Copyright
©2013 Baishideng Publishing Group Co.
World J Diabetes. Apr 15, 2013; 4(2): 19-26
Published online Apr 15, 2013. doi: 10.4239/wjd.v4.i2.19
Published online Apr 15, 2013. doi: 10.4239/wjd.v4.i2.19
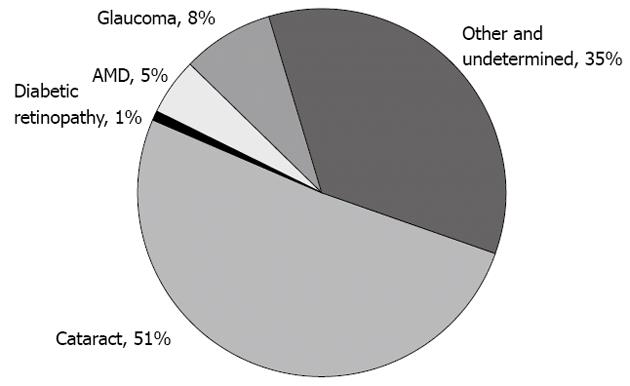
Figure 1 Pie chart displaying the distribution of global causes of blindness.
Although cataracts are responsible for more than half of the cases, they are potentially reversible. When considering the causes of permanent vision impairment, diabetic retinopathy contributes significantly to 1%-5% of cases of blindness. In addition, diabetic retinopathy is the major cause of irreversible blindness in the working-age patients worldwide. AMD: Age-related macular disease.
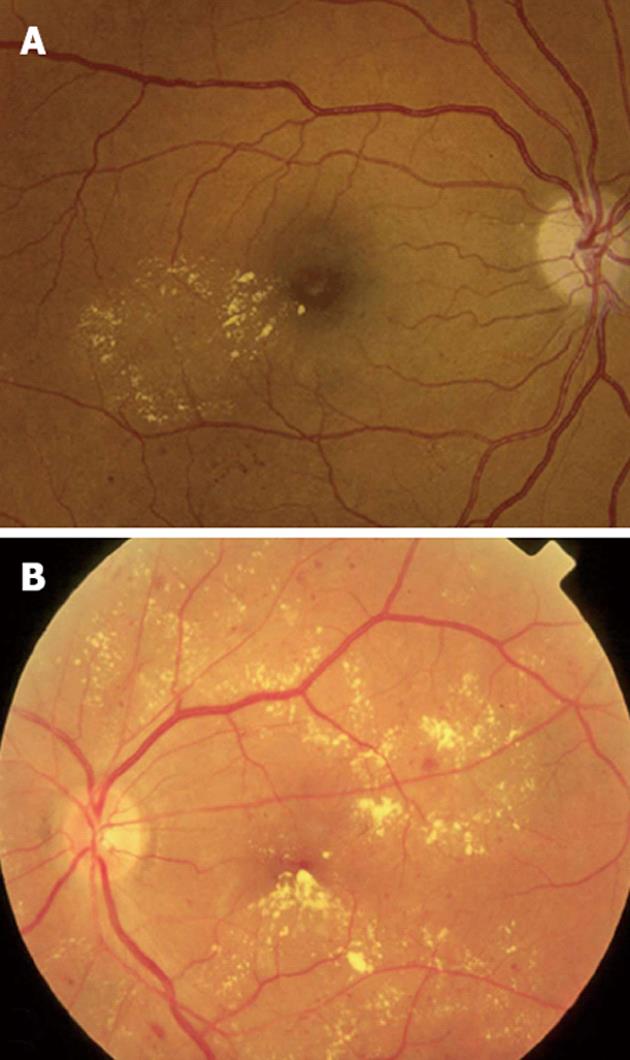
Figure 2 Clinical patterns of diabetic macular edema.
A: Focal macular edema marked by focal leakage from microaneurysms and dilated retinal capillaries with abnormal permeability, making a complete ring as a localized circinate pattern of hard exudates; B: Diffuse macular edema, characterized by hard exudates with generalized leakage from dilated capillaries throughout the posterior pole.
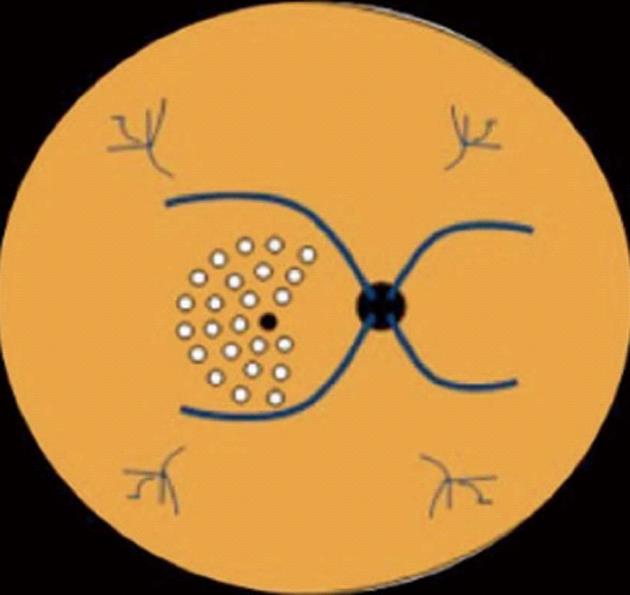
Figure 3 Macular area treated by laser photocoagulation using the scheme proposed by the Early Treatment Diabetic Retinopathy Study.
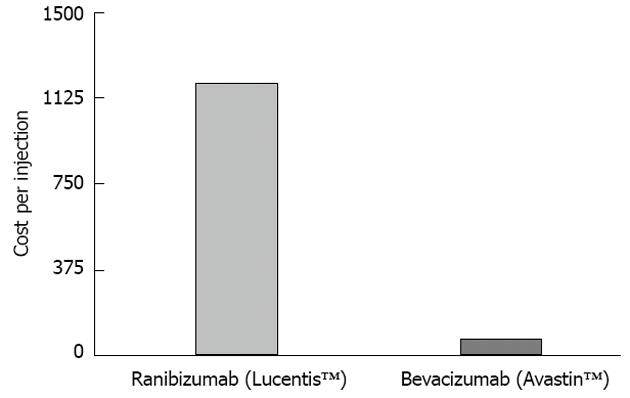
Figure 4 Cost per injection of ranibizumab (LucentisTM Genentech, United States), in the treatment of diabetic macular edema, compared with the cost per injection of bevacizumab (Avastin, Roche, United States).
The cost is, in average, 20-fold higher in for treatment with ranibizumab than bevacizumab. Depending on the country, this difference may vary from 20× to 50×.
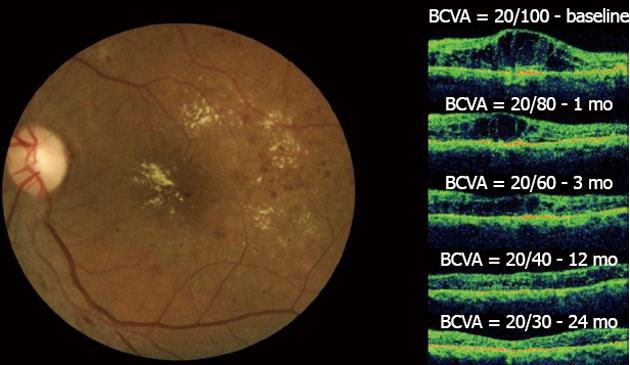
Figure 5 Diffuse diabetic macular edema treated with bevacizumab.
In the left figure, the clinical fundus photograph shows the macular edema and hard exudates at the foveal center.In the right figure, a series of optical coherence tomographys (OCTs) taken at a 24-mo follow-up can be observed. The OCT image at baseline shows the intraretinal fluid with increased central macular thickness (CMT) and best-corrected visual acuity (BCVA) = 20/100. One month after the first injection, improvement in both BCVA and CMT was observed. This result was maintained throughout the 24-mo follow-up period after six injections and with final central macular thickness within normal limits without intraretinal fluid and the improvement of BCVA to 20/30. No laser photocoagulation was performed in this case.
- Citation: Stefanini FR, Arevalo JF, Maia M. Bevacizumab for the management of diabetic macular edema. World J Diabetes 2013; 4(2): 19-26
- URL: https://www.wjgnet.com/1948-9358/full/v4/i2/19.htm
- DOI: https://dx.doi.org/10.4239/wjd.v4.i2.19