Published online Sep 15, 2021. doi: 10.4239/wjd.v12.i9.1518
Peer-review started: January 26, 2021
First decision: May 3, 2021
Revised: May 26, 2021
Accepted: July 26, 2021
Article in press: July 26, 2021
Published online: September 15, 2021
Processing time: 223 Days and 18.1 Hours
Type 1 diabetes (T1D) is one of the most common chronic diseases in children and adolescents worldwide. Its etiopathogenesis results from the interplay of genetic and environmental variables. Among the latter, psychological stress has been implicated in disease onset as well as disease management. Various studies, including large population-based studies, have highlighted the role of stressful life events in the etiopathogenesis of T1D. In this article, we also emphasize the importance of attachment in the early child-caregiver relationship, which can be seen as a measure of the quality of the relationship and is crucial for stress and emotional regulation. It serves as a model for all subsequent relationships in one’s life. We summarize some of the few studies performed in the field of attachment and T1D etiopathogenesis or management. T1D management demands a lifelong therapeutic regimen to prevent acute and chronic complications. In addition to psychological stress, psychological factors such as family functioning, developmental adjustment, autonomy, mental health problems and other factors have been found to relate to metabolic control. Psychological factors need to be understood not as a single directional causality-based principle but as a dynamic bi- or multidirectional system that is affected by the normal developmental transitions of childhood and adolescence.
Core Tip: The incidence of type 1 diabetes is increasing worldwide. Its diagnosis and management present a major burden for the child as well as the family. Different psychological factors affecting the development and course of type 1 diabetes need to be understood not as a single directional causality-based principle but as a dynamic bi- or multidirectional system that is affected by the normal developmental transitions of childhood and adolescence. The current article summarizes some of these factors, especially those related to stress and its regulation, both in an attachment context and in relation to family dynamics and psychopathology.
- Citation: Turin A, Drobnič Radobuljac M. Psychosocial factors affecting the etiology and management of type 1 diabetes mellitus: A narrative review. World J Diabetes 2021; 12(9): 1518-1529
- URL: https://www.wjgnet.com/1948-9358/full/v12/i9/1518.htm
- DOI: https://dx.doi.org/10.4239/wjd.v12.i9.1518
Type 1 diabetes (T1D) is the result of autoimmune-mediated destruction of insulin producing beta cells and is considered one of the most common pediatric illnesses with an increasing incidence of 2%-5% annually. It peaks in presentation between the ages of five to seven and puberty[1,2]. Its management demands a lifelong therapeutic regimen to prevent acute and chronic complications[3]. Psychosocial factors have been shown to play a role in both its etiopathogenesis and in disease management. However, recent studies have highlighted the importance of bidirectionality in the relationship between T1D and psychosocial well-being[4]. Stressful life events have been shown to be related to the onset and the course of T1D in various studies[5-9]. It is important to understand the effect of stress not only as an external factor influencing an individual, but to consider its effect in the light of a person’s distinct and unique way of stress regulation[10]. Younger children depend highly on their parents for disease management and stress regulation[11,12]. On the other hand, older children and adolescents transition from solely depending on their parents to achieving more independence and autonomy in stress regulation and disease management[13].
We conducted an electronic literature search through PubMed. The search was performed in four sessions using the keywords: “type 1 diabetes” and “attachment” (first session), “type 1 diabetes” and “glycemic control” or “management” and “stress” or “serious life events” and “children” or “adolescent” and “mother” or “parent” (second session), “type 1 diabetes” and “family functioning” (third session) and “type 1 diabetes” and “mental health” or “psychiatric” or “psychopathology” (fourth session). From the first session only 7 articles from 251 were relevant for the researched topic, in the second session from 175 articles, 14 were relevant, in third session from 4771, 24 were relevant and in the fourth session 25 were relevant from 1909 articles. Only articles related to child or adolescent T1D etiopathogenesis or management were included. Those that did not contain an abstract or were not in English were excluded. Subsequently, articles from the authors’ personal archives considered important were added.
Several studies, including large population-based prospective studies, have highlighted the role of stressful life events in the manifestation of T1D. The All Babies in Southeast Sweden study included 10495 non-diabetic children, and data was collected at the ages of 2–3, 5–6, 8 and 10–13 years. Fifty-eight children were subsequently diagnosed with T1D. Family psychological stress was measured via questionnaires given to the parents assessing serious life events, parenting stress, parental worries and the parental social support. The results showed that serious life events experienced in childhood, such as death or illness in the family, family conflicts, violence and unemployment were associated with a higher risk of future diagnosis of T1D independent of heredity[5]. In another study, based on the same registry, 4400 consecutive 1-year-old children were included. Parents completed questionnaires at birth and at 1 year, including various measures of psychosocial stress (e.g., parenting stress) and sociodemographic background. Blood samples drawn from the children at 1 year were analyzed for T1D-associated autoantibodies toward tyrosine phosphatase and glutamic acid decarboxylase. The results showed that psychological stress, measured as psychosocial strain in the family, was involved in the induction or progression of diabetes-related autoimmunity[6]. Lundgren et al[14] reported a significantly increased risk of T1D in children with stress and severe life events (such as severe disease in the family, death of a close relative, serious accident, violence, divorce, unemployment, etc.) occurring during the child's first 2 years of life as reported by the parents (n = 3784).
Virk et al[15] conducted a population-based follow-up study on subjects from Danish national registers. They categorized 1740245 children as exposed to bereavement if they lost a mother, a father or a sibling from the age of 5 years onwards. The children were then followed until a first diagnosis of diabetes, death or emigration. According to their results, bereavement was associated with an increased rate of T1D when the exposure began after the age of 11 years. However, a Swedish nationwide study did not support the hypothesis that psychosocial stressful life events were involved in the development of autoimmune T1D in young adults. The study included 349 newly diagnosed patients aged 15-34 years and 979 control subjects. They used questionnaires asking about diabetes heredity, social environment, educational level and life events experienced during the 12 mo before diagnosis. No major stress factors were detected in the patients with T1D. Nevertheless, in contrast with the control subjects, the T1D group had experienced fewer conflicts with their parents and had less often broken contacts with friends[16].
