Published online Apr 15, 2015. doi: 10.4239/wjd.v6.i3.534
Peer-review started: July 30, 2014
First decision: October 14, 2014
Revised: January 2, 2015
Accepted: January 15, 2015
Article in press: January 19, 2015
Published online: April 15, 2015
Processing time: 264 Days and 16.5 Hours
AIM: To evaluate the long-term effect of aerobic and/or anaerobic exercise on glycemic control in youths with type 1 diabetes.
METHODS: Literature review was performed in spring and summer 2014 using PubMed/MEDLINE, Google Scholar, Scopus, and ScienceDirect with the following terms: aerobic, anaerobic, high-intensity, resistance, exercise/training, combined with glycemic/metabolic control, glycated haemoglobin A1c (HbA1c) and type 1 diabetes. Only peer-reviewed articles in English were included published in the last 15 years. It was selected from 1999 to 2014. Glycemic control was measured with HbA1c. Studies with an intervention lasting at least 12 wk were included if the HbA1c was measured before and after the intervention.
RESULTS: A total of nine articles were found, and they were published between the years of 2002-2011. The sample size was 401 diabetic youths (166 males and 235 females) with an age range of 10-19 years except one study, in which the age range was 13-30 years. Study participants were from Australia, Tunisia, Lithuania, Taiwan, Turkey, Brazilia, Belgium, Egypt and France. Four studies were aerobic-based, four were combined aerobic and anaerobic programs, and one compared aerobic exercise to anaerobic one. Available studies had insufficient evidence that any type of exercise or combined training would clearly improve the glycemic control in type 1 diabetic youth. Only three (two aerobic-based and one combined) studies could provide a significant positive change in glycemic control.
CONCLUSION: The regular physical exercise has several other valuable physiological and health benefits that justify the inclusion of exercise in pediatric diabetes treatment and care.
Core tip: Diabetic patients should be aware that exercise interferes with the glucose homeostasis. Anaerobic exercise can increase glycemia, whereas the aerobic exercise may cause a decrease during the exercise and post-exercise. By evaluating the long-term effect of exercise on glycemic control in type 1 diabetic youths according to the major metabolic pathway involved in energy utilization (aerobic or anaerobic), we found insufficient evidence in the latest literature that any type of exercise or combined aerobic and anaerobic training would clearly improve the glycemic control. The regular physical exercise has several other valuable benefits that justify the inclusion of exercise in pediatric diabetes treatment and care.
- Citation: Lukács A, Barkai L. Effect of aerobic and anaerobic exercises on glycemic control in type 1 diabetic youths. World J Diabetes 2015; 6(3): 534-542
- URL: https://www.wjgnet.com/1948-9358/full/v6/i3/534.htm
- DOI: https://dx.doi.org/10.4239/wjd.v6.i3.534
Physiological, social and emotional benefits of regular exercise and physically active lifestyle are well documented mostly in a healthy population[1-4], but they are also important for diabetic patients regardless of the type of diabetes[5-8]. For type 1, successful diabetes management is based on individualized insulin therapy, adjusted diet and regular exercise[9].
Exercise used as prevention and therapy in diabetes is not a new concept in the literature. Even the ancient Ayurvedic physician, Susruta Shamita (born around 600 B.C.), noted the reduction in the sweetness of urine from diabetic patients with excecise, and included moderate exercise within his treatment regimens[10]. In 1919, Allen proved that exercise reduced blood glucose level and improved acutely the tolerance to a carbohydrate load[11]. After the discovery of insulin in 1921[12], Lawrence demonstrated that exercise has an effect on insulin requirements and glucose uptake[13]. Joslin believed in “troika” (group of three) in the treatment of diabetes, symbolizing insulin, diet and exercise correlation[14]. Regular exercise helps to improve overall health and fitness, and reduces risk factors for vascular complications. Diabetic youths with regular exercise have improved blood lipid profile, and increased insulin sensitivity, primarily in the skeletal muscles, which leads to a reduced need for insulin[15-17]. The American Diabetes Association recommends all levels of physical exercise including leisure activities, recreational sport and competitive sport for youths with type 1 diabetes mellitus (T1DM) if they are in good blood glucose control and have no long-term complications[18]. Until the sympathetic nervous and endocrine systems control the blood glucose level at the physiological levels during and after physical exercise in healthy subjects[19], the regulation is external in diabetic patients considering many internal influences. Youths with T1DM should be aware that exercise interferes with the glucose homeostasis, although there are individual differences in blood glucose response due to type, duration and intensity of the exercise, the pre-exercise level of counterregulatory hormones, and blood glucose concentrations[20,21]. Several studies examined the role of physical activity and exercise in the treatment of T1DM and considered it an important component. The evidence for improvement in glycemic control is equivocal. Some studies suggest a positive effect[22-27], whereas others fail to show this effect[28-34]. Scientific questions remain concerning what is the exact effect of different types of exercise on glycemic control in youths with T1DM.
In this systematic literature review, we evaluated the latest studies examining the long-term effect of aerobic and/or anaerobic exercise on glycemic control in youths with T1DM. We also made distinguishing between concepts of physical activity, physical fitness, and aerobic-anaerobic exercise. Finally, we considered clinical applications and future directions.
Physical activity: Physical activity encompasses body movement produced by skeletal muscles which requires energy consumption[35]. Physical activity can range from sports to any other lifestyle activities including school and out-of-school activities, weekend activities where youths play, are active and expend energy. There is evidence that behavioural patterns of physical activity in childhood are maintained throughout adulthood[36,37]. This term is often used interchangeably with regular exercise and physical fitness in studies, although they are different concepts[38].
Exercise: Exercise has been defined as any form of body movement that results in an increase in metabolic demand with the intention of developing one or more components of physical fitness. It is generally planned, structured and systematic[35]. Regular exercise improves physical fitness. Exercise is characterised by five components: type [dynamic (isotonic) or static (isometric), and both of them can be performed aerobically or anaerobically on the basis of energy utilization][39], intensity (degree of effort that individual puts into exercise), duration (the length of each training session), repetition (number of times individual performs a complete movement of a given exercise) and frequency (number of exercise sessions per week)[40].
Fitness: Fitness refers to the “possession of adequate levels of strength, endurance, and mobility to provide for successful participation in occupational effort, recreational pursuits, familial obligation, and that is consistent with a functional phenotyp expression of the human genotype”[41]. Physical fitness determines cardiovascular, respiratory, and musculosceletal systems in order to perform physically demanding activities such as exercise, sport, or work. Fit youth has normal body fat, good immune system and, in general, is in a physiologic state of well-being.
Aerobic-anaerobic exercise: Whether an activity is aerobic or anaerobic depends primarily on its intensity and duration. Most physical exercises are characterised by both static and dynamic contractions as well as aerobic and anaerobic metabolism. Thus, exercise is classified by their dominant features.
Aerobic exercise includes any type of exercise, typically those performed at moderate levels of intensity for extended periods of time that maintains an increased heart rate. Activities such as cycling, swimming, jogging, rowing, cross-country skiing, and aerobic dancing require oxygen to produce ATP. Regular aerobic exercise improves maximal oxygen consumption and overall endurance performances. Anaerobic exercise is used to promote strength, power, and speed. Generally, anaerobic exercise has a short duration and high intensity activity. Unlike aerobic exercise, it does not depend on exogenous oxygen. Activities such as heavy weightlifting, all types of sprint (running, cycling, or swimming) or any hard exercises require anaerobic metabolism. During exercise various forms of energy sources are utilized markedly depending on the intensity and duration of exercise, but the activity is classified typically based on the predominantly used system. The anaerobic energy system is used for resistance training and increasing speed[42]. During high intensity (anaerobic) exercise almost the entire metabolic fuel source is glucose, whereas during low intensity (aerobic) exercise fat utilization increases and glucose oxidation decrease[43]. Both types of exercise increase the mechanical efficiency of the heart (cardiac adaptation), changes in morphology and functionality of the left ventricle[44].
Measuring the intensity of exercise using maximal heart rate: Maximal heart rate (HRmax) is one of the most commonly used values in clinical settings and physiology. HR increases nearly linearly with the increase in the intensity of exercise; and this is the simplest physiological response to measure. As maximal exercise intensity is approached, HR begins to plateau even as the exercise workload continues to increase. This HRmax is a reliable value and it remains constant for a longer period[45]. To estimate HRmax for children, formula 208 - 0.7 × age in years is applied[46,47]. There are several more and less accurate types of estimation existing for determining the exercise intensity[48]. Aerobic training zone is around between 60%-70% of the HRmax. Between 70%-85% of HRmax, the youths are in the mixed zone, and above 85% of HRmax the anaerobic metabolism will come to the fore.
Different types of exercise produce different effects on blood glucose level. If the carbohydrate intake and the insulin dosage are not in line with the exercise the patient does, it will result in metabolic disturbances[49]. The most common problems are the evaluation of pre-exercise level of blood glucose, evaluation of the intensity and duration of the expected exercise, and to take into consideration the time of day when the patient exercises, because of the body’s different physiological insulin need[49]. Exercise functions like insulin, so the balance between the insulin therapy and diet could be facilitated if the daily schedule for exercise and the exercise parameters are consistent[50], although this goal is almost impossible to obtain in the real life for youths. Findings from exercise training studies support the concept that moderate intensity aerobic workload increases the risk of hypoglycemia during the exercise and several hours after the exercise. High-intensity training with anaerobic utilization may increase the blood glucose level due to the release of adrenaline and noradrenalin in the blood, which then stimulates the liver to release glucose faster than normal. The exercise-induced rise in glucose level is followed by hypoglycemia after hours of finishing the exercise as counterregulatory hormone levels decrease[21,51-53]. Both aerobic and anaerobic exercise training regimens improve glucose uptake and insulin sensitivity[21,54]. School-aged children engage a combination of moderate- and high-intensity sessions in their everyday sport activities. Their exercise is often spontaneous and unplanned. Thus, a different plan is needed for each type of exercise to optimize blood glucose level, but problems with the management are well recognised. Patients differ in tolerance to exercise and insulin requirements and it is impossible to give precise guidelines suitable for everyone with T1DM, therefore experiences with regular blood glucose testing are inevitable. Continuous glucose monitoring may assist the active diabetic participants to follow the changes in blood glucose level and give information about the individual response to the exercise[21,54]. There are several guidelines to discuss safe sport participation in children and adolescents with T1DM[5,55-59]. These guidelines can be adjusted to own measurements and awareness of the usual responses to a particular type of exercise.
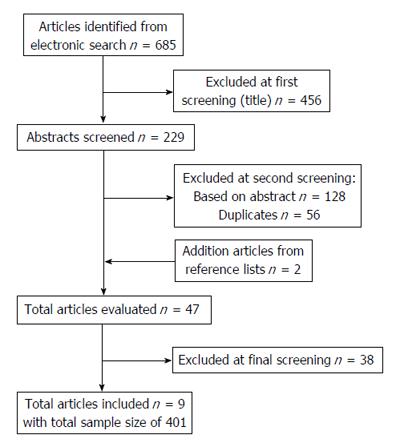
A systematic review was performed in spring and summer 2014 using PubMed/Medline, Google Scholar, Scopus, and ScienceDirect with the following terms: aerobic, anaerobic, high-intensity, resistance, exercise/training, combined with glycemic/metabolic control and type 1 diabetes. Only peer-reviewed articles in English were included published in the last 15 years with at least five subjects per group. Studies were selected from 1999 to 2014 that measured the long-term effect of aerobic and/or anaerobic exercise on glycemic control in type 1 diabetic children, adolescents and young adults without diabetes complications. Glycemic control was measured with glycated haemoglobin A1c (HbA1c). As the HbA1c provides an average of blood glucose control over a 12-wk period, we included studies with an intervention lasting at least 12 wk if the HbA1c was measured before and after the intervention. The flow diagram of study selection is shown in Figure 1.
This manuscript does not describe basic or clinical research using biostatistics for raw data, therefore biostatistics statement is not relevant.
A total of nine articles was evaluated from nine different countries including Australia[30], Tunisia[60], Lithuania[61], Taiwan[62], Turkey[63], Brazilia[64], Belgium[65], Egypt[66] and France[67], and they were published between the years of 2002-2011. The list of articles is presented in Table 1. Across included studies the total sample size was 401 (166 males and 235 females) with an age range of 10-19 years except one study, in which the age range was 13-30 years[64]. Four studies were aerobic-based[60-63], four were combined aerobic and anaerobic programs[30,65-67], and one compared aerobic exercise to anaerobic one[64]. The Turkish study[63] conducted a Pilates program that is considered low-impact aerobic workout[68]. All studies had diabetic control group except one[61].
| Source | RCT | Objective | Sample size/gender | Age (y/o) gender | Intervention | Duration, frequency | Significant positive change in GC |
| Aouadi et al[60], (2011) Tunisian | No | Effect of aerobic training on glycemic control and lipid profile | EG1: 11 (twice) EG2: 11 (4 times) DC: 11 no exerc | 12-14 33 M | Supervised aerobic exercise | 3 and 6 mo, twice vs four times a week (60 min) | Yes, but only 6 mo with four times a week duration |
| Sideraviciūte et al[61], (2006) Lithuanian | No | Effect of long-term physical activity in water on glucose control | EG: 19 (HC: 21) | 14-19 19 F | Supervised aerobic exercise | 14 wk, twice a week (45 min) | Yes |
| Wong et al[62], (2010) Taiwan | No | Effect of home-based exercise programme on HbA1c and peak oxygen uptake | EG: 12 video-, 5 self directed DC: 11 | 7-17 8 M, 20 F | Unsupervised aerobic exercise | 12 wk, three times a week (30 min) | No |
| Tunar et al[63], (2012) Turkish | Yes | Effect of pilates training on metabolic control and physical performance | EG: 17 DC: 14 | 12-17 15 M, 16 F | Supervised aerobic exercise | 12 wk, three times a week (40 min) | No |
| Ramalho et al[64], (2006) Brazilian | Yes | Effect of aerobic vs resistance training on metabolic control | EG: 7 DC: 6 | 13-30 3 M, 10 F | Both aerobic and anaerobic exercise were supervised | 12 wk, three times a week (40 min) | Sig. increase in aerobic group, not sig. decrease in anaerobic group |
| D'hooge et al[65], (2011) Belgian | Yes | Effect of combined exercise training on metabolic control, physical fitness and quality of life | EG: 8 DC: 8 | 10-17 7 M, 9 F | Supervised combined exercise | 20 wk, twice a week (70 min) | No |
| Roberts et al[30], (2002) Australian | Yes | Whether the change of the glycemic control after intervention is dependent on the initiation of quality of glycemic control | EG1: 12 HbA1c > 9% EG2: 12 HbA1c < 9% DC1: 12 HbA1c > 9% DC2: 12 HbA1c < 9% | Circa 11-17 24 M, 24 F | 12 wk supervised 12 wk unsuper-vised combined exercise | 24 wk, three times a week (45 min) | No |
| Salem et al[66], (2010) Egyptian | Yes | Effect of exercise on glycemic control, plasma lipids, blood pressure, severity and frequency of hypoglycemia, anthropometric measurements and insulin dose | EG1: 75 (once) EG2: 73 (3 times) DC: 48 | 12-18 76 M, 121 F | Supervised combined exercise | 6 mo, once and three times a week (70 min) | Yes, in both exercise groups |
| Heyman et al[67], (2007) French | Yes | Effect of exercise on quality of life, physical fitness, body composition, lipid and apolipoprotein profiles, and adiponectin and leptin levels | EG: 9 DC: 7 | 13-18 16 F | Supervised combined exercise | 6 mo, 2 h supervised, and 1 h unsupervised | No |
Studies investigating aerobic exercise: Studies measuring the effect of aerobic exercise on glycemic control presented variable results[60-63]. Only one study recognised a significant improvement in HbA1c after 12-wk exercise (girls swimming twice a week for 45 min a week)[61]. In a study investigating the impact of the frequency of the supervised aerobic training on glycemic control, exercise three times a week (one hour) for three months had no significant impact on glycemic control, but exercise four times a week (one hour) for 6 mo resulted in a significant improvement[60]. Neither guided or self-directed home-based aerobic exercise program nor supervised Pilates exercise had a significant effect on glycosylated haemoglobin after a 12-wk session[62,63].
Study investigating anaerobic exercise: We found only one study that measured the efficacy of resistance (anaerobic) and aerobic exercise in parallel. Both groups were trained three times a week (40 min) for 12 wk under supervision by a physical trainer and an endocrinologist. Interestingly, the HbA1c increased in the aerobic group significantly after 12 wk, whereas a non-significant reduction was observed in the resistance training group[64].
Studies investigating combined exercise program: Four randomised controlled trials examined the effect of combined (aerobic and anaerobic) exercise on glycemic control[30,65-67]. Supervised combined aerobic and resistance training twice a week (70 min) for 20 wk resulted in no significant change in glycemic control[65]. In a 12-wk supervised training followed by a 12-wk unsupervised training, HbA1c level remained unchanged regardless of the baseline HbA1c level[30]. There were two trials that explored the effect of supervised combined exercise on glycemic control for a longer duration (6 mo)[66,67]. The Egyptian study found significant improvements in HbA1c level in both training groups exercising three times a week and once a week. However, patients exercising three times a week produced significantly greater improvements[66]. In the Heyman’s study, the participants completed a two-hour supervised training and a one-hour unsupervised training a week including aerobic and strength exercises. The author could not prove a significant effect on glycated hemoglobin after a 6-mo session[67].
The primary aim of diabetes treatment and care is to achieve as stable glycemic control as possible in order to prevent or delay the long-term complications[69]. Regular exercise is recommended for diabetic youths for several psychological and health benefits[7,70]. It is evidence-based that regular exercise has a preventive and curative role in type 2 diabetes, but its physiological role in type 1 diabetes is not fully explored. Exercise physiology in diabetes is described thoroughly by Robertson et al[7] and Riddell et al[53,59]. Another issue that remains unresolved is related to the type of exercise: aerobic or anaerobic workout is most beneficial for glycemic control. We evaluated the studies from the previous 15 years that investigated the long-term effect of exercise on glycemic control in youths with T1DM according to the major metabolic pathway involved in energy utilization (predominantly aerobic or predominantly anaerobic). Results of investigated studies are open to debate. Most studies found no significant improvement in glycemic control regarding the aerobic[62,63] and combined exercise intervention[30,65,67]. The only study investigating the anaerobic effect on glycemic control presented a positive tendency, although there was no statistically significant effect[64]. One of the possible reasons for these varied results could be the small sample sizes. The glucose profile varies greatly in patients with T1DM before, during and after exercise, and can be very different in patients with similar HbA1c. All except one study[66] had less than 20 participants in a group in our studies. The other reason could be the short period. It seems that at least 6 mo of exercise intervention might lead to significant results[60,66]. Kennedy et al[71] also noticed in their systematic review and meta-analysis that longer duration of intervention shows a trend for HbA1c reduction. We had a total of 401 samples in our studies and the Egyptian study[66] alone offered 187 participants. Weighting its results, it might be supposed that combined long-term exercise intervention is more beneficial for the glycemic control, than aerobic or anaerobic alone. Irvine et al[72] in their systematic review with 372 patients with T2DM have reported that (anaerobic) progressive resistance exercise is not significantly better than aerobic exercise in improving glycosylated haemoglobin. There was a lack of evidence to suggest that one type of exercise was better than another[72]. Yang et al[73] in their systematic review with 595 patients with T2DM also enunciated that either form of exercise appears to have comparable effects on glycemic control. A meta-analysis by Tonoli et al[74] with type 1 diabetic participants explored a tendency for improvement in glycaemic control due to aerobic or combined training, but they could not confirm this statistically. Individual studies on aerobic training had no significant evidence, but “in total” demonstrated a reduction in HbA1c, although they carefully interpret their results because of insufficient data on these topics[74]. Neither Kennedy’s meta-analysis in children and adults[71] nor Kavookjian’s systematic review in the adult population[75] revealed evidence for statistically significant glycemic benefits of exercise. Kennedy et al[71] suggest that HbA1c may not be a sensitive indicator of glycaemic control, and that improvement in glycaemic variability may not be reflected in this measure. Tight metabolic control is very important for diabetic individuals, and the regular physical exercise is part of the diabetes management. Available studies provide insufficient evidence that any type of exercise or combined training would clearly improve the glycemic control in type 1 diabetic young patients. Long-term exercise-induced glycemic benefits are based on the continuous effect of each successive bout of exercise. Glycemic variability can be detected by continuous glucose monitoring that could help individuals to learn their own response to different type of physical exercise; and it might be a more appropriate marker to explore the exercise-induced beneficial effect than HbA1c[71]. Youths with T1DM are recommended to be engaged in a sport they like, and do it regularly as much as possible at the same period of the day. Having the appropriate exercise physiology knowledge, they can accumulate own experiences regarding exercise in addition to insulin requirement and dietary program that may result in stable glucose levels. The insulin-diet-exercise adjustment must be personalized and discussed with the patient’s endocrinologist. The regular exercise is associated with numerous health benefits and chronically ill youths enjoy the same benefits as the healthy counterparts[1,70].
There are miscellaneous results regarding the long-term effect of various forms of exercise on glycemic control. Meta-analyses also suffered from the insufficient randomised controlled trials with greater sample sizes to examine the short- and long-term effect of glycemic control on different exercise modalities in youths with T1DM. Patients and health professionals may want more information they currently received, but there are concerns that the results would be overestimated. Different forms of exercise generate different skills in youths. They need a comprehensive form of exercise to help their healthy many-sided physical development. Diabetic patients should be aware that glycemic control is influenced by multiple factors (initial blood glucose level, insulin absorption, time of the day), and shows individual responses to exercise. It is advisable that young patients choose some kind of sports or physical exercise they like and be engaged with it for a longer time. Clinical treatment and management should be adjusted to the exercise form and the diabetic patients should acquire how to change nutrition and insulin dose according to their daily physical exercise. Patients who can monitor themselves intensively around periods of activity can learn how to keep glucose levels in an acceptable range.
Although current studies have insufficient evidence of the beneficial effect of any type of exercise on glycemic control, any type of regular physical exercise has several other valuable physiological and health benefits that justify the inclusion of exercise in pediatric diabetes treatment and care.
This research was partially carried out with the contribution of the Workgroup for Health Sciences, Center of Excellence of Applied Materials Science and Nano-Technology at the University of Miskolc.
Regular exercise is recommended for diabetic youth for several psychological and health benefits, but its physiological role in type 1 diabetes is not fully explored. So far, there are only few studies evaluating the long-term effect of different types of exercise on glycemic control.
In this systematic literature review, the authors evaluated the latest studies examining the long-term effect of aerobic and/or anaerobic exercise on glycemic control in youths with type 1 diabetes. They also made distinguishing between concepts of physical activity, physical fitness, and aerobic-anaerobic exercise.
Most studies found no significant improvement in glycemic control regarding the aerobic and combined exercise intervention. The only one study evaluating anaerobic exercise observed a non-significant reduction in glycemic control. It might be supposed that longer duration (at least 6 mo) and more frequent (more than twice a week) exercise has a positive effect on glycemic control, but it is not proved yet.
Although current studies have insufficient evidence of the beneficial effect of any type of exercise on glycemic control, any type of regular physical exercise has several other valuable physiological and health benefits that justify the inclusion of exercise in pediatric diabetes treatment and care.
Aerobic exercise includes any type of exercise, typically those performed at moderate levels of intensity for extended periods of time that maintains an increased heart rate. Anaerobic exercise is used to promote strength, power, and speed. Generally, it has a short duration and high intensity activity. Unlike aerobic exercise, it does not depend on exogenous oxygen.
The manuscript covers an important topic in type 1 diabetes management. The contribution that the manuscript provides is an overview of the dearth of scientific evidence to support exercise intervention in this population.
P- Reviewer: Faulkner MS, Sanlioglu AD S- Editor: Ji FF L- Editor: Wang TQ E- Editor: Liu SQ
| 1. | Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2341] [Cited by in RCA: 2502] [Article Influence: 166.8] [Reference Citation Analysis (0)] |
| 2. | Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, Goldfield G, Connor Gorber S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1382] [Cited by in RCA: 1218] [Article Influence: 87.0] [Reference Citation Analysis (0)] |
| 3. | Downward P, Rasciute S. Does sport make you happy? An analysis of the well being derived from sports participation. Int Rev Appl Econ. 2011;25:331-348. [DOI] [Full Text] |
| 4. | Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1105] [Cited by in RCA: 902] [Article Influence: 75.2] [Reference Citation Analysis (0)] |
| 5. | Zinman B, Ruderman N, Campaigne BN, Devlin JT, Schneider SH. Physical activity/exercise and diabetes mellitus. Diabetes Care. 2003;26 Suppl 1:S73-S77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 192] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Giannini C, de Giorgis T, Mohn A, Chiarelli F. Role of physical exercise in children and adolescents with diabetes mellitus. J Pediatr Endocrinol Metab. 2007;20:173-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Robertson K, Adolfsson P, Scheiner G, Hanas R, Riddell MC. Exercise in children and adolescents with diabetes. Pediatr Diabetes. 2009;10 Suppl 12:154-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Leclair E, de Kerdanet M, Riddell M, Heyman E. Type 1 Diabetes and Physical Activity in Children and Adolescents. J Diabetes Metab. 2013;S10:004. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28:186-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 917] [Cited by in RCA: 873] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 10. | Tipton CM. Susruta of India, an unrecognized contributor to the history of exercise physiology. J Appl Physiol (1985). 2008;104:1553-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Allen FM. Note concerning exercise in the treatment of severe diabetes. Boston Med Surg J. 1915;173:743-744. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 12. | Banting FG, Best CH, Collip JB, Campbell WR, Fletcher AA. Pancreatic extracts in the treatment of diabetes mellitus. 1922. Indian J Med Res. 2007;125:141-146. [PubMed] |
| 13. | Lawrence RD. The Effect of Exercise on Insulin Action in Diabetes. Br Med J. 1926;1:648-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Joslin EP. The Prevention of Diabetes Mellitus. JAMA. 1922;76:79-84. [RCA] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Herbst A, Bachran R, Kapellen T, Holl RW. Effects of regular physical activity on control of glycemia in pediatric patients with type 1 diabetes mellitus. Arch Pediatr Adolesc Med. 2006;160:573-577. [PubMed] |
| 16. | Miculis CP, Mascarenhas LP, Boguszewski MC, Campos Wd. Physical activity in children with type 1 diabetes. J Pediatr (Rio J). 2010;86:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Schmitz KH, Jacobs DR, Hong CP, Steinberger J, Moran A, Sinaiko AR. Association of physical activity with insulin sensitivity in children. Int J Obes Relat Metab Disord. 2002;26:1310-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | American Diabetes Association. Physical activity/exercise and diabetes mellitus. Diabetes Care. 2004;27:S58-S62. |
| 19. | Suh SH, Paik IY, Jacobs K. Regulation of blood glucose homeostasis during prolonged exercise. Mol Cells. 2007;23:272-279. [PubMed] |
| 20. | Giannini C, Mohn A, Chiarelli F. Physical exercise and diabetes during childhood. Acta Biomed. 2006;77 Suppl 1:18-25. [PubMed] |
| 21. | Riddell M, Perkins BA. Exercise and glucose metabolism in persons with diabetes mellitus: perspectives on the role for continuous glucose monitoring. J Diabetes Sci Technol. 2009;3:914-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Zoppini G, Carlini M, Muggeo M. Self-reported exercise and quality of life in young type 1 diabetic subjects. Diabetes Nutr Metab. 2003;16:77-80. [PubMed] |
| 23. | Massin MM, Lebrethon MC, Rocour D, Gérard P, Bourguignon JP. Patterns of physical activity determined by heart rate monitoring among diabetic children. Arch Dis Child. 2005;90:1223-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Valerio G, Spagnuolo MI, Lombardi F, Spadaro R, Siano M, Franzese A. Physical activity and sports participation in children and adolescents with type 1 diabetes mellitus. Nutr Metab Cardiovasc Dis. 2007;17:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Schweiger B, Klingensmith G, Snell-Bergeon JK. Physical activity in adolescent females with type 1 diabetes. Int J Pediatr. 2010;2010:328318. [PubMed] |
| 26. | Lukács A, Mayer K, Juhász E, Varga B, Fodor B, Barkai L. Reduced physical fitness in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2012;13:432-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (2)] |
| 27. | Lukács A, Mayer K, Török A, Kiss-Tóth E, Barkai L. Better cardiorespiratory fitness associated with favourable metabolic control and health-related quality of life in youths with type 1 diabetes mellitus. Acta Physiol Hung. 2013;100:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Zinman B, Zuniga-Guajardo S, Kelly D. Comparison of the acute and long-term effects of exercise on glucose control in type I diabetes. Diabetes Care. 1984;7:515-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Raile K, Kapellen T, Schweiger A, Hunkert F, Nietzschmann U, Dost A, Kiess W. Physical activity and competitive sports in children and adolescents with type 1 diabetes. Diabetes Care. 1999;22:1904-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Roberts L, Jones TW, Fournier PA. Exercise training and glycemic control in adolescents with poorly controlled type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2002;15:621-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 31. | Särnblad S, Ekelund U, Aman J. Physical activity and energy intake in adolescent girls with Type 1 diabetes. Diabet Med. 2005;22:893-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Aman J, Skinner TC, de Beaufort CE, Swift PG, Aanstoot HJ, Cameron F. Associations between physical activity, sedentary behavior, and glycemic control in a large cohort of adolescents with type 1 diabetes: the Hvidoere Study Group on Childhood Diabetes. Pediatr Diabetes. 2009;10:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Edmunds S, Roche D, Stratton G. Levels and patterns of physical activity in children and adolescents with type 1 diabetes and associated metabolic and physiologic health outcomes. J Phys Act Health. 2010;7:68-77. [PubMed] |
| 34. | Galler A, Lindau M, Ernert A, Thalemann R, Raile K. Associations between media consumption habits, physical activity, socioeconomic status, and glycemic control in children, adolescents, and young adults with type 1 diabetes. Diabetes Care. 2011;34:2356-2359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 35. | Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126-131. [PubMed] |
| 36. | Twisk JW, Kemper HC, van Mechelen W. Tracking of activity and fitness and the relationship with cardiovascular disease risk factors. Med Sci Sports Exerc. 2000;32:1455-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 188] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 37. | Mikkelsson L, Kaprio J, Kautiainen H, Kujala U, Mikkelsson M, Nupponen H. School fitness tests as predictors of adult health-related fitness. Am J Hum Biol. 2006;18:342-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Vanhees L, Lefevre J, Philippaerts R, Martens M, Huygens W, Troosters T, Beunen G. How to assess physical activity? How to assess physical fitness? Eur J Cardiovasc Prev Rehabil. 2005;12:102-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 211] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 39. | Mitchell JH, Haskell W, Snell P, Van Camp SP. Task Force 8: classification of sports. J Am Coll Cardiol. 2005;45:1364-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 454] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 40. | Rodriguez NR, Di Marco NM, Langley S. American College of Sports Medicine position stand. Nutrition and athletic performance. Med Sci Sports Exerc. 2009;41:709-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 408] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 41. | Kilgore L, Rippetoe M. Redefining fitness for health and fitness professionals. J Exerc Physiol. 2007;10:34-39. |
| 42. | Plowman S, Smith D. Exercise Physiology for Health, Fitness, and Performance. 4th ed. 2004;. |
| 43. | Romijn JA, Coyle EF, Sidossis LS, Rosenblatt J, Wolfe RR. Substrate metabolism during different exercise intensities in endurance-trained women. J Appl Physiol (1985). 2000;88:1707-1714. [PubMed] |
| 44. | Dickhuth HH, Scharhag J, Röcker K, König D. Cardiovascular adaptation and exercise. Int SportMed J. 2012;13:1-7. |
| 45. | Kenney WL, Wilmore JH, Costill DL. Physiology of Sport and Exercise. 5th ed. Human Kinetics: Champaign, IL 2011; . |
| 46. | Mahon AD, Marjerrison AD, Lee JD, Woodruff ME, Hanna LE. Evaluating the prediction of maximal heart rate in children and adolescents. Res Q Exerc Sport. 2010;81:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 47. | Machado FA, Denadai BS. Validity of maximum heart rate prediction equations for children and adolescents. Arq Bras Cardiol. 2011;97:136-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 48. | American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed. Baltimore (MD): Lippincott Williams & Wilkins 2013; 162-174. |
| 49. | Yardley JE, Kenny GP, Perkins BA, Riddell MC, Malcolm J, Boulay P, Khandwala F, Sigal RJ. Effects of performing resistance exercise before versus after aerobic exercise on glycemia in type 1 diabetes. Diabetes Care. 2012;35:669-675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 126] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 50. | Apor P. [Physical activity in prevention and treatment of diabetes]. Orv Hetil. 2009;150:579-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 51. | Francescato MP, Geat M, Fusi S, Stupar G, Noacco C, Cattin L. Carbohydrate requirement and insulin concentration during moderate exercise in type 1 diabetic patients. Metabolism. 2004;53:1126-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 52. | Guelfi KJ, Jones TW, Fournier PA. The decline in blood glucose levels is less with intermittent high-intensity compared with moderate exercise in individuals with type 1 diabetes. Diabetes Care. 2005;28:1289-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 53. | Riddell M, Perkins B. Type 1 diabetes and vigorous exercise: Applications of exercise physiology to patient management. Can J Diab. 2006;30:63-71. [RCA] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 54. | Iscoe KE, Campbell JE, Jamnik V, Perkins BA, Riddell MC. Efficacy of continuous real-time blood glucose monitoring during and after prolonged high-intensity cycling exercise: spinning with a continuous glucose monitoring system. Diabetes Technol Ther. 2006;8:627-635. [PubMed] |
| 55. | Mullooly CA, Kemmis KL. Diabetes Educators and the Exercise prescription. Diabetes Spectr. 2005;18:108-113. [DOI] [Full Text] |
| 56. | Hornsby WG, Chetlin RD. Management of competitive athletes with diabetes. Diabetes Spectr. 2005;18:102-107. [DOI] [Full Text] |
| 57. | Draznin MB. Managing the adolescent athlete with type 1 diabetes mellitus. Pediatr Clin North Am. 2010;57:829-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 58. | Gallen I. Type 1 Diabetes. Clinical management of the Athlete. 2012;73-99. [DOI] [Full Text] |
| 59. | Riddell MC, Iscoe KE. Physical activity, sport, and pediatric diabetes. Pediatr Diabetes. 2006;7:60-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 60. | Aouadi R, Khalifa R, Aouidet A, Ben Mansour A, Ben Rayana M, Mdini F, Bahri S, Stratton G. Aerobic training programs and glycemic control in diabetic children in relation to exercise frequency. J Sports Med Phys Fitness. 2011;51:393-400. [PubMed] |
| 61. | Sideraviciūte S, Gailiūniene A, Visagurskiene K, Vizbaraite D. The effect of long-term swimming program on glycemia control in 14-19-year aged healthy girls and girls with type 1 diabetes mellitus. Medicina (Kaunas). 2006;42:513-518. [PubMed] |
| 62. | Wong CH, Chiang YC, Wai JP, Lo FS, Yeh CH, Chung SC, Chang CW. Effects of a home-based aerobic exercise programme in children with type 1 diabetes mellitus. J Clin Nurs. 2011;20:681-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Tunar M, Ozen S, Goksen D, Asar G, Bediz CS, Darcan S. The effects of Pilates on metabolic control and physical performance in adolescents with type 1 diabetes mellitus. J Diabetes Complications. 2012;26:348-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 64. | Ramalho AC, de Lourdes Lima M, Nunes F, Cambuí Z, Barbosa C, Andrade A, Viana A, Martins M, Abrantes V, Aragão C. The effect of resistance versus aerobic training on metabolic control in patients with type-1 diabetes mellitus. Diabetes Res Clin Pract. 2006;72:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 65. | D’hooge R, Hellinckx T, Van Laethem C, Stegen S, De Schepper J, Van Aken S, Dewolf D, Calders P. Influence of combined aerobic and resistance training on metabolic control, cardiovascular fitness and quality of life in adolescents with type 1 diabetes: a randomized controlled trial. Clin Rehabil. 2011;25:349-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 66. | Salem MA, Aboelasrar MA, Elbarbary NS, Elhilaly RA, Refaat YM. Is exercise a therapeutic tool for improvement of cardiovascular risk factors in adolescents with type 1 diabetes mellitus? A randomised controlled trial. Diabetol Metab Syndr. 2010;2:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 67. | Heyman E, Toutain C, Delamarche P, Berthon P, Briard D, Youssef H, Dekerdanet M, Gratas-Delamarche A. Exercise training and cardiovascular risk factors in type 1 diabetic adolescent girls. Pediatr Exerc Sci. 2007;19:408-419. [PubMed] |
| 68. | Adamany K, Loigerot D. The Pilates Edge: An Athlete’s Guide to Strength and Performance. New York, USA: Penguin Group Inc 2004; 17. |
| 69. | American Diabetes Association. Standards of Medical Care in Diabetes - 2013. Diabetes Care. 2013;36:S11-S66. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2371] [Cited by in RCA: 2483] [Article Influence: 206.9] [Reference Citation Analysis (0)] |
| 70. | Chimen M, Kennedy A, Nirantharakumar K, Pang TT, Andrews R, Narendran P. What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia. 2012;55:542-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 288] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 71. | Kennedy A, Nirantharakumar K, Chimen M, Pang TT, Hemming K, Andrews RC, Narendran P. Does exercise improve glycaemic control in type 1 diabetes? A systematic review and meta-analysis. PLoS One. 2013;8:e58861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 72. | Irvine C, Taylor NF. Progressive resistance exercise improves glycaemic control in people with type 2 diabetes mellitus: a systematic review. Aust J Physiother. 2009;55:237-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 73. | Yang Z, Scott CA, Mao C, Tang J, Farmer AJ. Resistance exercise versus aerobic exercise for type 2 diabetes: a systematic review and meta-analysis. Sports Med. 2014;44:487-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 198] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 74. | Tonoli C, Heyman E, Roelands B, Buyse L, Cheung SS, Berthoin S, Meeusen R. Effects of different types of acute and chronic (training) exercise on glycaemic control in type 1 diabetes mellitus: a meta-analysis. Sports Med. 2012;42:1059-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 75. | Kavookjian J, Elswick BM, Whetsel T. Interventions for being active among individuals with diabetes: a systematic review of the literature. Diabetes Educ. 2007;33:962-988; discussion 989-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |