Published online Nov 15, 2023. doi: 10.4239/wjd.v14.i11.1710
Peer-review started: July 9, 2023
First decision: August 10, 2023
Revised: August 31, 2023
Accepted: October 16, 2023
Article in press: October 16, 2023
Published online: November 15, 2023
Processing time: 127 Days and 10.3 Hours
The correction and control of chronic hyperglycemia are the management goals of patients living with diabetes. Chronic hyperglycemia is the main factor inducing diabetes-related complications. However, in certain situations, the rapid and intense correction of chronic hyperglycemia can paradoxically favor the onset of microvascular complications.
In this case report, we describe the case of a 25-year-old woman living with type 1 diabetes since the age of 9 years. Her diabetes was chronic and unstable but without complications. During an unplanned pregnancy, her diabetes was intensely managed with the rapid correction of her hyperglycemia. However, over the following 2 years, she developed numerous degenerative microvascular complications: Charcot neuroarthropathy with multiple joint involvement, severe proliferative diabetic retinopathy, gastroparesis, bladder voiding disorders, and end-stage renal failure requiring hemodialysis.
In the literature to date, the occurrence of multiple microvascular complications following the rapid correction of chronic hyperglycemia has been rarely described in the same individual.
Core Tip: Our case describes a sad and rare development of multiple microvascular complications: Charcot neuroarthropathy with multiple joint involvement, severe proliferative diabetic retinopathy, gastroparesis, bladder voiding disorders, and end-stage renal failure. These devastating complications, which were probably due to the rapid correction of long-term hyperglycemia, severely impacted the quality of life of a young patient with type 1 diabetes.
- Citation: Huret P, Lopes P, Dardari R, Penfornis A, Thomas C, Dardari D. Rapid correction of hyperglycemia: A necessity but at what price? A brief report of a patient living with type 1 diabetes. World J Diabetes 2023; 14(11): 1710-1716
- URL: https://www.wjgnet.com/1948-9358/full/v14/i11/1710.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i11.1710
The vascular complications of diabetes are generally linked to chronic hyperglycemia[1]. This is the case for patients living with both type 1 and type 2 diabetes[2,3]. Nevertheless, the intense treatment of hyperglycemia can favor the onset of macrovascular complications such as stroke and myocardial infarction[4]. Large randomized clinical studies have assessed the impact of the so-called intense correction of hyperglycemia on macrovascular complications in the subjects living with diabetes[5,6], although few studies have evaluated the consequences of this rapid correction in terms of microvascular complications. Several descriptive studies have highlighted the potential deterioration of diabetic neuropathy and retinopathy in the case of the rapid correction of chronic hyperglycemia in people living with type 1 diabetes[7,8]. However, these studies were unable to provide a clear explanation of the relation between the deterioration of these microvascular complications and the rapid correction of chronic hyperglycemia[7,8]. The authors described a few cases of patients who developed several complications simultaneously.
The understanding of this mechanism remains at the theoretical stage, particularly following the degradation of diabetic neuropathy after the rapid onset of chronic hyperglycemia[7]. Theorical research has described the presence of neuropathy induced by the treatment of diabetes, with the presence of arteriovenous shunts and hypervascularity in the extremities and a still-unexplained disruption of inflammation factors such as certain interleukins[9]. The contribution of the rapid correction of hyperglycemia to the worsening of retinopathy may be more easily understood due to the specific action of insulin on the retinal endothelium with the appearance of so-called florid retinopathy[10,11]. When describing the degradation of complications after the rapid correction of chronic hyperglycemia, the literature usually focuses on a single complication[12,13].
Our case describes a sad and rare development of multiple microvascular complications: Charcot neuroarthropathy with multiple joint involvement, severe proliferative diabetic retinopathy, gastroparesis, bladder voiding disorders, and end-stage renal failure. These devastating complications, which were probably due to the rapid correction of long-term hyperglycemia, severely impacted the quality of life of a young patient with type 1 diabetes.
Our 25-year-old patient had been diagnosed with type 1 diabetes at the age 9 years. She had no other medical history. Her sister, who was 3 years older, also had type 1 diabetes. The management of her diabetes was exacerbated by chronic hyperglycemia, which had been present since adolescence with this major imbalance continuing after the age of 20 years.
Her medical records provide the mean values of glycated hemoglobin (HbA1c) dosed using the high-performance liquid chromatography method[14]: 11.0% at 16 years, 12.5% at 17 years, 11.6% at 18 years, 10.9% at 20 years, 11.3% at 22 years, 12.8% at 23 years, 13.3% at 24 years, and 12.0% at 25 years. It should be noted that the young woman did not consult for diabetes but was hospitalized in 2010 due to acute metabolic ketoacidosis. Despite her high HbA1c levels, she systematically refused educational and therapeutic assistance as well as an interstitial glucose monitoring system.
After a lengthy period without consulting a diabetologist, our 25-year-old patient sought an evaluation and treatment in November 2017 at the Centre Hospitalier Sud Francilien in France. At the time, she was 2 mo into an unplanned pregnancy. Before receiving therapeutic care, a complete assessment was performed, detecting an HbA1c level of 12%. She measured 167 cm and weighed 62 kg. The clinical examination revealed peripheral neuropathy with paresthesia in the lower limbs. Monofilament test was abnormal, results showed microalbuminuria (289 mg/L) with a normal glomerular filtration rate (80 mL/min/1.73 m²), which suggested incipient nephropathy. Therapeutic care was rapidly implemented with a subcutaneous insulin infusion pump, leading to the rapid reduction of HbA1c to 7.4% vs 12.0% (P < 0.01), equivalent to a 60% reduction over 8 mo of pregnancy The patient’s weight increased to 72.6 kg. Fundus examination performed at the start, middle, and end of the pregnancy did not reveal the presence of diabetic retinopathy. This pregnancy presented a new opportunity to manage this patient’s disease due to her strong motivation and desire to achieve an HbA1c level below 7%.
In addition to insulin, the only other medication was Ramipril 10 mg, which was prescribed in the post-partum period due to the presence of early nephropathy.
Between the first consultation in November 2017 and March 2022, the patient presented multiple microvascular complications related to diabetes. These complications were not detected during the initial pregnancy assessments but instead occurred following the rapid correction of chronic hyperglycemia.
The complications began during pregnancy with a rare presentation of Charcot neuroarthropathy with multiple joint involvement in November 2017. This led to a left knee prosthesis with a transtibial amputation of the left lower limb in March 2018[9,10].
In January 2019, following a spontaneous decline in her visual acuity, the patient presented for ophthalmological consultation, which revealed severe diabetic pre-proliferative retinopathy with a bilateral macular edema. The diagnosis was confirmed by retinal angiography and optical coherence tomography. Her HbA1c level was 6.8%. The patient underwent more than 20 pan-photocoagulation sessions and received intravitreal injections of anti-vascular endothelial growth factor therapy.
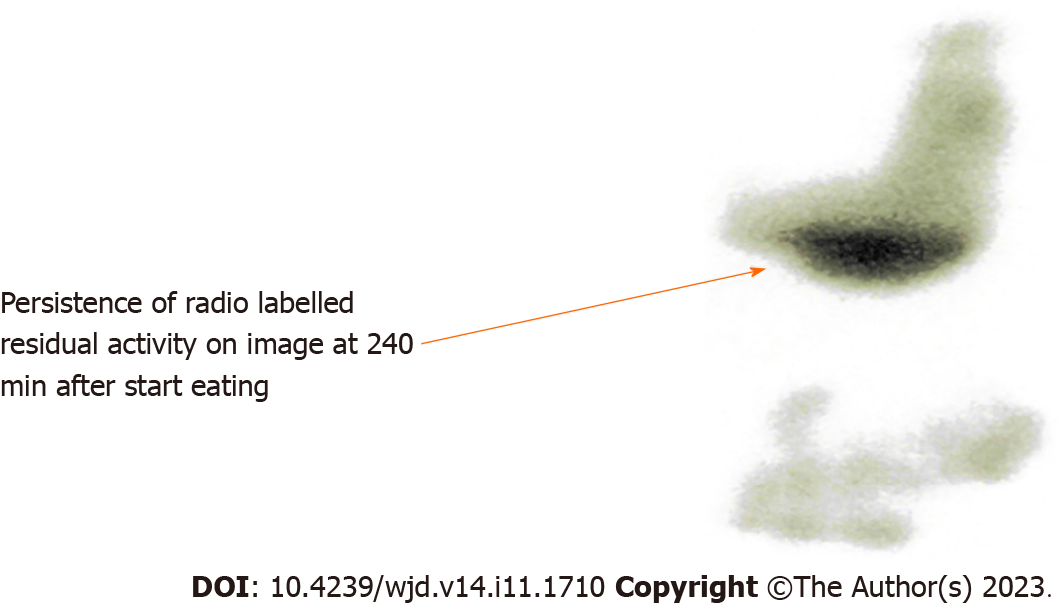
When this retinopathy was discovered in June 2019 about 1.5 years after achieving an HbA1c level below 7%, the patient also complained of abdominal discomfort with the presence of the following symptoms: nausea, vomiting, meteorism and abdominal pain, full feeling after a few mouthfuls (early satiety), heartburn or gastroesophageal reflux, and excessive weight loss. C reactive protein was 5 mg/L, and hepatic function was normal. The abdominopelvic ultrasound did not reveal any anomalies. Given the persistence of symptoms, an endoscopy of the upper gastrointestinal tract was performed, confirming the presence of non-erosive gastritis. Persistent symptoms were managed with a gastric emptying scintigraphy. During the scintigraphy, planar acquisitions were taken immediately after a meal comprised of 120 mg egg white labelled with 33 MBq of Technetium 99m-human albumin nanocolloids, two slices of sandwich bread, 30 g jam, and/or 250 mL fruit juice, and then after 15 min, 30 min, 45 min, 1 h, 2 h, and 4 h. The findings revealed an extremely slow progression of the radiolabeled meal in the stomach as well as substantial proximal and distal gastric retention due to decreased fundic tone. The findings pointed to diabetic gastroparesis (Figure 1). The patient was treated in the gastroenterology department, and prokinetic therapy was prescribed to improve gastric emptying and antiemetic agents.
Simultaneous with the onset of the digestive disorders, the patient described urinary symptoms with a decreased need to urinate along with less micturition, reduced flow rate, delayed urine flow with only a few drops, and the feeling of incomplete emptying, which sometimes led to overflow incontinence. The urodynamic assessment performed in response to the urinary symptoms confirmed the involvement of the bladder and highlighted potential complications. This assessment also revealed significant anomalies associated with diabetic cystopathy.
From June 2018, which was 1 year since the patient’s HbA1c level had been stabilized below 7%, the creatinine threshold showed a rapid upward trend with a marked increase in the microalbuminuria rate and a continuous decrease in the glomerular filtration rate (Figure 2).
Unfortunately, the management of the patient by nephrologists was unable to slow down the rapid development of end-stage renal failure over a period of 3 years from late 2017 to June 2020 when it was diagnosed, requiring treatment with thrice-weekly hemodialysis sessions. All diagnostic and therapeutic options were implemented following the initiation of care in nephrology. Other causes of this renal failure were eliminated via a kidney biopsy, with the histological results showing advanced nephropathy of metabolic origin. The early management of the ionic disorders by correcting the phosphate levels with calcium supplements and vitamin D aimed to reduce the excessive phosphate load and limit the protein intake.
Supplementary Figure 1 shows the timeline of each diabetes-related complication along with the time of diagnosis.
The patient currently lives with a left leg prosthesis and a left prosthetic knee. She uses a urinary catheter for her urinary incontinence and has tunnel vision due to her reduced visual field. She is on the national waiting list for a double kidney-pancreas transplant, and in the meantime, she undergoes peritoneal dialysis three times per week. Since December 2022, she has benefited from a hybrid closed-loop insulin delivery system (Medtronic 780 G).
Our 25-year-old patient had been diagnosed with type 1 diabetes at the age 9 years. Her sister, who was 3 years older, also had type 1 diabetes.
She measured 167 cm and weighed 62 kg. The clinical examination revealed peripheral neuropathy with paresthesia in the lower limbs. Monofilament test was abnormal.
Glycated hemoglobin (HbA1c) dosed using the high-performance liquid chromatography method[14]: 11.0% at 16 years, 12.5% at 17 years, 11.6% at 18 years, 10.9% at 20 years, 11.3% at 22 years, 12.8% at 23 years, 13.3% at 24 years, and 12.0% at 25 years.
Gastric scintigraphy, planar acquisitions were taken immediately after a meal comprised of 120 mg egg white labelled with 33 MBq of Technetium 99 m-human albumin nanocolloids, two slices of sandwich bread, 30 g jam, and/or 250 mL fruit juice, and then after 15 min, 30 min, 45 min, 1 h, 2 h, and 4 h. The findings revealed an extremely slow progression of the radiolabeled meal in the stomach as well as substantial proximal and distal gastric retention due to decreased fundic tone.
Type 1 diabetes with severe microvascular complications.
Hybrid closed-loop insulin delivery system (Medtronic 780 G).
After undergoing transtibial amputation of the lower limb and knee prosthesis surgery as part of therapy for Charcot’s neuroarthropathy, our patient received photocoagulation treatment for retinopathy and thrice-weekly hemodialysis for end-stage renal failure. The patient is currently registered on the French national waiting list for a double kidney-pancreas transplant.
The link between chronic glycemic imbalance and vascular complications is already well known and proven among people living with type 1 and type 2 diabetes[2,3]. The management of people living with diabetes should aim to prevent these complications by achieving long-term glycemic stability[11]. Nevertheless, the intense and rapid correction of glucose levels after a long period of hyperglycemia can produce or aggravate numerous macrovascular complications such as myocardial infarction or the risk of cardiovascular mortality[4]. Microvascular complications also seem prone to worsen with the rapid correction of chronic hyperglycemia[12]. Nevertheless, few studies have evaluated the impact of the rapid correction of HbA1c levels on microvascular complications among individuals living with diabetes. Gibbons et al[7] reported this impact with the well-known treatment-induced neuropathy in diabetes (TIND). The authors described a small number of cases in which preexisting minimal retinopathy deteriorated in patients who underwent the rapid correction of chronic hyperglycemia[7]. The degradation of renal function has previously been linked to the deterioration of retinopathy[15].
Our case report focuses on the rare presentation of numerous microvascular complications involving multiple joints and organs, probably induced by the rapid correction of HbA1c levels. Following the chronological order of the complications, the patient first presented acute Charcot neuroarthropathy that affected two joints[9]. The onset of acute Charcot neuroarthropathy can sometimes accompany the rapid correction of hyperglycemia, although it has been described in multiple sites in recent cohorts[16,17]. Regarding gastroparesis, very few descriptions associate this complication with the rapid correction of HbA1c levels. Data have also shown that the change is caused by the degree of HbA1c decrease rather than the type of therapy (insulin, oral hypoglycemic drugs, or diet control).
TIND is an acute neuropathy affecting the autonomic and small somatosensory nerve fibres that occurs subsequent to rapid improvements in glucose control. Gibbons et al[7] demonstrates that: (1) There is an unexpectedly high proportion of individuals with TIND in their tertiary referral diabetic clinic; (2) the risk of developing TIND is associated with the magnitude and rate of change in HbA1c; (3) the severity of neuropathic pain and autonomic dysfunction is correlated with the magnitude of change in HbA1c; (4) patients with type 1 diabetes and a history of eating disorders are at a high risk of developing TIND; and (5) TIND can occur following use of insulin or oral hypoglycemic agents[7]. Data from Gibbons et al[7] also provide indications for the prevention of TIND. As its incidence significantly increases when HbA1c decreases by 42% over 3 mo, this suggests that limiting treatment goals to an HbA1c reduction over 3 mo is a reasonable threshold. Patients with higher baseline HbA1c or a history of diabetic anorexia or weight loss may be at higher risk of TIND; special attention is therefore warranted in the case of intensive glycemic management in these patients[7].
Diabetes-related gastroparesis is a challenging complication of diabetes, which often results in intractable vomiting and recurrent hospitalizations. It is defined as delayed gastric emptying in the absence of mechanical obstruction. It is estimated that 30%-50% of patients with diabetes have delayed gastric emptying. Gastroparesis is most often diagnosed with type 1 diabetes and can occur as early as adolescence, although it can also occur in patients with type 2 diabetes, usually several years after diagnosis. The onset is insidious, with the disease course characterized by phases of exacerbation and remission[18]. In the literature, gastroparesis has been described during pregnancy and not 1-year post-partum as in the case of our patient[18]. The pathogenesis of diabetic gastroparesis is distinctly multifactorial. People living with diabetes often suffer from other physiological problems of the digestive tract that affect motor, absorptive, secretory, and sensorial systems. Gastropathy renders diabetic control very difficult, and poor diabetic control in turn worsens gastric emptying, thus making life difficult for people with gastropathy. It is vital that patients and their healthcare providers reach an agreement about a control goal that will allow patients to feel better and avoid further complications, while preventing severe hypoglycemia[18]. In the work of Gibbons, certain cases of gastroparesis were described along with TIDN[7].
Our case report also details the appearance of severe and debilitating diabetic retinopathy, which was not present before the rapid correction of HbA1c, as the three fundus examinations performed during pregnancy formally excluded the presence of retinopathy, even at the early stages. One potential explanation for this deterioration may be the intensity of insulin therapy, as the serum concentration probably increased following the correction of hyperglycemia, thus leading to a reduction in the availability of cellular energy substrates. A reduction in retinal vascular auto-regulation and an increase in growth factors trigger the neovascularization responsible for severe retinopathy[8]. Urinary retention leading to incontinence in our patient is a little-known mechanism linked to urinary disturbances in autonomic neuropathy[19]. Regarding the patient’s renal failure, she presented a very rapid decline in renal function, corresponding to an annual decrease in the glomerular filtration rate of more than 5 mL/min/1.73 m²[20]. The time to end-stage renal failure was only 3 years, which was much faster than described in the literature[21].
The association between the HbA1c variability score and the estimated glomerular filtration rate has been evaluated in people living with type 2 diabetes[22,23], although very few clinical trials have evaluated the same effect in patients living with type 1 diabetes.
One limitation of this case report is its retrospective nature, which may be an obstacle to the interpretation of the medical elements. Another limitation is the lack of data such as the presence or absence of glycemic variability, which prevented accurate HbA1c measurements. Unfortunately, the patient systematically refused to provide real-time glycemic data by either capillary blood glucose monitoring or continuous glucose measurements.
Our patient presented multiple rare conditions following the appearance of microvascular complications and their fast deterioration after the rapid correction of chronic hyperglycemia Our case description supports the use of personalized algorithms such as the hybrid closed-loop systems with automated insulin delivery to allow for more precise adjustments when high insulin doses are used in subjects living with chronic glycemic instability.
The association between the HbA1c variability score and the estimated glomerular filtration rate has been evaluated in people living with type 2 diabetes[24,25], although very few clinical trials have evaluated the same effect in patients living with type 1 diabetes. One limitation of this case report is its retrospective nature, which may be an obstacle to the interpretation of the medical elements. Another limitation is the lack of data such as the presence or absence of glycemic variability, which prevented accurate HbA1c measurements. Unfortunately, the patient systematically refused to provide real-time glycemic data by either capillary blood glucose monitoring or continuous glucose measurements.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: France
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li SY, China; Wu K, United States S-Editor: Chen YL L-Editor: A P-Editor: Yu HG
| 1. | Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of Diabetes 2017. J Diabetes Res. 2018;2018:3086167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 204] [Cited by in RCA: 311] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 2. | DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391:2449-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 969] [Article Influence: 138.4] [Reference Citation Analysis (0)] |
| 3. | Rouyard T, Kent S, Baskerville R, Leal J, Gray A. Perceptions of risks for diabetes-related complications in Type 2 diabetes populations: a systematic review. Diabet Med. 2017;34:467-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Rigalleau V, Larroumet A, Ducos C, Rigo M, Barbet-Massin MA, Majchrzak C, Mohammedi K, Baillet-Blanco L, Monlun M, Rami-Arab L, Foussard N. Cardiovascular events after a dramatic reduction of HbA1c in hospitalized subjects with type 2 diabetes and high long-term glucose exposure. J Diabetes Complications. 2022;36:108234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefèbvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Korányi L, Laakso M, Mokán M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J; PROactive Investigators. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366:1279-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3109] [Cited by in RCA: 2958] [Article Influence: 147.9] [Reference Citation Analysis (0)] |
| 6. | ADVANCE Collaborative Group; Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4759] [Cited by in RCA: 4892] [Article Influence: 287.8] [Reference Citation Analysis (0)] |
| 7. | Gibbons CH, Freeman R. Treatment-induced neuropathy of diabetes: an acute, iatrogenic complication of diabetes. Brain. 2015;138:43-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 146] [Article Influence: 13.3] [Reference Citation Analysis (2)] |
| 8. | Chantelau E, Meyer-Schwickerath R. Reversion of 'early worsening' of diabetic retinopathy by deliberate restoration of poor metabolic control. Ophthalmologica. 2003;217:373-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Gibbons CH. Treatment induced neuropathy of diabetes. Auton Neurosci. 2020;226:102668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Lattanzio R, Brancato R, Bandello FM, Azzolini C, Malegori A, Maestranzi G. Florid diabetic retinopathy (FDR): a long-term follow-up study. Graefes Arch Clin Exp Ophthalmol. 2001;239:182-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Henricsson M, Berntorp K, Fernlund P, Sundkvist G. Progression of retinopathy in insulin-treated type 2 diabetic patients. Diabetes Care. 2002;25:381-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Chantelau E. Effect of a growth hormone receptor antagonist on proliferative diabetic retinopathy. Ophthalmology. 2002;109:2187; author reply 2187-2187; author reply 2188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Agardh E. A case of progression of diabetic retinopathy during pregnancy. Acta Ophthalmol Scand. 2002;80:524-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Blum F. High performance liquid chromatography. Br J Hosp Med (Lond). 2014;75:C18-C21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Dardari D, Penfornis A, Amadou C, Phan F, Bourron O, Davaine JM, Foufelle F, Jaisser F, Laborne FX, Hartemann A. Multifocal (tarsus and knee) activation of neuroarthropathy following rapid glycaemic correction. J Diabetes Complications. 2019;33:107438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Dardari D, Penfornis A. Fracture of the Bone Inducing Its Necrosis as the End Point in the Evolution of Untreated Neuroarthropathy. Medicina (Kaunas). 2021;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 17. | Elafros MA, Callaghan BC, Skolarus LE, Vileikyte L, Lawrenson JG, Feldman EL. Patient and health care provider knowledge of diabetes and diabetic microvascular complications: a comprehensive literature review. Rev Endocr Metab Disord. 2023;24:221-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Dardari D, Schuldiner S, Julien CA, Ha Van G, M'Bemba J, Bourgeon M, Sultan A, Lepeut M, Grandperret-Vauthier S, Baudoux F, François M, Clavel S, Martini J, Vouillarmet J, Michon P, Moret M, Monnier A, Chingan-Martino V, Rigalleau V, Dumont I, Kessler L, Stifii I, Bouillet B, Bonnin P, Lemoine A, Da Costa Correia E, Faraill MMB, Muller M, Cazaubiel M, Zemmache MZ, Hartemann A. Trends in the relation between hyperglycemia correction and active Charcot neuroarthropathy: results from the EPICHAR study. BMJ Open Diabetes Res Care. 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 19. | Dardari D, Van GH, M'Bemba J, Laborne FX, Bourron O, Davaine JM, Phan F, Foufelle F, Jaisser F, Penfornis A, Hartemann A. Rapid glycemic regulation in poorly controlled patients living with diabetes, a new associated factor in the pathophysiology of Charcot's acute neuroarthropathy. PLoS One. 2020;15:e0233168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Fuglsang J, Ovesen PG. Pregnancy and delivery in a woman with type 1 diabetes, gastroparesis, and a gastric neurostimulator. Diabetes Care. 2015;38:e75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Palleschi G, Pastore AL, Maggioni C, Fuschi A, Pacini L, Petrozza V, Carbone A. Overactive bladder in diabetes mellitus patients: a questionnaire-based observational investigation. World J Urol. 2014;32:1021-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Farrington K, Covic A, Nistor I, Aucella F, Clyne N, De Vos L, Findlay A, Fouque D, Grodzicki T, Iyasere O, Jager KJ, Joosten H, Macias JF, Mooney A, Nagler E, Nitsch D, Taal M, Tattersall J, Stryckers M, van Asselt D, Van den Noortgate N, van der Veer S, van Biesen W. Clinical Practice Guideline on management of older patients with chronic kidney disease stage 3b or higher (eGFR<45 mL/min/1.73 m2): a summary document from the European Renal Best Practice Group. Nephrol Dial Transplant. 2017;32:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 23. | Nacak H, Bolignano D, Van Diepen M, Dekker F, Van Biesen W. Timing of start of dialysis in diabetes mellitus patients: a systematic literature review. Nephrol Dial Transplant. 2016;31:306-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Zhou Y, Huang H, Yan X, Hapca S, Bell S, Qu F, Liu L, Chen X, Zhang S, Shi Q, Zeng X, Wang M, Li N, Du H, Meng W, Su B, Tian H, Li S; On Behalf Of The WECODe Study Group. Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 25. | Qu F, Shi Q, Wang Y, Shen Y, Zhou K, Pearson ER, Li S. Visit-to-visit glycated hemoglobin A1c variability in adults with type 2 diabetes: a systematic review and meta-analysis. Chin Med J (Engl). 2022;135:2294-2300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |