Therefore, improvements in the hand-sewn technique for ED are still required to decrease morbidity associated with complications related to the transplanted duodenal segment.
There are abundant vessels in the submucosal plexus of the intestinal wall[18]. In one report, ligation or electric coagulation was performed for hemostasis in 46 cases involving anastomoses of the small bowel to the small bowel in the control group[17]; however, there is no report involving SPKT cases. GI bleeding that occurs within 7 d of pancreas transplantation with ED usually initiates from the anastomotic suture line[8-9,19]. Our study demonstrated that the incidence of EA bleeding within the first postoperative week could be minimized by using a careful plication technique during SPKT. Pancreas transplantation is a complicated transplant procedure, and the surgical experience for pancreas transplantation may influence the success and complication rates of such a complicated transplant procedure. The surgical team in the NSL group possessed much more surgical experience and should achieve lower EA bleeding rate than the relative younger surgical team in the SL group, but our data showed the opposite result: The EA bleeding rate was lower in the SL group. We think that the plication technique affected the EA bleeding rate more than surgical experience, leading to the decreasing EA bleeding rate in the SL group. Non-crushing bowel clamps should be applied to the ileum only, and the mesentery of the ileum should not be clamped, so that bleeding spots at the cut edge of the ileum of the patient could be thoroughly staunched. The blood vessels in the submucous layers might be destroyed by ligation, which may affect the anastomotic stoma healing rate, and cause anasto
Several factors may account for the anastomotic stoma’s propensity for EA bleeding. The transplanted duodenal segment is edematous after blood reperfusion. When edema subsides postoperatively, an onset of anastomotic stoma bleeding might occur at the anastomotic suture line due to the weakening compressive strength of the suture thread. Another factor is the exocrine output of the pancreas graft. Trypsinogen enters the small intestine and is stimulated as active trypsin by enterokinase in the small intestine. The introrsus cut edges of the bowel at the anastomotic site are directly exposed to the intestinal cavity and corroded by the active trypsin, thus increasing the susceptibility of the anastomotic stoma to bleeding. In 1982, Groth et al[20] inserted a catheter in the pancreatic duct to protect the anastomosis sutures during the segmental pancreas transplantation. Because of a propensity for thrombosis, most centers use some types of empiric thromboprophylaxis[21,22]. Poor coagulation function may be a risk factor for EA bleeding in SPKT. Our data showed no relationship between coagulation indicators and EA bleeding (Figure 3). Ulceration with bleeding due to CMV infections has been reported in the duodenal cuff of the transplanted pancreas[23], but CMV infection did not correlate with EA bleeding in our study.
The first limitation in this study is its retrospective approach. Another limitation of this study is the relatively small number of patients in the SL group; more cases are needed to confirm the benefit of SL technique in SPKT.
Compared with no SL, a two-layer running hand-sewn anastomosis with hemostasis by SL at the cut edge of the bowel (ileum of the recipient and duodenum of the donor organ) may help decrease the morbidity of early EA bleeding and the transfusion rate, without increasing the anastomotic leakage rate.
As a potentially life-threatening complication of simultaneous pancreas and kidney transplantation (SPKT), enteric anastomotic (EA) bleeding frequently results in surgical relaparotomy and graft loss; therefore, it is essential to decrease the incidence of EA bleeding.
An effort was made for submucosal hemostasis during enteric anastomosis in SPKT with a lower EA bleeding rate.
To investigate the advantages and disadvantages of suture ligation (SL) for submucosal hemostasis during enteric anastomosis on early EA bleeding and anastomotic leakage in SPKT.
We compared the outcomes of 134 patients classified into SL (n = 44) and no SL (NSL) groups (n = 90).
During the first postoperative week, the EA bleeding rate in the SL group was lower than that in the NSL group during the first postoperative week. No relationship was found between EA bleeding and donor age, mean pancreatic cold ischemia time, platelet count, prothrombin time international normalized rate, activated partial thromboplastin time, and thrombin time. No significant difference was noted between the two groups in terms of the anastomotic leakage rate, patient survival curve, pancreas graft survival curve, or kidney graft survival curve.
Compared with no SL, SL for submucosal hemostasis during enteric anastomosis in SPKT can decrease the EA bleeding rate and do not increase the anastomotic leakage rate.
