Published online Oct 15, 2017. doi: 10.4251/wjgo.v9.i10.431
Peer-review started: February 23, 2017
First decision: May 7, 2017
Revised: May 30, 2017
Accepted: July 14, 2017
Article in press: July 17, 2017
Published online: October 15, 2017
Processing time: 233 Days and 21.4 Hours
Primary non-Hodgkin lymphomas in the esophagus are rare. Tracheoesophageal fistulas mainly arise from solid esophageal carcinoma or mediastinal malignancies. Our patient presented with cough, dysphagia and weight loss, and upon initial computed tomography imaging and esophagogastroduodenoscopy, a malignant mass in the middle third of esophagus with tracheoesophageal fistula was found. The location of the mass and presence of malignant tracheoesophageal fistula were strongly suggestive of squamous cell carcinoma. However, tumor biopsy revealed diffuse large B-cell lymphoma. This case report details a rare incident of a primary diffuse large B-cell lymphoma presented as tracheoesophageal fistula and reviews previous literature.
Core tip: Primary non-Hodgkin lymphoma of esophagus is a rare disease, and tracheoesophageal fistula secondary to this condition prior to treatment is extremely rare and fatal. However, it has better prognosis than fistulas secondary to solid tumor if patients receive timely treatment.
- Citation: Teerakanok J, DeWitt JP, Juarez E, Thein KZ, Warraich I. Primary esophageal diffuse large B cell lymphoma presenting with tracheoesophageal fistula: A rare case and review. World J Gastrointest Oncol 2017; 9(10): 431-435
- URL: https://www.wjgnet.com/1948-5204/full/v9/i10/431.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v9.i10.431
Lymphomas, the most common blood cancers, are characterized by proliferation of lymphocytes in the lymph nodes and of lymphoid tissue[1,2]. Lymphomas are categorized into two groups: Hodgkin and non-Hodgkin lymphomas (NHLs). Among NHLs, diffuse large B-cell lymphomas (DLBCLs) account for 40% of all lymphoma cases worldwide[3]. Primary gastrointestinal (GI) lymphoma is the most common extranodal presentation NHL; however, most cases involve the stomach, small intestine and colon. Esophageal involvement is the rarest. Malignant tracheoesophageal fistula (TEF) from NHL is uncommon and presents mostly as complication of radiation therapy or chemotherapy.
Here, we present a rare case of a primary esophageal NHL presented with malignant TEF. To the best of our knowledge, this is the first case of primary DLBCL with malignant TEF prior to cancer treatment.
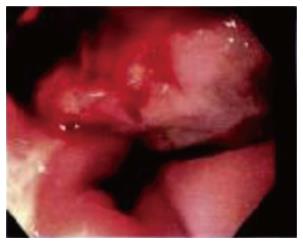
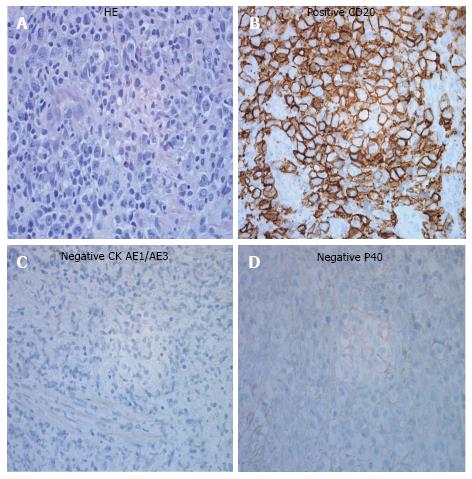
A 60-year-old male with past medical history of diabetes mellitus type 2, hypothyroidism and chronic tobacco smoking presented with gradually worsening 3-wk dry cough, dysphagia and cough provoked with all oral intake. On review of systems, patient had unintentional 30-pound weight loss in the past 3 mo. On physical exam vital signs were unremarkable except for oxygen saturation of 91% on room air with respiratory rate of 18 breaths per minute. Moreover, the patient was not in acute distress; his breathing was non-labored; liver and spleen were not palpable; superficial lymphadenopathy was not found. The initial CBC revealed a white blood cell count of 21900/μL, 5% bands, 81% segmented neutrophils, 5% lymphocyte, and 8% monocytes. Lactate dehydrogenase was 223 units/L (normal value; 135-225 units/L), liver functions and renal functions were unremarkable and human immunodeficiency virus (HIV) was negative. A chest computed tomography (CT) imaging revealed a mid-esophageal wall thickening and enhancement, a fistulous connection between the membranous portion of the trachea and the anterior portion of the mediastinum, nonspecific mediastinal lymph nodes enlargement and some of ground glass opacity in posterior segment of the upper lobes and superior segments of the lower lobes bilaterally (Figure 