Copyright
©The Author(s) 2023.
World J Diabetes. Jun 15, 2023; 14(6): 680-704
Published online Jun 15, 2023. doi: 10.4239/wjd.v14.i6.680
Published online Jun 15, 2023. doi: 10.4239/wjd.v14.i6.680
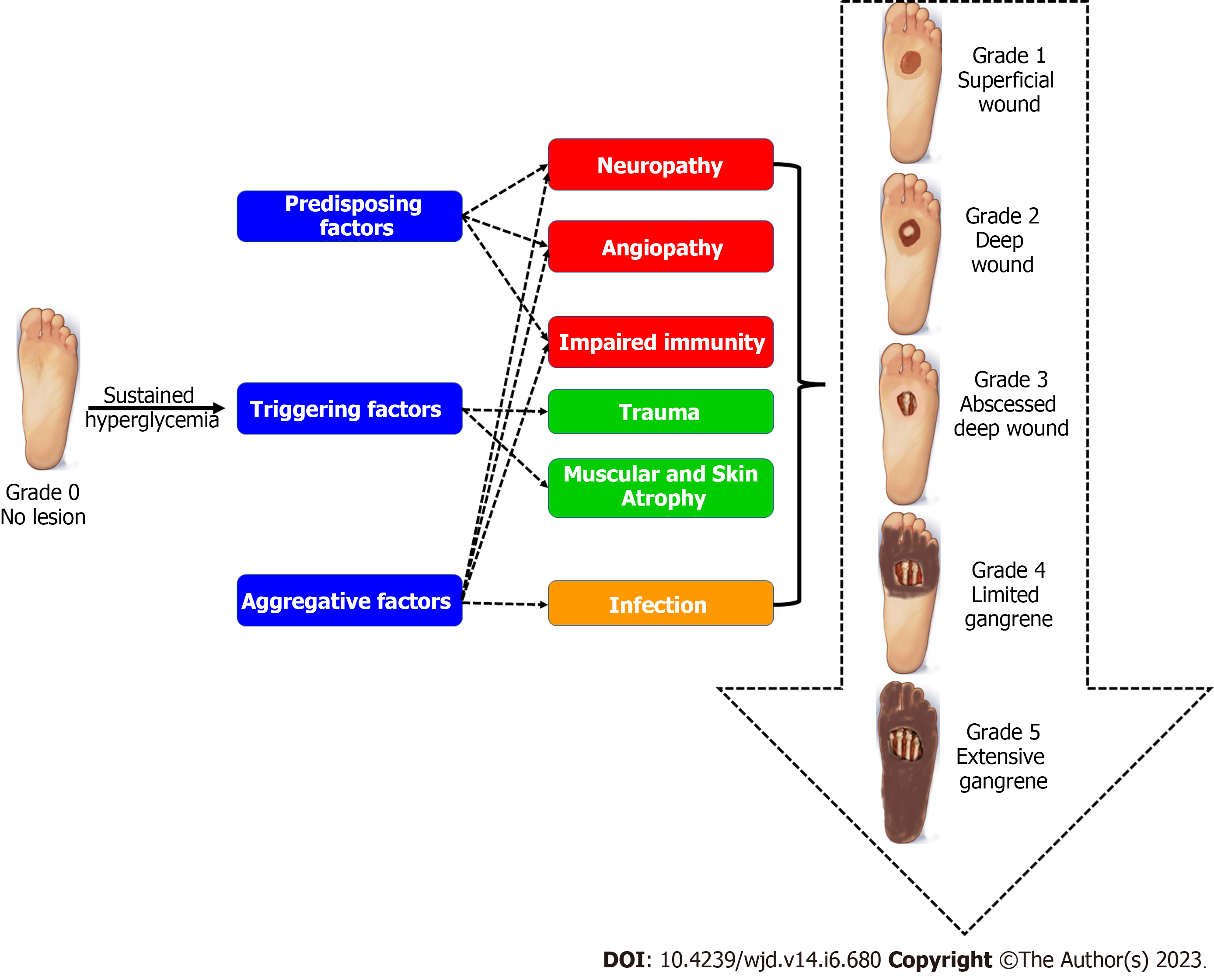
Figure 1 Risk factors for the development of diabetic foot infections.
Angiopathy and neuropathy are the main predisposing factors of diabetic foot infections (DFIs), together with muscular atrophy and extrinsic triggers, such as trauma, in the presence of abnormal immunity and ischemia as aggravating factors. These factors collectively result in the loss of skin integrity favoring the development of DFIs. The Meggitt-Wagner classification is commonly used to grade the DFIs (from 1 to 5) on three characteristics: the depth of ulcer; the degree of infection; and the necrosis.
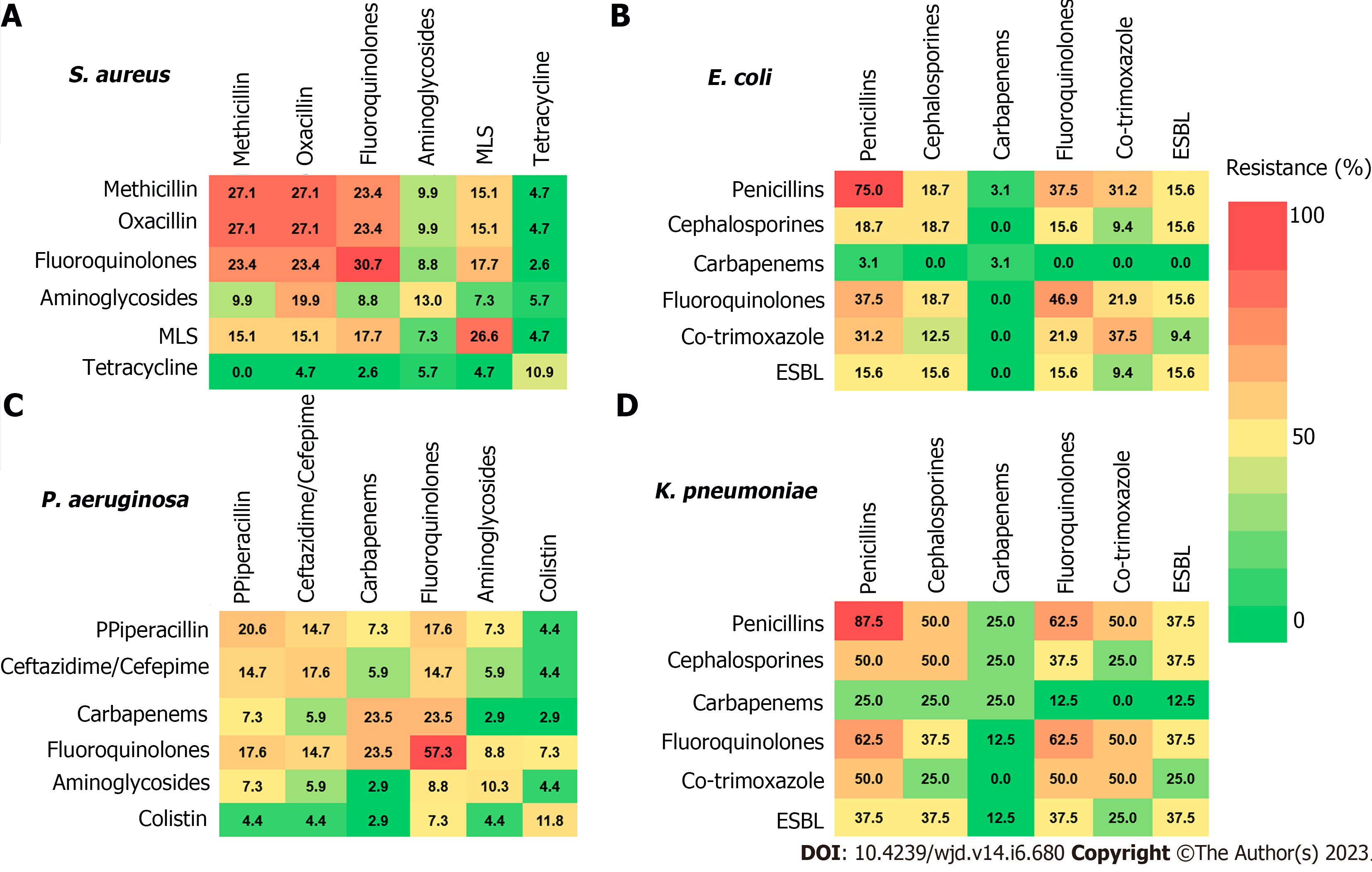
Figure 2 Resistance of bacteria isolated from diabetic foot infections to different classes of antibiotics as monotherapy or in combinations.
A: Staphylococcus aureus (S. aureus); B: Escherichia coli (E. coli); C: Pseudomonas aeruginosa (P. aeruginosa); D: Klebsiella pneumonia (K. pneumonia). The data presented as percentages of resistance, adopted from Boschetti et al[84]. Resistance to oxacillin expects resistance to cephalosporines, carbapenems, and β-lactams. MLS: Macrolides, lincosamides, and streptogramines; ESBL: Extended spectrum beta-lactamases.
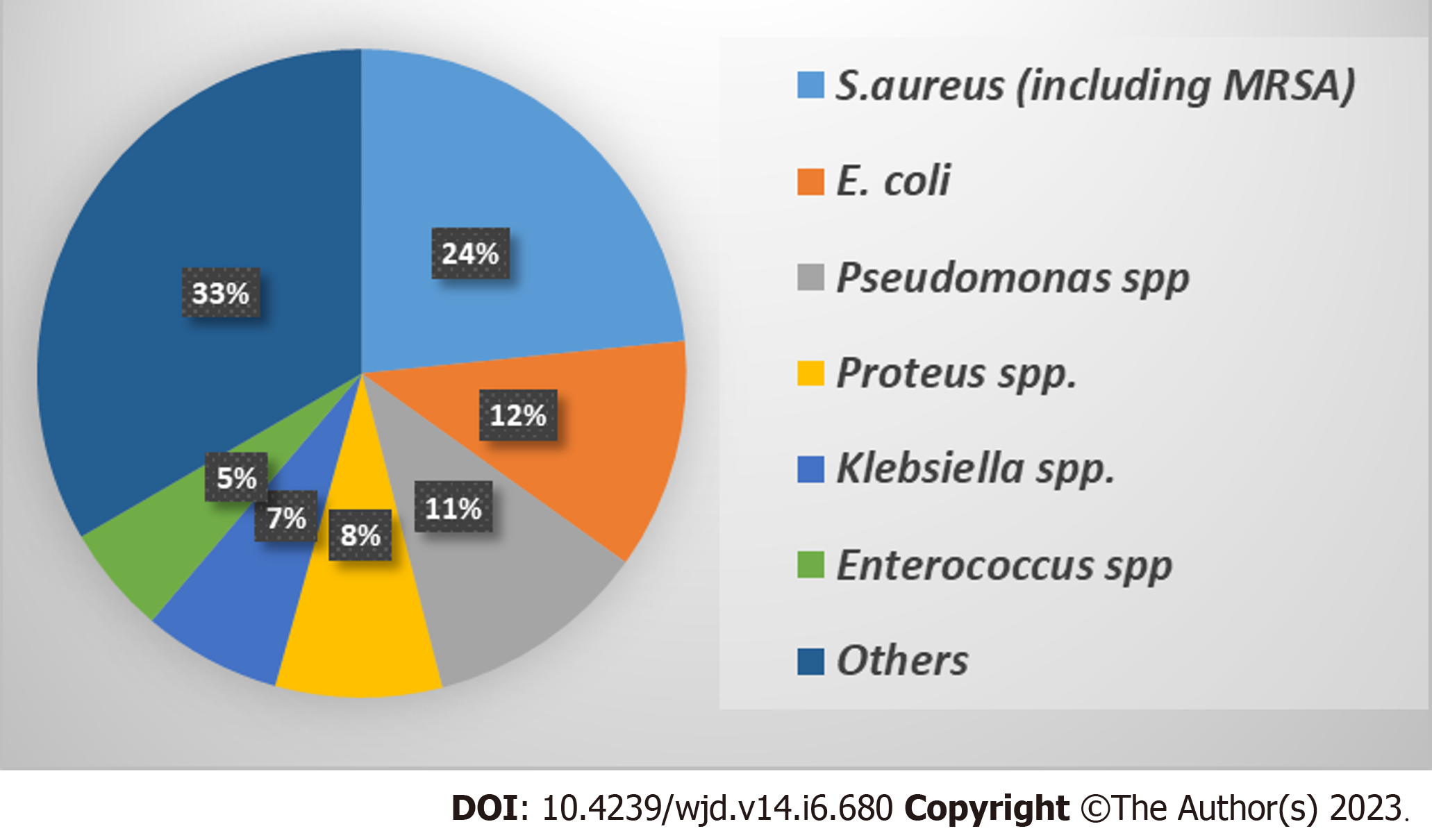
Figure 3 Frequency of isolated bacterial species from diabetic foot infections.
The presented data were collected from 57 studies that represented 6736 clinical samples, yielding 8418 microbial isolates[96]. S. aureus: Staphylococcus aureus; E. coli: Escherichia coli; MRSA: Methicillin-resistant Staphylococcus aureus.
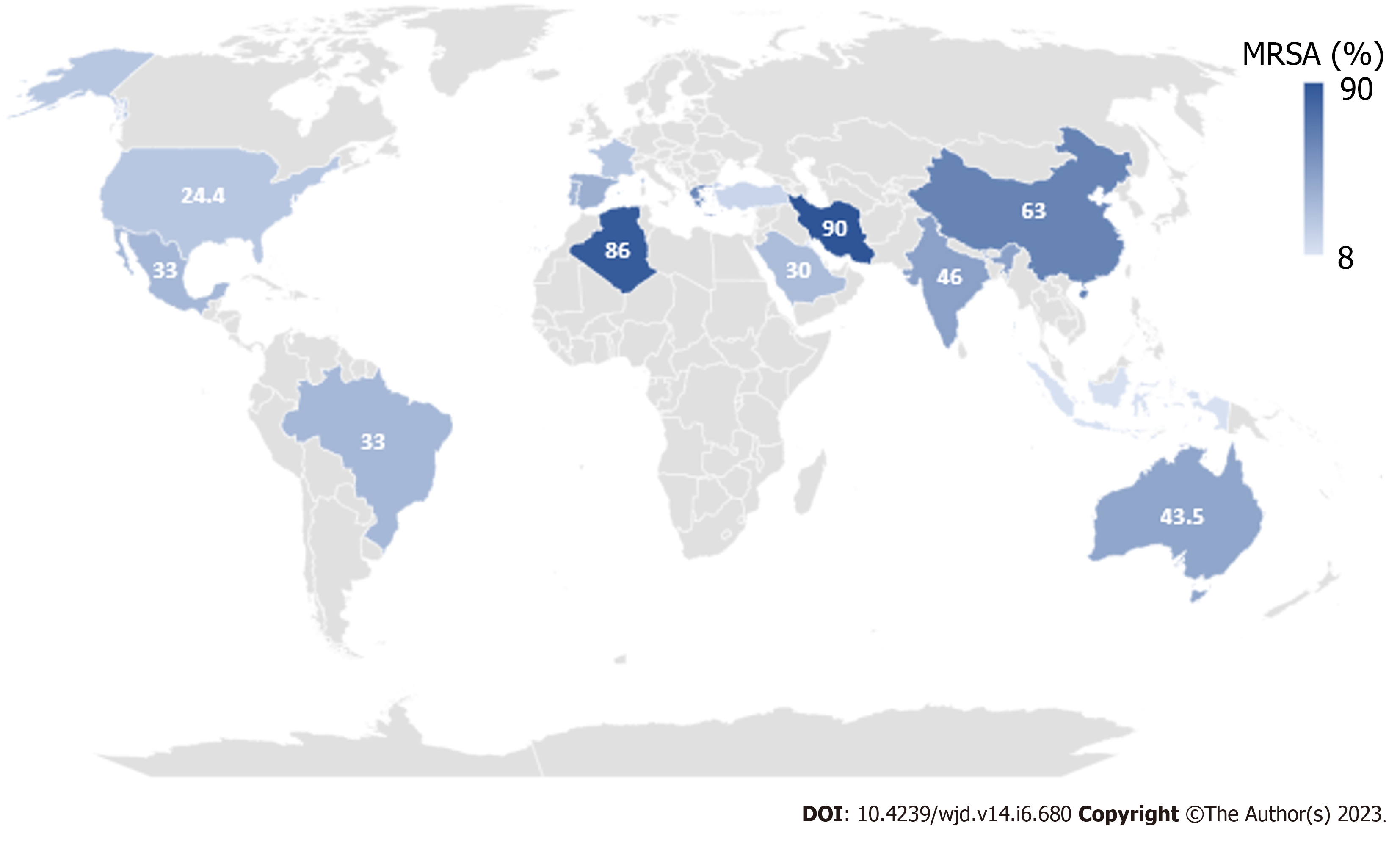
Figure 4 Prevalence of methicillin resistant Staphylococcusaureus isolated from diabetic foot infections around the world.
The presented data are percentage of methicillin resistant Staphylococcus aureus (S. aureus) from the isolated S. aureus from diabetic foot infections.
- Citation: Rajab AAH, Hegazy WAH. What’s old is new again: Insights into diabetic foot microbiome. World J Diabetes 2023; 14(6): 680-704
- URL: https://www.wjgnet.com/1948-9358/full/v14/i6/680.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i6.680