Further clinical randomized controlled studies with a large sample size are needed to confirm the effect of plication techniques on submucosal hemostasis during enteric anastomosis in SPKT in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Transplantation
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Carlis R S-Editor: Liu M L-Editor: A P-Editor: Li JH
| 1. | Kandaswamy R, Stock PG, Gustafson SK, Skeans MA, Urban R, Fox A, Israni AK, Snyder JJ, Kasiske BL. OPTN/SRTR 2018 Annual Data Report: Pancreas. Am J Transplant. 2020;20 Suppl s1:131-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Kerr HR, Hatipoglu B, Krishnamurthi V. Pancreas transplant for diabetes mellitus. Cleve Clin J Med. 2015;82:738-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Linhares MM, Beron RI, Gonzalez AM, Tarazona C, Salzedas A, Rangel EB, Sá JR, Melaragno C, Goldman SM, Souza MG, Sato NY, Matos D, Lopes-Filho GJ, Medina JO. Duodenum-stomach anastomosis: a new technique for exocrine drainage in pancreas transplantation. J Gastrointest Surg. 2012;16:1072-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Ryu JH, Lee TB, Park YM, Yang KH, Chu CW, Lee JH, Kim T, Choi BH. Pancreas transplant with duodeno-duodenostomy and caval drainage using a diamond patch graft: a single-center experience. Ann Transplant. 2017;22:24-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Walter M, Jazra M, Kykalos S, Kuehn P, Michalski S, Klein T, Wunsch A, Viebahn R, Schenker P. 125 cases of duodenoduodenostomy in pancreas transplantation: a single-centre experience of an alternative enteric drainage. Transpl Int. 2014;27:805-815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Squifflet JP, Gruessner RW, Sutherland DE. The history of pancreas transplantation: past, present and future. Acta Chir Belg. 2008;108:367-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Boggi U, Vistoli F, Del Chiaro M, Moretto C, Croce C, Signori S, D'Imporzano S, Amorese G, Campani D, Calabrese F, Capocasale E, Marchetti P. Total duodenectomy with enteric duct drainage: a rescue operation for duodenal complications occurring after pancreas transplantation. Am J Transplant. 2010;10:692-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Orsenigo E, Fiorina P, Dell'Antonio G, Cristallo M, Socci C, Invernizzi L, Maffi P, Secchi A, Di Carlo V. Gastrointestinal bleeding from enterically drained transplanted pancreas. Transpl Int. 2005;18:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Messner F, Bösmüller C, Oberhuber R, Maglione M, Cardini B, Resch T, Scheidl S, Öfner D, Schneeberger S, Margreiter C. Late recurrent bleeding episodes from duodenojejunostomy after pancreas transplantation. Clin Transplant. 2018;32:e13350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Li JQ, He ZJ, Si ZZ, Hu W, Li YN, Qi HZ. Gastroduodenal arterial reconstruction of the pancreaticoduodenal allograft. Transplant Proc. 2011;43:3905-3907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Tso PL, Cash MP, Pearson TC, Larsen CP, Newell KA. Simultaneous pancreas-kidney transplantation utilizing a common arterial conduit: early experience and potential applications. Am J Transplant. 2003;3:1440-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Humar A, Kandaswamy R, Granger D, Gruessner RW, Gruessner AC, Sutherland DE. Decreased surgical risks of pancreas transplantation in the modern era. Ann Surg. 2000;231:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 191] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Kelly WD, Lillehei RC, Merkel FK, Idezuki Y, Goetz FC. Allotransplantation of the pancreas and duodenum along with the kidney in diabetic nephropathy. Surgery. 1967;61:827-837. [PubMed] |
| 14. | Gruessner AC. 2011 update on pancreas transplantation: comprehensive trend analysis of 25,000 cases followed up over the course of twenty-four years at the International Pancreas Transplant Registry (IPTR). Rev Diabet Stud. 2011;8:6-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 224] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 15. | Verzaro R, de Simone P. Use of circular stapler for enteric drainage of the pancreatic graft. J Am Coll Surg. 2004;199:518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Lam VW, Wong K, Hawthorne W, Ryan B, Lau H, Robertson P, Allen RD, Pleass H. The linear cutting stapler for enteric anastomosis: a new technique in pancreas transplantation. Transpl Int. 2006;19:915-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Zhang Q, Zeng Q, Lin W, Chen Y, Yu Z, Zhou M, Han S, You J. Single-layer anastomosis without hemostasis in the submucosa layer by electric coagulation or ligation: a novel technique of anastomosis for all gastrointestinal tracts. Hepatogastroenterology. 2011;58:96-98. [PubMed] |
| 18. | BOULTER PS, PARKS AG. Submucosal vascular patterns of the alimentary tract and their significance. Br J Surg. 1960;47:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Dhanireddy KK. Pancreas transplantation. Gastroenterol Clin North Am. 2012;41:133-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Groth CG, Collste H, Lundgren G, Wilczek H, Klintmalm G, Ringdén O, Gunnarsson R, Ostman J. Successful outcome of segmental human pancreatic transplantation with enteric exocrine diversion after modifications in technique. Lancet. 1982;2:522-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 63] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Muthusamy AS, Giangrande PL, Friend PJ. Pancreas allograft thrombosis. Transplantation. 2010;90:705-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Raveh Y, Ciancio G, Burke GW, Figueiro J, Chen L, Morsi M, Namias N, Singh BP, Lindsay M, Alfahel W, Sleem MS, Nicolau-Raducu R. Susceptibility-directed anticoagulation after pancreas transplantation: a single-center retrospective study. Clin Transplant. 2019;33:e13619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Barone GW, Webb JW, Hudec WA. The enteric drained pancreas transplant: another potential source of gastrointestinal bleeding. Am J Gastroenterol. 1998;93:1369-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |