Published online Nov 15, 2023. doi: 10.4239/wjd.v14.i11.1621
Peer-review started: July 12, 2023
First decision: August 10, 2023
Revised: August 26, 2023
Accepted: September 27, 2023
Article in press: September 27, 2023
Published online: November 15, 2023
Processing time: 124 Days and 18.6 Hours
Diabetes mellitus (DM) and obesity have become two of the most prevalent and challenging diseases worldwide, with increasing incidence and serious complications. Recent studies have shown that noncoding RNA (ncRNA) and epigenetic regulation play crucial roles in the pathogenesis of DM complicated by obesity. Identification of the involvement of ncRNA and epigenetic regulation in the pathogenesis of diabetes with obesity has opened new avenues of investigation. Targeting these mechanisms with small molecules or RNA-based therapies may provide a more precise and effective approach to diabetes treatment than traditional therapies. In this review, we discuss the molecular mechanisms of ncRNA and epigenetic regulation and their potential therapeutic targets, and the research prospects for DM complicated with obesity.
Core Tip: Non-coding RNA (ncRNA) and epigenetic regulation play crucial roles in the pathogenesis of diabetes mellitus complicated by obesity. Identification of the involvement of ncRNA and epigenetic regulation in the pathogenesis of diabetes with obesity has opened new avenues. Targeting these mechanisms with small molecules or RNA-based therapies may provide a more precise and effective approach to diabetes treatment than traditional therapies.
- Citation: Guo YC, Cao HD, Lian XF, Wu PX, Zhang F, Zhang H, Lu DH. Molecular mechanisms of noncoding RNA and epigenetic regulation in obesity with consequent diabetes mellitus development. World J Diabetes 2023; 14(11): 1621-1631
- URL: https://www.wjgnet.com/1948-9358/full/v14/i11/1621.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i11.1621
The combination of diabetes mellitus (DM) and obesity has become a global health concern due to the high prevalence and serious consequences of these conditions. The pathogenesis of DM combined with obesity is complex and involves multiple mechanisms, including insulin resistance (IR), chronic inflammation, and adipokine dysregulation[1,2].
IR is a key factor in the development of both obesity and type 2 DM (T2DM)[3,4]. Adipose tissue, particularly visceral adipose tissue, produces a range of hormones, cytokines, and chemokines, collectively known as adipokines. In obesity, adipose tissue expands and produces increased amounts of proinflammatory adipokines, such as leptin, as well as decreased amounts of anti-inflammatory adipokines, such as adiponectin[5]. This leads to chronic inflammation, which exacerbates IR. Obesity and diabetes are associated with alterations in the gut microbiome, which can contribute to the pathogenesis of both conditions[6,7]. The gut microbiota of obese and diabetic individuals is distinct from that of healthy individuals, with reduced microbial diversity and altered microbial composition.
While the exact mechanisms underlying the development of DM complicated with obesity are still not fully understood, emerging evidence suggests that epigenetic modifications and noncoding RNA (ncRNA) play a critical role in its pathogenesis[8]. Epigenetic regulation refers to the modification of gene expression without changes to the underlying DNA sequence[9]. These modified activities can have a significant impact on gene expression and cellular function. Additionally, several genes are linked to an increased risk of developing these conditions, including genes involved in adipogenesis, lipid metabolism, and insulin signaling. Compounded obesity in DM is a multifactorial disorder that involves complicated interplay among genetic, environmental and lifestyle factors. It is vital to establish effective strategies for the prevention and treatment of these disorders by understanding these mechanisms.
ncRNAs, particularly microRNA (miRNA) and long noncoding RNA (lncRNA), have been shown to play critical roles in the development and progression of DM. Dysregulation of miRNA expression can lead to impaired glucose metabolism and IR[10]. For example, miRNA-29 regulates insulin signaling by targeting the insulin receptor substrate-1 (IRS-1) gene[11]. In obese mice, miRNA-29 expression is decreased, leading to increased IRS-1 expression and improved insulin sensitivity[11]. Similarly, miRNA-223 has been shown to regulate glucose uptake by targeting GLUT4, a glucose transporter protein. lncRNA has also been implicated in the pathogenesis of DM[12]. In addition, lncRNA MEG3 controls insulin secretion by modulating gene expression involved in insulin synthesis and secretion[13]. lncRNA taurine-upregulated gene 1 regulates the proliferation and differentiation of pancreatic beta cells, which are responsible for insulin production[14].
DNA methylation can alter gene expression patterns. The promoter region of the insulin gene is hypermethylated in patients with T2DM, leading to decreased insulin production[15]. Similarly, the promoter region of the adiponectin gene is hypomethylated in obese individuals, leading to increased adiponectin expression and improved insulin sensitivity[16]. The augmentation of gene expression is linked to histone acetylation, whereas histone methylation may either stimulate or hinder gene expression, contingent on the location and extent of methylation[17].
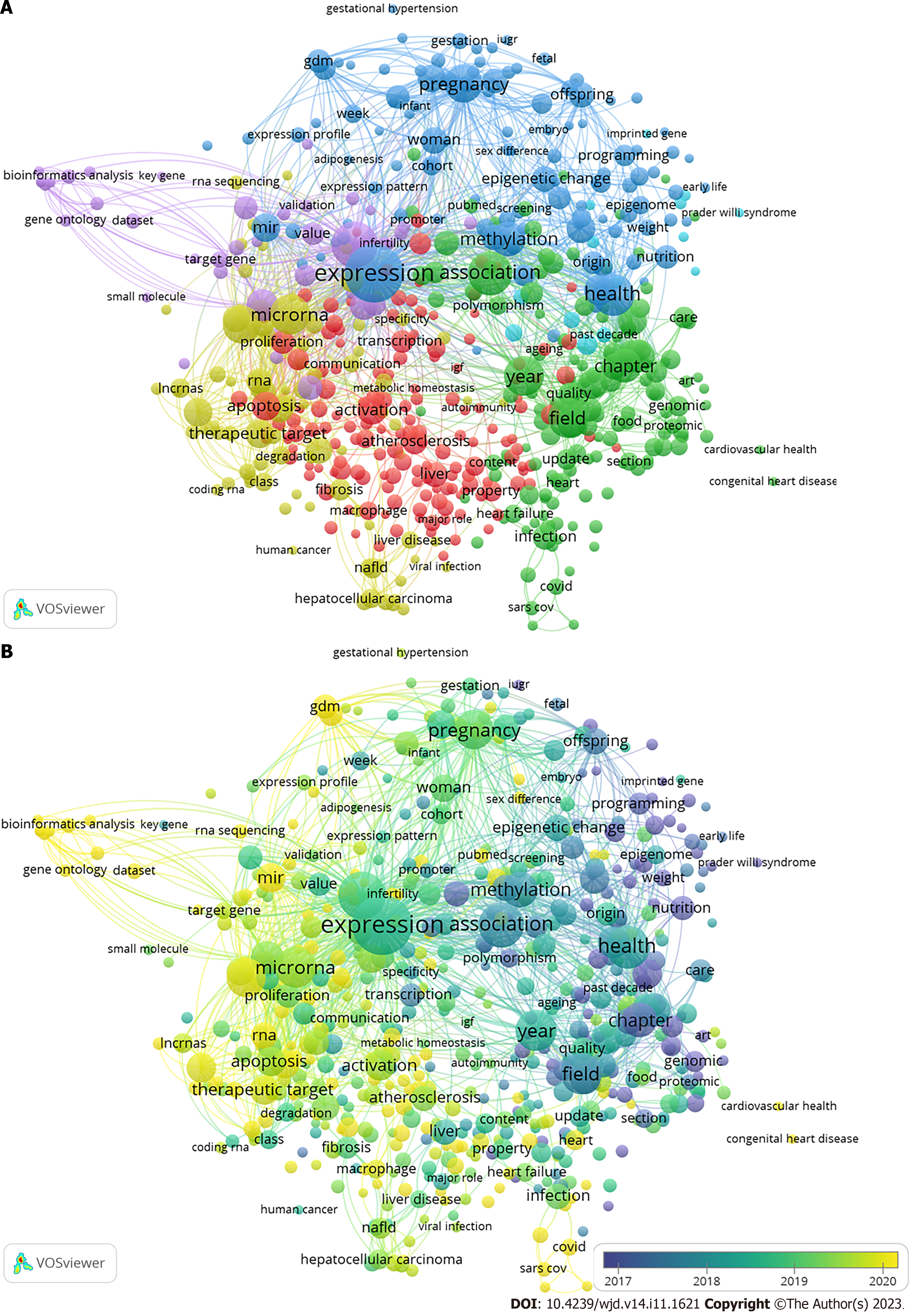
Emerging evidence suggests that epigenetic modifications and ncRNA play a critical role in the development and progression of DM complicated with obesity (Figure 1). Dysregulation of miRNA and lncRNA expression, as well as altered DNA methylation and histone modifications, can lead to impaired glucose metabolism and IR[18]. Although much is still unknown about the mechanisms underlying these epigenetic changes, identification of these modifications as potential therapeutic targets offers new hope for the prevention and treatment of DM. Future research should elucidate the role of epigenetic regulation and ncRNA in diabetes pathogenesis and develop effective therapies targeting these pathways. The aim of this review is to explore the molecular mechanisms of ncRNAs and epigenetic regulation in the pathogenesis of DM complicated by obesity. We intend to discuss the potential therapeutic targets associated with these mechanisms and highlight the research prospects for DM complicated with obesity.
lncRNAs in obesity and DM: The utilization of cutting-edge bioinformatic techniques has facilitated the identification of lncRNAs associated with obesity and adipocyte differentiation[19]. Investigations of gain-of-function and loss-of-function have both strongly pointed to the pivotal participation of lncRNAs in adipogenesis. To date, various lncRNAs have been examined in a range of models and they are potent modulators of diverse genetic pathways linked to white adipose tissue (WAT) compartmentalization and activity[20].
The first adipogenesis-related lncRNA was a steroid receptor RNA activator (SRA), which acts as a coactivator of peroxisome proliferator-activated receptor (PPAR)γ[21]. Among the lncRNAs involved in adipogenesis, ASMER-1 and ASMER-2 are upregulated in subcutaneous adipose tissue (ScAT) and are linked to adipocyte-specific metabolism and IR[20]. Several lncRNAs have roles in adipogenesis (the formation of fat cells), lipolysis (the breakdown of fat), and adiponectin secretion in human adipocytes (fat cells). ADNCR is an endogenous competitive RNA for miR-204, and overexpression of SIRT-1 inhibits adipocyte differentiation and impairs the PPARγ pathway in vitro. Finally, HOTAIR is implicated in preadipocyte differentiation[20,22-26].
Brown adipose tissue (BAT) is a specialized form of adipose tissue that is mainly responsible for thermogenesis and energy expenditure. It is characterized by the presence of uncoupling protein 1 (UCP1), leading to increased energy expenditure and weight loss[27,28]. Recent studies have identified several lncRNAs that are involved in BAT regulation, including brown fat lncRNA1 (Blnc1) and H19[25,29]. Research has indicated that Blnc1 plays a role in regulating thermogenic genes, resulting in an increase in the expression of UCP1 and mitochondrial genes[30]. Conversely, H19 has been found to have an inverse correlation with body mass index (BMI) and a positive correlation with browning markers. H19 is involved in modulating adipogenesis, oxidative metabolism, and mitochondrial respiration in BAT. Thus, the manipulation of lncRNA expression shows promise as a therapeutic approach for metabolic diseases. This could involve enhancing BAT activity or inducing browning in WAT[31]. Various studies have suggested the potential of different lncRNAs as biomarkers for diagnosing and managing obesity. For example, Sun et al[32] found reduced expression of three lncRNAs in obese but not in lean subjects. The expression of these lncRNAs was inversely correlated with waist-to-hip ratio, BMI and fasting plasma insulin levels. lncRNA-p19461 was upregulated following weight loss due to a 12-wk diet, suggesting that bariatric interventions could manage expressed lncRNA profiles. Alterations in the expression levels of lncRNAs were found following bariatric surgery in animals, particularly those engaged in digestive, absorptive and inflammatory pathways.
While the potential of lncRNAs as therapeutic targets for obesity management is promising, several challenges need to be addressed before their clinical application. One major challenge is the lack of understanding of the precise molecular mechanisms underlying the regulation of lncRNA expression in different tissues and under different physiological conditions[33]. The delivery of lncRNA-based therapeutics to specific tissues remains a major hurdle due to their large size and potential off-target effects[33,34]. Therefore, additional investigation is required to uncover the molecular pathways involved in the regulation of lncRNA and to develop delivery methods that can specifically target tissues while minimizing off-target effects.
lncRNAs in DM: In animal models and human islets, dysregulation of lncRNAs is engaged in various stages of insulin secretion and is implicated in the progression of IR[35,36] (Table 1). In addition, the genes that encode them are located near islet-specific chromatin domains that contain genes involved in β-cell function modulation[37]. The specific functions and action mechanisms of these lncRNAs are still not fully understood[36].
| Factors related to the development of IR | Names of lncRNAs | Targeted nuclear proteins |
| Lipogenic activity | H19, MALAT1, MEG3, and MIAT↑ | SREBP-1c, PPARγ, and FoxO1 |
| Gluconeogenesis | MEG3 and H19↑ | CRTC2/CREB, FoxO1, HNF4A and ATF4 |
| Inflammation and oxidative stress | MALAT1 and H19↑ | EZH2 and PRC2 |
| Cellular dysfunction | MEG3, MALAT1 and MIAT↑ | N/A |
In T2DM, metabolic syndrome and low-level high-density lipoprotein, a decline in MALAT1 expression was found, along with overexpressed H19 in patients with worse glycemic control than those with glycated hemoglobin concentration < 7%[38]. Additionally, MALAT1 is related to angiogenesis in diabetic eyes and kidneys. A few dysregulated lncRNAs in diabetic subjects are positively correlated with transcriptional markers of IR, impaired glucose control, and aging. These lncRNAs were apparently relevant to DM, even after correction[39]. Newly diagnosed diabetic patients exhibited similar results, indicating that dysregulated lncRNAs control IR and inflammation, ultimately resulting in disrupted glucose homeostasis[40].
The role of lncRNAs in both microvascular and macrovascular complications of DM has been investigated. A widely studied lncRNA associated with diabetic complications is ANRIL, which is considered a potential biomarker[41,42]. Another is MALAT1 in association with elevated production of reactive oxygen species and proinflammatory cytokines, contributing to endothelial lesions in the microvasculature[35,41].
Dysregulation of specific genes has been identified in renal biopsies affected by diabetic nephropathy. Additionally, a study of diabetic patients with chronic complications found downregulation of CASC2 in the serum and renal tissue of DM patients with chronic kidney disease when compared to healthy controls[36,43]. Both MIAT and MALAT1 were found to be over-regulated in renal specimens from diabetic subjects and in animal models[36]. The effect of lncRNAs in diabetic patients with peripheral neuropathy has also been investigated. Specifically, NONRATT021972 was shown to be increased in T2DM subjects with exacerbated symptoms connected to neuralgia, together with an increase in tumor necrosis factor (TNF)-α levels. Furthermore, siRNA-NONRATT021972 alleviated neuropathic pain by decreasing TNF-α in rats, resulting in decreased blood glucose and inflammation, which paved the way for potential therapies of neuropathic pain[44]. MALAT1 is over-expressed in gastrointestinal spasms and in T2DM sufferers with signs related to gastric spasms, and its impact is likely associated with smooth muscle cells.
Function of miRNAs in DM with obesity: miRNAs prevent the translation of mRNA into protein, leading to mRNA degradation or translational repression. miRNAs have been shown to regulate various cellular processes. Dysregulated miRNA has been implicated in metabolic disorders, such as in obesity (Table 2).
| Tissue or organs | Names of miRNAs | Targeted genes |
| Adipocytic tissue | miR-155, miR-27a, and miR-34a | SOCS1, PPAR |
| Liver | miR-99b and miR-155 | FGF21, PPAR |
| Muscle | miR-27a, miR-155, and miR-130b | PPAR, PGC1α |
| Pancreas | miR-132 and miR-92a | BTG2, PTBP1 |
| Cardiovascular system | miR-29a, miR-410-5p, and miR-194 | SMAD7 |
The pathogenesis of metabolic diseases has been linked to the expression of various miRNAs. Kunej et al[45] found that 221 of the 1736 Loci associated with obesity coincided with miRNAs. It has been reported that miRNAs can modulate pathways that control adipogenesis[46,47], which is impaired in obesity. Consequently, miRNA dysregulation could be involved in metabolic processes that contribute to obesity[48,49].
miRNA-375: The islet-specific miRNA-375 is expressed at high levels in pancreatic islets and regulates insulin secretion by modulating gene expression. The impact of miRNA-375 on glucose-stimulated insulin secretion (GSIS) and insulin gene transcription was investigated by Poy et al[50], who found that its overexpression suppressed GSIS and reduced insulin gene transcription, whereas its downregulation resulted in increased insulin secretion. This study confirmed the crucial role of miRNA-375 in the development of T2DM, as demonstrated by its higher expression in the pancreas of T2DM patients compared to healthy individuals. Dysregulation of miRNA-375 was observed 5 years prior to the start of T2DM and in prediabetes, indicating its potential use in the prediction and prevention of high-risk populations[51].
miRNA-130b: In prepubertal obesity, some miRNAs may become deregulated, as evidenced by a study which showed that the expression of miRNA-130b in plasma was upregulated and directly correlated with BMI and other indicators of obesity in children.
miRNA-200 family: The miRNA-200 family can contribute to protection against beta-cell apoptosis and dedifferentiation in vitro[52]. miRNA-200c is one of the most highly expressed miRNAs in beta cells, and partially protects against oxidative stress-induced beta-cell apoptosis, suggesting that the miRNA-200 family is essential in diabetes pathophysiology[53].
miRNA-7: Human islets are enriched in another miRNA named miRNA-7, which adversely modulates GSIS by restricting the expression of genes participating in the integration of insulin granules within the plasma membrane and the SNARE proteins[54]. The levels of hsa-miRNA-7-1-3p were reduced in pancreatic islets of individuals with T2DM compared to nondiabetic donors. The expression levels of hsa-miRNA-7-3-5p were increased in T2DM pancreatic islets[55].
miRNA-184: miRNA-184 is one of the miRNAs predominantly expressed in beta cells of pancreatic islets, regulating insulin secretion and beta-cell proliferation during IR[56]. Knockout of miRNA-184 in beta cells has been shown to increase their proliferation, resulting in improved insulin secretion following glucose stimulation. Blocking miRNA-184 in rat and human islets has been demonstrated to protect beta cells from apoptosis induced by prolonged exposure to proinflammatory cytokines and/or fatty acids.
Role of circular RNAs: Adipose tissue is a complex and metabolically active organ, playing an essential role in energy storage and homeostasis. Adipocytes are the primary cell type in adipose tissue, and their differentiation and function are tightly regulated by multiple molecular mechanisms. In recent years, the role of circular RNAs (circRNAs) in adipose tissue has gained significant attention.
circRNA expression in carboxy-terminal region, prediabetic and T2DM patients showed 411 downregulated and 78 upregulated circRNAs[57]. Notably, 220 circRNAs demonstrated differential expression, including 107 upregulated and 113 downregulated circRNAs[58]. Of particular interest were the ci-INS and ci-Ins2 Lariats, derived from human INS and mouse Ins2, respectively in beta cells[59].
Genetic variation is a crucial factor in the regulation of DNA methylation[60]. As methylated DNA predominantly arises on cytosine nucleotides after a guanine, it is evident additions or deletions of variants of cytosine-guanine dinucleotides(CG dinucleotides) affect the likelihood of methylated DNA at the loci[61]. Remarkably, roughly one-fourth of single nucleotide polymorphisms (SNPs) add or delete CpG site[62].
The presence of an SNP in NDUFB6 Led to the emergence of a CpG site that in turn affected DNA methylation and gene expression in human skeletal muscle, particularly age-related gene expression[63]. Although genetic variations can directly impact DNA methylation, it remains unclear whether they can affect methylation in more remote sites and, if so, what the underlying mechanism would be. The extent to which this phenomenon is widespread throughout the genome and its potential contribution to clinical phenotypes remain uncertain. Another study identified that nearly half of the genetic variations associated with diabetes introduce or remove a CpG site[64].
In 2014, a study extended previous research and provided a whole-genome description of genetic and epigenetically variations in human pancreatic islets[63]. Numerous cis- and trans-SNP–CpG pairs were determined, even though the machinery of the latter is still unclear[65]. Additionally, causal inference test established a catalytic interaction between SNPs, DNA methylation and genetic expression of annotated HLA regions highly correlated with type 1 DM[66]. More than 100000 DNA metylation quantitative trait loci (mQTLs) were identified by GWASs, which were linked to adipose-tissue gene expression, BMI, and insulin levels[67,68].
ncRNAs are involved in the development of both diabetes and obesity and may be potential early diagnostic markers for these conditions. miRNAs are small ncRNAs that play important roles in post-transcriptional gene regulation. These miRNAs are dysregulated in both DM and obesity and may serve as potential early diagnostic markers for these conditions[69]. For example, miRNA-126 has been shown to be downregulated in obese individuals and may serve as a potential early diagnostic marker in obesity[70]. Similarly, miRNA-375 has been shown to be upregulated in individuals with T2DM and may serve as a potential early diagnostic marker for this condition[71].
lncRNAs are longer ncRNAs that also play important roles in gene regulation, suggesting that lncRNAs are involved in the development of both diabetes and obesity and may serve as potential early diagnostic markers[19]. The lncRNAs HOTAIR and H19 have been shown to be upregulated in individuals with T2DM and may be early diagnostic markers[72,73].
circRNAs are a class of ncRNAs that form covalently closed circular RNA molecules, which have recently been observed in the dysregulation in both DM and obesity and may be early diagnostic markers[74]. For example, circRNA-000911 has been shown to be downregulated in individuals with T2DM, and may serve as a potential early diagnostic marker[75]. Similarly, serum and exosome circRNA-0000907 and circRNA-0057362 have been shown to be upregulated in patients with diabetic foot ulcer (DFU), indicating that they may have a potential role as early diagnostic markers for DFU[11].
ncRNAs have emerged as potential early diagnostic markers for both DM and obesity. Early diagnosis and management of DM and obesity are crucial to prevent complications and improve outcomes. Therefore, the identification of novel early diagnostic markers for these conditions is of utmost importance. ncRNAs may serve as valuable tools in this regard and may help improve patient outcomes. Therefore, further research is needed to validate the potential of ncRNAs in early diagnosis.
miRNAs are one of the best-studied classes of ncRNAs, and they have been implicated in the regulation of glucose homeostasis and insulin sensitivity. It was shown that miRNA-29a regulates insulin signaling by targeting IRS1 in adipocytes[76]. Additionally, miRNA-103 and miRNA-107 have been shown to promote IR by targeting the insulin receptor and GLUT4, respectively[77]. Another lncRNA, NEAT1, has been shown to regulate the expression of genes involved in the inhibition of high glucose-induced diabetic retinopathy[78]. Furthermore, S961-treated mouse sera reproduced beta-cell replication in pancreatic islets in an E2F1-dependent way, indicating that IR-induced adipocyte proliferation signaling activates E2F1 and is a potential target for promoting beta-cell compensation[79].
Epigenetic regulation has also emerged as an important contributor to the pathogenesis of DM with obesity. DNA methylation regulates motifs involved in glucose homeostasis and insulin signaling[80]. Histone modifications regulate the expression of key genes in the insulin signaling pathway[81].
In addition, lncRNAs are newly emerging and promising biomarkers, so we summarize the shared lncRNAs in both obesity and DM in order to provide further information (Table 3).
| lncRNA | Description | Expression in obesity | Expression in DM |
| SRA | Steroid receptor RNA activator | High | Low in patients with type II diabetic cardiovascular disease[74] |
| ASMER-1 | Adipocyte-associated metabolic related lncRNA 1 | High in ScAT | High expression related to IR[20] |
| ASMER-2 | Adipocyte-associated metabolic related lncRNA 2 | High in ScAT | High expression related to IR[20] |
| ADNCR | Adipocyte differentiation-associated lncRNA | Low | Low[23] |
| HOTAIR | HOX antisense intergenic RNA | High | High[71] |
| Blnc1 | Brown fat lncRNA 1 | High in high-fat-diet-fed mice[28] | High in the blood of patients with diabetic nephropathy[82] |
| H19 | LncRNA H19 | Low in obesity-associated inflammatory conditions[83] | Low[84] |
| MALAT1 | Metastasis-associated lung adenocarcinoma transcript 1 | High[85] | High expression in PBMCs from type 2 diabetes patients[39] |
Identification of the pathogenesis of DM with obesity has opened new avenues. Targeting these mechanisms with small molecules or RNA-based therapies may provide a more precise and effective approach to DM treatment than traditional therapies. For example, miRNA-based therapies have already been tested in preclinical models of DM, with promising results.
The pathogenesis of DM complicated with obesity involves complex molecular mechanisms, including ncRNA and epigenetic regulation. Understanding the roles of ncRNA and epigenetic regulation in the pathogenesis of DM complicated with obesity provides new insights into the development of novel therapeutic targets and strategies. Future research should focus on exploring the potential of ncRNA and epigenetic regulation as biomarkers for diagnosis and prognosis, as well as precision medicine and personalized treatment strategies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cigrovski Berkovic M, Croatia; Nwabo Kamdje AH, Cameroon S-Editor: Chen YL L-Editor: A P-Editor: Chen YX
| 1. | Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P. Obesity and diabetes-Not only a simple link between two epidemics. Diabetes Metab Res Rev. 2018;34:e3042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 186] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 2. | Barb D, Repetto EM, Stokes ME, Shankar SS, Cusi K. Type 2 diabetes mellitus increases the risk of hepatic fibrosis in individuals with obesity and nonalcoholic fatty liver disease. Obesity (Silver Spring). 2021;29:1950-1960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 3. | Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3146] [Cited by in RCA: 3642] [Article Influence: 202.3] [Reference Citation Analysis (0)] |
| 4. | Malone JI, Hansen BC. Does obesity cause type 2 diabetes mellitus (T2DM)? Pediatr Diabetes. 2019;20:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 221] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 5. | Czaja-Stolc S, Potrykus M, Stankiewicz M, Kaska Ł, Małgorzewicz S. Pro-Inflammatory Profile of Adipokines in Obesity Contributes to Pathogenesis, Nutritional Disorders, and Cardiovascular Risk in Chronic Kidney Disease. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 6. | de Vos WM, Tilg H, Van Hul M, Cani PD. Gut microbiome and health: mechanistic insights. Gut. 2022;71:1020-1032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 1260] [Article Influence: 420.0] [Reference Citation Analysis (0)] |
| 7. | Singer-Englar T, Barlow G, Mathur R. Obesity, diabetes, and the gut microbiome: an updated review. Expert Rev Gastroenterol Hepatol. 2019;13:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 8. | Formichi C, Nigi L, Grieco GE, Maccora C, Fignani D, Brusco N, Licata G, Sebastiani G, Dotta F. Non-Coding RNAs: Novel Players in Insulin Resistance and Related Diseases. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Ling C, Rönn T. Epigenetics in Human Obesity and Type 2 Diabetes. Cell Metab. 2019;29:1028-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 566] [Article Influence: 94.3] [Reference Citation Analysis (0)] |
| 10. | Kiran S, Kumar V, Kumar S, Price RL, Singh UP. Adipocyte, Immune Cells, and miRNA Crosstalk: A Novel Regulator of Metabolic Dysfunction and Obesity. Cells. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Yang WM, Jeong HJ, Park SY, Lee W. Induction of miR-29a by saturated fatty acids impairs insulin signaling and glucose uptake through translational repression of IRS-1 in myocytes. FEBS Lett. 2014;588:2170-2176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Zhang X, Xue XC, Wang Y, Cao FF, You J, Uzan G, Peng B, Zhang DH. Celastrol Reverses Palmitic Acid-Induced Insulin Resistance in HepG2 Cells via Restoring the miR-223 and GLUT4 Pathway. Can J Diabetes. 2019;43:165-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Li X, Bai C, Wang H, Wan T, Li Y. LncRNA MEG3 regulates autophagy and pyroptosis via FOXO1 in pancreatic β-cells. Cell Signal. 2022;92:110247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Yin DD, Zhang EB, You LH, Wang N, Wang LT, Jin FY, Zhu YN, Cao LH, Yuan QX, De W, Tang W. Downregulation of lncRNA TUG1 affects apoptosis and insulin secretion in mouse pancreatic β cells. Cell Physiol Biochem. 2015;35:1892-1904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 15. | Kim AY, Park YJ, Pan X, Shin KC, Kwak SH, Bassas AF, Sallam RM, Park KS, Alfadda AA, Xu A, Kim JB. Obesity-induced DNA hypermethylation of the adiponectin gene mediates insulin resistance. Nat Commun. 2015;6:7585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 170] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 16. | Ou XH, Zhu CC, Sun SC. Effects of obesity and diabetes on the epigenetic modification of mammalian gametes. J Cell Physiol. 2019;234:7847-7855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 17. | Sankar A, Mohammad F, Sundaramurthy AK, Wang H, Lerdrup M, Tatar T, Helin K. Histone editing elucidates the functional roles of H3K27 methylation and acetylation in mammals. Nat Genet. 2022;54:754-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 94] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 18. | Ling C, Bacos K, Rönn T. Epigenetics of type 2 diabetes mellitus and weight change - a tool for precision medicine? Nat Rev Endocrinol. 2022;18:433-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 74] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 19. | Rey F, Urrata V, Gilardini L, Bertoli S, Calcaterra V, Zuccotti GV, Cancello R, Carelli S. Role of long non-coding RNAs in adipogenesis: State of the art and implications in obesity and obesity-associated diseases. Obes Rev. 2021;22:e13203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 20. | Gao H, Kerr A, Jiao H, Hon CC, Rydén M, Dahlman I, Arner P. Long Non-Coding RNAs Associated with Metabolic Traits in Human White Adipose Tissue. EBioMedicine. 2018;30:248-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 21. | Chawla A, Schwarz EJ, Dimaculangan DD, Lazar MA. Peroxisome proliferator-activated receptor (PPAR) gamma: adipose-predominant expression and induction early in adipocyte differentiation. Endocrinology. 1994;135:798-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 561] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 22. | Giroud M, Scheideler M. Long Non-Coding RNAs in Metabolic Organs and Energy Homeostasis. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 23. | Li M, Sun X, Cai H, Sun Y, Plath M, Li C, Lan X, Lei C, Lin F, Bai Y, Chen H. Long non-coding RNA ADNCR suppresses adipogenic differentiation by targeting miR-204. Biochim Biophys Acta. 2016;1859:871-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 24. | Huang Y, Zheng Y, Jin C, Li X, Jia L, Li W. Long Non-coding RNA H19 Inhibits Adipocyte Differentiation of Bone Marrow Mesenchymal Stem Cells through Epigenetic Modulation of Histone Deacetylases. Sci Rep. 2016;6:28897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 25. | Squillaro T, Peluso G, Galderisi U, Di Bernardo G. Long non-coding RNAs in regulation of adipogenesis and adipose tissue function. Elife. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 26. | Divoux A, Karastergiou K, Xie H, Guo W, Perera RJ, Fried SK, Smith SR. Identification of a novel lncRNA in gluteal adipose tissue and evidence for its positive effect on preadipocyte differentiation. Obesity (Silver Spring). 2014;22:1781-1785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 27. | Lorente-Cebrián S, González-Muniesa P, Milagro FI, Martínez JA. MicroRNAs and other non-coding RNAs in adipose tissue and obesity: emerging roles as biomarkers and therapeutic targets. Clin Sci (Lond). 2019;133:23-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 28. | Zhao XY, Li S, Wang GX, Yu Q, Lin JD. A long noncoding RNA transcriptional regulatory circuit drives thermogenic adipocyte differentiation. Mol Cell. 2014;55:372-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 198] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 29. | Schmidt E, Dhaouadi I, Gaziano I, Oliverio M, Klemm P, Awazawa M, Mitterer G, Fernandez-Rebollo E, Pradas-Juni M, Wagner W, Hammerschmidt P, Loureiro R, Kiefer C, Hansmeier NR, Khani S, Bergami M, Heine M, Ntini E, Frommolt P, Zentis P, Ørom UA, Heeren J, Blüher M, Bilban M, Kornfeld JW. LincRNA H19 protects from dietary obesity by constraining expression of monoallelic genes in brown fat. Nat Commun. 2018;9:3622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 30. | Mi L, Zhao XY, Li S, Yang G, Lin JD. Conserved function of the long noncoding RNA Blnc1 in brown adipocyte differentiation. Mol Metab. 2017;6:101-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 31. | Knoll M, Lodish HF, Sun L. Long non-coding RNAs as regulators of the endocrine system. Nat Rev Endocrinol. 2015;11:151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 174] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 32. | Sun J, Ruan Y, Wang M, Chen R, Yu N, Sun L, Liu T, Chen H. Differentially expressed circulating LncRNAs and mRNA identified by microarray analysis in obese patients. Sci Rep. 2016;6:35421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Izquierdo AG, Crujeiras AB. Obesity-Related Epigenetic Changes After Bariatric Surgery. Front Endocrinol (Lausanne). 2019;10:232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 34. | Liang Y, Yu B, Wang Y, Qiao Z, Cao T, Zhang P. Duodenal long noncoding RNAs are associated with glycemic control after bariatric surgery in high-fat diet-induced diabetic mice. Surg Obes Relat Dis. 2017;13:1212-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | De Rosa S, Arcidiacono B, Chiefari E, Brunetti A, Indolfi C, Foti DP. Type 2 Diabetes Mellitus and Cardiovascular Disease: Genetic and Epigenetic Links. Front Endocrinol (Lausanne). 2018;9:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 231] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 36. | Guo J, Liu Z, Gong R. Long noncoding RNA: an emerging player in diabetes and diabetic kidney disease. Clin Sci (Lond). 2019;133:1321-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 37. | Goyal N, Kesharwani D, Datta M. Lnc-ing non-coding RNAs with metabolism and diabetes: roles of lncRNAs. Cell Mol Life Sci. 2018;75:1827-1837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 38. | Tello-Flores VA, Valladares-Salgado A, Ramírez-Vargas MA, Cruz M, Del-Moral-Hernández O, Cahua-Pablo JÁ, Ramírez M, Hernández-Sotelo D, Armenta-Solis A, Flores-Alfaro E. Altered levels of MALAT1 and H19 derived from serum or serum exosomes associated with type-2 diabetes. Noncoding RNA Res. 2020;5:71-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 39. | Sathishkumar C, Prabu P, Mohan V, Balasubramanyam M. Linking a role of lncRNAs (long non-coding RNAs) with insulin resistance, accelerated senescence, and inflammation in patients with type 2 diabetes. Hum Genomics. 2018;12:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 40. | Wang X, Chang X, Zhang P, Fan L, Zhou T, Sun K. Aberrant Expression of Long Non-Coding RNAs in Newly Diagnosed Type 2 Diabetes Indicates Potential Roles in Chronic Inflammation and Insulin Resistance. Cell Physiol Biochem. 2017;43:2367-2378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 41. | Tang N, Jiang S, Yang Y, Liu S, Ponnusamy M, Xin H, Yu T. Noncoding RNAs as therapeutic targets in atherosclerosis with diabetes mellitus. Cardiovasc Ther. 2018;36:e12436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 42. | Zhang L, Wang YM. Expression and function of lncRNA ANRIL in a mouse model of acute myocardial infarction combined with type 2 diabetes mellitus. J Chin Med Assoc. 2019;82:685-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Wang L, Su N, Zhang Y, Wang G. Clinical Significance of Serum lncRNA Cancer Susceptibility Candidate 2 (CASC2) for Chronic Renal Failure in Patients with Type 2 Diabetes. Med Sci Monit. 2018;24:6079-6084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 44. | Yu W, Zhao GQ, Cao RJ, Zhu ZH, Li K. LncRNA NONRATT021972 Was Associated with Neuropathic Pain Scoring in Patients with Type 2 Diabetes. Behav Neurol. 2017;2017:2941297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 45. | Kunej T, Jevsinek Skok D, Zorc M, Ogrinc A, Michal JJ, Kovac M, Jiang Z. Obesity gene atlas in mammals. J Genomics. 2013;1:45-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 46. | Klöting N, Berthold S, Kovacs P, Schön MR, Fasshauer M, Ruschke K, Stumvoll M, Blüher M. MicroRNA expression in human omental and subcutaneous adipose tissue. PLoS One. 2009;4:e4699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 241] [Cited by in RCA: 267] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 47. | Ortega FJ, Moreno-Navarrete JM, Pardo G, Sabater M, Hummel M, Ferrer A, Rodriguez-Hermosa JI, Ruiz B, Ricart W, Peral B, Fernández-Real JM. MiRNA expression profile of human subcutaneous adipose and during adipocyte differentiation. PLoS One. 2010;5:e9022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 275] [Cited by in RCA: 296] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 48. | Kim Y, Kim OK. Potential Roles of Adipocyte Extracellular Vesicle-Derived miRNAs in Obesity-Mediated Insulin Resistance. Adv Nutr. 2021;12:566-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 49. | Lee EK, Lee MJ, Abdelmohsen K, Kim W, Kim MM, Srikantan S, Martindale JL, Hutchison ER, Kim HH, Marasa BS, Selimyan R, Egan JM, Smith SR, Fried SK, Gorospe M. miR-130 suppresses adipogenesis by inhibiting peroxisome proliferator-activated receptor gamma expression. Mol Cell Biol. 2011;31:626-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 304] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 50. | Poy MN, Eliasson L, Krutzfeldt J, Kuwajima S, Ma X, Macdonald PE, Pfeffer S, Tuschl T, Rajewsky N, Rorsman P, Stoffel M. A pancreatic islet-specific microRNA regulates insulin secretion. Nature. 2004;432:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1531] [Cited by in RCA: 1602] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 51. | Jiménez-Lucena R, Camargo A, Alcalá-Diaz JF, Romero-Baldonado C, Luque RM, van Ommen B, Delgado-Lista J, Ordovás JM, Pérez-Martínez P, Rangel-Zúñiga OA, López-Miranda J. A plasma circulating miRNAs profile predicts type 2 diabetes mellitus and prediabetes: from the CORDIOPREV study. Exp Mol Med. 2018;50:1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 52. | Sebastiani G, Grieco GE, Brusco N, Ventriglia G, Formichi C, Marselli L, Marchetti P, Dotta F. MicroRNA Expression Analysis of In Vitro Dedifferentiated Human Pancreatic Islet Cells Reveals the Activation of the Pluripotency-Related MicroRNA Cluster miR-302s. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 53. | Belgardt BF, Ahmed K, Spranger M, Latreille M, Denzler R, Kondratiuk N, von Meyenn F, Villena FN, Herrmanns K, Bosco D, Kerr-Conte J, Pattou F, Rülicke T, Stoffel M. The microRNA-200 family regulates pancreatic beta cell survival in type 2 diabetes. Nat Med. 2015;21:619-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 54. | Latreille M, Hausser J, Stützer I, Zhang Q, Hastoy B, Gargani S, Kerr-Conte J, Pattou F, Zavolan M, Esguerra JL, Eliasson L, Rülicke T, Rorsman P, Stoffel M. MicroRNA-7a regulates pancreatic β cell function. J Clin Invest. 2014;124:2722-2735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 237] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 55. | Nesca V, Guay C, Jacovetti C, Menoud V, Peyot ML, Laybutt DR, Prentki M, Regazzi R. Identification of particular groups of microRNAs that positively or negatively impact on beta cell function in obese models of type 2 diabetes. Diabetologia. 2013;56:2203-2212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 56. | Tattikota SG, Rathjen T, McAnulty SJ, Wessels HH, Akerman I, van de Bunt M, Hausser J, Esguerra JL, Musahl A, Pandey AK, You X, Chen W, Herrera PL, Johnson PR, O'Carroll D, Eliasson L, Zavolan M, Gloyn AL, Ferrer J, Shalom-Feuerstein R, Aberdam D, Poy MN. Argonaute2 mediates compensatory expansion of the pancreatic β cell. Cell Metab. 2014;19:122-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 57. | Zhao Z, Li X, Jian D, Hao P, Rao L, Li M. Hsa_circ_0054633 in peripheral blood can be used as a diagnostic biomarker of pre-diabetes and type 2 diabetes mellitus. Acta Diabetol. 2017;54:237-245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 161] [Cited by in RCA: 189] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 58. | Fang Y, Wang X, Li W, Han J, Jin J, Su F, Zhang J, Huang W, Xiao F, Pan Q, Zou L. Screening of circular RNAs and validation of circANKRD36 associated with inflammation in patients with type 2 diabetes mellitus. Int J Mol Med. 2018;42:1865-1874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 59. | Stoll L, Rodríguez-Trejo A, Guay C, Brozzi F, Bayazit MB, Gattesco S, Menoud V, Sobel J, Marques AC, Venø MT, Esguerra JLS, Barghouth M, Suleiman M, Marselli L, Kjems J, Eliasson L, Renström E, Bouzakri K, Pinget M, Marchetti P, Regazzi R. A circular RNA generated from an intron of the insulin gene controls insulin secretion. Nat Commun. 2020;11:5611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 60. | Zhu W, Shen Y, Liu J, Fei X, Zhang Z, Li M, Chen X, Xu J, Zhu Q, Zhou W, Zhang M, Liu S, Du J. Epigenetic alternations of microRNAs and DNA methylation contribute to gestational diabetes mellitus. J Cell Mol Med. 2020;24:13899-13912. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 61. | He L, Huang H, Bradai M, Zhao C, You Y, Ma J, Zhao L, Lozano-Durán R, Zhu JK. DNA methylation-free Arabidopsis reveals crucial roles of DNA methylation in regulating gene expression and development. Nat Commun. 2022;13:1335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 111] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 62. | Olsson AH, Volkov P, Bacos K, Dayeh T, Hall E, Nilsson EA, Ladenvall C, Rönn T, Ling C. Genome-wide associations between genetic and epigenetic variation influence mRNA expression and insulin secretion in human pancreatic islets. PLoS Genet. 2014;10:e1004735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 136] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 63. | Rautenberg EK, Hamzaoui Y, Coletta DK. Mini-review: Mitochondrial DNA methylation in type 2 diabetes and obesity. Front Endocrinol (Lausanne). 2022;13:968268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 64. | Shah UJ, Xie W, Flyvbjerg A, Nolan JJ, Højlund K, Walker M, Relton CL, Elliott HR; RISC consortium. Differential methylation of the type 2 diabetes susceptibility locus KCNQ1 is associated with insulin sensitivity and is predicted by CpG site specific genetic variation. Diabetes Res Clin Pract. 2019;148:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 65. | Uno Y, Murayama N, Kato M, Tanaka S, Ohkoshi T, Yamazaki H. Genetic Variants of Glutathione S-Transferase GSTT1 and GSTT2 in Cynomolgus Macaques: Identification of GSTT Substrates and Functionally Relevant Alleles. Chem Res Toxicol. 2018;31:1086-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 66. | Volkov P, Olsson AH, Gillberg L, Jørgensen SW, Brøns C, Eriksson KF, Groop L, Jansson PA, Nilsson E, Rönn T, Vaag A, Ling C. A Genome-Wide mQTL Analysis in Human Adipose Tissue Identifies Genetic Variants Associated with DNA Methylation, Gene Expression and Metabolic Traits. PLoS One. 2016;11:e0157776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 67. | Walaszczyk E, Luijten M, Spijkerman AMW, Bonder MJ, Lutgers HL, Snieder H, Wolffenbuttel BHR, van Vliet-Ostaptchouk JV. DNA methylation markers associated with type 2 diabetes, fasting glucose and HbA(1c) levels: a systematic review and replication in a case-control sample of the Lifelines study. Diabetologia. 2018;61:354-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 68. | Shvangiradze TA, Bondarenko IZ, Troshina EA, Shestakova MV. [MiRNAs in the diagnosis of cardiovascular diseases associated with type 2 diabetes mellitus and obesity]. Ter Arkh. 2016;88:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 69. | López-Armas GC, Yessenbekova A, González-Castañeda RE, Arellano-Arteaga KJ, Guerra-Librero A, Ablaikhanova N, Florido J, Escames G, Acuña-Castroviejo D, Rusanova I. Role of c-miR-21, c-miR-126, Redox Status, and Inflammatory Conditions as Potential Predictors of Vascular Damage in T2DM Patients. Antioxidants (Basel). 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 70. | Li X. MiR-375, a microRNA related to diabetes. Gene. 2014;533:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 71. | Wang H, Xia Y, Zhang Y. Diagnostic significance of serum lncRNA HOTAIR and its predictive value for the development of chronic complications in patients with type 2 diabetes mellitus. Diabetol Metab Syndr. 2021;13:97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 72. | Costa-Júnior JM, Ferreira SM, Kurauti MA, Bernstein DL, Ruano EG, Kameswaran V, Schug J, Freitas-Dias R, Zoppi CC, Boschero AC, Oliveira CAM, Santos GJ, Carneiro EM, Kaestner KH. Paternal Exercise Improves the Metabolic Health of Offspring via Epigenetic Modulation of the Germline. Int J Mol Sci. 2021;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 73. | Zhang YP, Ye SZ, Li YX, Chen JL, Zhang YS. Research Advances in the Roles of Circular RNAs in Pathophysiology and Early Diagnosis of Gestational Diabetes Mellitus. Front Cell Dev Biol. 2021;9:739511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 74. | Ren S, Lin P, Wang J, Yu H, Lv T, Sun L, Du G. Circular RNAs: Promising Molecular Biomarkers of Human Aging-Related Diseases via Functioning as an miRNA Sponge. Mol Ther Methods Clin Dev. 2020;18:215-229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 75. | Chen ZJ, Shi XJ, Fu LJ, Liu J, Shi K, Zhang WB, Su PK. Serum and exosomal hsa_circ_0000907 and hsa_circ_0057362 as novel biomarkers in the early diagnosis of diabetic foot ulcer. Eur Rev Med Pharmacol Sci. 2020;24:8117-8126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 76. | Behrooz M, Hajjarzadeh S, Kahroba H, Ostadrahimi A, Bastami M. Expression pattern of miR-193a, miR122, miR155, miR-15a, and miR146a in peripheral blood mononuclear cells of children with obesity and their relation to some metabolic and inflammatory biomarkers. BMC Pediatr. 2023;23:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 77. | Chen Q, Xi X, Ma J, Wang X, Xia Y, Deng Y, Li Y. The mechanism by which crocetin regulates the lncRNA NEAT1/miR-125b-5p/SOX7 molecular axis to inhibit high glucose-induced diabetic retinopathy. Exp Eye Res. 2022;222:109157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 78. | Shirakawa J, Togashi Y, Basile G, Okuyama T, Inoue R, Fernandez M, Kyohara M, De Jesus DF, Goto N, Zhang W, Tsuno T, Kin T, Pan H, Dreyfuss JM, Shapiro AMJ, Yi P, Terauchi Y, Kulkarni RN. E2F1 transcription factor mediates a link between fat and islets to promote β cell proliferation in response to acute insulin resistance. Cell Rep. 2022;41:111436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 79. | Liu J, Carnero-Montoro E, van Dongen J, Lent S, Nedeljkovic I, Ligthart S, Tsai PC, Martin TC, Mandaviya PR, Jansen R, Peters MJ, Duijts L, Jaddoe VWV, Tiemeier H, Felix JF, Willemsen G, de Geus EJC, Chu AY, Levy D, Hwang SJ, Bressler J, Gondalia R, Salfati EL, Herder C, Hidalgo BA, Tanaka T, Moore AZ, Lemaitre RN, Jhun MA, Smith JA, Sotoodehnia N, Bandinelli S, Ferrucci L, Arnett DK, Grallert H, Assimes TL, Hou L, Baccarelli A, Whitsel EA, van Dijk KW, Amin N, Uitterlinden AG, Sijbrands EJG, Franco OH, Dehghan A, Spector TD, Dupuis J, Hivert MF, Rotter JI, Meigs JB, Pankow JS, van Meurs JBJ, Isaacs A, Boomsma DI, Bell JT, Demirkan A, van Duijn CM. An integrative cross-omics analysis of DNA methylation sites of glucose and insulin homeostasis. Nat Commun. 2019;10:2581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 80. | Liu D, Yang KY, Chan VW, Ye W, Chong CCN, Wang CC, Wang H, Zhou B, Cheng KKY, Lui KO. YY1 Regulates Glucose Homeostasis Through Controlling Insulin Transcription in Pancreatic β-Cells. Diabetes. 2022;71:961-977. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 81. | Ji C, Guo X. The clinical potential of circulating microRNAs in obesity. Nat Rev Endocrinol. 2019;15:731-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 191] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 82. | Zhao XY, Xiong X, Liu T, Mi L, Peng X, Rui C, Guo L, Li S, Li X, Lin JD. Long noncoding RNA licensing of obesity-linked hepatic lipogenesis and NAFLD pathogenesis. Nat Commun. 2018;9:2986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 126] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 83. | Wijesinghe SN, Nicholson T, Tsintzas K, Jones SW. Involvements of long noncoding RNAs in obesity-associated inflammatory diseases. Obes Rev. 2021;22:e13156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 84. | Alfaifi M, Verma AK, Alshahrani MY, Joshi PC, Alkhathami AG, Ahmad I, Hakami AR, Beg MMA. Assessment of Cell-Free Long Non-Coding RNA-H19 and miRNA-29a, miRNA-29b Expression and Severity of Diabetes. Diabetes Metab Syndr Obes. 2020;13:3727-3737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 85. | Guo X, Wu X, Han Y, Tian E, Cheng J. LncRNA MALAT1 protects cardiomyocytes from isoproterenol-induced apoptosis through sponging miR-558 to enhance ULK1-mediated protective autophagy. J Cell Physiol. 2019;234:10842-10854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |