Published online Sep 25, 2015. doi: 10.4239/wjd.v6.i12.1223
Peer-review started: May 8, 2015
First decision: July 10, 2015
Revised: August 26, 2015
Accepted: September 7, 2015
Article in press: September 8, 2015
Published online: September 25, 2015
Processing time: 160 Days and 1 Hours
Diabetes mellitus (DM), a metabolic disorder is a major orchestra influencing brain and behavioral responses via direct or indirect mechanisms. Many lines of evidence suggest that diabetic patients apparently face severe brain complications, but the story is far from being fully understood. Type 2 diabetes, an ever increasing epidemic and its chronic brain complications are implicated in the development of Alzheimer’s disease (AD). Evidences from clinical and experimental studies suggest that insulin draws a clear trajectory from the peripheral system to the central nervous system. This review is a spot light on striking pathological, biochemical, molecular and behavioral commonalities of AD and DM. Incidence of cognitive decline in diabetic patients and diabetic symptoms in AD patients has brought the concept of brain diabetes to attention. Brain diabetes reflects insulin resistant brain state with oxidative stress, cognitive impairment, activation of various inflammatory cascade and mitochondrial vulnerability as a shared footprint of AD and DM. It has become extremely important for the investigators to understand the patho-physiology of brain complications in diabetes and put intensive pursuits for therapeutic interventions. Although, decades of research have yielded a range of molecules with potential beneficial effects, but they are yet to meet the expectations.
Core tip: This review provides a synopsis in which a metabolic disturbance becomes indispensible for life and emerges as a molecular signal defect leading to a syndrome with multiple complications. Insulin is a spotlight player which draws a trajectory from diabetes to Alzheimer’s disease with multiple divergence and convergence. We have discussed their interplay to speculate their shared molecular footprints. These biochemical and molecular commonalities provide a clue to the investigators to look inside a therapy with a common experimental and clinical platform and also provide an insight for new interventions as future perspective to find a potential stone to kill two birds together.
- Citation: Sandhir R, Gupta S. Molecular and biochemical trajectories from diabetes to Alzheimer’s disease: A critical appraisal. World J Diabetes 2015; 6(12): 1223-1242
- URL: https://www.wjgnet.com/1948-9358/full/v6/i12/1223.htm
- DOI: https://dx.doi.org/10.4239/wjd.v6.i12.1223
Every human cell relies on a complex set of programs installed during ontogeny. These programs and commands over them are the two interfaces which need faultless execution for normal body physiology. Physiology, behavior and defense are three eventful networks, which are supposed to function in synchronicity. A defect in any of these three events alters rest of two without any delay. Diabetes is a complex disorder where a molecular compromise alters the physiology with significant changes in behavioral responses.
Diabetes is associated with the production of auto-antibodies against pancreatic β-cells, i.e., type 1 diabetes (T1D) or with insulin resistance (IR), i.e., T2D[1,2]. T1D is a chronic hyperglycemic condition which affects multiple systems like brain, heart, eyes and kidneys[3]. Diabetes is found to be one of the causes of brain atrophy, mild cognitive impairment and white matter abnormalities[4-6]. In T2D insulin fails to stimulate utilization of glucose which gives rise to a phenomenon called IR. Chronic IR leads to several other complications such as lack of cellular energy, increased plasma lipids, cardiovascular problems and hypertension[7-11]. Increased risk of developing dementia and Alzheimer’s disease (AD) was suggested in T2D, which was further supported by clinical and epidemiological studies[12,13]. Diabetes patients have two fold higher risk of AD as compare to non-diabetic patients[12]. In central nervous system (CNS), presence and distribution of insulin, insulin receptors (IRs) and its substrate are region specific[14,15]. Insulin is found to play important role in learning and memory by regulating the release of neurotransmitters and synaptic plasticity[16]. It is inferred from the literature that defective insulin signaling in diabetic patients plays a crucial role in synaptic physiology[17-19]. Many other molecules participating in insulin signaling pathway have been reported to be crucial for normal physiology[20]. Remarkable presence of IRs in different brain areas has provided a clue of possible link between insulin signaling and synaptic plasticity. This fact is strongly supported by up-regulation of IRs in hippocampus after training for spatial memory task via Morris-Water Maze[21].
In 1998, a possible link between insulin dysfunction and AD was established[22,23]. The postmortem AD brains showed reduced insulin like growth factor (IGF) mRNA levels and its receptor as compared to controls[24]. Impaired peripheral glucose sensitivity[25] and elevated plasma and cerebro-spinal fluid (CSF) levels of insulin[26-28] were also reported in AD patients. Thus, there are consistent reports showing involvement of impaired insulin signaling in cognitive decline in AD patients. The role of insulin in enhancing memory performance in AD patients was confirmed by rescuing effect of intravenous and intranasal insulin administration[29,30].
Attempts are being made to unscramble the cellular and molecular mechanisms connects diabetes and AD. Present review critically examines impaired insulin signaling in diabetes as well as in AD patients with emphasis on critical molecular players such as fork head box O-1 (FOXO1), mammalian target of rapamaycin (mTOR) and glycogen synthase kinase 3 beta (GSK3β) which can be potential therapeutic targets.
Diabetes mellitus (DM), a complex metabolic disorder is characterized by hyperglycemia with several macrovascular (coronary artery disease, peripheral arterial disease, and stroke) and microvascular complications (diabetic nephropathy, neuropathy, and retinopathy)[31]. Risk of developing any of microvascular complications of diabetes depends upon both the duration and the severity of hyperglycemia. Aldose reductase, initial enzyme in the intracellular polyol pathway is a key player involved in the development of diabetic complications. Polyol pathway converts glucose into sorbitol (glucose alcohol). Hyperglycemic condition increases the flux of glucose into this pathway and results in sorbitol accumulation which further leads to osmotic stress. Osmotic stress is reported to be most common underlying mechanism in the development of microvascular complications of diabetes[31]. American Diabetes Association has categorized diabetes as T1D and T2D. T1D is characterized by autoimmune destruction of pancreatic beta cells resulting in absolute absence of insulin whereas T2D is identified by peripheral IR. According to WHO reports 2012, 90% cases of diabetes are from T2D. Clinical and experimental studies suggested strong association between diabetes and cognitive impairment[32-35]. T2D is at the edge of several risk factors such as life style, obesity, physical inactivity, gestational diabetes history as well as genetic predispositions[36,37]. The hallmark symptoms of the disease are polyurea, polydipsia, polyphagia and weight loss[38]. Mechanisms of T2D involves lipid breakdown within fat cells, elevated plasma glucagon levels as well as an increase in electrolyte retention[39].
AD is an age dependent neurodegenerative disorder associated with deposits of plaques and tangles in brain[40]. Only 1%-5% of the AD cases are found to have genetic differences and out of these cases, only 0.1% cases follow familial autosomal non-sex linked inheritance pattern[41]. AD was for the first time reported in 1906 by Alois Alzheimer, a German psychiatrist and pathologist as a progressive neurodegenerative disorder of memory loss and confusion[42]. Postmortem AD brains revealed intracellular accumulation of neurofibrillary tangles (NFTs) and extracellular deposition of amyloid beta (Aβ) plaques as two major hallmarks of AD. NFTs are hyperphosphorylated form of tau protein, which are involved in microtubule dynamics while Aβ plaques are the cleavage product of amyloid precursor protein (APP) which is a transmembrane glycoprotein of unknown function. Mutation in three genes encoding APP, presenilin 1 (PSEN1) and presenilin 2 (PSEN2) contributes to genetic cases of AD[43]. These loci are responsible for the familial type of disease while environmental factors influence sporadic form of AD with unclear etiology. Mutated form of these genes increase production of Aβ-42 protein product, a major component of senile plaques. ε4 allele of the apolipoprotein E (APOEε4) is another risk factor for AD[44,45] which is thought to contribute in neuronal lipid homeostasis, repairs injured neurons, maintains synapto-dendritic connections and scavenges neurotoxins. Loss of cholinergic system is a major cause of cognitive deficit in AD patients and the current therapies are targeted at improving cholinergic functions[46].
In 1980, first line of evidence appeared when Adolfsson et al[47] performed glucose tolerance test on AD type dementia patients and hypothesized that hypoglycemic condition can ameliorate brain status. In 1994, Razay et al[48] spotted light on disturbed glucose metabolism and hyper-insulinemia in female AD patients and tried to establish a link between insulin dysfunction and dementia. In 1996, Messier et al[23] strengthened the evidences by uncovering the potential effects of glucose on memory and cognition of AD patients. In 2003, Messier[49] further established a clear association between non-insulin dependent diabetes mellitus with neuropathy which is an incidence of vascular disease and retinopathy, he further suggested that DM is a probable risk factor for AD. Many more groups stepped ahead to address the fundamental question of whether the basic premise about the disease is true or not.
In 2005, Susanne de la Monte’s group at Brown University introduced the concept of brain diabetes or type 3 diabetes (T3D) and observed that after blocking brain insulin supply, neurons get disoriented and develops AD pathology in rats. This provided a promising platform to investigators to touch insight into T3D or brain diabetes[50]. In 2007, Li et al[50] published a review dedicated to common pathological process in AD and T2D which shared molecular degenerative cascades like dysfunction in insulin signaling pathway. In 2008, de la Monte et al[51] reappeared with some more set of explanations which were unclear in 2005. Diabetic brain was found to be compromised for acetylcholine homeostasis and cognitive impairment, whereas insulin sensitizers rescued these effects[52]. In 2009, Gotz et al[52] described the molecular commonalities between T2D and AD with hallmark feature of amylin deposition in pancreatic islets of T2D patients, whereas Aβ and NFTs deposition in AD brain which are characteristic fibrillar proteins leading to cell loss. In 2010, Saini et al[53] contributed a relevant publication to World Journal of Diabetes, establishing a molecular mechanism of IR in T2D. Crucial molecular players in these pathways came into the picture and provided new therapeutic targets. In 2011, Park[54] suggested that pathogenic alterations in insulin signaling, Aβ aggregation, oxidative stress, inflammation and glucose metabloism contributes to AD as well as DM. Streptozotocin induced diabetic rat model showed co-appearance of tau hyperphosphorylation and cognitive decline as an interesting evidence[55]. On the basis of clinical and biochemical evidences, it was further suggested that both of these diseases promote each other’s progression[56]. It has recently been found that proinflammatory signals in the brain impair insulin signaling, mitochondrial dysfunction, synaptic crosstalk as well as cognitive impairment[57].
Since 1980, many reports appeared in literature to describe the correlation between these two distinct problems with common molecular and cellular interface. Glucose metabolism and insulin signaling are major elements bridging AD and diabetes. Some relevant reports, unraveling the twin mystery of AD and DM are listed in Table 1.
| Ref. | Key findings |
| Adolfsson et al[47] | Hypoglycemic condition can ameliorate brain status in AD |
| Razay et al[48] | Disturbances in glucose metabolism and hyper-insulinemia in female AD patients are responsible for cognitive decline |
| Ruigómez et al[58] | Documented a relationship between non-insulin dependent diabetes and neuropathy |
| Li et al[50] | Defective insulin signaling is a shared degenerative cascade in disease pathology of both AD and DM |
| Ke et al[59] | Amylin deposition in pancreatic islets of T2D patients whereas, Aβ and NFTs deposition in AD brain are common hallmarks feature of diabetes and Alzheimer’s in terms of protein deposition |
| Saini[53] | Elucidated cellular and molecular mechanisms of insulin resistance and provided understanding for the molecular therapeutic targets |
| Park[54] | T2D and AD have some common pathogenic alterations like defects in insulin signaling, Aβ clearance, glucose metabolism, O-GlcNAcylation, Aβ aggregation by AGEs, inflammation, oxidative stress and circulating cortisol levels |
| Correia et al[55] | Amyloidogenesis and mitochondrial dysfunction are common denominators potentiating brain dysfunctions |
| Talbot et al[57] | Brain insulin signaling pathway including IGF-1R → IRs-2 → PI3K signaling is directly involved in AD and thus one of a causal factor in disease pathogenesis |
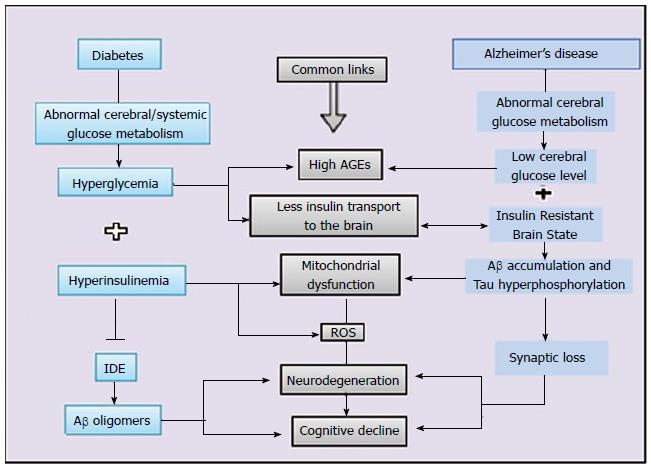
In spite of so many striking evidences, due to common interface of homeostatic mechanisms of AD and DM, the chicken or the egg question has remained unresolved. Citing all relevant findings, in 2005, first time Suzanne de la Monte has introduced insulin signaling dysfunction as a core of AD. To untangle this mystery, evidence of crosstalk between AD and DM, were put forward as crucial milestones. Patients with T2D were found to be at high risk of developing mild cognitive impairment (MCI), dementia and AD[60,61]. Similar type of evidence for MCI, dementia and AD were found in experimental models of diabetes[56,62-65]. AD brains have similar pathogenesis as observed during insulin deficiency[24,66-68]. Studies with AD patients and animal model of AD showed that intranasal insulin therapy significantly improved cognitive performance[69-71]. These clinical and experimental studies suggested that both of these disorders share common biochemical and molecular cascades[60,72,73]. Some of these common bridging elements have been schematically represented in Figure 1. Interestingly, insulin has been found to regulate Aβ and tau metabolism, which are major hallmarks of AD[74,75]. It is also evident that in T2D patients insulin signaling dysfunction accelerates AβPP (amyloid beta precursor proten)/Aβ trafficking from trans-Golgi network, a major site for Aβ generation and alters dynamicity of a Aβ synthesis[75]. Some studies report the presence of some downstream regulators of insulin signaling pathway which are involved in cleavage of AβPP at γ-secretase site, a determining site for Aβ amyloidogenicity[76]. Although, investigators found many evidences of common features in both of these disorders, the chicken or the egg question is still valid and needs parsimonious explanations. Key reports supporting AD like symptoms in DM patients and DM like symptoms in AD patients are listed in Table 2.
| Ref. | Key findings |
| Gasparini et al[75] | In T2D patients insulin metabolism dysfunction accelerates AβPP/Aβ trafficking from trans-Golgi network, a major site for a Aβ generation |
| Phiel et al[76] | Some studies claim for the presence of downstream regulators of insulin signaling pathway which are involved in cleavage of AβPP at gamma-secretase site, a determining site for Aβ amyloidogenicity |
| Steen et al[24] | Extensive dysfunction of IGF-I and IGF II signaling mechanisms reported in AD brain |
| Rivera et al[66] | Insulin and IGF gene expression altered with abnormal receptor binding in AD brain |
Protein structure and function is crucial for maintenance of life, moreover its mishandling leads to diverse pathological conditions. Neurodegenerative disorders lie in a class of disorders associated with different types of abnormal fibrous, extracellular poteinaceous deposits which are referred as amyloid[77]. β-sheet structured insoluble moieties play an important role in the pathology of many protein misfolding diseases[77]. Globular proteins due to their tertiary structure constrain, undergo destabilization of their native structure and adopt partial folded and unfolded form while natively folded proteins are devoid of any ordered form so they passes through the stabilization process of fibrillogenesis and acquire a partially folded conformation[78]. In a crowded cellular milieu when functional protein erroneously interacts with other components and transforms itself into ordered stable form, the phenomenon is known as amyloidogenesis.
Interestingly AD and DM both involve amyloidogenesis. Extracellular deposition of Aβ plaques is a feature of AD while amyloidogenic peptide deposition in pancreatic islets of Langerhans is a characteristic feature of T2D[79,80]. Amyloid deposits in islets consist of 37 amino acid peptide referred to as islet amyloid polypeptide (IAPP) amylin[81,82]. Aβ and IAPP have same folding patterns and configuration[83]. IAPP is reported to generate islet β-cells toxicity in the same way as Aβ do in neurons. Although we are far to understand the exact mechanism of amyloid formation, it can be speculated from the emerging data that amyloid formation is a basic cause of AD, DM and other disorders related to protein deposition[84-86].
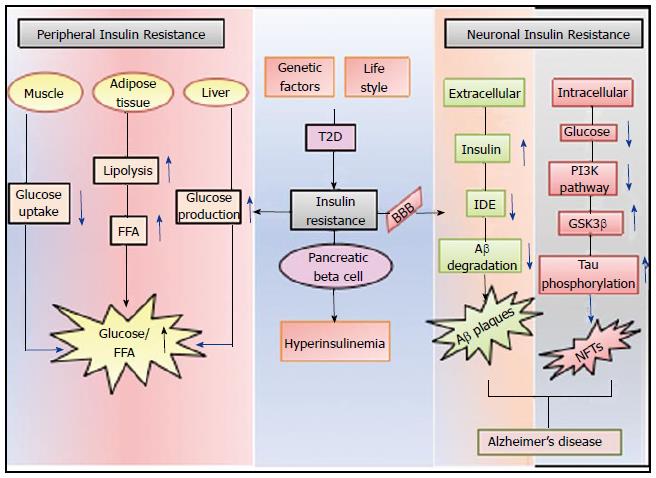
Glucose is the only required source of energy for neurons and any disruption in glucose metabolism leads to compromised neuronal functions[39]. Presence of insulin is crucial for brain in terms of its peculiar CNS functions[87] but any disturbance in its physiological level leads to CNS dysfunction. IRs are reported with low binding affinity with insulin in postmortem AD brain[87,88]. Moreover many other insulin signaling markers were altered in AD brain[24]. Elevated insulin plasma level in AD patients indicates a closed association of AD and IR[26,28]. Animal model studies revealed that factors contributing to T2D also regulate Aβ dynamics[89]. With this set of data it is clearly understood that IR or impaired IRs not only typify T2D but also orchestrate AD. Figure 2 depicts that how IR bridges peripheral and neuronal IR and leads to AD.
Insulin expression in brain remained a debated topic for investigators and raised a question on its significance at ectopic site. Brain synthesizes insulin locally as well as receives through the blood brain barrier (BBB) mediated transfer[90]. With curious attempts, scientists documented its role in feeding behavior and energy homeostasis which integrate whole body physiology[91]. The first article unpinning the relation between brain and insulin was reported in 1960, in which intracisternal injection of insulin in dogs reduced glucose levels, both in CSF and blood with its direct effects on the parasympathetic area of the brainstem[92]. Later, brain-centered glucoregulatory system (BCGS) that is involved in maintenance of blood glucose levels was found to act via insulin dependent as well as independent mechanisms[93]. The hypothesis of BCGS and its crosstalk with pancreatic islets gained experimental momentum by multiple supporting evidences that provided a clear understanding of BCGS[93]. BCGS is recognized as mechanistic node present in CNS which is channeled through peripheral hormone status[93]. Both of these regulatory nodes co-operate with each other and compensate the load of other’s failure but when both are compromised, DM is an unavoidable issue.
Insulin has drawn a wide trajectory in brain molecular milieu from cognitive function to orchestrate functions like development of neurite outgrowth, modulation of catecholamine release and uptake, regulation and trafficking of ligand-gated ion channels, expression and localization gamma-aminobutyric acid (GABA), N-methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, synaptic plasticity regulation via NMDA, Phosphoinositide 3-kinase-Akt (PI3K-Akt)[94] and maintenance of excitatory synapses[95].
Presence of IRs at synapses rich in plasticity (hippocampus and cortex) reveals its involvement in cognition[90]. This fact was further strengthened in 1999 when Zhao et al[21] reported that rat hippocampus IRs expression is up-regulated when they are subjected to spatial memory task in Morris water maze. IRs are enriched in synaptosomes[96], co-localizes with axon terminal markers synaptophysin, synapsin, etc.[97], and dominates in post-synaptic density (PSD) fractions to interact with scaffolding protein shank and PSD-95. Insulin is also involved in various neuromodulatory functions such as electrophysiological properties of neurons[98,99], neurotransmitter receptors[100,101], trafficking of ion channels[102], neurotrophic effects[103,104] and the neuroprotective role against a wide range of insults such as apoptosis[105], oxidative stress[106], β-amyloid toxicity[107] and ischemia[108] in animal models as well as human studies.
Hyperinsulinemia is reported to reduce cholinergic activity in mice brain and resulted in impaired retention of an inhibitory avoidance[109]. It also alters membrane potential to affect the ion transport[110,111]. In streptozotocin induced rat model of DM, long term memory potentiation was found to be impaired and insulin treatment rescued the effects[112-114]. With these set of potential findings, it is evident that insulin is crucial synapto-dendritic player altering dendritic arbor morphology as well physiology.
Investigators unraveled the IRs downstream molecular orchestra and speculated that IRs activation further activates PI3K/protein kinase B (PI3K/PKB) pathway[115]. GSK3β is a major player of this pathway and involved in long term potentiation/long term depression (LTP/LTD) which is a sole mechanism of memory formation and synaptic plasticity[116]. Other than insulin, PI3K can be activated by multiple growth factor ligands including nerve growth factor, brain-derived neurotrophic factor (BDNF), glial cell-derived neurotrophic factor (GDNF), insulin like growth factor-1 (IGF-1)[117].
After investigating for over two decades, it is safe to accept that PI3K/Akt signaling pathway is a potential window through which various ON/OFF switches of cognitive decline get operated. Protein kinase B (PKB), also known as Akt is a main downstream hub of various other pathways and exists with its widely expressed isoforms such as PKB-α, PKB-β and PKB-γ (predominates in CNS)[118]. Akt pathway has its regulating arms over neuronal survival, glucose uptake, angiogenesis, metabolism and proliferation[119]. Moreover Akt has a negative feedback regulation over these via phosphatase and tensin homolog, protein phosphatase 2A, c-jun N-terminal kinases (JNK) and forkhead box O (FOXO)[119].
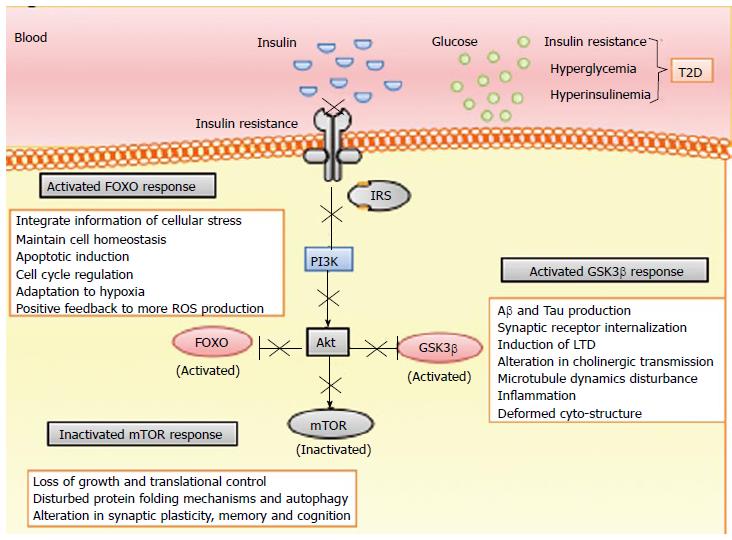
Loss of PI3K control is a central mechanism of neurodegeneration in DM patients[120]. Moreover, AD patients are reported with sustained PI3K/AKT signaling which is a primary response linking insulin, IGF resistance, tau pathogenesis and synaptic decline[121]. GSK3, mammalian target of rapamycin (mTOR) and FOXO are three main downstream targets playing this whole orchestra (represented in Figure 3).
Extensive reports supporting pivotal role of GSK3β proposed “GSK3β hypothesis of AD”[107], according to which GSK3β over-expression leads to impaired memory, amyloid β accumulation, tau hyperphosphorylation, neuronal defects and microglial mediated inflammation cascades. Genetic studies established that insulin signaling genes are also loci of AD[106]. Cholinergic system is one of the major regulating knob under GSK3β control with choline acetyltransferase and acetylcholinesterase as regulating keys[107,108]. GSK3β leads to reduction of acetylcholine synthesis, which is in accordance with the cholinergic deficit observed in AD brain[122]. GSK3β negatively affects axonal transport, microtubule dynamics and destabilizes microtubule by lowering its affinity with GSK3β phosphorylated tau[95-97] and contributes to AD pathology. Being a key mediator of apoptosis it may directly contribute to neuronal loss in AD[105,123]. GSK3β interestingly controls cell cycle in two way system by activating intrinsic pathway to trigger cell death and by inhibiting death receptors by extrinsic pathway[124]. In 2002, Sun et al[125] and in 2003, Phiel et al[76] reported that GSK3β increases Aβ production by regulating APP cleavage. On exposure of Aβ, neurons inhibit PI3K pathway and increase GSK3β activity[126]. GSK3α as well as GSK3β both are found to be an inducer of tau phosphorylation[127-132]. Drastic alteration in dendritic arbor and post synaptic density, a common morphological feature of AD brain has been observed in GSK3β deficient mice[132]. GSK3β is the only kinase involved in NMDAR-LTD[124]. It also maintains a threshold of LTP and LTD, i.e., maintenance of metaplasticity[116,133,134]. Modulation in regulated/constituted expression of GSK3β orchestrates neuronal plasticity[84,116,134-140]. GSK3β dramatically induces the internalization of AMPA and NMDA receptors[141,142] and decreases the level of PSD proteins, a molecular marker of memory acquisition[77]. GSK3β phosphorylates CREB protein to inhibit its function which is a universal modulator of memory. It aids in cyto-architecture of cell by promoting actin and tubulin assembly for synaptic reorganization[143]. GSK3β is also a pivotal kinase involved in adult hippocampal neurogenesis which negatively regulates it by reducing the number of proliferating neurons in the dentate gyrus region[144,145]. GSK3β is directly involved in the production of pro-inflammatory cytokines such as interleukin (IL) 6, IL-1β, TNF-α which indicates its positive regulation towards inflammatory mechanisms[146,147].
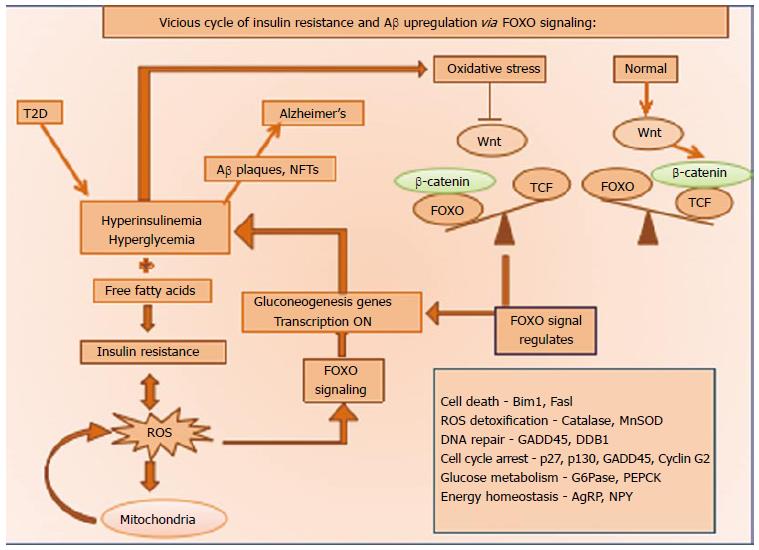
FOXO1 signaling is a mechanistic node and regulates the fine balance of oxidative stress pathways (depicted in Figure 4). Before moving into the mechanism part, it has been briefly discussed about the dramatic story of its evolution in molecular series under discovery[148]. Many lines of evidence suggest its role in AD as well as IR with major involvement in cell proliferation, differentiation, cell survival, apoptosis and development of proliferative late onset diseases[148]. Short term activation of this player leads to protective mechanism of scavenging reactive oxygen species (ROS) which is a part of normal cell physiology but its persistent activation awakes the apoptosis pathway[148]. Cellular milieu tends to maintain a balance oxidant and antioxidants concentration to cope up any environmental stress, but whenever this balance acquires any plane of inclination, it comes to the cell survival[148].
Wnt and β catenin up-regulate FOXO signaling via oxidative stress pathways[148]. Wnt signaling inhibits GSK3β expression and mediates β catenin transport into the nucleus and modulates transcription of T cell factor family gene, which has function opposite to FOXO1, this is known as the canonical pathway of Wnt signaling and involved in lipid and glucose metabolism[149]. ROS production inhibits canonical pathway of Wnt signaling and guides β catenin towards FOXO which acts as a cofactor of FOXO and enhance its transcription. Foxo signaling promotes gluconeogenesis and leads to hyperglycemia and hyperinsulinemia which further increases NFTs and Aβ accumulation to gear up ROS production and drives the vicious cycle of Oxidative stress[150].
When insulin is absent, FOXO1 is located in the nucleus and promotes transcription of respective enzymes for hepatic glucose production while in the presence of insulin; PKB is activated and leads to nuclear exclusion of FOXO 1 by phosphorylating it. State of IR in case of DM leads to impairment of PKB pathway and inhibition of FOXO activity resulting in hepatic glucose production triggering a vicious cycle of hyperglycemia and oxidative stress. FOXO, the downstream activator of PI3K/AKT controls energy homeostasis, locomotor behavior and leptin sensitivity[151,152].
mTOR pathway has been evolved as environment sensor and growth promoter in unicellular organisms but as multi-cellularity emerged it acquired its role in central growth and homeostasis mechanisms. Metabolism and cell growth are two basic requirements and their proper functioning depends upon each other. Since mTOR pathway is centered for growth processes, it is activated by nutrition as well as insulin[136]. In evolutionary history from yeast to rodents, mTOR has evolved as key modulator of aging. Many investigators attempted to understand its basic role and decades of extensive pursuit revealed extensive network of mTOR. mTOR is found to accelerate growth but it has compromised some of metabolic signals by conflicting pathways and introduced a paradox or better to say insulin paradox[137].
This paradox appeared from the evidences of compromised insulin signaling with good health and IR leading to compromised health while both of the cases are of poor insulin signaling[138]. Parsimonious explanations are, compromised insulin signaling is unable to activate mTOR (good for health) while IR may be due to hyperactive mTOR which is bad. So in previous case compromised insulin signaling inhibits mTOR insurgence while active mTOR is promoting IR in the later case[138]. Mechanistic node of this story, S6 kinase (S6K) is activated by mTOR to phosphorylate and degrade insulin receptor substrate-1 (IRS-1) which ultimately leads to insulin desensitization[139,140].
mTOR signaling has a dramatic interplay with Aβ and tau proteins which are two hallmarks of AD in their aggregated forms. It was reported in 2012 that Aβ is an activator of PI3K/Akt pathway which further switches on mTOR cascade[153]. In vitro studies suggest that Aβ application elevates the level of p70S6K, a downstream target of mTOR which contributes in development of NFTs[154,155]. Consistent in vitro reports validated the fact that mTOR activity and activated p70S6K are either cause or consequence of the molecular cascade and hence are found with elevated levels in hippocampus and cortex of animal model of AD[156,157]. mTOR suppression leads to induction of autophagy which is a cell cleaning process. In AD brain it is evident that neuronal autophagy is induced to end up with impaired steps and leads to massive accumulation of Aβ plaques[158].
mTOR has characteristic property of maintenance of protein homeostasis, translational control and cellular maintenance, which plays an important role in the maintenance of synaptic plasticity. Figure 5 provides detailed information of mTOR domain. To execute these entire tasks mTOR pathway is operated under fine control of several surface receptors such as NMDA, dopaminergic and metabotropic glutamate receptors (mGluRs) and BDNF[159-163]. mTORC1 is one of the downstream targets of PI3K/AKT pathway which is very important for synaptic plasticity, neuronal repair, protein folding mechanism and autophagy[164,165].
Inflammation is an exceedingly complex but equally fascinating and costly host defense system evolved with proximate set of mechanisms and exhibit phenotypic plasticity. It is crucial for life but once dysregulated, it can be detrimental. Emerging field of metabolic and aging syndromes spurred a renewed interest of scientists into inflammatory mechanisms. This is a compensatory mechanism for body to cope up with the hostile environment which involves many subtle factors and specialized cells to fight against any threat[166]. It has very critical progressive role with analogous mechanism in diabetic patients showing IR and defective neuronal signaling in AD patients[167]. Thus, DM and AD share inflammation as a common pathological feature.
Studies have reported elevated levels of proinflammatory cytokines such as TNF-α, IL-6, IL-1β, etc., in AD patients[168]. In diabetes patients, elevated TNF-α triggers various stress kinases to phosphorylate IRS-1 (at inhibitory serine residues) and disrupts insulin signaling[169-171] (explained in Figure 6), while blocking TNF-α rescues its effects in obese mouse model[172,173]. JNK and double-stranded RNA-dependent protein kinase are major stress kinases which are common regulatory nodes between inflammation and metabolism[174,175]. Since insulin signaling contributes to normal functioning of neurons, any inflammation mediated alteration in these, results into defective neuronal function[95,176,177]. These evidences suggest that there is a common mechanistic pathway adopted by peripheral IR in T2D as well as impaired brain insulin signaling in AD.
Normal body physiology tends to maintain a balance between production of ROS and body’s antioxidant defense system and any sort of imbalance altering this dynamic system leads to onset of metabolic disorder with cognitive dysfunction[178]. Hydrogen peroxide, hydroxyl radical, superoxide ion and singlet oxygen are such reactive species which are abundantly produced in cellular respiration cycles and have very short half life[179]. It is known that diabetic patients have more oxidative cellular environment as compared to healthy ones[180-182]. Hyperglycemic condition has proportionality with sorbitol production which reduces NADPH, a cofactor for GSH production and hence decreases antioxidant levels in the body[183-185]. One more prevalent mechanism of diabetes contributing towards ROS is insurgence of advanced glycation end products (AGEs) production[183,184,186], which binds to cell surface receptors, i.e., receptor for advanced glycation end roducts (RAGEs). RAGEs-AGEs interaction leads to ROS production via NADPH oxidase system which in turn activates Ras-MAPK pathway and ultimately nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) activation[184,187]. Hyperglycemia also leads to flux of glucose or FFA into blood which turns hexosamine pathway on[188] for further ROS production[189]. Elevated levels of FFA have an adverse effect on mitochondrial functioning and uncouple oxidative phosphorylation to contribute in ROS production[190,191]. ROS production worsens the status of insulin signaling and stress pathways which lead to further ROS production to turn a vicious cycle on.
High polyunsaturated fatty acid proportion with GSH content leave neurons vulnerable and make them prone to free radical attack[192]. A noticeable increase in lipid peroxidation was observed in brain of AD patients[193-195]. Oxidative stress and Aβ aggregation has both way relationships controlling each other’s turnover. Oxidative stress channels regulate Aβ dynamicity from non-aggregated form to aggregated form[196]. Aggregated Aβ acts like a source of free radical production and lipid peroxidation[197] to drive brain towards neurodegeneration.
Mitochondria, a result of 1.5 billion years of obligate endosymbiotic co-evolution is a sub-cellular niche to take care of cell survival as well as programmed cell death[198]. Several decades of research has established that fission-fusion dynamicity of mitochondria is critical in neurodegeneration[198]. As the brain is offered with limited capacity of glycolysis, neuronal cells are highly dependent on aerobic oxidative phosphorylation for energy production which is an electron transfer event from lower redox potential to higher redox potential[199-202]. Although, this electron chain transfer process is very efficient, still some ROS are produced which leads to oxidation of mitochondrial DNA, lipids and proteins further contributing to mitochondrial dysfunction which is a prominent feature of AD[181,203].
Substantial data from diabetic patients and animal model systems revealed that brain faces several structural and functional deficits. Functional impairment of mitochondria leads to neurodegeneration and loss of control over neuronal metabolism. A study reflected that there is a significant decrease in coenzyme Q levels in diabetic animals which represents a marked deficit in antioxidant defense system[204]. There are reports which are directly linking impairment in glucose utilization with mitochondrial dysfunction and metabolic disturbances[205-208]. In 2003, clear evidence of oxidative phosphorylation uncoupling was found in rat model of T2D[209]. Mitochondrial capacity of Ca2+ accumulation was also found to decrease in case of diabetes which is a favorable environment for mitochondrial permeability transition (MPT) opening and ultimately leads to cell death[210,211].
AD animal models as well as human studies suggested that AD pathology leads to mitochondrial dysfunction and ROS production. Some crucial molecules such as Aβ binding alcohol dehydrogenase are reported to aid to AD pathology by mediating Aβ induced cell death via mitochondrial channel[209,212]. In some reports it is mentioned that one of the insulin degrading enzymes isoform, a well established regulator of Aβ dynamicity targets mitochondria and interfere with its normal functioning[213]. Aβ is also found to be a good inhibitor of respiratory chain complex and thus leads to marked decrease in cellular ATP levels[214,215]. Importantly, Aβ 40 and Aβ 25-35 contribute in uncoupling of oxidative phosphorylation and impair respiratory chain as well as MPT opening[204,210,211]. Moreover Aβ induces H2O2 production which is rescued by CoQ10, a key enzyme of electron transport chain[216]. Various tri-carboxylic acid (TCA) cycle enzymes such as pyruvate dehydrogenase, α-ketoglutarate dehydrogenase and ATP citrate lyase were also found to be dysregulated in case of AD[217].
Mitochondrial morphology was found to be altered with some functional loss in neurodegenerative disorders such as AD[218-221]. In brief it can be mentioned that a small metabolic compromise is sufficient to trigger a cascade and disrupt normal mitochondrial function which plays a vital role in neuronal survival, growth and plasticity.
Sedentary life style, dietary changes and genetic predisposition are conspired forces responsible for worldwide epidemic of metabolic and aging syndrome. Discovered molecular trajectories from T2D to T3D gained experimental momentum for new therapeutic interventions. Elucidating role of anti-diabetic drug for the treatment of AD translated the disease information and added new armaments to the arsenal of putative therapies. It is unquestionable issue that both of these disorders share common pathologies including glucose metabolism defects, mitochondrial dysfunction, oxidative stress and abnormal deposition of amyloidogenic proteins[55]. The reason why insulin got this recognition under frontier’s of Alzheimer research is that its high level in CNS revealed its own crucial role in learning, memory, cognition and synaptic plasticity[222]. Although, brain has potential pyramidal neurons involved in synthesis and secretion of insulin, majority of brain insulin is replenished by peripheral source from pancreatic β cells transported through blood across BBB[223].
There are some well known potential oral drugs [such as biguanides, sulfonylureas (SUs), thiazolidinediones (TZDs), and dipeptidyl peptidase-IV (DPP-IV) inhibitors], injections (e.g., insulin and GLP-1 analogs), and some other molecules like glucokinase activators, amylin analogs, D2-dopamine agonists, bile acid chelators, and sodium/glucose-linked transporter-2 inhibitors etc., established for T2D. Most of the anti-diabetic drugs act through the mechanism of maintenance of plasma glucose level, regulation of inflammatory cascades and establishing the balance between ROS and antioxidants. We will briefly provide an overview of experimental and clinical trials of some anti-diabetic drugs which are being tested in patients with AD and with low to moderate mild cognitive impairment.
Metformin, a well known biguanide anti-diabetic drug is used to reduce IR. It sensitizes liver and skeletal muscle cell via AMP kinase cascade[224,225]. Brain is most vulnerable vital organ for oxidative stress, because of high oxidative metabolism rate and limited antioxidant level. Under oxidative stress mitochondrial permeability pores open up to release cytochrome c and trigger apoptotic cascade. Metformin is reported to inhibit opening of these permeability pores in ectoposide-induced cell death model to inhibit apoptotic cascade[226]. Metformin is also involved in neurogenesis by activation of protein kinase C-CREB binding pathway (PKC-CBP) pathway in neuronal cell culture study, in human and rodent model system[227]. In neuronal cell lines (neuro2A), metformin promotes insulin action and attenuates molecular and pathological features observed in AD. Metformin treatment was found to reduce the risk of dementia in human aged subjects[228]. AD patients taking calcium in diet supplemented with metformin were found to have better cognitive performance[229]. Thus these evidences support the fact that metformin is not only a known anti-diabetic agent but also an effective neuroprotective molecule.
SUs is a class of anti-diabetic drugs which are used as mono or combined therapy to increase insulin secretion by enhancing pro-insulin level via voltage gated calcium channel but the actual mechanistic target is still under investigation[230]. SUs limits liver glucose production and decreases insulin clearance by liver. Glipizide and Glyburide (glibenclamide) are the main SUs compounds which are investigated for memory and cognition in diabetic patients.
In case of diabetes and AD, PI3K/mTOR is found to be aberrantly activated. Glyburide and glipizide are reported to have properties of mTOR antagonist[231] but their efficacy to recover AD patients is yet to be determined. Inflammosomes are involved in the secretion of proinflammatory cytokines that results in inflammation and associates it to AD. Along with inhibiting mTOR pathway, gliburide is found to inhibit inflammosome and thus brain inflammation[232]. Exalto et al[230] reported that SUs treated T2D patients shows improved AD type dementia symptoms but the precise mechanism is still unknown.
DM patients treated with glipizide are reported to have better learning efficiency[233]. Some recent studies show that there is no alteration in the development of AD in population using SUs in long term[234]. Metformin and SUs in combination are reported to reduce the risk of dementia upto 35% in a prospective cohort study[228].
Intranasal administration of insulin is reported to attenuate reduced insulin signaling in AD[235]. Importantly, intranasal insulin does not adversely affect blood insulin or glucose levels.
It is evident that AD patients have low insulin level and brain insulin resistant state which leads to impaired energy metabolism of neurons and make them vulnerable for survival. Insulin has been reported with its anti-amyloidogenic effect in human neuronal cell lines[236]. Some reports have shown that Aβ induced neuronal IR is attenuated by insulin treatment[237].
In a study it is found that 20 IU insulin twice a day over a period of 21 d in early AD or MCI subject’s helps to retain verbal information more effectively[30]. In 2006 Reger et al[30] showed that 10 IU intranasal insulin improves cognition in APOE4 AD/MCI subjects.
TZDs (also represented as glitazones) are a potential class of drug used for T2D which includes rosiglitazone (avandia), pioglitazone (actos) and troglitazone (rezulin). Mechanism of this group lies in activation of peroxisome proliferator-activated receptors by mimicking as a potential agonist of it and involved in transcription of lipid and glucose metabolism genes[238,239]. Since TZDs are anti-amyloidogenic and anti-inflammatory compounds with insulin sensitizing role, these delay neurodegeneration[240]. It also improves glycemic control in diabetic patients by inhibiting hepatic gluconeogenesis. Moreover, TZDs (mainly Troglitazone) are supposed to have their involvement in rescuing memory loss and decreasing plasma Aβ 40 and Aβ 42 levels[241,242] but again it needs to be investigated further.
Rosiglitazone is reported to attenuate neuronal IR induced by Aβ oligomers[237]. Pioglitazone is found to improve cognitive performance in a rodent dementia model induced by intracerebroventricular (ICV) injection of streptozotocin[243].
In a randomized trial rosiglitazone (8 mg) is reported to improve cognitive function in mild to moderate AD patients (non APOE4 carrier[244]). In contrast, a recent phase III trial of the same drug has failed to show similar effects in AD subjects[245]. Moreover, long term use of TZDs, in general has no effect on risk of AD development[234].
Glucagon like peptide 1 (GLP1) analogs are “incretin mimetics”, used to treat T2D. Exenatide, a 39 amino acid long peptide is analogous to human GLP1 which stimulates insulin secretion in a glucose dependent fashion. In brain these analogues bind tor GLP receptors and mediate various functions like suppression of glucagon production, slow down gastric emptying, increase satiety and reduce food intake with lower risk of hypoglycemia.
In an animal study, GLP1 is reported to protect neurons from oxidative stress with reduced apoptosis, plaque formation and inflammatory response. Moreover, it strengthens synaptic plasticity in AD mouse brain l[246]. It is shown to improve spatial memory in transgenic AD mice model[247]. Liraglutide and lixisenatide are GLP1 receptor agonists which are reported to activate cAMP in the brain and induce neurogenesis[248]. In addition, liraglutide attenuates memory impairments in a mouse model of AD[249]. Subcutaneous administration of liraglutide is reported to restore both peripheral and brain insulin sensitivity and ameliorates tau hyperphosphorylation in rat model of T2D[250]. Clinical research on the effect of liraglutide on AD patients is still going to evaluate the changes in cognition using a neuropsychological test battery[251].
DPP-IV, pharmacological inhibitors are oral hypoglycemic. These compounds reduce blood glucose levels by increasing incretin (GLP-1 and GIP levels) and attenuating glucagon effects. Sitagliptin, Vildagliptin, Saxagliptin, Linagliptin, Teneligliptin, Gemigliptin and Dutogliptin are major members of gliptins, out of which Dutogliptin is under Phase III clinical trial[252]. Effect of sitagliptin administration is studied double transgenic mice model of AD and reported to significantly delay AD pathology including amyloid deposition and taupathies[253].
Combination of insulin and other oral anti-diabetic drugs are reported to lower neuritic plaque density by 20% in AD brains[253]. Metformin in combination with rosiglitazone or glyburide is reported to improve working memory very significantly[253]. In a prospective cohort study, metformin and SUs are reported to reduce risk of dementia by 35%[228]. Although, a number of anti-diabetic drugs are reported to improve cognitive effect, it is still not well understood whether these effects are due to glucose lowering effects or adopt different pathways of neuroprotection. A broad range of anti diabetic therapies are undergoing clinical trials including those involving stimulation of the pancreatic beta-cell with the gut-derived insulinotropic hormones (incretins), GIP and GLP-1[254]. Some drugs have good glycemic control but have no history to improve cognitive functions[255]. In a study diabetes patients were maintained at normoglycemia over 3 mo but no significant improvement in cognitive performance was observed[256]. Other than glycemic control, anti-diabetic drugs improve cognitive function. Although various clinical trials are underway to evaluate the role of anti-diabetic drugs in treatment of neurodegenerative disorders such as dementia and AD but the search is still not over.
This review provides a synopsis in which a metabolic disturbance becomes indispensible for life. This is a talk of a metabolic problem which emerges as a molecular signal defect and takes a form of syndrome with multiple complications. Spotlighted player, insulin draws a trajectory from diabetes to AD with multiple divergence and convergence.
AD and DM are two devastating syndromes with complex molecular interplay. Evidences of their shared molecular and biochemical footprints shed light on the therapeutic interventions as major future perspectives.
The authors would like to thank Dr. Aditya Sunkaria for his advice and support.
P- Reviewer: Charoenphandhu N, Das UN, Takebayashi K S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Mehers KL, Gillespie KM. The genetic basis for type 1 diabetes. Br Med Bull. 2008;88:115-129. [PubMed] |
| 2. | Wright E, Scism-Bacon JL, Glass LC. Oxidative stress in type 2 diabetes: the role of fasting and postprandial glycaemia. Int J Clin Pract. 2006;60:308-314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 339] [Cited by in RCA: 334] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 3. | Nordwall M, Abrahamsson M, Dhir M, Fredrikson M, Ludvigsson J, Arnqvist HJ. Impact of HbA1c, followed from onset of type 1 diabetes, on the development of severe retinopathy and nephropathy: the VISS Study (Vascular Diabetic Complications in Southeast Sweden). Diabetes Care. 2015;38:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 4. | Sima AA. Encephalopathies: the emerging diabetic complications. Acta Diabetol. 2010;47:279-293. [PubMed] |
| 5. | den Heijer T, Vermeer SE, Clarke R, Oudkerk M, Koudstaal PJ, Hofman A, Breteler MM. Homocysteine and brain atrophy on MRI of non-demented elderly. Brain. 2003;126:170-175. [PubMed] |
| 6. | Schmidt R, Launer LJ, Nilsson LG, Pajak A, Sans S, Berger K, Breteler MM, de Ridder M, Dufouil C, Fuhrer R. Magnetic resonance imaging of the brain in diabetes: the Cardiovascular Determinants of Dementia (CASCADE) Study. Diabetes. 2004;53:687-692. [PubMed] |
| 7. | García RG, Rincón MY, Arenas WD, Silva SY, Reyes LM, Ruiz SL, Ramirez F, Camacho PA, Luengas C, Saaibi JF. Hyperinsulinemia is a predictor of new cardiovascular events in Colombian patients with a first myocardial infarction. Int J Cardiol. 2011;148:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Kasai T, Miyauchi K, Kajimoto K, Kubota N, Dohi T, Kurata T, Amano A, Daida H. The adverse prognostic significance of the metabolic syndrome with and without hypertension in patients who underwent complete coronary revascularization. J Hypertens. 2009;27:1017-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Agnoli C, Berrino F, Abagnato CA, Muti P, Panico S, Crosignani P, Krogh V. Metabolic syndrome and postmenopausal breast cancer in the ORDET cohort: a nested case-control study. Nutr Metab Cardiovasc Dis. 2010;20:41-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 143] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | Faulds MH, Dahlman-Wright K. Metabolic diseases and cancer risk. Curr Opin Oncol. 2012;24:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Colonna SV, Douglas Case L, Lawrence JA. A retrospective review of the metabolic syndrome in women diagnosed with breast cancer and correlation with estrogen receptor. Breast Cancer Res Treat. 2012;131:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Kroner Z. The relationship between Alzheimer’s disease and diabetes: Type 3 diabetes? Altern Med Rev. 2009;14:373-379. [PubMed] |
| 13. | Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53:1937-1942. [PubMed] |
| 14. | Baskin DG, Wilcox BJ, Figlewicz DP, Dorsa DM. Insulin and insulin-like growth factors in the CNS. Trends Neurosci. 1988;11:107-111. [PubMed] |
| 15. | Adamo M, Raizada MK, LeRoith D. Insulin and insulin-like growth factor receptors in the nervous system. Mol Neurobiol. 1989;3:71-100. [PubMed] |
| 16. | Biessels GJ, Bravenboer B, Gispen WH. Glucose, insulin and the brain: modulation of cognition and synaptic plasticity in health and disease: a preface. Eur J Pharmacol. 2004;490:1-4. [PubMed] |
| 17. | Gerozissis K. Brain insulin: regulation, mechanisms of action and functions. Cell Mol Neurobiol. 2003;23:1-25. [PubMed] |
| 18. | Plitzko D, Rumpel S, Gottmann K. Insulin promotes functional induction of silent synapses in differentiating rat neocortical neurons. Eur J Neurosci. 2001;14:1412-1415. [PubMed] |
| 19. | Skeberdis VA, Lan J, Zheng X, Zukin RS, Bennett MV. Insulin promotes rapid delivery of N-methyl-D- aspartate receptors to the cell surface by exocytosis. Proc Natl Acad Sci USA. 2001;98:3561-3566. [PubMed] |
| 20. | Hooper PL. Insulin Signaling, GSK-3, Heat Shock Proteins and the Natural History of Type 2 Diabetes Mellitus: A Hypothesis. Metab Syndr Relat Disord. 2007;5:220-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Zhao W, Chen H, Xu H, Moore E, Meiri N, Quon MJ, Alkon DL. Brain insulin receptors and spatial memory. Correlated changes in gene expression, tyrosine phosphorylation, and signaling molecules in the hippocampus of water maze trained rats. J Biol Chem. 1999;274:34893-34902. [PubMed] |
| 22. | Hoyer S. Is sporadic Alzheimer disease the brain type of non-insulin dependent diabetes mellitus? A challenging hypothesis. J Neural Transm. 1998;105:415-422. [PubMed] |
| 23. | Messier C, Gagnon M. Glucose regulation and cognitive functions: relation to Alzheimer’s disease and diabetes. Behav Brain Res. 1996;75:1-11. [PubMed] |
| 24. | Steen E, Terry BM, Rivera EJ, Cannon JL, Neely TR, Tavares R, Xu XJ, Wands JR, de la Monte SM. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease--is this type 3 diabetes? J Alzheimers Dis. 2005;7:63-80. [PubMed] |
| 25. | Craft S, Dagogo-Jack SE, Wiethop BV, Murphy C, Nevins RT, Fleischman S, Rice V, Newcomer JW, Cryer PE. Effects of hyperglycemia on memory and hormone levels in dementia of the Alzheimer type: a longitudinal study. Behav Neurosci. 1993;107:926-940. [PubMed] |
| 26. | Craft S, Peskind E, Schwartz MW, Schellenberg GD, Raskind M, Porte D. Cerebrospinal fluid and plasma insulin levels in Alzheimer’s disease: relationship to severity of dementia and apolipoprotein E genotype. Neurology. 1998;50:164-168. [PubMed] |
| 27. | Meneilly GS, Hill A. Alterations in glucose metabolism in patients with Alzheimer’s disease. J A m Geriatr Soc. 1993;41:710-714. [PubMed] |
| 28. | Craft S, Asthana S, Schellenberg G, Cherrier M, Baker LD, Newcomer J, Plymate S, Latendresse S, Petrova A, Raskind M. Insulin metabolism in Alzheimer’s disease differs according to apolipoprotein E genotype and gender. Neuroendocrinology. 1999;70:146-152. [PubMed] |
| 29. | Craft S, Newcomer J, Kanne S, Dagogo-Jack S, Cryer P, Sheline Y, Luby J, Dagogo-Jack A, Alderson A. Memory improvement following induced hyperinsulinemia in Alzheimer’s disease. Neurobiol Aging. 1996;17:123-130. [PubMed] |
| 30. | Reger MA, Watson GS, Green PS, Wilkinson CW, Baker LD, Cholerton B, Fishel MA, Plymate SR, Breitner JC, DeGroodt W. Intranasal insulin improves cognition and modulates beta-amyloid in early AD. Neurology. 2008;70:440-448. [PubMed] |
| 31. | Klein R. Hyperglycemia and microvascular and macrovascular disease in diabetes. Diabetes Care. 1995;18:258-268. [PubMed] |
| 32. | Strachan MW, Deary IJ, Ewing FM, Frier BM. Is type II diabetes associated with an increased risk of cognitive dysfunction? A critical review of published studies. Diabetes Care. 1997;20:438-445. [PubMed] |
| 33. | Stewart R, Liolitsa D. Type 2 diabetes mellitus, cognitive impairment and dementia. Diabet Med. 1999;16:93-112. [PubMed] |
| 34. | Manschot SM, Brands AM, van der Grond J, Kessels RP, Algra A, Kappelle LJ, Biessels GJ. Brain magnetic resonance imaging correlates of impaired cognition in patients with type 2 diabetes. Diabetes. 2006;55:1106-1113. [PubMed] |
| 35. | Cukierman T, Gerstein HC, Williamson JD. Cognitive decline and dementia in diabetes--systematic overview of prospective observational studies. Diabetologia. 2005;48:2460-2469. [PubMed] |
| 36. | Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med. 2009;169:798-807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 267] [Cited by in RCA: 242] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 37. | Jakicic JM, Jaramillo SA, Balasubramanyam A, Bancroft B, Curtis JM, Mathews A, Pereira M, Regensteiner JG, Ribisl PM. Effect of a lifestyle intervention on change in cardiorespiratory fitness in adults with type 2 diabetes: results from the Look AHEAD Study. Int J Obes (Lond). 2009;33:305-316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 38. | Vijan S. In the clinic. Type 2 diabetes. Ann Intern Med. 2010;152:ITC31-IT15; quiz ITC316. [PubMed] |
| 39. | Hoyer S. Brain glucose and energy metabolism during normal aging. Aging (Milano). 1990;2:245-258. [PubMed] |
| 40. | Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J. The importance of neuritic plaques and tangles to the development and evolution of AD. Neurology. 2004;62:1984-1989. [PubMed] |
| 41. | Qiu C, Kivipelto M, von Strauss E. Epidemiology of Alzheimer’s disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009;11:111-128. [PubMed] |
| 42. | Tagarelli A, Piro A, Tagarelli G, Lagonia P, Quattrone A. Alois Alzheimer: a hundred years after the discovery of the eponymous disorder. Int J Biomed Sci. 2006;2:196-204. [PubMed] |
| 43. | Waring SC, Rosenberg RN. Genome-wide association studies in Alzheimer disease. Arch Neurol. 2008;65:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 44. | Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS, Roses AD. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci USA. 1993;90:1977-1981. [PubMed] |
| 45. | Mahley RW, Weisgraber KH, Huang Y. Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer’s disease. Proc Natl Acad Sci USA. 2006;103:5644-5651. [PubMed] |
| 46. | Francis PT, Palmer AM, Snape M, Wilcock GK. The cholinergic hypothesis of Alzheimer’s disease: a review of progress. J Neurol Neurosurg Psychiatry. 1999;66:137-147. [PubMed] |
| 47. | Adolfsson R, Bucht G, Lithner F, Winblad B. Hypoglycemia in Alzheimer’s disease. Acta Med Scand. 1980;208:387-388. [PubMed] |
| 48. | Razay G, Wilcock GK. Hyperinsulinaemia and Alzheimer’s disease. Age Ageing. 1994;23:396-399. [PubMed] |
| 49. | Messier C. Diabetes, Alzheimer’s disease and apolipoprotein genotype. Exp Gerontol. 2003;38:941-946. [PubMed] |
| 50. | Li L, Hölscher C. Common pathological processes in Alzheimer disease and type 2 diabetes: a review. Brain Res Rev. 2007;56:384-402. [PubMed] |
| 51. | de la Monte SM, Wands JR. Alzheimer’s disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. 2008;2:1101-1113. [PubMed] |
| 52. | Götz J, Ittner LM, Lim YA. Common features between diabetes mellitus and Alzheimer’s disease. Cell Mol Life Sci. 2009;66:1321-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 53. | Saini V. Molecular mechanisms of insulin resistance in type 2 diabetes mellitus. World J Diabetes. 2010;1:68-75. [PubMed] |
| 54. | Park SA. A common pathogenic mechanism linking type-2 diabetes and Alzheimer’s disease: evidence from animal models. J Clin Neurol. 2011;7:10-18. [PubMed] |
| 55. | Correia SC, Santos RX, Carvalho C, Cardoso S, Candeias E, Santos MS, Oliveira CR, Moreira PI. Insulin signaling, glucose metabolism and mitochondria: major players in Alzheimer’s disease and diabetes interrelation. Brain Res. 2012;1441:64-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 56. | Biju MP, Paulose CS. Brain glutamate dehydrogenase changes in streptozotocin diabetic rats as a function of age. Biochem Mol Biol Int. 1998;44:1-7. [PubMed] |
| 57. | Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, Fuino RL, Kawaguchi KR, Samoyedny AJ, Wilson RS. Demonstrated brain insulin resistance in Alzheimer’s disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest. 2012;122:1316-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1129] [Cited by in RCA: 1401] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 58. | Ruigómez A, García Rodríguez LA. Presence of diabetes related complication at the time of NIDDM diagnosis: an important prognostic factor. Eur J Epidemiol. 1998;14:439-445. [PubMed] |
| 59. | Ke YD, Delerue F, Gladbach A, Götz J, Ittner LM. Experimental diabetes mellitus exacerbates tau pathology in a transgenic mouse model of Alzheimer’s disease. PLoS One. 2009;4:e7917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 60. | Pasquier F, Boulogne A, Leys D, Fontaine P. Diabetes mellitus and dementia. Diabetes Metab. 2006;32:403-414. [PubMed] |
| 61. | Verdelho A, Madureira S, Ferro JM, Basile AM, Chabriat H, Erkinjuntti T, Fazekas F, Hennerici M, O’Brien J, Pantoni L. Differential impact of cerebral white matter changes, diabetes, hypertension and stroke on cognitive performance among non-disabled elderly. The LADIS study. J Neurol Neurosurg Psychiatry. 2007;78:1325-1330. [PubMed] |
| 62. | Winocur G, Greenwood CE. Studies of the effects of high fat diets on cognitive function in a rat model. Neurobiol Aging. 2005;26 Suppl 1:46-49. [PubMed] |
| 63. | Winocur G, Greenwood CE, Piroli GG, Grillo CA, Reznikov LR, Reagan LP, McEwen BS. Memory impairment in obese Zucker rats: an investigation of cognitive function in an animal model of insulin resistance and obesity. Behav Neurosci. 2005;119:1389-1395. [PubMed] |
| 64. | Lester-Coll N, Rivera EJ, Soscia SJ, Doiron K, Wands JR, de la Monte SM. Intracerebral streptozotocin model of type 3 diabetes: relevance to sporadic Alzheimer’s disease. J Alzheimers Dis. 2006;9:13-33. [PubMed] |
| 65. | Weinstock M, Shoham S. Rat models of dementia based on reductions in regional glucose metabolism, cerebral blood flow and cytochrome oxidase activity. J Neural Transm. 2004;111:347-366. [PubMed] |
| 66. | Rivera EJ, Goldin A, Fulmer N, Tavares R, Wands JR, de la Monte SM. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer’s disease: link to brain reductions in acetylcholine. J Alzheimers Dis. 2005;8:247-268. [PubMed] |
| 67. | Craft S. Insulin resistance syndrome and Alzheimer disease: pathophysiologic mechanisms and therapeutic implications. Alzheimer Dis Assoc Disord. 2006;20:298-301. [PubMed] |
| 68. | Craft S. Insulin resistance and Alzheimer’s disease pathogenesis: potential mechanisms and implications for treatment. Curr Alzheimer Res. 2007;4:147-152. [PubMed] |
| 69. | de la Monte SM, Tong M, Lester-Coll N, Plater M, Wands JR. Therapeutic rescue of neurodegeneration in experimental type 3 diabetes: relevance to Alzheimer’s disease. J Alzheimers Dis. 2006;10:89-109. [PubMed] |
| 70. | Haan MN. Therapy Insight: type 2 diabetes mellitus and the risk of late-onset Alzheimer’s disease. Nat Clin Pract Neurol. 2006;2:159-166. [PubMed] |
| 71. | Watson GS, Bernhardt T, Reger MA, Cholerton BA, Baker LD, Peskind ER, Asthana S, Plymate SR, Frölich L, Craft S. Insulin effects on CSF norepinephrine and cognition in Alzheimer’s disease. Neurobiol Aging. 2006;27:38-41. [PubMed] |
| 72. | Marchesini G, Marzocchi R. Metabolic syndrome and NASH. Clin Liver Dis. 2007;11:105-117, ix. [PubMed] |
| 73. | Yeh MM, Brunt EM. Pathology of nonalcoholic fatty liver disease. Am J Clin Pathol. 2007;128:837-847. [PubMed] |
| 74. | Mandelkow EM, Drewes G, Biernat J, Gustke N, Van Lint J, Vandenheede JR, Mandelkow E. Glycogen synthase kinase-3 and the Alzheimer-like state of microtubule-associated protein tau. FEBS Lett. 1992;314:315-321. [PubMed] |
| 75. | Gasparini L, Gouras GK, Wang R, Gross RS, Beal MF, Greengard P, Xu H. Stimulation of beta-amyloid precursor protein trafficking by insulin reduces intraneuronal beta-amyloid and requires mitogen-activated protein kinase signaling. J Neurosci. 2001;21:2561-2570. [PubMed] |
| 76. | Phiel CJ, Wilson CA, Lee VM, Klein PS. GSK-3alpha regulates production of Alzheimer’s disease amyloid-beta peptides. Nature. 2003;423:435-439. [PubMed] |
| 77. | Zhao WQ, Townsend M. Insulin resistance and amyloidogenesis as common molecular foundation for type 2 diabetes and Alzheimer’s disease. Biochim Biophys Acta. 2009;1792:482-496. [PubMed] |
| 78. | Uversky VN. Amyloidogenesis of natively unfolded proteins. Curr Alzheimer Res. 2008;5:260-287. [PubMed] |
| 79. | Haass C, Koo EH, Mellon A, Hung AY, Selkoe DJ. Targeting of cell-surface beta-amyloid precursor protein to lysosomes: alternative processing into amyloid-bearing fragments. Nature. 1992;357:500-503. [PubMed] |
| 80. | Shoji M, Golde TE, Ghiso J, Cheung TT, Estus S, Shaffer LM, Cai XD, McKay DM, Tintner R, Frangione B. Production of the Alzheimer amyloid beta protein by normal proteolytic processing. Science. 1992;258:126-129. [PubMed] |
| 81. | Westermark P, Wernstedt C, Wilander E, Hayden DW, O’Brien TD, Johnson KH. Amyloid fibrils in human insulinoma and islets of Langerhans of the diabetic cat are derived from a neuropeptide-like protein also present in normal islet cells. Proc Natl Acad Sci USA. 1987;84:3881-3885. [PubMed] |
| 82. | Cooper GJ, Willis AC, Clark A, Turner RC, Sim RB, Reid KB. Purification and characterization of a peptide from amyloid-rich pancreases of type 2 diabetic patients. Proc Natl Acad Sci USA. 1987;84:8628-8632. [PubMed] |
| 83. | Kayed R, Head E, Thompson JL, McIntire TM, Milton SC, Cotman CW, Glabe CG. Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis. Science. 2003;300:486-489. [PubMed] |
| 84. | Kelly A, Lynch MA. Long-term potentiation in dentate gyrus of the rat is inhibited by the phosphoinositide 3-kinase inhibitor, wortmannin. Neuropharmacology. 2000;39:643-651. [PubMed] |
| 85. | Selkoe DJ. Soluble oligomers of the amyloid beta-protein impair synaptic plasticity and behavior. Behav Brain Res. 2008;192:106-113. [PubMed] |
| 86. | Dobson CM. The structural basis of protein folding and its links with human disease. Philos Trans R Soc Lond B Biol Sci. 2001;356:133-145. [PubMed] |
| 87. | Heidenreich KA, Zahniser NR, Berhanu P, Brandenburg D, Olefsky JM. Structural differences between insulin receptors in the brain and peripheral target tissues. J Biol Chem. 1983;258:8527-8530. [PubMed] |
| 88. | Frölich L, Blum-Degen D, Riederer P, Hoyer S. A disturbance in the neuronal insulin receptor signal transduction in sporadic Alzheimer’s disease. Ann N Y Acad Sci. 1999;893:290-293. [PubMed] |
| 89. | Ho L, Qin W, Pompl PN, Xiang Z, Wang J, Zhao Z, Peng Y, Cambareri G, Rocher A, Mobbs CV. Diet-induced insulin resistance promotes amyloidosis in a transgenic mouse model of Alzheimer’s disease. FASEB J. 2004;18:902-904. [PubMed] |
| 90. | Valatx JL, Douhet P, Bucchini D. Human insulin gene insertion in mice. Effects on the sleep-wake cycle? J Sleep Res. 1999;8 Suppl 1:65-68. [PubMed] |
| 91. | Varela L, Horvath TL. Leptin and insulin pathways in POMC and AgRP neurons that modulate energy balance and glucose homeostasis. EMBO Rep. 2012;13:1079-1086. [PubMed] |
| 92. | Chowers I, Lavy S, Halpern L. Effect of insulin administered intracisternally on the glucose level of the blood and the cerebrospinal fluid in vagotomized dogs. Exp Neurol. 1966;14:383-389. [PubMed] |
| 93. | Schwartz MW, Seeley RJ, Tschöp MH, Woods SC, Morton GJ, Myers MG, D’Alessio D. Cooperation between brain and islet in glucose homeostasis and diabetes. Nature. 2013;503:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 222] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 94. | van der Heide LP, Kamal A, Artola A, Gispen WH, Ramakers GM. Insulin modulates hippocampal activity-dependent synaptic plasticity in a N-methyl-d-aspartate receptor and phosphatidyl-inositol-3-kinase-dependent manner. J Neurochem. 2005;94:1158-1166. [PubMed] |
| 95. | Chiu SL, Chen CM, Cline HT. Insulin receptor signaling regulates synapse number, dendritic plasticity, and circuit function in vivo. Neuron. 2008;58:708-719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 346] [Cited by in RCA: 326] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 96. | Werther GA, Hogg A, Oldfield BJ, McKinley MJ, Figdor R, Allen AM, Mendelsohn FA. Localization and characterization of insulin receptors in rat brain and pituitary gland using in vitro autoradiography and computerized densitometry. Endocrinology. 1987;121:1562-1570. [PubMed] |
| 97. | Mielke JG, Taghibiglou C, Wang YT. Endogenous insulin signaling protects cultured neurons from oxygen-glucose deprivation-induced cell death. Neuroscience. 2006;143:165-173. [PubMed] |
| 98. | Kovacs P, Hajnal A. In vivo electrophysiological effects of insulin in the rat brain. Neuropeptides. 2009;43:283-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 99. | Palovcik RA, Phillips MI, Kappy MS, Raizada MK. Insulin inhibits pyramidal neurons in hippocampal slices. Brain Res. 1984;309:187-191. [PubMed] |
| 100. | Wan Q, Xiong ZG, Man HY, Ackerley CA, Braunton J, Lu WY, Becker LE, MacDonald JF, Wang YT. Recruitment of functional GABA(A) receptors to postsynaptic domains by insulin. Nature. 1997;388:686-690. [PubMed] |
| 101. | Lozovsky DB, Kopin IJ, Saller CF. Modulation of dopamine receptor supersensitivity by chronic insulin: implication in schizophrenia. Brain Res. 1985;343:190-193. [PubMed] |
| 102. | Fadool DA, Tucker K, Phillips JJ, Simmen JA. Brain insulin receptor causes activity-dependent current suppression in the olfactory bulb through multiple phosphorylation of Kv1.3. J Neurophysiol. 2000;83:2332-2348. [PubMed] |
| 103. | Farrar C, Houser CR, Clarke S. Activation of the PI3K/Akt signal transduction pathway and increased levels of insulin receptor in protein repair-deficient mice. Aging Cell. 2005;4:1-12. [PubMed] |
| 104. | Schubert M, Brazil DP, Burks DJ, Kushner JA, Ye J, Flint CL, Farhang-Fallah J, Dikkes P, Warot XM, Rio C. Insulin receptor substrate-2 deficiency impairs brain growth and promotes tau phosphorylation. J Neurosci. 2003;23:7084-7092. [PubMed] |
| 105. | Ryu BR, Ko HW, Jou I, Noh JS, Gwag BJ. Phosphatidylinositol 3-kinase-mediated regulation of neuronal apoptosis and necrosis by insulin and IGF-I. J Neurobiol. 1999;39:536-546. [PubMed] |
| 106. | Duarte AI, Santos MS, Oliveira CR, Rego AC. Insulin neuroprotection against oxidative stress in cortical neurons--involvement of uric acid and glutathione antioxidant defenses. Free Radic Biol Med. 2005;39:876-889. [PubMed] |
| 107. | Rensink AA, Otte-Höller I, de Boer R, Bosch RR, ten Donkelaar HJ, de Waal RM, Verbeek MM, Kremer B. Insulin inhibits amyloid beta-induced cell death in cultured human brain pericytes. Neurobiol Aging. 2004;25:93-103. [PubMed] |
| 108. | Voll CL, Auer RN. Insulin attenuates ischemic brain damage independent of its hypoglycemic effect. J Cereb Blood Flow Metab. 1991;11:1006-1014. [PubMed] |
| 109. | Kopf SR, Baratti CM. The impairment of retention induced by insulin in mice may be mediated by a reduction in central cholinergic activity. Neurobiol Learn Mem. 1995;63:220-228. [PubMed] |
| 110. | Park CR. Cognitive effects of insulin in the central nervous system. Neurosci Biobehav Rev. 2001;25:311-323. [PubMed] |
| 111. | Moore RD. Effects of insulin upon ion transport. Biochim Biophys Acta. 1983;737:1-49. [PubMed] |
| 112. | Biessels GJ, Kamal A, Ramakers GM, Urban IJ, Spruijt BM, Erkelens DW, Gispen WH. Place learning and hippocampal synaptic plasticity in streptozotocin-induced diabetic rats. Diabetes. 1996;45:1259-1266. [PubMed] |
| 113. | Biessels GJ, Kamal A, Urban IJ, Spruijt BM, Erkelens DW, Gispen WH. Water maze learning and hippocampal synaptic plasticity in streptozotocin-diabetic rats: effects of insulin treatment. Brain Res. 1998;800:125-135. [PubMed] |
| 114. | Kamal A, Biessels GJ, Urban IJ, Gispen WH. Hippocampal synaptic plasticity in streptozotocin-diabetic rats: impairment of long-term potentiation and facilitation of long-term depression. Neuroscience. 1999;90:737-745. [PubMed] |
| 115. | Johnston AM, Pirola L, Van Obberghen E. Molecular mechanisms of insulin receptor substrate protein-mediated modulation of insulin signalling. FEBS Lett. 2003;546:32-36. [PubMed] |
| 116. | Bradley CA, Peineau S, Taghibiglou C, Nicolas CS, Whitcomb DJ, Bortolotto ZA, Kaang BK, Cho K, Wang YT, Collingridge GL. A pivotal role of GSK-3 in synaptic plasticity. Front Mol Neurosci. 2012;5:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 117. | Brietzke E, Kapczinski F, Grassi-Oliveira R, Grande I, Vieta E, McIntyre RS. Insulin dysfunction and allostatic load in bipolar disorder. Expert Rev Neurother. 2011;11:1017-1028. [PubMed] |
| 118. | Schultze SM, Jensen J, Hemmings BA, Tschopp O, Niessen M. Promiscuous affairs of PKB/AKT isoforms in metabolism. Arch Physiol Biochem. 2011;117:70-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 119. | Cooray S. The pivotal role of phosphatidylinositol 3-kinase-Akt signal transduction in virus survival. J Gen Virol. 2004;85:1065-1076. [PubMed] |
| 120. | Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5794] [Cited by in RCA: 6584] [Article Influence: 506.5] [Reference Citation Analysis (1)] |
| 121. | de la Monte SM. Brain insulin resistance and deficiency as therapeutic targets in Alzheimer’s disease. Curr Alzheimer Res. 2012;9:35-66. [PubMed] |
| 122. | Hoshi M, Takashima A, Noguchi K, Murayama M, Sato M, Kondo S, Saitoh Y, Ishiguro K, Hoshino T, Imahori K. Regulation of mitochondrial pyruvate dehydrogenase activity by tau protein kinase I/glycogen synthase kinase 3beta in brain. Proc Natl Acad Sci USA. 1996;93:2719-2723. [PubMed] |
| 123. | Hooper C, Killick R, Lovestone S. The GSK3 hypothesis of Alzheimer’s disease. J Neurochem. 2008;104:1433-1439. [PubMed] |
| 124. | Beurel E, Jope RS. The paradoxical pro- and anti-apoptotic actions of GSK3 in the intrinsic and extrinsic apoptosis signaling pathways. Prog Neurobiol. 2006;79:173-189. [PubMed] |
| 125. | Sun X, Sato S, Murayama O, Murayama M, Park JM, Yamaguchi H, Takashima A. Lithium inhibits amyloid secretion in COS7 cells transfected with amyloid precursor protein C100. Neurosci Lett. 2002;321:61-64. [PubMed] |
| 126. | Takashima A, Noguchi K, Sato K, Hoshino T, Imahori K. Tau protein kinase I is essential for amyloid beta-protein-induced neurotoxicity. Proc Natl Acad Sci USA. 1993;90:7789-7793. [PubMed] |
| 127. | Hanger DP, Hughes K, Woodgett JR, Brion JP, Anderton BH. Glycogen synthase kinase-3 induces Alzheimer’s disease-like phosphorylation of tau: generation of paired helical filament epitopes and neuronal localisation of the kinase. Neurosci Lett. 1992;147:58-62. [PubMed] |
| 128. | Ishiguro K, Omori A, Takamatsu M, Sato K, Arioka M, Uchida T, Imahori K. Phosphorylation sites on tau by tau protein kinase I, a bovine derived kinase generating an epitope of paired helical filaments. Neurosci Lett. 1992;148:202-206. [PubMed] |
| 129. | Lovestone S, Reynolds CH, Latimer D, Davis DR, Anderton BH, Gallo JM, Hanger D, Mulot S, Marquardt B, Stabel S. Alzheimer’s disease-like phosphorylation of the microtubule-associated protein tau by glycogen synthase kinase-3 in transfected mammalian cells. Curr Biol. 1994;4:1077-1086. [PubMed] |
| 130. | Cho JH, Johnson GV. Glycogen synthase kinase 3beta phosphorylates tau at both primed and unprimed sites. Differential impact on microtubule binding. J Biol Chem. 2003;278:187-193. [PubMed] |
| 131. | Asuni AA, Hooper C, Reynolds CH, Lovestone S, Anderton BH, Killick R. GSK3alpha exhibits beta-catenin and tau directed kinase activities that are modulated by Wnt. Eur J Neurosci. 2006;24:3387-3392. [PubMed] |
| 132. | Llorens-Martín M, Fuster-Matanzo A, Teixeira CM, Jurado-Arjona J, Ulloa F, Defelipe J, Rábano A, Hernández F, Soriano E, Avila J. GSK-3β overexpression causes reversible alterations on postsynaptic densities and dendritic morphology of hippocampal granule neurons in vivo. Mol Psychiatry. 2013;18:451-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 116] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 133. | Abraham WC, Tate WP. Metaplasticity: a new vista across the field of synaptic plasticity. Prog Neurobiol. 1997;52:303-323. [PubMed] |
| 134. | Peineau S, Bradley C, Taghibiglou C, Doherty A, Bortolotto ZA, Wang YT, Collingridge GL. The role of GSK-3 in synaptic plasticity. Br J Pharmacol. 2008;153 Suppl 1:S428-S437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 207] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 135. | Lucas FR, Goold RG, Gordon-Weeks PR, Salinas PC. Inhibition of GSK-3beta leading to the loss of phosphorylated MAP-1B is an early event in axonal remodelling induced by WNT-7a or lithium. J Cell Sci. 1998;111:1351-1361. [PubMed] |
| 136. | Lin CH, Yeh SH, Lin CH, Lu KT, Leu TH, Chang WC, Gean PW. A role for the PI-3 kinase signaling pathway in fear conditioning and synaptic plasticity in the amygdala. Neuron. 2001;31:841-851. [PubMed] |
| 137. | Daw MI, Bortolotto ZA, Saulle E, Zaman S, Collingridge GL, Isaac JT. Phosphatidylinositol 3 kinase regulates synapse specificity of hippocampal long-term depression. Nat Neurosci. 2002;5:835-836. [PubMed] |
| 138. | Sanna PP, Cammalleri M, Berton F, Simpson C, Lutjens R, Bloom FE, Francesconi W. Phosphatidylinositol 3-kinase is required for the expression but not for the induction or the maintenance of long-term potentiation in the hippocampal CA1 region. J Neurosci. 2002;22:3359-3365. [PubMed] |
| 139. | Liu SJ, Zhang AH, Li HL, Wang Q, Deng HM, Netzer WJ, Xu H, Wang JZ. Overactivation of glycogen synthase kinase-3 by inhibition of phosphoinositol-3 kinase and protein kinase C leads to hyperphosphorylation of tau and impairment of spatial memory. J Neurochem. 2003;87:1333-1344. [PubMed] |
| 140. | Kimura T, Yamashita S, Nakao S, Park JM, Murayama M, Mizoroki T, Yoshiike Y, Sahara N, Takashima A. GSK-3beta is required for memory reconsolidation in adult brain. PLoS One. 2008;3:e3540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 141. | Chen P, Gu Z, Liu W, Yan Z. Glycogen synthase kinase 3 regulates N-methyl-D-aspartate receptor channel trafficking and function in cortical neurons. Mol Pharmacol. 2007;72:40-51. [PubMed] |
| 142. | Wei J, Liu W, Yan Z. Regulation of AMPA receptor trafficking and function by glycogen synthase kinase 3. J Biol Chem. 2010;285:26369-26376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 143. | Koivisto L, Häkkinen L, Matsumoto K, McCulloch CA, Yamada KM, Larjava H. Glycogen synthase kinase-3 regulates cytoskeleton and translocation of Rac1 in long cellular extensions of human keratinocytes. Exp Cell Res. 2004;293:68-80. [PubMed] |
| 144. | Sirerol-Piquer M, Gomez-Ramos P, Hernández F, Perez M, Morán MA, Fuster-Matanzo A, Lucas JJ, Avila J, García-Verdugo JM. GSK3β overexpression induces neuronal death and a depletion of the neurogenic niches in the dentate gyrus. Hippocampus. 2011;21:910-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 145. | Fuster-Matanzo A, Llorens-Martín M, Sirerol-Piquer MS, García-Verdugo JM, Avila J, Hernández F. Dual effects of increased glycogen synthase kinase-3β activity on adult neurogenesis. Hum Mol Genet. 2013;22:1300-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 146. | Martin M, Rehani K, Jope RS, Michalek SM. Toll-like receptor-mediated cytokine production is differentially regulated by glycogen synthase kinase 3. Nat Immunol. 2005;6:777-784. [PubMed] |
| 147. | Jope RS, Yuskaitis CJ, Beurel E. Glycogen synthase kinase-3 (GSK3): inflammation, diseases, and therapeutics. Neurochem Res. 2007;32:577-595. [PubMed] |
| 148. | Tao GZ, Lehwald N, Jang KY, Baek J, Xu B, Omary MB, Sylvester KG. Wnt/β-catenin signaling protects mouse liver against oxidative stress-induced apoptosis through the inhibition of forkhead transcription factor FoxO3. J Biol Chem. 2013;288:17214-17224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 149. | Komiya Y, Habas R. Wnt signal transduction pathways. Organogenesis. 2008;4:68-75. [PubMed] |
| 150. | Parker JA, Vazquez-Manrique RP, Tourette C, Farina F, Offner N, Mukhopadhyay A, Orfila AM, Darbois A, Menet S, Tissenbaum HA. Integration of β-catenin, sirtuin, and FOXO signaling protects from mutant huntingtin toxicity. J Neurosci. 2012;32:12630-12640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 151. | Ren H, Plum-Morschel L, Gutierrez-Juarez R, Lu TY, Kim-Muller JY, Heinrich G, Wardlaw SL, Silver R, Accili D. Blunted refeeding response and increased locomotor activity in mice lacking FoxO1 in synapsin-Cre-expressing neurons. Diabetes. 2013;62:3373-3383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 152. | Kim KW, Donato J, Berglund ED, Choi YH, Kohno D, Elias CF, Depinho RA, Elmquist JK. FOXO1 in the ventromedial hypothalamus regulates energy balance. J Clin Invest. 2012;122:2578-2589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 153. | Oddo S. The role of mTOR signaling in Alzheimer disease. Front Biosci (Schol Ed). 2012;4:941-952. [PubMed] |
| 154. | An WL, Cowburn RF, Li L, Braak H, Alafuzoff I, Iqbal K, Iqbal IG, Winblad B, Pei JJ. Up-regulation of phosphorylated/activated p70 S6 kinase and its relationship to neurofibrillary pathology in Alzheimer’s disease. Am J Pathol. 2003;163:591-607. [PubMed] |
| 155. | Zhang F, Beharry ZM, Harris TE, Lilly MB, Smith CD, Mahajan S, Kraft AS. PIM1 protein kinase regulates PRAS40 phosphorylation and mTOR activity in FDCP1 cells. Cancer Biol Ther. 2009;8:846-853. [PubMed] |
| 156. | Caccamo A, Majumder S, Richardson A, Strong R, Oddo S. Molecular interplay between mammalian target of rapamycin (mTOR), amyloid-beta, and Tau: effects on cognitive impairments. J Biol Chem. 2010;285:13107-13120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 703] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 157. | Caccamo A, Maldonado MA, Majumder S, Medina DX, Holbein W, Magrí A, Oddo S. Naturally secreted amyloid-beta increases mammalian target of rapamycin (mTOR) activity via a PRAS40-mediated mechanism. J Biol Chem. 2011;286:8924-8932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 142] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 158. | Nixon RA. Autophagy, amyloidogenesis and Alzheimer disease. J Cell Sci. 2007;120:4081-4091. [PubMed] |
| 159. | Dobashi Y, Watanabe Y, Miwa C, Suzuki S, Koyama S. Mammalian target of rapamycin: a central node of complex signaling cascades. Int J Clin Exp Pathol. 2011;4:476-495. [PubMed] |
| 160. | Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471-484. [PubMed] |
| 161. | Betz C, Hall MN. Where is mTOR and what is it doing there? J Cell Biol. 2013;203:563-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 378] [Cited by in RCA: 426] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 162. | Kim DH, Sarbassov DD, Ali SM, King JE, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. mTOR interacts with raptor to form a nutrient-sensitive complex that signals to the cell growth machinery. Cell. 2002;110:163-175. [PubMed] |
| 163. | Kim DH, Sarbassov DD, Ali SM, Latek RR, Guntur KV, Erdjument-Bromage H, Tempst P, Sabatini DM. GbetaL, a positive regulator of the rapamycin-sensitive pathway required for the nutrient-sensitive interaction between raptor and mTOR. Mol Cell. 2003;11:895-904. [PubMed] |
| 164. | Stoica L, Zhu PJ, Huang W, Zhou H, Kozma SC, Costa-Mattioli M. Selective pharmacogenetic inhibition of mammalian target of Rapamycin complex I (mTORC1) blocks long-term synaptic plasticity and memory storage. Proc Natl Acad Sci USA. 2011;108:3791-3796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 188] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 165. | Son JH, Shim JH, Kim KH, Ha JY, Han JY. Neuronal autophagy and neurodegenerative diseases. Exp Mol Med. 2012;44:89-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 257] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 166. | Ferreira ST, Clarke JR, Bomfim TR, De Felice FG. Inflammation, defective insulin signaling, and neuronal dysfunction in Alzheimer’s disease. Alzheimers Dement. 2014;10:S76-S83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 264] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 167. | De Felice FG, Ferreira ST. Inflammation, defective insulin signaling, and mitochondrial dysfunction as common molecular denominators connecting type 2 diabetes to Alzheimer disease. Diabetes. 2014;63:2262-2272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 453] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 168. | Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N. A meta-analysis of cytokines in Alzheimer’s disease. Biol Psychiatry. 2010;68:930-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 740] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 169. | Kanety H, Feinstein R, Papa MZ, Hemi R, Karasik A. Tumor necrosis factor alpha-induced phosphorylation of insulin receptor substrate-1 (IRS-1). Possible mechanism for suppression of insulin-stimulated tyrosine phosphorylation of IRS-1. J Biol Chem. 1995;270:23780-23784. [PubMed] |
| 170. | Rui L, Aguirre V, Kim JK, Shulman GI, Lee A, Corbould A, Dunaif A, White MF. Insulin/IGF-1 and TNF-alpha stimulate phosphorylation of IRS-1 at inhibitory Ser307 via distinct pathways. J Clin Invest. 2001;107:181-189. [PubMed] |
| 171. | Hirosumi J, Tuncman G, Chang L, Görgün CZ, Uysal KT, Maeda K, Karin M, Hotamisligil GS. A central role for JNK in obesity and insulin resistance. Nature. 2002;420:333-336. [PubMed] |
| 172. | Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409-2415. [PubMed] |
| 173. | Samad F, Uysal KT, Wiesbrock SM, Pandey M, Hotamisligil GS, Loskutoff DJ. Tumor necrosis factor alpha is a key component in the obesity-linked elevation of plasminogen activator inhibitor 1. Proc Natl Acad Sci USA. 1999;96:6902-6907. [PubMed] |
| 174. | Bonnet MC, Weil R, Dam E, Hovanessian AG, Meurs EF. PKR stimulates NF-kappaB irrespective of its kinase function by interacting with the IkappaB kinase complex. Mol Cell Biol. 2000;20:4532-4542. [PubMed] |
| 175. | Takada Y, Ichikawa H, Pataer A, Swisher S, Aggarwal BB. Genetic deletion of PKR abrogates TNF-induced activation of IkappaBalpha kinase, JNK, Akt and cell proliferation but potentiates p44/p42 MAPK and p38 MAPK activation. Oncogene. 2007;26:1201-1212. [PubMed] |
| 176. | Costello DA, Claret M, Al-Qassab H, Plattner F, Irvine EE, Choudhury AI, Giese KP, Withers DJ, Pedarzani P. Brain deletion of insulin receptor substrate 2 disrupts hippocampal synaptic plasticity and metaplasticity. PLoS One. 2012;7:e31124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 177. | Zhao WQ, Chen H, Quon MJ, Alkon DL. Insulin and the insulin receptor in experimental models of learning and memory. Eur J Pharmacol. 2004;490:71-81. [PubMed] |
| 178. | Smith MA, Sayre LM, Monnier VM, Perry G. Radical AGEing in Alzheimer’s disease. Trends Neurosci. 1995;18:172-176. [PubMed] |
| 179. | Li X, Fang P, Mai J, Choi ET, Wang H, Yang XF. Targeting mitochondrial reactive oxygen species as novel therapy for inflammatory diseases and cancers. J Hematol Oncol. 2013;6:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 453] [Cited by in RCA: 557] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 180. | Moreira PI, Harris PL, Zhu X, Santos MS, Oliveira CR, Smith MA, Perry G. Lipoic acid and N-acetyl cysteine decrease mitochondrial-related oxidative stress in Alzheimer disease patient fibroblasts. J Alzheimers Dis. 2007;12:195-206. [PubMed] |
| 181. | Hauptmann S, Scherping I, Dröse S, Brandt U, Schulz KL, Jendrach M, Leuner K, Eckert A, Müller WE. Mitochondrial dysfunction: an early event in Alzheimer pathology accumulates with age in AD transgenic mice. Neurobiol Aging. 2009;30:1574-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 352] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 182. | Fu YJ, Xiong S, Lovell MA, Lynn BC. Quantitative proteomic analysis of mitochondria in aging PS-1 transgenic mice. Cell Mol Neurobiol. 2009;29:649-664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 183. | Nunomura A, Perry G, Aliev G, Hirai K, Takeda A, Balraj EK, Jones PK, Ghanbari H, Wataya T, Shimohama S. Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol. 2001;60:759-767. [PubMed] |
| 184. | Aliyev A, Chen SG, Seyidova D, Smith MA, Perry G, de la Torre J, Aliev G. Mitochondria DNA deletions in atherosclerotic hypoperfused brain microvessels as a primary target for the development of Alzheimer’s disease. J Neurol Sci. 2005;229-230:285-292. [PubMed] |
| 185. | Devi L, Prabhu BM, Galati DF, Avadhani NG, Anandatheerthavarada HK. Accumulation of amyloid precursor protein in the mitochondrial import channels of human Alzheimer’s disease brain is associated with mitochondrial dysfunction. J Neurosci. 2006;26:9057-9068. [PubMed] |
| 186. | Su B, Wang X, Nunomura A, Moreira PI, Lee HG, Perry G, Smith MA, Zhu X. Oxidative stress signaling in Alzheimer’s disease. Curr Alzheimer Res. 2008;5:525-532. [PubMed] |
| 187. | Anandatheerthavarada HK, Biswas G, Robin MA, Avadhani NG. Mitochondrial targeting and a novel transmembrane arrest of Alzheimer’s amyloid precursor protein impairs mitochondrial function in neuronal cells. J Cell Biol. 2003;161:41-54. [PubMed] |
| 188. | Marshall S, Garvey WT, Traxinger RR. New insights into the metabolic regulation of insulin action and insulin resistance: role of glucose and amino acids. FASEB J. 1991;5:3031-3036. [PubMed] |
| 189. | Schleicher ED, Weigert C. Role of the hexosamine biosynthetic pathway in diabetic nephropathy. Kidney Int Suppl. 2000;77:S13-S18. [PubMed] |
| 190. | Wojtczak L, Schönfeld P. Effect of fatty acids on energy coupling processes in mitochondria. Biochim Biophys Acta. 1993;1183:41-57. [PubMed] |
| 191. | Bakker SJ, IJzerman RG, Teerlink T, Westerhoff HV, Gans RO, Heine RJ. Cytosolic triglycerides and oxidative stress in central obesity: the missing link between excessive atherosclerosis, endothelial dysfunction, and beta-cell failure? Atherosclerosis. 2000;148:17-21. [PubMed] |
| 192. | Hazel JR, Williams EE. The role of alterations in membrane lipid composition in enabling physiological adaptation of organisms to their physical environment. Prog Lipid Res. 1990;29:167-227. [PubMed] |
| 193. | Lovell MA, Ehmann WD, Butler SM, Markesbery WR. Elevated thiobarbituric acid-reactive substances and antioxidant enzyme activity in the brain in Alzheimer’s disease. Neurology. 1995;45:1594-1601. [PubMed] |
| 194. | Palmer AM, Burns MA. Selective increase in lipid peroxidation in the inferior temporal cortex in Alzheimer’s disease. Brain Res. 1994;645:338-342. [PubMed] |
| 195. | Marcus DL, Thomas C, Rodriguez C, Simberkoff K, Tsai JS, Strafaci JA, Freedman ML. Increased peroxidation and reduced antioxidant enzyme activity in Alzheimer’s disease. Exp Neurol. 1998;150:40-44. [PubMed] |
| 196. | Dyrks T, Dyrks E, Hartmann T, Masters C, Beyreuther K. Amyloidogenicity of beta A4 and beta A4-bearing amyloid protein precursor fragments by metal-catalyzed oxidation. J Biol Chem. 1992;267:18210-18217. [PubMed] |
| 197. | Thomas T, Thomas G, McLendon C, Sutton T, Mullan M. beta-Amyloid-mediated vasoactivity and vascular endothelial damage. Nature. 1996;380:168-171. [PubMed] |
| 198. | Knott AB, Bossy-Wetzel E. Impairing the mitochondrial fission and fusion balance: a new mechanism of neurodegeneration. Ann N Y Acad Sci. 2008;1147:283-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 197] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 199. | Desco MC, Asensi M, Márquez R, Martínez-Valls J, Vento M, Pallardó FV, Sastre J, Viña J. Xanthine oxidase is involved in free radical production in type 1 diabetes: protection by allopurinol. Diabetes. 2002;51:1118-1124. [PubMed] |
| 200. | Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991;40:405-412. [PubMed] |
| 201. | Reagan LP, Magariños AM, Yee DK, Swzeda LI, Van Bueren A, McCall AL, McEwen BS. Oxidative stress and HNE conjugation of GLUT3 are increased in the hippocampus of diabetic rats subjected to stress. Brain Res. 2000;862:292-300. [PubMed] |
| 202. | Evans JL, Goldfine ID, Maddux BA, Grodsky GM. Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev. 2002;23:599-622. [PubMed] |
| 203. | Schmitt K, Grimm A, Kazmierczak A, Strosznajder JB, Götz J, Eckert A. Insights into mitochondrial dysfunction: aging, amyloid-β, and tau-A deleterious trio. Antioxid Redox Signal. 2012;16:1456-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 103] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 204. | Moreira PI, Santos MS, Sena C, Nunes E, Seiça R, Oliveira CR. CoQ10 therapy attenuates amyloid beta-peptide toxicity in brain mitochondria isolated from aged diabetic rats. Exp Neurol. 2005;196:112-119. [PubMed] |
| 205. | Kristal BS, Jackson CT, Chung HY, Matsuda M, Nguyen HD, Yu BP. Defects at center P underlie diabetes-associated mitochondrial dysfunction. Free Radic Biol Med. 1997;22:823-833. [PubMed] |
| 206. | Calabrese V, Scapagnini G, Giuffrida Stella AM, Bates TE, Clark JB. Mitochondrial involvement in brain function and dysfunction: relevance to aging, neurodegenerative disorders and longevity. Neurochem Res. 2001;26:739-764. [PubMed] |
| 207. | Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615-1625. [PubMed] |
| 208. | Gerbitz KD, Gempel K, Brdiczka D. Mitochondria and diabetes. Genetic, biochemical, and clinical implications of the cellular energy circuit. Diabetes. 1996;45:113-126. [PubMed] |
| 209. | Takuma K, Yao J, Huang J, Xu H, Chen X, Luddy J, Trillat AC, Stern DM, Arancio O, Yan SS. ABAD enhances Abeta-induced cell stress via mitochondrial dysfunction. FASEB J. 2005;19:597-598. [PubMed] |
| 210. | Moreira PI, Santos MS, Sena C, Seiça R, Oliveira CR. Insulin protects against amyloid beta-peptide toxicity in brain mitochondria of diabetic rats. Neurobiol Dis. 2005;18:628-637. [PubMed] |
| 211. | Moreira PI, Santos MS, Moreno AM, Seiça R, Oliveira CR. Increased vulnerability of brain mitochondria in diabetic (Goto-Kakizaki) rats with aging and amyloid-beta exposure. Diabetes. 2003;52:1449-1456. [PubMed] |
| 212. | Lustbader JW, Cirilli M, Lin C, Xu HW, Takuma K, Wang N, Caspersen C, Chen X, Pollak S, Chaney M. ABAD directly links Abeta to mitochondrial toxicity in Alzheimer’s disease. Science. 2004;304:448-452. [PubMed] |
| 213. | Leissring MA, Farris W, Wu X, Christodoulou DC, Haigis MC, Guarente L, Selkoe DJ. Alternative translation initiation generates a novel isoform of insulin-degrading enzyme targeted to mitochondria. Biochem J. 2004;383:439-446. [PubMed] |
| 214. | Pereira C, Santos MS, Oliveira C. Mitochondrial function impairment induced by amyloid beta-peptide on PC12 cells. Neuroreport. 1998;9:1749-1755. [PubMed] |
| 215. | Pereira C, Santos MS, Oliveira C. Involvement of oxidative stress on the impairment of energy metabolism induced by A beta peptides on PC12 cells: protection by antioxidants. Neurobiol Dis. 1999;6:209-219. [PubMed] |
| 216. | Dumont M, Kipiani K, Yu F, Wille E, Katz M, Calingasan NY, Gouras GK, Lin MT, Beal MF. Coenzyme Q10 decreases amyloid pathology and improves behavior in a transgenic mouse model of Alzheimer’s disease. J Alzheimers Dis. 2011;27:211-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 217. | Perry EK, Perry RH, Tomlinson BE, Blessed G, Gibson PH. Coenzyme A-acetylating enzymes in Alzheimer’s disease: possible cholinergic ‘compartment’ of pyruvate dehydrogenase. Neurosci Lett. 1980;18:105-110. [PubMed] |
| 218. | Wang X, Su B, Siedlak SL, Moreira PI, Fujioka H, Wang Y, Casadesus G, Zhu X. Amyloid-beta overproduction causes abnormal mitochondrial dynamics via differential modulation of mitochondrial fission/fusion proteins. Proc Natl Acad Sci USA. 2008;105:19318-19323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 565] [Cited by in RCA: 678] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 219. | Wang X, Su B, Fujioka H, Zhu X. Dynamin-like protein 1 reduction underlies mitochondrial morphology and distribution abnormalities in fibroblasts from sporadic Alzheimer’s disease patients. Am J Pathol. 2008;173:470-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 286] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 220. | Oettinghaus B, Licci M, Scorrano L, Frank S. Less than perfect divorces: dysregulated mitochondrial fission and neurodegeneration. Acta Neuropathol. 2012;123:189-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 221. | Pagani L, Eckert A. Amyloid-Beta interaction with mitochondria. Int J Alzheimers Dis. 2011;2011:925050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 156] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 222. | Zhao WQ, Alkon DL. Role of insulin and insulin receptor in learning and memory. Mol Cell Endocrinol. 2001;177:125-134. [PubMed] |
| 223. | Erol A. An integrated and unifying hypothesis for the metabolic basis of sporadic Alzheimer’s disease. J Alzheimers Dis. 2008;13:241-253. [PubMed] |
| 224. | Zang M, Zuccollo A, Hou X, Nagata D, Walsh K, Herscovitz H, Brecher P, Ruderman NB, Cohen RA. AMP-activated protein kinase is required for the lipid-lowering effect of metformin in insulin-resistant human HepG2 cells. J Biol Chem. 2004;279:47898-47905. [PubMed] |
| 225. | Hilder TL, Baer LA, Fuller PM, Fuller CA, Grindeland RE, Wade CE, Graves LM. Insulin-independent pathways mediating glucose uptake in hindlimb-suspended skeletal muscle. J Appl Physiol (1985). 2005;99:2181-2188. [PubMed] |
| 227. | Wang J, Gallagher D, DeVito LM, Cancino GI, Tsui D, He L, Keller GM, Frankland PW, Kaplan DR, Miller FD. Metformin activates an atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory formation. Cell Stem Cell. 2012;11:23-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 358] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 228. | Hsu CC, Wahlqvist ML, Lee MS, Tsai HN. Incidence of dementia is increased in type 2 diabetes and reduced by the use of sulfonylureas and metformin. J Alzheimers Dis. 2011;24:485-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 281] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 229. | Moore EM, Mander AG, Ames D, Kotowicz MA, Carne RP, Brodaty H, Woodward M, Boundy K, Ellis KA, Bush AI. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care. 2013;36:2981-2987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 290] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 230. | Exalto LG, Whitmer RA, Kappele LJ, Biessels GJ. An update on type 2 diabetes, vascular dementia and Alzheimer’s disease. Exp Gerontol. 2012;47:858-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 231. | Khanfar MA, AbuKhader MM, Alqtaishat S, Taha MO. Pharmacophore modeling, homology modeling, and in silico screening reveal mammalian target of rapamycin inhibitory activities for sotalol, glyburide, metipranolol, sulfamethizole, glipizide, and pioglitazone. J Mol Graph Model. 2013;42:39-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 232. | Lamkanfi M, Mueller JL, Vitari AC, Misaghi S, Fedorova A, Deshayes K, Lee WP, Hoffman HM, Dixit VM. Glyburide inhibits the Cryopyrin/Nalp3 inflammasome. J Cell Biol. 2009;187:61-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 548] [Cited by in RCA: 673] [Article Influence: 42.1] [Reference Citation Analysis (0)] |
| 233. | Gradman TJ, Laws A, Thompson LW, Reaven GM. Verbal learning and/or memory improves with glycemic control in older subjects with non-insulin-dependent diabetes mellitus. J Am Geriatr Soc. 1993;41:1305-1312. [PubMed] |
| 234. | Imfeld P, Bodmer M, Jick SS, Meier CR. Metformin, other antidiabetic drugs, and risk of Alzheimer’s disease: a population-based case-control study. J Am Geriatr Soc. 2012;60:916-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 286] [Article Influence: 22.0] [Reference Citation Analysis (1)] |
| 235. | Hoyer S. Glucose metabolism and insulin receptor signal transduction in Alzheimer disease. Eur J Pharmacol. 2004;490:115-125. [PubMed] |
| 236. | Pandini G, Pace V, Copani A, Squatrito S, Milardi D, Vigneri R. Insulin has multiple antiamyloidogenic effects on human neuronal cells. Endocrinology. 2013;154:375-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 237. | De Felice FG, Vieira MN, Bomfim TR, Decker H, Velasco PT, Lambert MP, Viola KL, Zhao WQ, Ferreira ST, Klein WL. Protection of synapses against Alzheimer’s-linked toxins: insulin signaling prevents the pathogenic binding of Abeta oligomers. Proc Natl Acad Sci USA. 2009;106:1971-1976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 503] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 238. | Gavin JR, Stolar MW, Freeman JS, Spellman CW. Improving outcomes in patients with type 2 diabetes mellitus: practical solutions for clinical challenges. J Am Osteopath Assoc. 2010;110:S2-14; quiz S15-S16. [PubMed] |
| 239. | Cignarelli A, Giorgino F, Vettor R. Pharmacologic agents for type 2 diabetes therapy and regulation of adipogenesis. Arch Physiol Biochem. 2013;119:139-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 240. | Heneka MT, Landreth GE, Feinstein DL. Role for peroxisome proliferator-activated receptor-gamma in Alzheimer’s disease. Ann Neurol. 2001;49:276. [PubMed] |
| 241. | Watson GS, Cholerton BA, Reger MA, Baker LD, Plymate SR, Asthana S, Fishel MA, Kulstad JJ, Green PS, Cook DG. Preserved cognition in patients with early Alzheimer disease and amnestic mild cognitive impairment during treatment with rosiglitazone: a preliminary study. Am J Geriatr Psychiatry. 2005;13:950-958. [PubMed] |
| 242. | Landreth G, Jiang Q, Mandrekar S, Heneka M. PPARgamma agonists as therapeutics for the treatment of Alzheimer’s disease. Neurotherapeutics. 2008;5:481-489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 210] [Cited by in RCA: 209] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 243. | Pathan AR, Viswanad B, Sonkusare SK, Ramarao P. Chronic administration of pioglitazone attenuates intracerebroventricular streptozotocin induced-memory impairment in rats. Life Sci. 2006;79:2209-2216. [PubMed] |
| 244. | Risner ME, Saunders AM, Altman JF, Ormandy GC, Craft S, Foley IM, Zvartau-Hind ME, Hosford DA, Roses AD. Efficacy of rosiglitazone in a genetically defined population with mild-to-moderate Alzheimer’s disease. Pharmacogenomics J. 2006;6:246-254. [PubMed] |
| 245. | Gold M, Alderton C, Zvartau-Hind M, Egginton S, Saunders AM, Irizarry M, Craft S, Landreth G, Linnamägi U, Sawchak S. Rosiglitazone monotherapy in mild-to-moderate Alzheimer’s disease: results from a randomized, double-blind, placebo-controlled phase III study. Dement Geriatr Cogn Disord. 2010;30:131-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 266] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 246. | Hölscher C. The role of GLP-1 in neuronal activity and neurodegeneration. Vitam Horm. 2010;84:331-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 247. | Bomfim TR, Forny-Germano L, Sathler LB, Brito-Moreira J, Houzel JC, Decker H, Silverman MA, Kazi H, Melo HM, McClean PL. An anti-diabetes agent protects the mouse brain from defective insulin signaling caused by Alzheimer’s disease- associated Aβ oligomers. J Clin Invest. 2012;122:1339-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 574] [Cited by in RCA: 683] [Article Influence: 52.5] [Reference Citation Analysis (0)] |
| 248. | Hunter K, Hölscher C. Drugs developed to treat diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. BMC Neurosci. 2012;13:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 298] [Cited by in RCA: 381] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 249. | McClean PL, Parthsarathy V, Faivre E, Hölscher C. The diabetes drug liraglutide prevents degenerative processes in a mouse model of Alzheimer’s disease. J Neurosci. 2011;31:6587-6594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 539] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 250. | Yang Y, Zhang J, Ma D, Zhang M, Hu S, Shao S, Gong CX. Subcutaneous administration of liraglutide ameliorates Alzheimer-associated tau hyperphosphorylation in rats with type 2 diabetes. J Alzheimers Dis. 2013;37:637-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 251. | Egefjord L, Gejl M, Møller A, Brændgaard H, Gottrup H, Antropova O, Møller N, Poulsen HE, Gjedde A, Brock B. Effects of liraglutide on neurodegeneration, blood flow and cognition in Alzheimer´s disease - protocol for a controlled, randomized double-blinded trial. Dan Med J. 2012;59:A4519. [PubMed] |
| 252. | D’Amico M, Di Filippo C, Marfella R, Abbatecola AM, Ferraraccio F, Rossi F, Paolisso G. Long-term inhibition of dipeptidyl peptidase-4 in Alzheimer’s prone mice. Exp Gerontol. 2010;45:202-207. [PubMed] |
| 253. | Beeri MS, Schmeidler J, Silverman JM, Gandy S, Wysocki M, Hannigan CM, Purohit DP, Lesser G, Grossman HT, Haroutunian V. Insulin in combination with other diabetes medication is associated with less Alzheimer neuropathology. Neurology. 2008;71:750-757. [PubMed] |
| 254. | McIntosh CH, Demuth HU, Pospisilik JA, Pederson R. Dipeptidyl peptidase IV inhibitors: how do they work as new antidiabetic agents? Regul Pept. 2005;128:159-165. [PubMed] |
| 255. | Ryan CM, Freed MI, Rood JA, Cobitz AR, Waterhouse BR, Strachan MW. Improving metabolic control leads to better working memory in adults with type 2 diabetes. Diabetes Care. 2006;29:345-351. [PubMed] |
| 256. | Hewer W, Mussell M, Rist F, Kulzer B, Bergis K. Short-term effects of improved glycemic control on cognitive function in patients with type 2 diabetes. Gerontology. 2003;49:86-92. [PubMed] |