To understand the role of stress we must consider how it is regulated and managed inside the family dynamics. Individual stressful life events and the effect of these events on an individual in terms of stress regulation and resilience are important. The impact of stressful life events on the individual is influenced by genetic vulnerability, coping mechanisms, personality type and social support[10]. A dysregulated individual response to psychological stress was proposed as one of the factors contributing in a complex way to increased insulin demands and pancreatic beta-cell overload[17-21], which in turn is believed to mediate their destruction and consequently the emergence of T1D[22].
A rather interesting approach to understanding the role of stress is via the theory of attachment, an early theory of psychological development, which has received a lot of attention in recent years. Attachment is described as a behavioral and physiological system, which enables an individual’s dynamic adaptation to his or her environment. It develops in close interaction between an infant and his/her caretaker and influences the quality of interpersonal relationships throughout life. It is inextricably linked to the way one regulates stress, at the beginning with the help of the primary caretaker and later by oneself in accordance with the internal attachment representations. These are categorized as secure or insecure, the latter being related to a more intensive stress response compared to the former[23]. Few studies have been carried out to determine the role of attachment in the risk of T1D. Sepa et al[22] explored the connection between the mothers’ attachment insecurity and diabetes-related autoimmunity in early childhood using Adult Attachment Interviews with a group of mothers with antibody-positive infants and a group of mothers with antibody-negative infants. Their results showed a larger proportion of insecure mothers in the antibody-positive group, although the association was not statistically significant. They concluded that if an association between mothers’ attachment and diabetes-related autoimmunity in children exists, it is not very strong, acknowledging their small sample size as well as a generally imperfect correlation between mother and child attachment. Based on their findings, our group conducted a study that included 101 dyads of children with T1D and their caretakers and 106 healthy control pairs. Attachment between the children and their parents was evaluated via a questionnaire (the parents) and the Child Attachment Interview (the children). The results showed no correlation between the attachment of the children to their parents and T1D. However, a correlation between higher caretaker attachment anxiety and child’s T1D diagnosis was revealed[24].
Various studies have highlighted the role of stress in T1D management and thus metabolic control. In a cross-sectional study, Commissariat et al[7] studied the association between stressful life events, T1D management and psychological measures in adolescents with T1D. One hundred and seventy-eight teens and their parents were included in the research. Results showed that teens with more stressful life events such as the hospitalization of a family member, getting a bad report card, witnessing serious arguments between parents or a serious illness or injury of a family member, reported lower self-efficacy, poorer adherence, poorer quality of life and higher glycated hemoglobin (HbA1c).
In a prospective study of 128 families, Stanek et al[8] investigated the occurrence of stressful life events within the first year of T1D diagnosis in children, assessing correlations with family functioning and parental psychosocial measures and diabetes management. More than half of the families reported one or more stressful life events, such as the child attending a different school, caregiver job change, a change in household income, a change in caregiver marital status and/or a significant change in the health of a family member. Baseline active avoidance coping, parental depression and diabetes-related family conflict correlated with a higher number of stressful life events. There were also cross-sectional associations between HbA1c, a decrease in household income, a school change and/or a job change at various time points in the study. Rechenberg et al[9] included 320 adolescents in their cross-sectional research examining the associations between general stress (the degree to which an individual considers his or her life to be stressful over the previous month), diabetes-specific stress (such as telling others about the diabetes diagnosis or others noticing the insulin pump, stress about “bad numbers”, stress about parental involvement in diabetes care and stress about interference of diabetes in daily activities), glycemic control (HbA1c), self-management and diabetes-specific quality of life. Higher general and diabetes-specific stress were significantly associated with higher HbA1c, poorer self-management activities and lower diabetes-specific quality of life. Diabetes-specific stress accounted for a significant proportion of the variance in HbA1c, while general stress did not. On the other hand, in a study with 132 children with T1D, Helgeson et al[25] found that only general parental stress was associated with poorer child outcomes, whereas diabetes-specific parental stress was associated with better child outcomes. Both types of stress, however, were associated with poorer parental mental health.
Rosenberg and Shields[26] conducted a pilot study on 31 families that explored the associations between parent and adolescent reports of adolescent attachment and glycemic control in adolescents with T1D. Adolescents and parents reported on their perceptions of the adolescents’ attachment to their mothers and fathers. The mothers’ perceptions of adolescents’ attachment were significantly correlated with adolescents’ HbA1c, indicating that maternal perceptions of more secure attachment were associated with better glycemic control. Neither fathers’ perceptions nor adolescents’ reports of attachment significantly correlated with glycemic control.
Ciechanowski et al[27] conducted their attachment-based research on an adult sample and presented evidence that dismissing attachment (a type of insecure attachment) was related to poor glycemic control. Costa-Cordella et al[28] assessed the role of attachment in T1D management in children. The results on 77 mother-child dyads showed a negative correlation of secure child attachment and HbA1c, which was seen only in boys but not in girls. The same author conducted a study in which mentalization (assessed by the Reflective Functioning Scale) was determined in two groups of mother-son dyads (with good vs poor diabetes control). Reflective functioning refers to an essential human capacity to understand other’s behavior considering their underlying mental states and intentions. Better reflective functioning correlates with more secure attachment. Their results showed that both maternal and child reflective functioning were higher in the good diabetes control group compared to the poor diabetes control group and were negatively correlated with HbA1c in the total sample. Meaning the higher the reflective functioning, the lower the HbA1c[4].
The diagnosis of T1D is a source of stress for the family and can have a negative impact on family functioning[29-31]. Additionally, numerous studies have linked various aspects of family functioning to metabolic control[32-42]. Factors such as positive parental emotional support, family communication and sufficient parental guidance with diabetes-related care have been linked to improved metabolic control, while a high level of family conflict as well as negative and unsupportive parental behavior are linked to poorer metabolic control and adherence[32,34,43-47].
In a study by Lewin et al[32] of 109 children, two dimensions of family functioning, warm/caring and guidance/control, were assessed. The results demonstrated that family functioning and adherence were strongly associated with metabolic control and accounted for as much as 34% of its variance. The research highlighted the role of adherence as a mediating factor between the family functioning and metabolic control.
A Danish population-based study included all families with a child diagnosed with T1D. They assessed seven dimensions of family functioning and their relationship to metabolic control: problem solving; communication; roles; affective responsiveness; affective involvement; behavior control; and overall family functioning. Their results showed that discrepancies in family functioning were associated with higher HbA1c levels[34].
However, other studies have found no association between aspects of family life and metabolic control[48,49]. For example, Kovacs et al[48] conducted a study of 85 children with T1D and assessed the relationship between two aspects of family functioning: parental perception of overall quality of family life and quality of the parent’s marriage. Their results showed no relationship between family functioning and the child’s glycemic control. Similarly, Gowers et al[49] found no association between various aspects of family functioning and metabolic control, among a sample of 60 children and adolescents with T1D. They found, however, a significant positive association of the parental involvement in administering injections.
Patients with T1D need the support of their family and the diabetes team to keep up with their diabetes management. The roles of the young patients and their families change throughout the developmental span from childhood to adolescence. Over time, the responsibility for diabetes management transitions from the parents (caregivers) to a shared responsibility between youth and caregivers, with older teens ultimately taking on the majority of self-care responsibilities[13].
Berg et al[12] suggested a developmental model for understanding the interplay of the child’s self-regulation skills, the parents’ involvement and diabetes management as a dynamic bidirectional system changing throughout development. Each developmental period has its unique developmental challenges that affect diabetes management. Very young children, for example, are completely dependent on parental caretaking. Their capacity to self-regulate behavior, emotions, sleeping, eating and physical activity is labile, which may complicate TD1 care[11,12]. Parental characteristics, such as marital status, socioeconomic status and coping style also influence diabetes management, as does the individual child’s character, such as temperament. For example, higher activity levels and shorter attention span were associated with poor child cooperation with daily T1D care in a study performed on 34 children with T1D[11,50].
Many studies have shown deterioration of metabolic control when children transition into adolescence, with a subsequent improvement during adulthood[25,51-54]. Therefore, adolescence itself is a stage that poses a specific risk to the management of diabetes. It is a period of complex physiological and psychological changes that can all influence diabetes management. Teens move from complete dependence on their caregivers to a more independent lifestyle. This occurs against a background of major changes in the hormonal mediators of puberty, the latter representing a biological factor contributing to deteriorated metabolic control due to insulin resistance[25]. As such, adolescents not only have to master the skills of diabetes self-management but also negotiate a new balance between autonomy and connectedness with their caregivers[12]. However, family support in terms of the caregiver’s involvement in diabetes management continues to be important[55]. Different studies have shown that supportive, cohesive families with low levels of conflict were more likely to have adolescents with strong adherence and good metabolic control than families without such cohesion[36]. Despite being less involved in the management of T1D in adolescence, greater parental monitoring was related to better adherence and lower levels of HbA1c[43,56,57].
A higher incidence of mental health problems such as depression, anxiety and eating disorders were reported in children or adolescents with T1D compared to their healthy peers[58-65].
Butwicka et al[59] conducted a population-based case-cohort study on individuals born in Sweden between 1973 and 2009. Children with T1D (n = 17122) and their healthy siblings (n = 18847) were identified and followed until their 18th birthday. Their results showed that the risk of psychiatric morbidity in children with T1D compared with the general population was tripled within 6 mo of diabetes onset and doubled within the total observation period. They also reported an increased risk of attempted suicide[59].
Another population-based national register study, conducted on 5084 Danish children and adolescents with T1D and 35588 healthy controls, reported an increased risk of eating disorders, anxiety and mood disorders, substance misuse and personality disorders in the years following T1D onset. The highest risk was seen in subjects with diabetes onset between the ages of 10 and 14 years. The risk increased with the duration of T1D, with the highest risk occurring 5 or more years after the diagnosis[60].
Contrary to the research mentioned above, there are also studies that have shown a lower or equal prevalence of mental health problems in youth with T1D compared to healthy populations[66-69].
Silverstein et al[67] found no evidence of increased psychopathology across a wide range of mental health measures in youth with T1D in a large Norwegian population study that included 9883 adolescents aged 16-19 years, 40 of whom were diagnosed with T1D.
Another large population-based study on Brazilian adolescents aged 12-17 years compared 116 youth with T1D and 73508 healthy youth. The results showed that mental health symptoms but not disorders were more common in youth with T1D[68].
A case-control study on a Slovene cohort of 126 adolescents with T1D and 499 healthy controls reported a lower prevalence of suicidal thoughts, suicide attempts and self-injurious and other risk-taking behaviors in adolescents with T1D (especially males) as compared to the general population of adolescents and a higher prevalence of disturbed eating behavior in females with T1D[70,71]. Suicidal behavior in adolescents with T1D, however, was related to poorer metabolic control in the same cohort[71].
According to the research, mental health problems are related to poor glycemic control[61,64,71-75]. However, the results of studies in this area are mixed, as some studies have found only a weak association, or no association at all, between mental health problems and glycemic control[76-79].
In a Danish population-based study of 4725 children and adolescents with T1D, 1035 had at least one psychiatric disorder. A high average HbA1c level during the first 2 years predicted a higher risk of psychiatric diagnosis. Patients with psychiatric comorbidities had higher HbA1c levels and an increased risk of hospitalization with diabetic ketoacidosis[72].
On the other hand, T1D is also related to an increased risk of neurodevelopmental disorders such as attention-deficit/hyperactivity disorder and autism spectrum disorders. The risk, according to a recent Swedish population-based cohort study, increases with HbA1c levels[80]. Previous studies have shown a relationship between attention-deficit/hyperactivity disorder and poor metabolic control suggesting that patients with T1D should be assessed for attention-deficit/hyperactivity disorder symptoms[81,82].
Having T1D necessarily means having to conform to a strict behavioral and dietary regime, which is a source of stress for the children and their parents, especially the mothers, who are usually responsible for most of the diabetes management[83]. Post-traumatic stress symptoms have been commonly described in children and mothers as well as clinically significant levels of symptoms of anxiety and depression[30,84-86]. While post-traumatic stress symptoms were most severe at disease onset, they often persisted until 1 to 5 years after the diagnosis of T1D[83,84]. Together with diabetes-specific stress, the post-traumatic stress symptoms following the diagnosis of T1D adversely affect children’s health[83]. Landolt et al[87] evaluated the rates of post-traumatic stress disorder and symptoms in mothers and fathers of children with newly diagnosed T1D. Parents of 38 children with newly diagnosed T1D were included in the assessment. Twenty-four percent of the mothers and 22% of the fathers met full diagnostic criteria for current post-traumatic stress disorder. In addition, 51% of the mothers and 41% of the fathers met criteria for partial or subclinical post-traumatic stress disorder.
A study by Rumburg et al[86] included 81 mothers of youth aged 10-16 with T1D duration of at least 1 year. They measured diabetes distress and maternal depressive symptoms. The results showed that mothers’ overall diabetes distress was strongly related to maternal depressive symptoms, and relationship-related diabetes distress was significantly associated with adolescents’ HbA1c. Fear of hypoglycemia, one of the most disturbing acute complications, is an important source of parental stress, which is in turn related to worse metabolic control. Nevertheless, some studies propose that the fear of hypoglycemia is to a certain extent adaptive because it leads to more frequent diabetes monitoring[88,89].
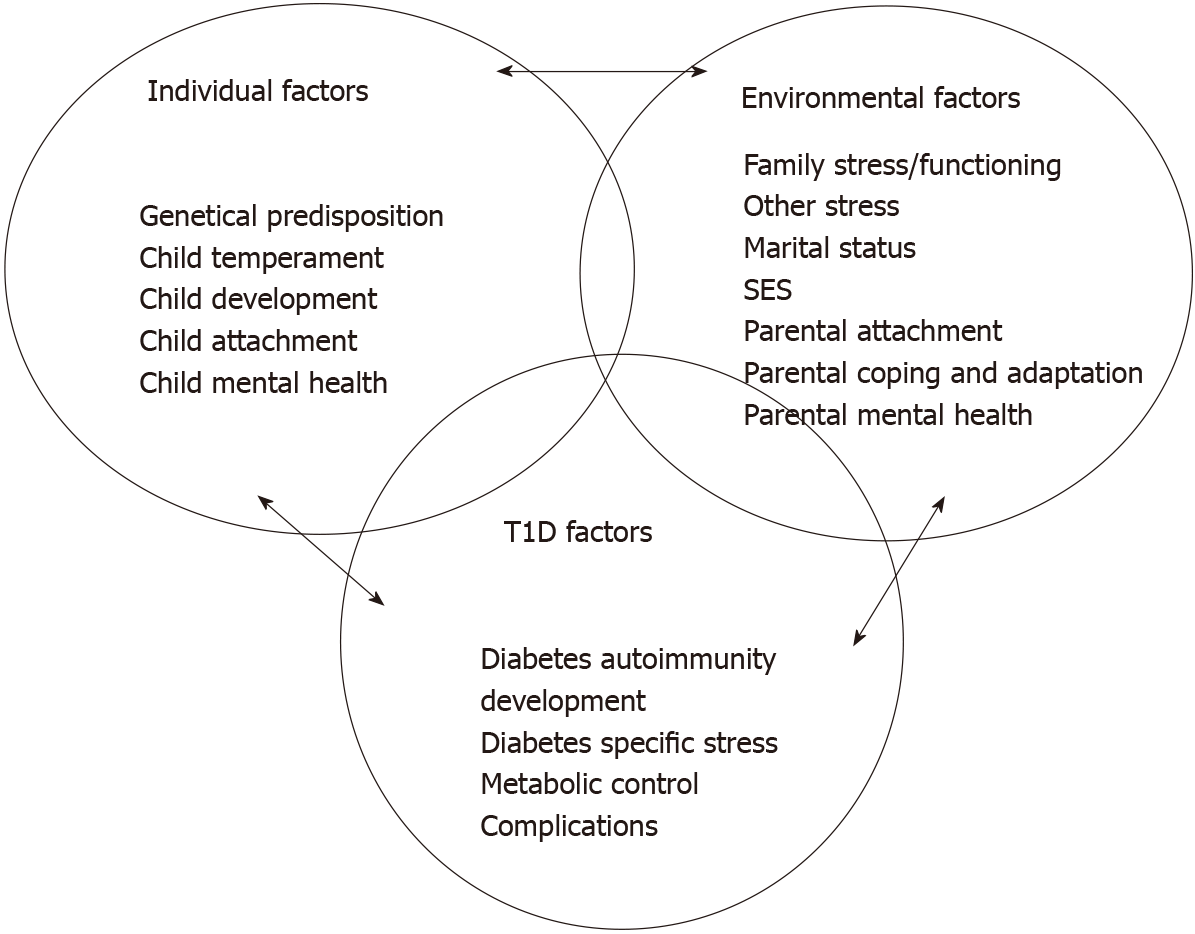
So far, we have presented the role of psychosocial factors such as stress, security of attachment to parents, family dynamics and mental disorder in the etiology of T1D and metabolic control. The recent literature, however, emphasizes the bidirectionality between psychosocial variables and T1D: T1D affects psychosocial functioning in a negative way, which in turn negatively impacts the course of T1D[4]. An attempt of a diagrammatic presentation of these influences is shown in Figure 1.
According to the transactional stress and coping model, a chronic childhood illness is seen as a stressor to which children and families attempt to adapt. The ways in which mothers cope with the stress has an important impact on both maternal and adolescent adjustment to the disease[90]. Many studies have shown that T1D poses diabetes-specific risk to the mental health of mothers who usually bear higher responsibility for their child’s diabetes care. The stress often results in clinical symptoms of depression and anxiety, which are related to poor glycemic control of the child’s T1D[86,91].
Jaser et al[90] measured diabetes-related stress and coping in 118 mothers of adolescents aged 10-16 years with T1D. The mothers were asked how often they experienced diabetes-related stress (e.g., taking care of diabetes, frequently reminding an adolescent to take care of him/herself), and they then completed a questionnaire asking how they responded to these stressors. Three ways of coping were sub
This bidirectional system must also be understood as a dynamic system that moves through different developmental stages. Young children depend mostly on their parents in diabetes care[11,12], while adolescents gradually take over the management control[13]. According to this, diabetes-specific family stress was shown to be negatively associated to the age of the affected children[92].
The present narrative review summarizes some of the psychosocial factors that influence the etiology and management of T1D in children and adolescents, with an emphasis on stressful life events and stress regulation inside the family dynamic and highlighting the role of the attachment. Stressful life events have been associated with T1D etiology and T1D management in many studies, as have family dynamics and the child and parent psychiatric morbidity. Many clinical guidelines thus emphasize the importance of family support as well as performing an assessment of psychosocial functioning and screening for psychiatric disorders. There is also a vast literature considering the impact of development and normal transitions throughout a child’s life on the management of T1D. Less research has been performed in the field of attachment and understanding the significance of the primary relationships between the children and their caregivers for the regulation of stress and successful management of T1D. To better understand the complex multidirectional interplay of psychosocial factors between the individual and the family in the induction, progression and management of T1D, more longitudinal and interdisciplinary studies combining the fields of (neuro)endocrinology, stress regulation and developmental psychology are needed.
The authors wish to thank all the children, adolescents and their parents as well as the staff from the Department of Endocrinology, Diabetes and Metabolism, University Medical Centre Ljubljana for their kind cooperation and dedicated work on the diabetes research.
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Slovenia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He X, Klobucar Majanovic S S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Liu JH
| 1. | Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014;383:69-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1462] [Cited by in RCA: 1642] [Article Influence: 149.3] [Reference Citation Analysis (0)] |
| 2. | Patterson CC, Harjutsalo V, Rosenbauer J, Neu A, Cinek O, Skrivarhaug T, Rami-Merhar B, Soltesz G, Svensson J, Parslow RC, Castell C, Schoenle EJ, Bingley PJ, Dahlquist G, Jarosz-Chobot PK, Marčiulionytė D, Roche EF, Rothe U, Bratina N, Ionescu-Tirgoviste C, Weets I, Kocova M, Cherubini V, Rojnic Putarek N, deBeaufort CE, Samardzic M, Green A. Trends and cyclical variation in the incidence of childhood type 1 diabetes in 26 European centres in the 25 year period 1989-2013: a multicentre prospective registration study. Diabetologia. 2019;62:408-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 321] [Article Influence: 53.5] [Reference Citation Analysis (0)] |
| 3. | American Diabetes Association. 13. Children and Adolescents: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44:S180-S199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 143] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 4. | Costa-Cordella S, Luyten P, Cohen D, Mena F, Fonagy P. Mentalizing in mothers and children with type 1 diabetes. Dev Psychopathol. 2021;33:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Nygren M, Carstensen J, Koch F, Ludvigsson J, Frostell A. Experience of a serious life event increases the risk for childhood type 1 diabetes: the ABIS population-based prospective cohort study. Diabetologia. 2015;58:1188-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Sepa A, Wahlberg J, Vaarala O, Frodi A, Ludvigsson J. Psychological stress may induce diabetes-related autoimmunity in infancy. Diabetes Care. 2005;28:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Commissariat PV, Volkening LK, Guo Z, ElBach JL, Butler DA, Laffel LM. Associations between major life events and adherence, glycemic control, and psychosocial characteristics in teens with type 1 diabetes. Pediatr Diabetes. 2018;19:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Stanek KR, Noser AE, Patton SR, Clements MA, Youngkin EM, Majidi S. Stressful life events, parental psychosocial factors, and glycemic management in school-aged children during the 1 year follow-up of new-onset type 1 diabetes. Pediatr Diabetes. 2020;21:673-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Rechenberg K, Whittemore R, Holland M, Grey M. General and diabetes-specific stress in adolescents with type 1 diabetes. Diabetes Res Clin Pract. 2017;130:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Sharif K, Watad A, Coplan L, Amital H, Shoenfeld Y, Afek A. Psychological stress and type 1 diabetes mellitus: what is the link? Expert Rev Clin Immunol. 2018;14:1081-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Pierce JS, Kozikowski C, Lee JM, Wysocki T. Type 1 diabetes in very young children: a model of parent and child influences on management and outcomes. Pediatr Diabetes. 2017;18:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Berg CA, Butner J, Wiebe DJ, Hughes Lansing A, Osborn P, King PS, Palmer DL, Butler JM. Developmental model of parent-child coordination for self-regulation across childhood and into emerging adulthood: Type 1 diabetes management as an example. Dev Rev. 2017;46:1-26. [RCA] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Markowitz JT, Garvey KC, Laffel LM. Developmental changes in the roles of patients and families in type 1 diabetes management. Curr Diabetes Rev. 2015;11:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 14. | Lundgren M, Ellström K, Elding Larsson H; DiPiS study group. Influence of early-life parental severe life events on the risk of type 1 diabetes in children: the DiPiS study. Acta Diabetol. 2018;55:797-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Virk J, Ritz B, Li J, Obel C, Olsen J. Childhood Bereavement and Type 1 Diabetes: a Danish National Register Study. Paediatr Perinat Epidemiol. 2016;30:86-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Littorin B, Sundkvist G, Nyström L, Carlson A, Landin-Olsson M, Ostman J, Arnqvist HJ, Björk E, Blohmé G, Bolinder J, Eriksson JW, Scherstén B, Wibell L; Diabetes Incidence Study in Sweden (DISS). Family characteristics and life events before the onset of autoimmune type 1 diabetes in young adults: a nationwide study. Diabetes Care. 2001;24:1033-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | de Kloet ER, de Kloet SF, de Kloet CS, de Kloet AD. Top-down and bottom-up control of stress-coping. J Neuroendocrinol. 2019;31:e12675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Godoy LD, Rossignoli MT, Delfino-Pereira P, Garcia-Cairasco N, de Lima Umeoka EH. A Comprehensive Overview on Stress Neurobiology: Basic Concepts and Clinical Implications. Front Behav Neurosci. 2018;12:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 432] [Cited by in RCA: 446] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 19. | Dahlquist G. Can we slow the rising incidence of childhood-onset autoimmune diabetes? Diabetologia. 2006;49:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 125] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Ludvigsson J. Why diabetes incidence increases--a unifying theory. Ann N Y Acad Sci. 2006;1079:374-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Drobnič Radobuljac M, Shmueli-Goetz Y. Attachment to Caregivers and Type 1 Diabetes in Children. Zdr Varst. 2015;54:126-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Sepa A, Frodi A, Ludvigsson J. Mothers' attachment insecurity and diabetes-related autoantibodies in their infants. Ann N Y Acad Sci. 2004;1037:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Schore AN. Attachment and the regulation of the right brain. Attach Hum Dev. 2000;2:23-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 205] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 24. | Turin A, Dovč K, Klemenčič S, Bratina N, Battelino T, Lipovšek JK, Uršič K, Shmueli-Goetz Y, Drobnič-Radobuljac M. Carer's Attachment Anxiety, Stressful Life-Events and the Risk of Childhood-Onset Type 1 Diabetes. Front Psychiatry. 2021;12:657982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (2)] |
| 25. | Helgeson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: a 4-year longitudinal study. J Pediatr Psychol. 2009;34:254-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 165] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 26. | Rosenberg T, Shields CG. The role of parent-adolescent attachment in the glycemic control of adolescents with Type 1 diabetes: a pilot study. Fam Syst Health. 2009;27:237-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Ciechanowski PS, Hirsch IB, Katon WJ. Interpersonal predictors of HbA(1c) in patients with type 1 diabetes. Diabetes Care. 2002;25:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Costa-Cordella S, Luyten P, Giraudo F, Mena F, Shmueli-Goetz Y, Fonagy P. Attachment and stress in children with type 1 Diabetes and their mothers. Rev Chil Pediatr. 2020;91:68-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Grey M. Coping and Psychosocial Adjustment in Mothers of Young Children with Type 1 Diabetes. Child Health Care. 2009;38:91-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Şişmanlar ŞG, Demirbaş-Çakir E, Karakaya I, Çizmecioğlu F, Yavuz CI, Hatun Ş, Ağaoğlu B. Posttraumatic stress symptoms in children diagnosed with type 1 diabetes. Ital J Pediatr. 2012;38:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Piazza-Waggoner C, Modi AC, Powers SW, Williams LB, Dolan LM, Patton SR. Observational assessment of family functioning in families with children who have type 1 diabetes mellitus. J Dev Behav Pediatr. 2008;29:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Lewin AB, Heidgerken AD, Geffken GR, Williams LB, Storch EA, Gelfand KM, Silverstein JH. The relation between family factors and metabolic control: the role of diabetes adherence. J Pediatr Psychol. 2006;31:174-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 149] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | Leonard BJ, Jang YP, Savik K, Plumbo MA. Adolescents with type 1 diabetes: family functioning and metabolic control. J Fam Nurs. 2005;11:102-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Pedersen MAM, Kristensen LJ, Sildorf SM, Kreiner S, Svensson J, Mose AH, Thastum M, Birkebaek N. Assessment of family functioning in families with a child diagnosed with type 1 diabetes: Validation and clinical relevance of the general functioning subscale of the McMaster family assessment device. Pediatr Diabetes. 2019;20:785-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Tsiouli E, Alexopoulos EC, Stefanaki C, Darviri C, Chrousos GP. Effects of diabetes-related family stress on glycemic control in young patients with type 1 diabetes: Systematic review. Can Fam Physician. 2013;59:143-149. [PubMed] |
| 36. | Luo D, Xu JJ, Cai X, Zhu M, Wang H, Yan D, Li MZ. The effects of family functioning and resilience on self-management and glycaemic control among youth with type 1 diabetes. J Clin Nurs. 2019;28:4478-4487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 37. | Cameron FJ, Skinner TC, de Beaufort CE, Hoey H, Swift PG, Aanstoot H, Aman J, Martul P, Chiarelli F, Daneman D, Danne T, Dorchy H, Kaprio EA, Kaufman F, Kocova M, Mortensen HB, Njølstad PR, Phillip M, Robertson KJ, Schoenle EJ, Urakami T, Vanelli M, Ackermann RW, Skovlund SE; Hvidoere Study Group on Childhood Diabetes. Are family factors universally related to metabolic outcomes in adolescents with Type 1 diabetes? Diabet Med. 2008;25:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 38. | Burroughs TE, Harris MA, Pontious SL, Santiago JV. Research on social support in adolescents with IDDM: a critical review. Diabetes Educ. 1997;23:438-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 39. | Jacobson AM, Hauser ST, Lavori P, Willett JB, Cole CF, Wolfsdorf JI, Dumont RH, Wertlieb D. Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosom Med. 1994;56:401-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 114] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 40. | Marteau TM, Bloch S, Baum JD. Family life and diabetic control. J Child Psychol Psychiatry. 1987;28:823-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Anderson BJ, Miller JP, Auslander WF, Santiago JV. Family characteristics of diabetic adolescents: relationship to metabolic control. Diabetes Care. 1981;4:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 164] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 42. | Lawler MK, Volk R, Viviani N, Mengel MB. Individual and family factors impacting diabetic control in the adolescent: a preliminary study. Matern Child Nurs J. 1990;19:331-345. [PubMed] |
| 43. | Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. J Adolesc Health. 2013;52:28-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 177] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 44. | Vaid E, Lansing AH, Stanger C. Problems With Self-Regulation, Family Conflict, and Glycemic Control in Adolescents Experiencing Challenges With Managing Type 1 Diabetes. J Pediatr Psychol. 2018;43:525-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Rybak TM, Ali JS, Berlin KS, Klages KL, Banks GG, Kamody RC, Ferry RJ, Alemzadeh R, Diaz-Thomas AM; Guest Editors: Cynthia A. Gerhardt, Cynthia A. Berg, Deborah J. Wiebe and Grayson N. Holmbeck. Patterns of Family Functioning and Diabetes-Specific Conflict in Relation to Glycemic Control and Health-Related Quality of Life Among Youth With Type 1 Diabetes. J Pediatr Psychol. 2017;42:40-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 46. | Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LM. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabet Med. 2002;19:635-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 233] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 47. | Drotar D, Ittenbach R, Rohan JM, Gupta R, Pendley JS, Delamater A. Diabetes management and glycemic control in youth with type 1 diabetes: test of a predictive model. J Behav Med. 2013;36:234-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 48. | Kovacs M, Kass RE, Schnell TM, Goldston D, Marsh J. Family functioning and metabolic control of school-aged children with IDDM. Diabetes Care. 1989;12:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Gowers SG, Jones JC, Kiana S, North CD, Price DA. Family functioning: a correlate of diabetic control? J Child Psychol Psychiatry. 1995;36:993-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Garrison WT, Biggs D, Williams K. Temperament characteristics and clinical outcomes in young children with diabetes mellitus. J Child Psychol Psychiatry. 1990;31:1079-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22:405-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 271] [Cited by in RCA: 239] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 52. | Daneman D, Hamilton J. Is poor metabolic control inevitable in adolescents with type 1 diabetes? An Pediatr. 2001;54:40-44. |
| 53. | Demirel F, Tepe D, Esen I, Buber N, Boztepe H. Individual and familial factors associated with metabolic control in children with type 1 diabetes. Pediatr Int. 2013;55:710-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 54. | Urbach SL, LaFranchi S, Lambert L, Lapidus JA, Daneman D, Becker TM. Predictors of glucose control in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2005;6:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 55. | La Greca AM. It's "all in the family": responsibility for diabetes care. J Pediatr Endocrinol Metab. 1998;11 Suppl 2:379-385. [PubMed] |
| 56. | Berg CA, King PS, Butler JM, Pham P, Palmer D, Wiebe DJ. Parental involvement and adolescents' diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. J Pediatr Psychol. 2011;36:329-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 57. | Horton D, Berg CA, Butner J, Wiebe DJ. The role of parental monitoring in metabolic control: effect on adherence and externalizing behaviors during adolescence. J Pediatr Psychol. 2009;34:1008-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2016;70:70-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 296] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 59. | Butwicka A, Frisén L, Almqvist C, Zethelius B, Lichtenstein P. Risks of psychiatric disorders and suicide attempts in children and adolescents with type 1 diabetes: a population-based cohort study. Diabetes Care. 2015;38:453-459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 60. | Dybdal D, Tolstrup JS, Sildorf SM, Boisen KA, Svensson J, Skovgaard AM, Teilmann GK. Increasing risk of psychiatric morbidity after childhood onset type 1 diabetes: a population-based cohort study. Diabetologia. 2018;61:831-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 61. | Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. BMJ. 2000;320:1563-1566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 318] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 62. | Blanz BJ, Rensch-Riemann BS, Fritz-Sigmund DI, Schmidt MH. IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care. 1993;16:1579-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 95] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 63. | Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: rates and risk factors. Diabetes Care. 1997;20:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 234] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 64. | Hannonen R, Eklund K, Tolvanen A, Komulainen J, Riikonen R, Delamater AM, Ahonen T. Psychological distress of children with early-onset type 1 diabetes and their mothers' well-being. Acta Paediatr. 2015;104:1144-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 65. | Sendela J, Zduńczyk B, Trippenbach-Dulska H, Szypowska A. Prevalence of depressive symptoms in school aged children with type 1 diabetes - a questionnaire study. Psychiatr Pol. 2015;49:1005-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 66. | Peveler RC, Fairburn CG, Boller I, Dunger D. Eating disorders in adolescents with IDDM. A controlled study. Diabetes Care. 1992;15:1356-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 93] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 67. | Sivertsen B, Petrie KJ, Wilhelmsen-Langeland A, Hysing M. Mental health in adolescents with Type 1 diabetes: results from a large population-based study. BMC Endocr Disord. 2014;14:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 68. | Telo GH, Cureau FV, Lopes CS, Schaan BD. Common mental disorders in adolescents with and without type 1 diabetes: Reported occurrence from a countrywide survey. Diabetes Res Clin Pract. 2018;135:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 69. | Striegel-Moore RH, Nicholson TJ, Tamborlane WV. Prevalence of eating disorder symptoms in preadolescent and adolescent girls with IDDM. Diabetes Care. 1992;15:1361-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 70. | Radobuljac MD, Bratina NU, Battelino T, Tomori M. Lifetime prevalence of suicidal and self-injurious behaviors in a representative cohort of Slovenian adolescents with type 1 diabetes. Pediatr Diabetes. 2009;10:424-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 71. | Radobuljac MD, Tomori M, Battelino T, Bratina N. Adolescent Risk Behavior is Less Frequent in Patients with Type 1 Diabetes. J Diabetes Metab. 2013;S12:007. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 72. | Sildorf SM, Breinegaard N, Lindkvist EB, Tolstrup JS, Boisen KA, Teilmann GK, Skovgaard AM, Svensson J. Poor Metabolic Control in Children and Adolescents With Type 1 Diabetes and Psychiatric Comorbidity. Diabetes Care. 2018;41:2289-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 73. | Young V, Eiser C, Johnson B, Brierley S, Epton T, Elliott J, Heller S. Eating problems in adolescents with Type 1 diabetes: a systematic review with meta-analysis. Diabet Med. 2013;30:189-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 251] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 74. | Northam EA, Matthews LK, Anderson PJ, Cameron FJ, Werther GA. Psychiatric morbidity and health outcome in Type 1 diabetes--perspectives from a prospective longitudinal study. Diabet Med. 2005;22:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 75. | Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, Soren K. Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr (Phila). 2013;52:10-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 159] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 76. | Kovacs M, Mukerji P, Iyengar S, Drash A. Psychiatric disorder and metabolic control among youths with IDDM. A longitudinal study. Diabetes Care. 1996;19:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 77. | Eaton WW, Mengel M, Mengel L, Larson D, Campbell R, Montague RB. Psychosocial and psychopathologic influences on management and control of insulin-dependent diabetes. Int J Psychiatry Med. 1992;22:105-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 78. | Colton PA, Olmsted MP, Daneman D, Rodin GM. Depression, disturbed eating behavior, and metabolic control in teenage girls with type 1 diabetes. Pediatr Diabetes. 2013;14:372-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 79. | Engström I, Kroon M, Arvidsson CG, Segnestam K, Snellman K, Aman J. Eating disorders in adolescent girls with insulin-dependent diabetes mellitus: a population-based case-control study. Acta Paediatr. 1999;88:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 80. | Liu S, Kuja-Halkola R, Larsson H, Lichtenstein P, Ludvigsson JF, Svensson AM, Gudbjörnsdottir S, Tideman M, Serlachius E, Butwicka A. Poor glycaemic control is associated with increased risk of neurodevelopmental disorders in childhood-onset type 1 diabetes: a population-based cohort study. Diabetologia. 2021;64:767-777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 81. | Nylander C, Lindström K, Khalifa N, Fernell E. Previously undiagnosed attention-deficit/hyperactivity disorder associated with poor metabolic control in adolescents with type 1 diabetes. Pediatr Diabetes. 2018;19:816-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 82. | Macek J, Battelino T, Bizjak M, Zupanc C, Bograf AK, Vesnic S, Klemencic S, Volk E, Bratina N. Impact of attention deficit hyperactivity disorder on metabolic control in adolescents with type1 diabetes. J Psychosom Res. 2019;126:109816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 83. | Rechenberg K, Grey M, Sadler L. Stress and Posttraumatic Stress in Mothers of Children With Type 1 Diabetes. J Fam Nurs. 2017;23:201-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 84. | Schiaffini R, Carducci C, Cianfarani S, Mauti M, Nicolais G. Post-traumatic Stress Disorder in Children Affected by Type 1 Diabetes and Their Parents. SN Compr Clin Med. 2019;1:349-353. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 85. | Bassi G, Mancinelli E, Di Riso D, Salcuni S. Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review. Int J Environ Res Public Health. 2020;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 86. | Rumburg TM, Lord JH, Savin KL, Jaser SS. Maternal diabetes distress is linked to maternal depressive symptoms and adolescents' glycemic control. Pediatr Diabetes. 2017;18:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 87. | Landolt MA, Ribi K, Laimbacher J, Vollrath M, Gnehm HE, Sennhauser FH. Posttraumatic stress disorder in parents of children with newly diagnosed type 1 diabetes. J Pediatr Psychol. 2002;27:647-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 79] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 88. | Viaene AS, Van Daele T, Bleys D, Faust K, Massa GG. Fear of Hypoglycemia, Parenting Stress, and Metabolic Control for Children with Type 1 Diabetes and Their Parents. J Clin Psychol Med Settings. 2017;24:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 89. | Driscoll KA, Raymond J, Naranjo D, Patton SR. Fear of Hypoglycemia in Children and Adolescents and Their Parents with Type 1 Diabetes. Curr Diab Rep. 2016;16:77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 90. | Jaser SS, Linsky R, Grey M. Coping and psychological distress in mothers of adolescents with type 1 diabetes. Matern Child Health J. 2014;18:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 91. | Whittemore R, Jaser S, Chao A, Jang M, Grey M. Psychological experience of parents of children with type 1 diabetes: a systematic mixed-studies review. Diabetes Educ. 2012;38:562-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 271] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 92. | Stallwood L. Influence of caregiver stress and coping on glycemic control of young children with diabetes. J Pediatr Health Care. 2005;19:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |