Published online May 15, 2023. doi: 10.4239/wjd.v14.i5.585
Peer-review started: December 28, 2022
First decision: January 9, 2023
Revised: January 20, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: May 15, 2023
Processing time: 137 Days and 18.4 Hours
Diabetes mellitus (DM) is still one of the most common diseases worldwide, and its prevalence is still increasing globally. According to the American and European recommendations, metformin is considered a first-line oral hypo-glycemic drug for controlling type 2 DM (T2DM) patients. Metformin is the ninth most often prescribed drug in the world, and at least 120 million diabetic people are estimated to receive the drug. In the last 20 years, there has been increasing evidence of vitamin B12 deficiency among metformin-treated diabetic patients. Many studies have reported that vitamin B12 deficiency is related to the ma-labsorption of vitamin B12 among metformin-treated T2DM patients. Vitamin B12 deficiency may have a very bad complication for the T2DM patient. In this review, we will focus on the effect of metformin on the absorption of vitamin B12 and on its proposed mechanisms in hindering vitamin B12 absorption. In addition, the review will describe the clinical outcomes of vitamin B12 deficiency in metformin-treated T2DM.
Core Tip: In the last 20 years, there was increasing evidence of the presence of vitamin B12 deficiency among metformin-treated diabetic patients. Vitamin B12 deficiency may have a very bad complication for the T2DM patient. This review will focus on the effect of metformin on the absorption of vitamin B12 and on its proposed mechanisms in hindering vitamin B12 absorption. In addition to that, the review will describe the clinical outcomes of vitamin B12 deficiency in metformin-treated T2DM.
- Citation: Sayedali E, Yalin AE, Yalin S. Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes. World J Diabetes 2023; 14(5): 585-593
- URL: https://www.wjgnet.com/1948-9358/full/v14/i5/585.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i5.585
Diabetes mellitus (DM) is a chronic metabolic disorder diagnosed by abnormally high blood glucose levels. It is considered one of the most common diseases that lead to mortality and morbidity worldwide. Despite the development of health systems and public health concepts, the prevalence of DM is increasing globally[1]. According to current estimates, the number of people with diabetes in France and Belgium will rise by 17% by 2035, with an increase of 22% in the United States and the United Kingdom, 31% in Canada, and 3% to 37% in other European Union nations[2,3]. As known, uncontrolled DM may be the main cause of mortality among people[4]. The leading cause of morbidity and mortality in people with diabetes is vascular complications, which affect both the macrovascular system [cardiovascular disease (CVD)] and the microvascular system [diabetic kidney disease (DKD)], as well as diabetic retinopathy and neuropathy[5].
Metformin is considered one of the most important hypoglycemic drugs used to control the hyperglycemic state in patients with DM. It is mainly used in patients with Type 2 DM (T2DM) and both European and American recommendations recommend it as a first-line pharmacological treatment for T2DM[6-8]. According to many clinical trials, the drug improves cardiovascular outcomes in T2DM patients. Metformin is currently the most frequently given oral anti-diabetic drug because of its demonstrated efficacy, comparatively low risk, and potential for usage with other anti-diabetic drugs. More than 150 million diabetic patients are thought to receive the drug regularly worldwide[9].
In the last 20 years, there was increasing evidence of vitamin B12 deficiency among metformin-treated diabetic patients[10,11]. Many studies have reported that vitamin B12 deficiency is related to the malabsorption of vitamin B12 among metformin-treated T2DM patients[11-13]. Vitamin B12 deficiency may have terrible complications for T2DM patients, which should be considered during the therapeutic plan[12,14]. In this review, we will focus on the effect of metformin on the absorption of vitamin B12 and on its proposed mechanisms in hindering vitamin B12 absorption. In addition, the review will describe the clinical outcomes of vitamin B12 deficiency in metformin-treated T2DM and the impact of metformin use on serum vitamin B12.
DM is a chronic metabolic disorder characterized to be an elevation in blood glucose levels caused by an absolute or relative insulin insufficiency, insulin resistance due to dysfunctional cells, or both. Other clinically discernible subtypes of diabetes exist, including monogenic diabetes (such as maturity-onset diabetes of the young or neonatal diabetes), gestational diabetes, and possibly a late-onset autoimmune form (latent autoimmune diabetes in adults)[12,15].
Diabetes is traditionally divided into an early-onset autoimmune form (T1D) and a late-onset non-autoimmune form (T2D). In fact, T2D is generally used to describe any type of diabetes that is not autoimmune or monogenic in origin, and it is becoming more widely acknowledged that it may reflect a collection of several pathophysiological states[4].
Deficient insulin production is a hallmark of T1D, sometimes referred to as insulin-dependent, juvenile, or childhood-onset, which necessitates daily insulin therapy. T1D affected 9 million people in 2017, the majority of whom reside in high-income regions. Its etiology and prevention methods are unknown. Some of the symptoms are polyuria, polydipsia, polyphagia, weight loss, visual abnormalities, and exhaustion. These signs could appear out of nowhere[16].
The body’s inefficient use of insulin causes T2D; it is also known as non-insulin-dependent or adult-onset diabetes. T2D affects more than 95% of those who have the disease and is primarily caused by increased total body mass index and low physical activity[17].
Symptoms may be like those of T1D but are often less marked. As a result, the disease may be diagnosed several years after onset, after complications have already arisen. This type of diabetes was previously exclusively found in adults, but it is now increasingly common in kids as well.
Both types of DM have a lot of complications in different vital systems in the human body. Diabetes is linked with long-term damage to both large and small blood vessels throughout the body, referred to as the macrovascular and microvascular systems[18]. Even though damage from high blood sugar to the macrovascular system, such as the coronary and cerebral arteries, is the primary cause of death in people with T2D, damage from high blood sugar to the microvascular system in the kidney, eyes, and nerves is far more frequent and significantly affects mortality[1].
Macrovascular complications: CVD is the primary cause of mortality for most of the diabetic population. Macrovascular problems are mostly caused by atherosclerotic constriction of arteries and veins, which results in cardiovascular, cerebrovascular, or peripheral artery diseases (PADs). Diabetes is a significant, manageable, independent risk factor for the development of CVD[19]. Cerebrovascular diseases, such as stroke and ischemia, occur in 20%-40% of diabetics due to atherosclerotic narrowing of the intracranial vessels and carotid artery. About 80% of diabetics over the age of 65 die of heart disease, and about 16% die from stroke[15,18].
Another very important complication is PAD which is an atherosclerotic occlusive disease of the lower extremities. And it carries a considerable risk of amputation for the affected limbs. One of the independent risk factors for the onset of PAD is DM. Particularly, diabetic people frequently experience critical limb ischemia, an advanced type of PAD that causes rest pain and long-term disability[20].
Microvascular complications: Uncontrolled hyperglycemic status can lead to microvascular complications like microangiopathy, nephropathy, neuropathy, and retinopathy by affecting small vessels, including capillaries[21]. One of the most common complications among diabetic patients is diabetes-related kidney dysfunction, also known as diabetic nephropathy or DKD. It is characterized by unusually high levels of albumin excretion with urine and a decreased glomerular filtration rate because of lesions that have developed in the glomerulus. In addition to that, people with long-term diabetes develop diabetic neuropathy because of chronic nerve damage[4,15,22].
Another common complication is diabetic retinopathy, where one-third of people with hypertension and high blood sugar are also diagnosed with diabetic retinopathy. Increased vascular permeability, the thickness of the retina, and neovascularization of the retina are its defining features, all of which cause vision loss. It is among the leading causes of long-term blindness and vision impairment in diabetics[23].
As we have mentioned before, the main feature of DM is the uncontrolled hyperglycemic state closely related to cell damage. Hyperglycemia causes an increase in reactive oxygen species (ROS) production, which causes oxidative stress in the body[18]. In normal circumstances, glucose is metabolized by way of the glycolysis pathways, followed by the tricarboxylic acid (TCA) cycle in mitochondria. This results in the generation of electron donors such as NADH (reduced nicotinamide adenine dinucleotide) and FADH2 (reduced flavin adenine dinucleotide), which play an essential role in transferring electrons to the molecular oxygen by the electron transport chain (ETC), so reducing the oxygen to water[18,24].
On the other hand, in the case of uncontrolled hyperglycemia, the increased rate of glucose oxidation in the TCA cycle increases the transport of electron donors into the ETC. This hinders the ETC, causing superoxide to be produced instead of water as the voltage gradient increases and reaches a critical threshold limit[18]. As a result, the increase in ROS-like superoxide in diabetic microvasculature can stimulate endothelial cell damage and, consequently a lot of micro and macrovascular complications.
Metformin is a biguanide derivative and one of the most common oral anti-diabetic drugs. It is used mainly to treat T2D, especially in obese people. Compared to insulin, glibenclamide, and chlorpropamide, metformin has been found to reduce diabetes mortality and complications by 30%[7,11,25].
Metformin lowers serum glucose levels through several mechanisms without increasing insulin secretion. It is recognized as an insulin sensitizer because it enhances the cells’ response to insulin[25]. In addition, metformin suppresses the liver’s endogenous glucose synthesis primarily due to a decrease in the rate of gluconeogenesis and a minor impact on glycogenolysis. Furthermore, metformin stimulates insulin signaling and glucose transport in muscles while inhibiting critical enzymes involved in gluconeogenesis and glycogen production in the liver when the enzyme adenosine monophosphate kinase (AMPK) is activated[7,25,26].
Recent studies showed that metformin could reduce microvascular and macrovascular complications by its role in inhibiting the cell damage process in big and small vessels. This effect of metformin is mainly mediated by its action on AMP-activated kinase in tissues and its ability to reduce intracellular ROS[8,27]. In the same context, many studies showed that metformin could decrease the prevalence of nephropathy among diabetic patients by controlling oxidative stress and reversing the biochemical changes in renal tubules, consequently preventing tubular injury[28]. According to the previous findings, metformin is currently the most frequently given oral anti-diabetic drug because of its demonstrated efficacy, comparatively low risk, and potential for usage with other anti-diabetic medications. 150 million diabetic individuals are estimated to receive the drug regularly worldwide[25].
Metformin does not have many side effects, but it can result in lactic acidosis, a severe condition with the following symptoms: Dizziness, significant drowsiness, pain in the muscles, fatigue, chills, blue or pale skin, rapid or difficult breathing, slow or irregular heartbeat, stomach pain with diarrhea, nausea, or vomiting[29].
The possibility of lactic acidosis can increase in the presence of other conditions that cause a low level of oxygen in the blood or poor circulation (such as a recent stroke, congestive heart failure, or recent heart attack), heavy alcohol use, and dehydration[30]. While lactic acidosis is uncommon, gas-trointestinal intolerance is one of the most frequently occurring side effects among metformin-treated T2DM patients[7].
Vitamin B12 malabsorption is another reported side effect of metformin usage in T2DM patients. There are varying degrees of evidence to support the link between metformin use and low vitamin B12 levels[13,31,32]. However, a few issues with the topic need to be clarified. Through this review, we will try to focus mainly on the possible relationship between metformin use and vitamin B12 deficiency.
In the last two decades, there has been an increasing interest in the relationship between metformin and vitamin B12 deficiency. The first report of metformin-associated vitamin B12 malabsorption was made in 1971 by Tomkin et al[33]. After that, many experimental, observational studies, and systematic reviews described the relationship between metformin and vitamin B12 deficiency in T2DM patients[6,13,31,32]. The effect of metformin on vitamin B12 absorption is also reported in metformin-treated polycystic ovary syndrome (PCOS) patients. A meta-analysis of six randomized controlled trials showed that metformin use caused dose-dependent drops in vitamin B12 levels in patients with T2DM or PCOS[34]. The importance of an accurate description of the association between the use of metformin and vitamin B12 comes from the significance of the clinical manifestations of vitamin B12 deficiency and its impact on the quality of diabetic patients’ life. To better understand the relationship between metformin and vitamin B12 deficiency, we should have a good understanding of the nature of vitamin B12, the mechanism of its absorption, and how metformin can decrease its absorption.
Cobalamin, often known as vitamin B12, is a water-soluble vitamin that contains cobalt and functions as a co-factor for enzymes that are important for metabolism[35]. All cobalamin active in humans, such as cyanocobalamin, hydroxocobalamin, methyl cobalamin, and 5-deoxyadenosine cobalamin, are referred to as vitamin B12 (adenosyl-Cbl). However, different dosage forms of the first three types are offered as commercial products. The physiologically active forms of vitamin B12, adenosyl-Cbl, and methyl cobalamin, are produced intracellularly from all forms of the vitamin[5,36,37]. Vitamin B12 is an essential co-factor in intracellular enzyme activities involved in DNA synthesis and amino acid and fatty acid metabolism. In addition, it is necessary for erythropoiesis and the proper function of the central nervous system[35,37].
Vitamin B12 is absorbed by target cells through a difficult course that includes various proteins and receptors. Understanding the multistep process of vitamin B12 absorption is very important to understand the link between malabsorption of vitamin B12 in the presence of other medications like metformin.
Dietary vitamin B12 is generally founded in a protein-bound form. Protein-bound vitamin B12 is detached in the stomach because of gastric acid and pepsin. After that, the free vitamin is joined to R-binder, a salivary and gastric glycoprotein that shields vitamin B12 from the highly acidic stomach environment. R-binder is broken down by pancreatic proteases in the duodenum, releasing vitamin B12. The intrinsic factor (IF), a glycosylated protein released by stomach parietal cells, binds the free vitamin to create the IF vitamin B12 complex[5,38].
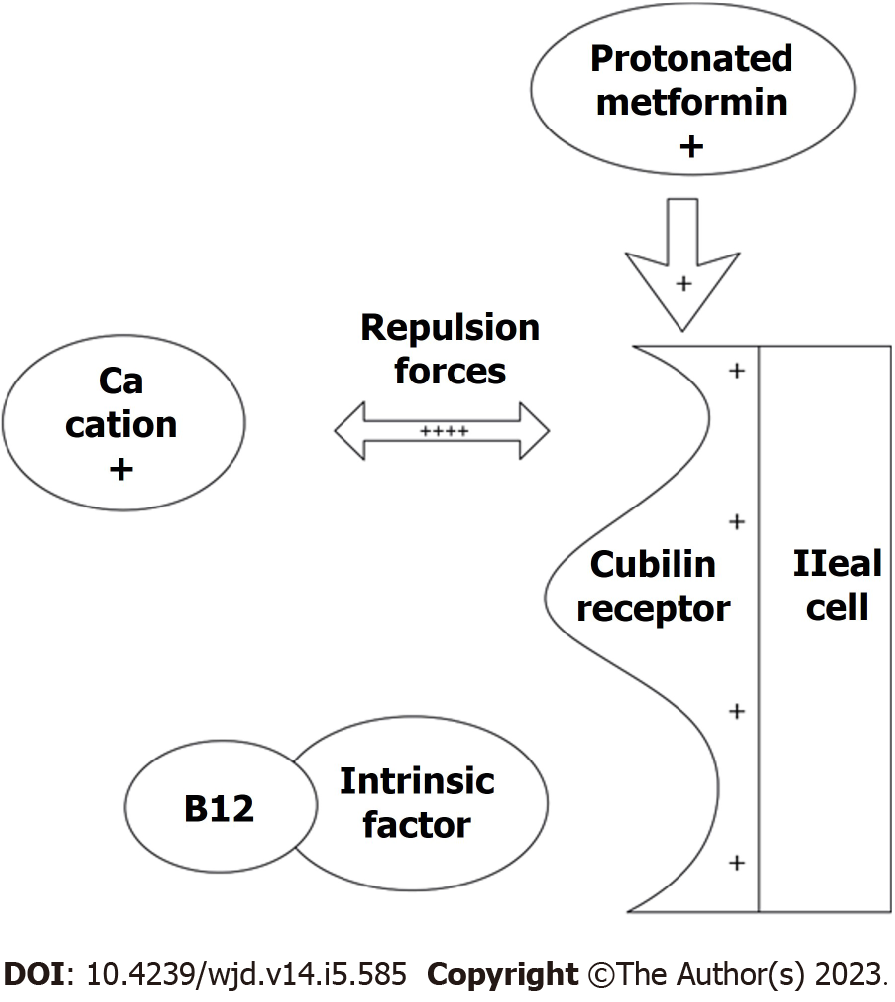
The IF-vitamin B12 complex passes via receptor-mediated endocytosis in the terminal ileum while avoiding proteolysis and acting as a carrier for the vitamin. The IF-vitamin B12 complex binds to the ileal cubilin receptor, a glycosylated protein expressed on the apical side of ileal enterocytes. Specific cubilin domains are engaged by the IF-vitamin B12 complex. And calcium cations are necessary for this interaction, where calcium can increase the complex’s functional affinity to the receptor[39].
The ileal enterocyte then endocytoses the IF-vitamin B12-cubilin receptor complex. The IF-vitamin B12 complex separates from cubilin after endocytosis. When the complex enters the lysosome, IF is broken down and vitamin B12 crosses the membrane into the cytoplasm[39]. The vitamin then circulates with transcobalamin-I (TC-I) or TC-II linked to it. 20%-30% of the total amount of circulating vitamin B12 is thought to be bound to the TC-II protein. Newly absorbed vitamins are bound by the protein and transported to the target tissues where they are absorbed via a receptor-mediated internalization process[5,39].
Metformin can reduce the absorption of vitamin B12 through a mechanism that has not been established clearly[40]. Until now, several theories describe how metformin prevents the absorption of vitamin B12. These include compromised enterohepatic B12 circulation, increased vitamin B12 hepatic storage, decreased IF production, and decreased intestinal motility with bacterial overgrowth[12,40]. The most accepted theory is that metformin antagonizes the calcium cation and prevents the calcium-dependent IF-vitamin B12 complex from binding to the ileal cubilin receptor and consequently will reduce the endocytosis process of vitamin B12[5,12].
It is proposed that metformin could give a positive charge to the membrane’s surface of cubilin receptor[41]. The positively charged receptor will push the divalent calcium cations by repulsion forces. This will lead to vitamin B12 malabsorption because the calcium-dependent binding of the IF-vitamin B12 complex to the ileal cubilin receptor is compromised[12]. Figure 1 shows how metformin can affect the absorption of vitamin B12.
As we mentioned before, many observational and experimental described the association between long-term metformin use and low vitamin B12 levels. The deficiency of vitamin B12 may lead to many clinical symptoms that may impact the quality of diabetic patients’ life. In this review we tried to summarize the most important complications of vitamin B12 deficiency in metformin-treated T2DM patients through the following.
Neuropathy is a primary complication of T2DM and a direct manifestation of vitamin B12 deficiency. Weakness, numbness, and pain are common symptoms of peripheral neuropathy, which develop when the peripheral nerves outside the brain and spinal cord are damaged. Many recent studies found that the long-term use of metformin could be a cause for increasing the prevalence of peripheral neuropathy among T2DM patients[13,31,42,43]. A recently published study showed a positive correlation between the period of metformin therapy and the severity of peripheral neuropathy[13].
The complications were not limited to peripheral neuropathy but also included autonomic cardiac neuropathy. In this context, Hansen et al[44] conducted a randomized, placebo-controlled trial that included 469 diabetic individuals who were using insulin and had an average duration of diabetes of 10 years. In this study, three cardiovascular reflex tests were used to evaluate the patients for cardiovascular autonomic neuropathy; after that, they were randomly assigned to either metformin or a placebo. The researchers observed that the vitamin B12 levels were steady with placebo after 18 months but dropped with metformin treatment. In addition, a significant reduction in orthostatic blood pressure in the metformin group indicated a worsening of cardiovascular autonomic neuropathy[44]. A recently published study reported that cardiac autonomic neuropathy is linked to cardiac events, cardiac arrhythmias, and sudden death. The study reported that cardiac autonomic neuropathy had been observed to be associated with a 3.16-fold [95% confidence interval (CI): 2.42-4.13, P = 0.0001] increase in cardiovascular disorders and a 3.17-fold increase (95%CI: 2.11-4.78, P = 0.0001) in mortality[45].
The decrease in the absorption of vitamin B12 due to metformin may affect the treated patients’ cognitive function since several studies connected the decline in cognitive functions and some depressive symptoms to low vitamin B12 levels[35]. A cohort study conducted by Porter et al[46] showed that metformin use was associated with decreased vitamin B12 and vitamin B6 levels along with an increased risk of cognitive dysfunction. Another two recent studies reported that metformin-treated patients suffering from vitamin B12 deficiency have lower cognitive function and a higher chance of developing depression[47,48].
As metformin can cause vitamin B12 deficiency, it may cause anemia. Vitamin B12 deficiency can cause a delay in the maturation of red blood cells (RBCs) and many changes in their shape, leading to megaloblastic anemia. Megaloblastic anemias are characterized by an imbalance between nuclear and cytoplasmic maturation and abnormal nuclear maturation in RBCs. Vitamin B12 deficiency and a lack of folates affect DNA synthesis, which slows nuclear replication and postpones all stages of development[49,50].
Although many studies support the positive correlation between metformin use and vitamin B12 deficiency, there is still uncertainty about whether metformin causes anemia and whether this is triggered by B12 deficiency or not in metformin-treated T2DM patients[51,52]. In this context, Donnelly et al[53] made various statistical analyses using data exported from two randomized clinical trials and one observational study. The findings of this study showed that metformin use could cause a decrease in hemoglobin levels, and it is correlated to the early risk of anemia in individuals with T2DM. Unfortunately, the other previously performed high-quality evidence clinical studies on low vitamin B12 levels related to metformin did not investigate the significance of metformin use on hematological values. However, many case report studies linked megaloblastic anemia to the long-term use of metformin in T2DM patients[14,40,54].
As we stated before, several studies including interventional studies, observational studies, and meta-analyses concluded that chronic use of metformin could be a cause of vitamin B12 deficiency, and many complications may accompany this. To avoid all these complications, vitamin B12 supplementation may be required[55]. In this context, a newly published systematic review including seven clinical trials showed that the application of vitamin B12 supplementation for metformin-treated T2DM patients will be valuable in preventing or treating vitamin B12 deficiency and neuropathy and should be considered during the T2DM management plan[32].
Similarly, a recently performed randomized, double-blind, placebo-controlled trial concluded that the treatment of metformin-treated patients with diabetic neuropathy with 1 mg of oral methylcobalamin for twelve months improved plasma B12 levels and improved all neurophysiological symptoms[56]. Since the typical amount of vitamin B12 stored in the liver is 2500 pg, it is believed that, in most cases, it will take at least five years of metformin use to deplete these reserves. However, other causes could increase the decrease of hepatic reserves, especially in the elderly due to the high prevalence of atrophic gastritis and proton pump inhibitor users. A recently published study reported that the monitoring of B12 levels might be important only for patients on long-term therapy of metformin (more than four years), especially when combined with proton pump inhibitors[57].
Metformin can cause vitamin B12 deficiency by reducing the absorption of the IF complex through the enteral cubilin receptor in the terminal ileum, which can either cause peripheral neuropathy, cardiac autonomic neuropathy, neuropsychiatric symptoms, or hematological disorders. The most severe side effect of metformin-induced vitamin B12 deficiency may be the development or acceleration of cardiac autonomic neuropathy, which is linked to an increase in cardiac arrhythmias, cardiac events, and mortality. Therefore, it is advised that people taking metformin undergo annual testing for vitamin B12 deficiency. In case of vitamin B12 deficiency, early replacement with intramuscular vitamin B12 to restore hepatic storage of vitamin B12 is recommended.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ji G, China; Liu D, China; Peng YF, China S-Editor: Wang JJ L-Editor: A P-Editor: Chen YX
| 1. | Harreiter J, Roden M. [Diabetes mellitus-Definition, classification, diagnosis, screening and prevention (Update 2019)]. Wien Klin Wochenschr. 2019;131:6-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 115] [Article Influence: 19.2] [Reference Citation Analysis (1)] |
| 2. | Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5345] [Cited by in RCA: 5935] [Article Influence: 989.2] [Reference Citation Analysis (8)] |
| 3. | Glovaci D, Fan W, Wong ND. Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Curr Cardiol Rep. 2019;21:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 402] [Article Influence: 67.0] [Reference Citation Analysis (1)] |
| 4. | Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020;16:377-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 825] [Cited by in RCA: 949] [Article Influence: 189.8] [Reference Citation Analysis (0)] |
| 5. | Ahmed MA. Metformin and Vitamin B12 Deficiency: Where Do We Stand? J Pharm Pharm Sci. 2016;19:382-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (2)] |
| 6. | Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes: A systematic review and meta-analysis. Diabetes Metab. 2016;42:316-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 113] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 7. | Nasri H, Rafieian-Kopaei M. Metformin: Current knowledge. J Res Med Sci. 2014;19:658-664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Herman R, Kravos NA, Jensterle M, Janež A, Dolžan V. Metformin and Insulin Resistance: A Review of the Underlying Mechanisms behind Changes in GLUT4-Mediated Glucose Transport. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 118] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 9. | Konopka AR, Esponda RR, Robinson MM, Johnson ML, Carter RE, Schiavon M, Cobelli C, Wondisford FE, Lanza IR, Nair KS. Hyperglucagonemia Mitigates the Effect of Metformin on Glucose Production in Prediabetes. Cell Rep. 2016;15:1394-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 10. | Alhaji JH. Vitamin B12 Deficiency in Patients with Diabetes on Metformin: Arab Countries. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (1)] |
| 11. | Almatrafi SB, Bakr ESH, Almatrafi AA, Altayeb MM. Prevalence of vitamin B12 deficiency and its association with metformin-treated type 2 diabetic patients: A cross sectional study. Hum Nutr Metab. 2022;27:2001138. [DOI] [Full Text] |
| 12. | Bell DSH. Metformin-induced vitamin B12 deficiency can cause or worsen distal symmetrical, autonomic and cardiac neuropathy in the patient with diabetes. Diabetes Obes Metab. 2022;24:1423-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 13. | Gupta K, Jain A, Rohatgi A. An observational study of vitamin b12 levels and peripheral neuropathy profile in patients of diabetes mellitus on metformin therapy. Diabetes Metab Syndr. 2018;12:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Albai O, Timar B, Paun DL, Sima A, Roman D, Timar R. Metformin Treatment: A Potential Cause of Megaloblastic Anemia in Patients with Type 2 Diabetes Mellitus. Diabetes Metab Syndr Obes. 2020;13:3873-3878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand. 2022;37:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 136] [Article Influence: 45.3] [Reference Citation Analysis (1)] |
| 16. | Syed FZ. Type 1 Diabetes Mellitus. Ann Intern Med. 2022;175:ITC33-ITC48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 119] [Article Influence: 39.7] [Reference Citation Analysis (0)] |
| 17. | Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. Lancet. 2022;400:1803-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 516] [Article Influence: 172.0] [Reference Citation Analysis (0)] |
| 18. | Paul S, Ali A, Katare R. Molecular complexities underlying the vascular complications of diabetes mellitus - A comprehensive review. J Diabetes Complications. 2020;34:107613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (1)] |
| 19. | Gottwald-Hostalek U, Gwilt M. Vascular complications in prediabetes and type 2 diabetes: a continuous process arising from a common pathology. Curr Med Res Opin. 2022;38:1841-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Achim A, Stanek A, Homorodean C, Spinu M, Onea HL, Lazăr L, Marc M, Ruzsa Z, Olinic DM. Approaches to Peripheral Artery Disease in Diabetes: Are There Any Differences? Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 21. | Stephens JW, Williams DM, Chudleigh R. Diabetes mellitus: what the neurologists need to know. Pract Neurol. 2022;22:532-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Li X, Lu L, Hou W, Huang T, Chen X, Qi J, Zhao Y, Zhu M. Epigenetics in the pathogenesis of diabetic nephropathy. Acta Biochim Biophys Sin (Shanghai). 2022;54:163-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 23. | Fung TH, Patel B, Wilmot EG, Amoaku WM. Diabetic retinopathy for the non-ophthalmologist. Clin Med (Lond). 2022;22:112-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 64] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 24. | Nellaiappan K, Preeti K, Khatri DK, Singh SB. Diabetic Complications: An Update on Pathobiology and Therapeutic Strategies. Curr Diabetes Rev. 2022;18:e030821192146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 25. | Triggle CR, Mohammed I, Bshesh K, Marei I, Ye K, Ding H, MacDonald R, Hollenberg MD, Hill MA. Metformin: Is it a drug for all reasons and diseases? Metabolism. 2022;133:155223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 150] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 26. | Seo-Mayer PW, Thulin G, Zhang L, Alves DS, Ardito T, Kashgarian M, Caplan MJ. Preactivation of AMPK by metformin may ameliorate the epithelial cell damage caused by renal ischemia. Am J Physiol Renal Physiol. 2011;301:F1346-F1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 27. | Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60:1577-1585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1320] [Cited by in RCA: 1452] [Article Influence: 181.5] [Reference Citation Analysis (0)] |
| 28. | Kawanami D, Takashi Y, Tanabe M. Significance of Metformin Use in Diabetic Kidney Disease. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 29. | Flory J, Lipska K. Metformin in 2019. JAMA. 2019;321:1926-1927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 323] [Article Influence: 53.8] [Reference Citation Analysis (1)] |
| 30. | DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism. 2016;65:20-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 384] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 31. | Niafar M, Hai F, Porhomayon J, Nader ND. The role of metformin on vitamin B12 deficiency: a meta-analysis review. Intern Emerg Med. 2015;10:93-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 32. | Pratama S, Lauren BC, Wisnu W. The efficacy of vitamin B12 supplementation for treating vitamin B12 deficiency and peripheral neuropathy in metformin-treated type 2 diabetes mellitus patients: A systematic review. Diabetes Metab Syndr. 2022;16:102634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 33. | Tomkin GH, Hadden DR, Weaver JA, Montgomery DA. Vitamin-B12 status of patients on long-term metformin therapy. Br Med J. 1971;2:685-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 131] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 34. | Liu Q, Li S, Quan H, Li J. Vitamin B12 status in metformin treated patients: systematic review. PLoS One. 2014;9:e100379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 35. | Gille D, Schmid A. Vitamin B12 in meat and dairy products. Nutr Rev. 2015;73:106-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 36. | Pavlov CS, Damulin IV, Shulpekova YO, Andreev EA. Neurological disorders in vitamin B12 deficiency. Ter Arkh. 2019;91:122-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 37. | Hannibal L, Jacobsen DW. Intracellular processing of vitamin B12 by MMACHC (CblC). Vitam Horm. 2022;119:275-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Guéant JL, Guéant-Rodriguez RM, Alpers DH. Vitamin B12 absorption and malabsorption. Vitam Horm. 2022;119:241-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 56] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 39. | Kozyraki R, Cases O. Vitamin B12 absorption: mammalian physiology and acquired and inherited disorders. Biochimie. 2013;95:1002-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 40. | Infante M, Leoni M, Caprio M, Fabbri A. Long-term metformin therapy and vitamin B12 deficiency: An association to bear in mind. World J Diabetes. 2021;12:916-931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 117] [Cited by in RCA: 102] [Article Influence: 25.5] [Reference Citation Analysis (13)] |
| 41. | Di Magno L, Di Pastena F, Bordone R, Coni S, Canettieri G. The Mechanism of Action of Biguanides: New Answers to a Complex Question. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 42. | Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ, Bray GA, Schade DS, Temprosa MG, White NH, Crandall JP; Diabetes Prevention Program Research Group. Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study. J Clin Endocrinol Metab. 2016;101:1754-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 303] [Article Influence: 33.7] [Reference Citation Analysis (1)] |
| 43. | Alvarez M, Sierra OR, Saavedra G, Moreno S. Vitamin B12 deficiency and diabetic neuropathy in patients taking metformin: a cross-sectional study. Endocr Connect. 2019;8:1324-1329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 44. | Hansen CS, Lundby-Christiansen L, Tarnow L, Gluud C, Hedetoft C, Thorsteinsson B, Hemmingsen B, Wiinberg N, Sneppen SB, Lund SS, Krarup T, Madsbad S, Almdal T, Carstensen B, Jørgensen ME; CIMT study group. Metformin may adversely affect orthostatic blood pressure recovery in patients with type 2 diabetes: substudy from the placebo-controlled Copenhagen Insulin and Metformin Therapy (CIMT) trial. Cardiovasc Diabetol. 2020;19:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 45. | Chowdhury M, Nevitt S, Eleftheriadou A, Kanagala P, Esa H, Cuthbertson DJ, Tahrani A, Alam U. Cardiac autonomic neuropathy and risk of cardiovascular disease and mortality in type 1 and type 2 diabetes: a meta-analysis. BMJ Open Diabetes Res Care. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 46. | Porter KM, Ward M, Hughes CF, O'Kane M, Hoey L, McCann A, Molloy AM, Cunningham C, Casey MC, Tracey F, Strain S, McCarroll K, Laird E, Gallagher AM, McNulty H. Hyperglycemia and Metformin Use are Associated with B Vitamin Deficiency and Cognitive Dysfunction in Older Adults. J Clin Endocrinol Metab. 2019;104:4837-4847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 47. | Biemans E, Hart HE, Rutten GE, Cuellar Renteria VG, Kooijman-Buiting AM, Beulens JW. Cobalamin status and its relation with depression, cognition and neuropathy in patients with type 2 diabetes mellitus using metformin. Acta Diabetol. 2015;52:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 48. | Moore EM, Mander AG, Ames D, Kotowicz MA, Carne RP, Brodaty H, Woodward M, Boundy K, Ellis KA, Bush AI, Faux NG, Martins R, Szoeke C, Rowe C, Watters DA; AIBL Investigators. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care. 2013;36:2981-2987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 293] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 49. | Torrez M, Chabot-Richards D, Babu D, Lockhart E, Foucar K. How I investigate acquired megaloblastic anemia. Int J Lab Hematol. 2022;44:236-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 50. | Obeagu EI, Babar Q, Obeagu GU. Megaloblastic Anaemia - A Review. Int J Curr Res Med Sci. 2021;7:17-24. [DOI] [Full Text] |
| 51. | Yang W, Cai X, Wu H, Ji L. Associations between metformin use and vitamin B12 levels, anemia, and neuropathy in patients with diabetes: a meta-analysis. J Diabetes. 2019;11:729-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 52. | Angelousi A, Larger E. Anaemia, a common but often unrecognized risk in diabetic patients: a review. Diabetes Metab. 2015;41:18-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 53. | Donnelly LA, Dennis JM, Coleman RL, Sattar N, Hattersley AT, Holman RR, Pearson ER. Risk of Anemia with Metformin Use in Type 2 Diabetes: A MASTERMIND Study. Diabetes Care. 2020;43:2493-2499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 54. | Callaghan TS, Hadden DR, Tomkin GH. Megaloblastic anaemia due to vitamin B12 malabsorption associated with long-term metformin treatment. Br Med J. 1980;280:1214-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 55. | Didangelos T, Karlafti E, Kotzakioulafi E, Margariti E, Giannoulaki P, Batanis G, Tesfaye S, Kantartzis K. Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 56. | Chappell L, Brown SA, Wensel TM. Evaluation of Vitamin B12 Monitoring in Patients on Concomitant Metformin and Proton Pump Inhibitors. Innov Pharm. 2020;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 57. | Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pract. 2012;97:359-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (1)] |