Copyright
©2014 Baishideng Publishing Group Co.
World J Diabetes. Apr 15, 2014; 5(2): 128-140
Published online Apr 15, 2014. doi: 10.4239/wjd.v5.i2.128
Published online Apr 15, 2014. doi: 10.4239/wjd.v5.i2.128
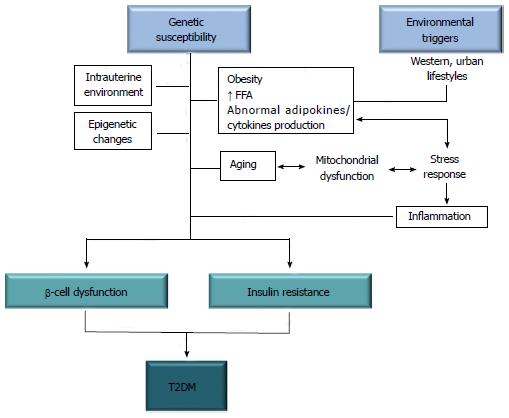
Figure 1 Overview of the pathogenic factors underlying development of type 2 diabetes mellitus.
As a complex disease, T2DM is caused by a combination of genetic, environmental and lifestyle factors, all of which interact together to produce insulin resistance and β-cell dysfunction, leading to hyperglycemia, which is the clinical hallmark of diabetes. FFA: Free fatty acids.T2DM: Type 2 diabetes mellitus.
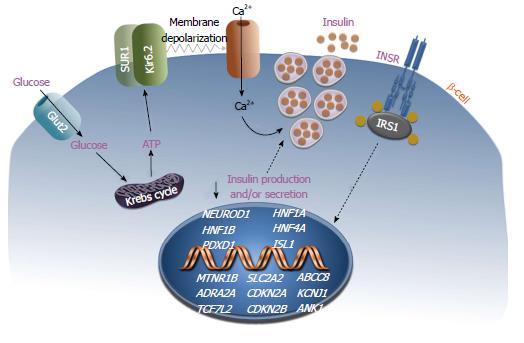
Figure 2 Schematic representation of the pancreatic β-cell.
Reduced insulin secretion is shown in β-cells with gene variants linked to T2DM. Genes associated with defects in β-cell mass and/or function are indicated in white italic uppercase. T2DM: Type 2 diabetes mellitus.
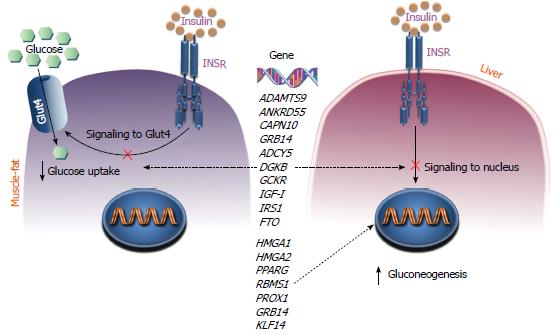
Figure 3 Mechanisms of insulin resistance.
The figure shows the mechanisms by which gene variants may impair insulin action in the insulin target tissues muscle, fat and liver. Peripheral insulin resistance in muscle and fat reduces cellular glucose uptake, whereas insulin resistance in liver results in a failure to suppress glucose production and gluconeogenesis. Genes whose variations can influence the risk of developing insulin resistance and T2DM are indicated in black italic uppercase. T2DM: Type 2 diabetes mellitus.
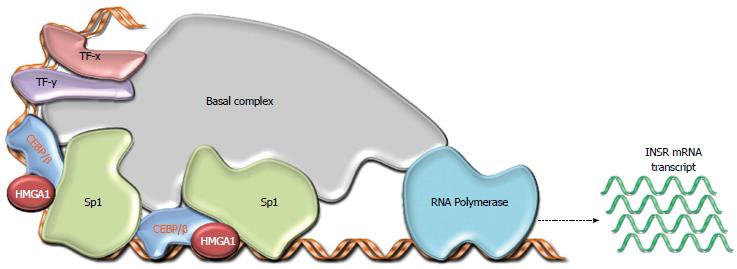
Figure 4 Model for the role of High Mobility Group A1 in type 2 diabetes mellitus.
As a transcriptional regulator of the INSR gene, HMGA1 gene variants may lead to decreased INSR gene transcription. This loss of insulin receptor (INSR) underlies the resultant insulin resistance and T2D in affected individuals. T2D: Type 2 diabetes.
- Citation: Brunetti A, Chiefari E, Foti D. Recent advances in the molecular genetics of type 2 diabetes mellitus. World J Diabetes 2014; 5(2): 128-140
- URL: https://www.wjgnet.com/1948-9358/full/v5/i2/128.htm
- DOI: https://dx.doi.org/10.4239/wjd.v5.i2.128