Published online Feb 10, 2016. doi: 10.4239/wjd.v7.i3.45
Peer-review started: October 2, 2015
First decision: November 4, 2015
Revised: November 26, 2015
Accepted: January 8, 2016
Article in press: January 11, 2016
Published online: February 10, 2016
Processing time: 119 Days and 10 Hours
The incidence of diabetes mellitus (DM) is increasing rapidly. DM is the leading cause of cardiovascular diseases, which can lead to varied cardiovascular complications by aggravated atherosclerosis in large arteries and coronary atherosclerosis, thereby grows the risk for macro and microangiopathy such as myocardial infarction, stroke, limb loss and retinopathy. Moreover diabetes is one of the strongest and independent risk factor for cardiovascular morbidity and mortality, which associated frequently rhythm disorders such as atrial fibrillation (AF) and ventricular arrhythmias (VA). The present article provides a concise overview of the association between DM and rhythm disorders such as AF and VA with underlying pathophysiological mechanisms.
Core tip: The incidence of diabetes mellitus (DM) is increasing rapidly. DM is the leading cause of cardiovascular diseases. Atrial fibrillation (AF) and ventricular arrhythmias (VA) are most common form of arrhythmias, which lead to cardiovascular complications and mortality in patients with DM. The present article provides a concise overview of the association between DM and rhythm disorders such as AF and VA with underlying pathophysiological mechanisms.
- Citation: Koektuerk B, Aksoy M, Horlitz M, Bozdag-Turan I, Turan RG. Role of diabetes in heart rhythm disorders. World J Diabetes 2016; 7(3): 45-49
- URL: https://www.wjgnet.com/1948-9358/full/v7/i3/45.htm
- DOI: https://dx.doi.org/10.4239/wjd.v7.i3.45
Diabetes mellitus (DM) is recognized as a major cardiovascular (CV) risk factor and its close relationship with cardiovascular morbidity and mortality is well established[1]. Although coronary artery disease and related cardiac events are the most documented diabetic cardiovascular effects, cardiac electrical system is also an important target for diabetic damage. In Framingham heart study, DM is established as an independent risk factor for atrial fibrillation (AF) after 38 years of follow-up[2]. A recent meta-analyses published by Huxley et al[3] revealed that patients with DM had a 40% greater risk of developing AF compared to patients without. On the other hand, there has been growing evidence about the relationship between hypoglycaemic episodes and ventricular rhythm disorders for the recent years[4,5]. The relationship between DM and arrhythmic disorders is not fully understood yet and there is a growing population of DM patients everyday. This relationship is expected to become more of an issue in the near future. Here we would like to present a brief overview on this relationship especially for AF and ventricular arrhythmias.
AF is the most common arrhythmia in clinical practice resulting in major cardiovascular morbidity and mortality[6]. Earlier The Framingham Study and recently a study from Movahed et al[7] clearly established that DM is a powerful and independent risk factor for the development of AF. This close relationship between AF and DM raises the question for pathophysiological basis for this entity. Although there is no single and easy answer for this question, both electrical and anatomical remodelling seems to be important keys of these complex pathophysiological changes.
Extensive fibrosis in the atrial tissue is the anatomical hallmark of AF with a role in both starting and perpetuation of the arrhythmia and as the fibrosis expands it is more likely that paroxysmal AF transforms into permanent or anti arrhythmic resistant type[8,9]. Kato et al[10] showed that DM related atrial fibrosis has a potential role in starting AF in diabetic rat models. Exaggerated systemic and tissue level oxidative stress seems to be the key element in atrial fibrosis related to DM. Dudley et al[11] evaluated the superoxide anyone levels in a pig atrial model. The study compared the levels of superoxide in left atrial appendage between the sinus rhythm group and atrial rapid pacing (ARP) group. Results showed that in the ARP group left atrial superoxide anion levels were almost three times higher than the control group. Another study from Anderson et al[12] showed that mitochondrial oxidative stress is increased in diabetic human atrial tissue. These studies may show that despite increased levels of systemic oxidative stress in DM, there may be a production of reactive oxygen species via mitochondrial pathway specifically at the atrial tissue level.