1). Abdominal and pelvic CT imaging revealed multiple lytic lesions in pelvic bone, mild hepatic steatosis, normal spleen and no intraabdominal or pelvic lymphadenopathy. Our patient was started on levofloxacin for concern of aspiration pneumonia. Esophagogastroduodenoscopy (EGD) found a large fungating and ulcerating mass in the middle third of the esophagus with partial obstruction, and TEF was found in the middle third of the esophagus with tracheal rings (Figure 2). Bronchoscopy revealed 3 cm TEF in the trachea and 1.5 cm bronchoesophageal fistula in left mainstem. The esophageal mass biopsy showed large, highly pleomorphic cells with diffuse growth pattern (Figure 3A). Various immunohistochemical staining were performed. Tumor cells had strong and diffuse expression for CD20 (Figure 3B), CD10, CD45, CD79a and bcl2. CD 3 and CD5 were negative. Cytokeratin (CK) AE1/AE3 was negative for the cells of tumor infiltrate (Figure 3C). Tumor cells did not show any expression for P40, a marker for squamous cell carcinoma (Figure 3D). These findings were consistent with diffuse large B-cell lymphoma diagnosis. Bone marrow biopsy was not performed because CT imaging suggested bone marrow involvement. Lumbar puncture was not done as well. Patient underwent for percutaneous endoscopic gastrostomy tube placement, esophageal stent placement and tracheobronchial stent placement. He received rituximab 375 mg/m2 for 1 dose, and a week later he subsequently received complete first cycle of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP regimen). Patient completed 6 cycles of R-CHOP with good response in tumor but still has persistent TEF with intermittent aspiration. He lost 30 pounds during the course of treatment due to poor feeding intolerance.
GI lymphomas comprise 5%-20% of extranodal lymphomas[4] and only 1%-4% of all GI cancers[5]. Primary esophageal lymphoma accounts for less than 1% of GI lymphomas. The earliest reported primary esophageal NHL was in 1979[6]. Heretofore, there have been less than 25 reported cases of primary esophageal cancer from NHL[7-16]. Sometimes, it can be difficult to differentiate between primary GI lymphomas and lymphomas that disseminated to GI tract. Dawson et al[17] described the diagnostic criteria of primary GI lymphomas: (1) absence of peripheral lymphadenopathy; (2) absence of mediastinal adenopathy; (3) no involvement of liver and spleen; and (4) normal peripheral blood count. Majority of primary GI lymphomas are DLBCL[18]. A major risk factor for primary esophageal lymphoma is immunosuppression, such as HIV infection[19]. Radiologic features of primary esophageal lymphoma are ulceration, stenosis, polypoid masses, aneurysmal dilatation and TEF, which are non-specific[19,20].
Malignant TEF is a serious late complication of cancers. Most malignant TEF cases are related to esophageal and lung cancers[21]. TEF from primary esophageal lymphoma is an uncommon complication. TEF in lymphoma frequently develops during or after treatment with radiation or chemotherapy, but it can occur due to the disease itself. Most of the reports were of Hodgkin lymphomas[22-25]. Even though literature review reveals case reports of NHL with esophageal-tracheobronchial connection, the reported NHLs are not primary esophageal NHLs[26-28]. Malignant TEF usually has very poor prognosis; however, if lymphomas are recognized and treated early, TEF repair and chemotherapy treatment will result in good prognosis[29]. Standard treatment of DLBCL is R-CHOP regimen. Management of TEF is predominantly a non-surgical intervention because of the difficulty of and risk from surgery. Esophageal stent and/or airway stent is effective to prevent aspiration of GI contents and risk of pneumonia. In addition, general treatments, such as gastrostomy/jejunostomy tube, antibiotics and airway secretion prevention help reduce further risk of aspiration[22,30].
Novelty of this case report is the co-presence of malignant TEF with primary DLBCL in the esophagus. Primary esophageal lymphoma-related TEF is extremely rare but fatal. Physicians should suspect it for timely diagnosis since NHL with TEF has better prognosis with interventions and chemotherapy alone than TEFs caused by esophageal cancer or lung cancer.
A 60-year-old man presented with worsening 3-wk dry cough, dysphagia and cough provoked with all oral intake.
Clinical examination was unremarkable.
Stroke, esophageal spasm, esophageal tumor, tracheoesophageal fistula-related or pulmonary infection.
Blood count showed leukocytosis suggested of infection or inflammation, but lactate dehydrogenase andliver function were unremarkable.
Chest, abdominal and pelvic computed tomography imaging revealed fungating and ulcerating mass in the middle third of the esophagus with partial obstructionand tracheoesophageal fistula (TEF) without significant lymphadenopathy.
Esophageal mass biopsy revealed diffuse large B-cell lymphoma.
Patient received chemotherapy R-CHOP regimen and underwent to have PEG tube placement, tracheal and esophageal stents.
Most primary esophageal lymphoma cases are the rarest among primary gastrointestinal lymphoma, and TEF is seldom found as a presenting symptom.
Tracheoesophageal fistula is an abnormal connection between the esophagus and trachea. Diffuse large B cell lymphoma is a subtype of non-Hodgkin lymphoma.
Primary esophageal lymphoma is extremely rare, and malignant TEF is fatal. However, patients with this condition have better prognosis if they receive a proper management.
This case report is very interesting and rare. It is helpful to know if the patient has been immunologically investigated. The manuscript is well written and illustrations are informative.
Manuscript source: Unsolicited Manuscript
Specialty type: Oncology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Droz JP, Gorodetskiy VR, Mihaila RG S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Perry RR, Rosenberg RK, Pass HI. Tracheoesophageal fistula in the patient with lymphoma: case report and review of the literature. Surgery. 1989;105:770-777. [PubMed] |
| 2. | Perry AM, Diebold J, Nathwani BN, MacLennan KA, Müller-Hermelink HK, Bast M, Boilesen E, Armitage JO, Weisenburger DD. Non-Hodgkin lymphoma in the developing world: review of 4539 cases from the International Non-Hodgkin Lymphoma Classification Project. Haematologica. 2016;101:1244-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 122] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 3. | Caimi PF, Hill BT, Hsi ED, Smith MR. Clinical approach to diffuse large B cell lymphoma. Blood Rev. 2016;30:477-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252-260. [PubMed] |
| 5. | Gurney KA, Cartwright RA. Increasing incidence and descriptive epidemiology of extranodal non-Hodgkin lymphoma in parts of England and Wales. Hematol J. 2002;3:95-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Berman MD, Falchuk KR, Trey C, Gramm HF. Primary histiocytic lymphoma of the esophagus. Dig Dis Sci. 1979;24:883-886. [PubMed] |
| 7. | Chadha KS, Hernandez-Ilizaliturri FJ, Javle M. Primary esophageal lymphoma: case series and review of the literature. Dig Dis Sci. 2006;51:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Doki T, Hamada S, Murayama H, Suenaga H, Sannohe Y. Primary malignant lymphoma of the esophagus. A case report. Endoscopy. 1984;16:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Ghimire P, Wu GY, Zhu L. Primary esophageal lymphoma in immunocompetent patients: Two case reports and literature review. World J Radiol. 2010;2:334-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Gupta NM, Goenka MK, Jindal A, Behera A, Vaiphei K. Primary lymphoma of the esophagus. J Clin Gastroenterol. 1996;23:203-206. [PubMed] |
| 11. | Kim Jh, Jung Yh, Woo IS, Ha SY. Two Cases of Primary Esophageal Diffuse Large B Cell Lymphoma: Therapeutic Considerations and a Literature Review. Korean J Med. 2015;88:224-230. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Matsuura H, Saito R, Nakajima S, Yoshihara W, Enomoto T. Non-Hodgkin’s lymphoma of the esophagus. Am J Gastroenterol. 1985;80:941-946. [PubMed] |
| 13. | Mengoli M, Marchi M, Rota E, Bertolotti M, Gollini C, Signorelli S. Primary non-Hodgkin’s lymphoma of the esophagus. Am J Gastroenterol. 1990;85:737-741. [PubMed] |
| 14. | Sabljak P, Stojakov D, Bjelovic M, Mihaljevic B, Velickovic D, Ebrahimi K, Spica B, Pesko P. Primary esophageal diffuse large B-cell lymphoma: report of a case. Surg Today. 2008;38:647-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Tsukada T, Ohno T, Kihira H, Taniguchi M, Takahashi T, Arima S, Yamada H, Akasaka Y, Yokoi H, Kita K. Primary esophageal non-Hodgkin’s lymphoma. Intern Med. 1992;31:569-572. [PubMed] |
| 16. | Ximenes M, Piauilino MA, Oliveira HA, Vaz Neto JP. [Primary esophageal lymphoma]. Rev Col Bras Cir. 2012;39:243-246. [PubMed] |
| 17. | Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80-89. [PubMed] |
| 18. | Howell JM, Auer-Grzesiak I, Zhang J, Andrews CN, Stewart D, Urbanski SJ. Increasing incidence rates, distribution and histological characteristics of primary gastrointestinal non-Hodgkin lymphoma in a North American population. Can J Gastroenterol. 2012;26:452-456. [PubMed] |
| 19. | Tirumani H, Rosenthal MH, Tirumani SH, Shinagare AB, Krajewski KM, Ramaiya NH. Imaging of uncommon esophageal malignancies. Dis Esophagus. 2015;28:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Carnovale RL, Goldstein HM, Zornoza J, Dodd GD. Radiologic manifestations of esophageal lymphoma. AJR Am J Roentgenol. 1977;128:751-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 31] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Rodriguez AN, Diaz-Jimenez JP. Malignant respiratory-digestive fistulas. Curr Opin Pulm Med. 2010;16:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Westin JR, Gibbs A, Mills KR, Neelapu SS. Hodgkin lymphoma untreated for six years presenting with tracheoesophageal fistula. Case Rep Med. 2012;2012:457908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Kutchuk M, Edelstein Y, Ellis MH. Late relapse of Hodgkin’s lymphoma presenting as fatal hematemesis caused by an esophago-tracheo-arterial fistula. Isr Med Assoc J. 2009;11:637-638. [PubMed] |
| 24. | Coppens E, El Nakadi I, Nagy N, Zalcman M. Primary Hodgkin’s lymphoma of the esophagus. AJR Am J Roentgenol. 2003;180:1335-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Alba D, Lobato SD, Alvarez-Sala R, Villasante C, Echevarría C. Tracheoesophageal fistula as the presenting manifestation of Hodgkin’s lymphoma. Postgrad Med J. 1994;70:49-50. [PubMed] |
| 26. | Sharma M, Aronow WS, O’Brien M, Gandhi K, Amin H, Desai H. T cell lymphoma presenting as esophageal obstruction and bronchoesophageal fistula. Med Sci Monit. 2011;17:CS66-CS69. [PubMed] |
| 27. | Sawyer R, Rosenthal DI, Maniglia AJ, Goodwin WJ. Unusual head and neck manifestations of non-Hodgkin’s lymphomas in children and adults. Laryngoscope. 1987;97:1136-1140. [PubMed] |
| 28. | Joshi A, Fields P, Simo R. Anaplastic lymphoma of the cervical esophagus presenting as a tracheoesophageal fistula. Head Neck. 2008;30:1264-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Gschossmann JM, Bonner JA, Foote RL, Shaw EG, Martenson JA Jr, Su J. Malignant tracheoesophageal fistula in patients with esophageal cancer. Cancer. 1993;72:1513-1521. [PubMed] |
| 30. | Ke M, Wu X, Zeng J. The treatment strategy for tracheoesophageal fistula. J Thorac Dis. 2015;7:S389-S397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 33] [Reference Citation Analysis (0)] |