Non-enzymatic glycosylation of proteins and the end products of this pathway (Advanced Glycation End products; AGEs) interact with their receptors (RAGE) and upregulate the connective tissue growth factor (CGTF)[13]. This system (AGERAGE) may start or contribute to atrial fibrosis in diabetic patients via stimulation of connective tissue growth factor in the atrial myocardium[14].
Dysfunction in the autonomic innervation and control of cardiovascular system is defined in diabetic patients[15]. It seems that autonomic imbalance in favour of sympathetic system, which might have a role in the onset of AF. Otake et al[16] previously documented that excessive sympathetic stimulation in streptozocin induced diabetic rats increases the incidence of AF compared to control group. Further electrophysiological studies in the diabetic rat atrium revealed shortened atrial effective refractory period (AERP) and increased dispersion of AERP. Another clinical study suggested that reduced heart rate recovery in type 2 DM patients with preserved ejection fraction is associated with increase in the incidence of AF[17]. These clinical and laboratory studies imply that autonomic dysfunction has a role in the pathogenesis of AF in DM patients.
Atrial electrical structure is also affected in diabetic patients. Shortened AERP increased dispersion of AERD and intra atrial conduction time, which are the key elements of atrial electrical remodeling[16,18]. Chao et al[19] analyzed the detailed three-dimensional electro anatomic mapping of 228 patients who has DM or abnormal glucose metabolism (AGM) and underwent AF ablation for the first time. Results showed that biatrial voltage measurements in DM and AGM group were significantly lower than control group. Furthermore these patients also had increased recurrence rate of AF in the follow up period. Acar et al[20] has shown in their published study, that patients with DM had significantly increased inter and intra atrial electro mechanic delay with impaired diastolic functions comparing to control group. On the other hand, it has been shown that there is a specific change in cell to cell integration in DM patients. In a streptozocin induced diabetic rat model study, connexin 43 expression was significantly higher than connexin 40 in diabetic rat atria, which may sign that connexin 43 expression is upregulated in diabetics as a gap junction protein[21].
Conversely, there are some other data suggesting that fluctuations in the blood glucose level rather than the long-term hyperglycemic environment is related to increase in the incidence of AF in diabetic patients[22]. Saito et al[23] showed that glucose fluctuations increase the incidence of AF in streptozocin induced diabetic rat models. Huxley et al[24] failed to show any correlation between fasting glucose, insulin levels, HbA1c levels measurements and AF onset in patients without diabetes. Another clinical study from Fatemi et al[25] prospectively evaluated the affect of intense glycemic control on incidence of AF in diabetic patients. Interestingly, they failed to present any association between incident AF and intense therapy comparing to standard therapy group. However, their choice of periodic electrocardiographic testing instead of event recorders might alter the results in terms of missing the paroxysmal AF episodes occurring any time besides the office control.
There are no randomized data specifically addressing the effect of DM in other supraventricular arrhythmias, but there are case reports discussing whether acute changes in metabolic profile during ketoacidosis episodes might trigger arrhythmias such as supraventricular tachycardia[26].
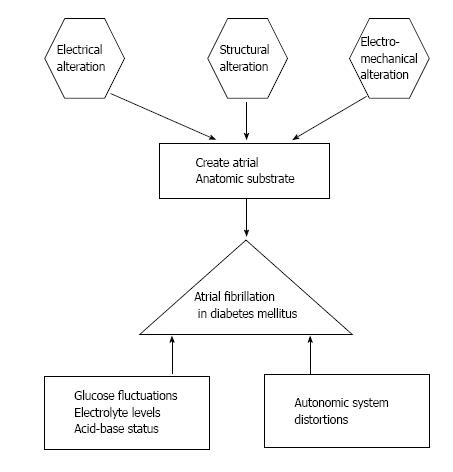
Overall, DM seems to be acting a pivotal role in generation and maintenance of AF in diabetic patients. Specific structural, electrical and electromechanically alterations in diabetic heart might create an anatomic substrate for the development of AF. On the other hand, acute hypo or hyperglycemia changes in electrolyte levels or acid-base status and autonomic system distortions may be a trigger mechanism for the arrhythmia (Figure 1). It is clear that there are still dark spots about the relationship between AF and DM that warrants further studies.
Cardiovascular diseases (CVD) are the leading cause of death in diabetics and DM is almost a synonym for atherosclerosis and coronary artery disease. High incidence and extent of atherosclerotic heart disease in diabetics leads to high incidence of ventricular arrhythmias (VA) and sudden cardiac death (SCD) inevitably[27-29]. Although this close relationship between VA, SCDs and DM is mostly based on the extent of coronary artery disease among diabetics, non-coronary atherosclerotic processes like autonomic neuropathy, microvascular disease, ventricular structural and electrical changes may partly play a role in this phenomenon[30].
A ventricular repolarization anomaly, which is reflected by QTc interval prolongation, is associated with high risk of VA. There are several studies showing, marked QTc prolongation in diabetic patients[31]. Another strong predictor of VA, microvolt T wave alternans (TWA) measurement, has been studied in type 2 diabetic patients without known CVD, considering the glycemic status in each patient (which is reflected by HbA1c levels)[32]. In this small study, the frequencies of atypical TWA patients were significantly higher than the control group. In the diabetic patient group, patients with atypical TWA measurements had significantly elevated HbA1c levels, which is concluded as every 1% rise in HbA1c levels is linked with 13 fold higher risk of having atypical TWA and suboptimal glycemic control is linked with higher risk of spontaneous VA independent of QTc interval duration. These results from the studies are signing an electrical instability of diabetic myocardium, which creates a potential substrate for ventricular arrhythmias independent from the scarred myocardium areas from previous ischemic cardiac damages. On the other hand, autonomic neuropathy of diabetes results in an unbalanced sympathetic stimulation on myocardium, which may further contribute to this electrical instability and predispose to lethal arrhythmias[33]. In this context, cardiac sensory neuropathy of diabetics is another important issue that causes VA and sudden death indirectly via silent ischemia[34].
As DM creates a vulnerable myocardium for arrhythmias, it seems to be involved in the triggering mechanism for these arrhythmias too. A study from Chen-Scarabelli et al[35] investigated if there is a relationship between HbA1c levels and risk of VA in patients with implantable cardioverter defibrillators retrospectively. The study included 141 patients with DM and 195 patients without DM. A significant association between HbA1c levels of 8%-10% and spontaneous VA incidence in diabetic patients was observed, rather than the diabetic condition and independent from QT prolongation, stating that suboptimal glycemic control and persistent hyperglycemia is related with higher risk of spontaneous VA. On the other hand, in another randomized prospective study, link between hypoglycemic episodes and VA in patients with type 2 DM and documented CVD is investigated[4]. In this study, there were 30 patients treated either with insulin and/or sulfonylureas (SU) and there was an age matched control group of 12 patients treated with anti hyperglycemic agents with low risk of hypoglycemia. There were high incidence of hypoglycemia and silent VA in the insulin and/or SU group comparing to control subjects. A study from Pistrosch et al[5] further analyzed effects of hypoglycemia as a trigger for VA in larger patient cohort with type 2 DM revealed that hypoglycemia might be able to trigger VA and interestingly a tiroid stimulating hormone level in the low-normal range, which indicates subclinical hypertiroidism, is indepently associated with occurrence of VA. Although these two studies provide no casual relationship between hypoglycemia and VA in diabetic patients, it may be postulated that hypoglycemia may be triggering VA either with sympathetic overstimulation or QT prolongation[36].
Interestingly, another study investigating the association between diabetes and VA in patients with severe heart failure revealed a negative independent relationship with diabetes and VA in this patient group. Moreover, the authors concluded that DM might have a protective effect for the occurrence of VA in the setting of decompensated heart failure[37].
In summary, DM might play a critical role in creating a vulnerable substrate and/or as a trigger for VA besides the expected risk based on the high extent and incidence of coronary artery disease. Conversely, there is clinical data that claims DM has a protector effect for VA at least in certain group of patients. Unfortunately, there is not enough randomized large-scale data in the literature to suggest a definite relationship and clear pathophysiological mechanisms for this entity.
AF and VA are most common form of arrhythmias, which lead to cardiovascular complications and mortality in patients with DM. Although, there are an evidence based risk factors for an arrhythmogenic substrate that may be specifically related to diabetes, such as heterogeneities in atrial and ventricular repolarization, the extend of myocardial damage, scar formation, autonomic system distortion, glucose fluctuations as well as structural and electrical alterations, the causal pathophysiological and electrophysiological mechanisms are warranted in further studies.
P- Reviewer: Carbucicchio C, De Ponti R, Kettering K S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Garcia MJ, McNamara PM, Gordon T, Kannel WB. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study. Diabetes. 1974;23:105-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1146] [Cited by in RCA: 1038] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 2. | Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1974] [Cited by in RCA: 1996] [Article Influence: 64.4] [Reference Citation Analysis (0)] |
| 3. | Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011;108:56-62. [PubMed] |
| 4. | Stahn A, Pistrosch F, Ganz X, Teige M, Koehler C, Bornstein S, Hanefeld M. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: silent hypoglycemias and silent arrhythmias. Diabetes Care. 2014;37:516-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 5. | Pistrosch F, Ganz X, Bornstein SR, Birkenfeld AL, Henkel E, Hanefeld M. Risk of and risk factors for hypoglycemia and associated arrhythmias in patients with type 2 diabetes and cardiovascular disease: a cohort study under real-world conditions. Acta Diabetol. 2015;52:889-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Ball J, Carrington MJ, McMurray JJ, Stewart S. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol. 2013;167:1807-1824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 467] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 7. | Movahed MR, Hashemzadeh M, Jamal MM. Diabetes mellitus is a strong, independent risk for atrial fibrillation and flutter in addition to other cardiovascular disease. Int J Cardiol. 2005;105:315-318. [PubMed] |
| 8. | Burstein B, Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol. 2008;51:802-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 828] [Cited by in RCA: 938] [Article Influence: 55.2] [Reference Citation Analysis (0)] |
| 9. | Corradi D. Atrial fibrillation from the pathologist’s perspective. Cardiovasc Pathol. 2006;23:71-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Kato T, Yamashita T, Sekiguchi A, Sagara K, Takamura M, Takata S, Kaneko S, Aizawa T, Fu LT. What are arrhythmogenic substrates in diabetic rat atria? J Cardiovasc Electrophysiol. 2006;17:890-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 106] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Dudley SC, Hoch NE, McCann LA, Honeycutt C, Diamandopoulos L, Fukai T, Harrison DG, Dikalov SI, Langberg J. Atrial fibrillation increases production of superoxide by the left atrium and left atrial appendage: role of the NADPH and xanthine oxidases. Circulation. 2005;112:1266-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 282] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 12. | Anderson EJ, Kypson AP, Rodriguez E, Anderson CA, Lehr EJ, Neufer PD. Substrate-specific derangements in mitochondrial metabolism and redox balance in the atrium of the type 2 diabetic human heart. J Am Coll Cardiol. 2009;54:1891-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 343] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 13. | Twigg SM, Cao Z, MCLennan SV, Burns WC, Brammar G, Forbes JM, Cooper ME. Renal connective tissue growth factor induction in experimental diabetes is prevented by aminoguanidine. Endocrinology. 2002;143:4907-4915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 101] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Kato T, Yamashita T, Sekiguchi A, Tsuneda T, Sagara K, Takamura M, Kaneko S, Aizawa T, Fu LT. AGEs-RAGE system mediates atrial structural remodeling in the diabetic rat. J Cardiovasc Electrophysiol. 2008;19:415-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 15. | Pop-Busui R. Cardiac autonomic neuropathy in diabetes: a clinical perspective. Diabetes Care. 2010;33:434-441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 316] [Cited by in RCA: 330] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 16. | Otake H, Suzuki H, Honda T, Maruyama Y. Influences of autonomic nervous system on atrial arrhythmogenic substrates and the incidence of atrial fibrillation in diabetic heart. Int Heart J. 2009;50:627-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 17. | Negishi K, Seicean S, Negishi T, Yingchoncharoen T, Aljaroudi W, Marwick TH. Relation of heart-rate recovery to new onset heart failure and atrial fibrillation in patients with diabetes mellitus and preserved ejection fraction. Am J Cardiol. 2013;111:748-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Heijman J, Voigt N, Nattel S, Dobrev D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res. 2014;114:1483-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 515] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 19. | Chao TF, Suenari K, Chang SL, Lin YJ, Lo LW, Hu YF, Tuan TC, Tai CT, Tsao HM, Li CH. Atrial substrate properties and outcome of catheter ablation in patients with paroxysmal atrial fibrillation associated with diabetes mellitus or impaired fasting glucose. Am J Cardiol. 2010;106:1615-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Acar G, Akcay A, Sokmen A, Ozkaya M, Guler E, Sokmen G, Kaya H, Nacar AB, Tuncer C. Assessment of atrial electromechanical delay, diastolic functions, and left atrial mechanical functions in patients with type 1 diabetes mellitus. J Am Soc Echocardiogr. 2009;22:732-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 21. | Watanabe M, Yokoshiki H, Mitsuyama H, Mizukami K, Ono T, Tsutsui H. Conduction and refractory disorders in the diabetic atrium. Am J Physiol Heart Circ Physiol. 2012;303:H86-H95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 22. | Lip GY, Varughese GI. Diabetes mellitus and atrial fibrillation: perspectives on epidemiological and pathophysiological links. Int J Cardiol. 2005;105:319-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Saito S, Teshima Y, Fukui A, Kondo H, Nishio S, Nakagawa M, Saikawa T, Takahashi N. Glucose fluctuations increase the incidence of atrial fibrillation in diabetic rats. Cardiovasc Res. 2014;104:5-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 24. | Huxley RR, Alonso A, Lopez FL, Filion KB, Agarwal SK, Loehr LR, Soliman EZ, Pankow JS, Selvin E. Type 2 diabetes, glucose homeostasis and incident atrial fibrillation: the Atherosclerosis Risk in Communities study. Heart. 2012;98:133-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 164] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 25. | Fatemi O, Yuriditsky E, Tsioufis C, Tsachris D, Morgan T, Basile J, Bigger T, Cushman W, Goff D, Soliman EZ. Impact of intensive glycemic control on the incidence of atrial fibrillation and associated cardiovascular outcomes in patients with type 2 diabetes mellitus (from the Action to Control Cardiovascular Risk in Diabetes Study). Am J Cardiol. 2014;114:1217-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 26. | Thomas N, Scanlon J, Ahmed M. Supraventricular tachycardia in association with diabetic ketoacidosis. B J Diabetes Vasc Dis. 2007;7:244-245. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Fox CS, Coady S, Sorlie PD, Levy D, Meigs JB, D’Agostino RB, Wilson PW, Savage PJ. Trends in cardiovascular complications of diabetes. JAMA. 2004;292:2495-2499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 420] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 28. | Cho E, Rimm EB, Stampfer MJ, Willett WC, Hu FB. The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol. 2002;40:954-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 150] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 29. | Balkau B, Jouven X, Ducimetière P, Eschwège E. Diabetes as a risk factor for sudden death. Lancet. 1999;354:1968-1969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Wheeler SG, Ahroni JH, Boyko EJ. Prospective study of autonomic neuropathy as a predictor of mortality in patients with diabetes. Diabetes Res Clin Pract. 2002;58:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Cardoso CR, Salles GF, Deccache W. Prognostic value of QT interval parameters in type 2 diabetes mellitus: results of a long-term follow-up prospective study. J Diabetes Complications. 2003;17:169-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Molon G, Costa A, Bertolini L, Zenari L, Arcaro G, Barbieri E, Targher G. Relationship between abnormal microvolt T-wave alternans and poor glycemic control in type 2 diabetic patients. Pacing Clin Electrophysiol. 2007;30:1267-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 33. | Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115:387-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 816] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 34. | Faerman I, Faccio E, Milei J, Nuñez R, Jadzinsky M, Fox D, Rapaport M. Autonomic neuropathy and painless myocardial infarction in diabetic patients. Histologic evidence of their relationship. Diabetes. 1977;26:1147-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 90] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Chen-Scarabelli C, Scarabelli TM. Suboptimal glycemic control, independently of QT interval duration, is associated with increased risk of ventricular arrhythmias in a high-risk population. Pacing Clin Electrophysiol. 2006;29:9-14. [PubMed] |
| 36. | Laitinen T, Lyyra-Laitinen T, Huopio H, Vauhkonen I, Halonen T, Hartikainen J, Niskanen L, Laakso M. Electrocardiographic alterations during hyperinsulinemic hypoglycemia in healthy subjects. Ann Noninvasive Electrocardiol. 2008;13:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 37. | Aronson D, Burger AJ. Diabetes and the occurrence of ventricular arrhythmic events in patients with severe left ventricular dysfunction. Diabetologia. 2002;45:1440-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |