Published online Feb 16, 2017. doi: 10.4253/wjge.v9.i2.99
Peer-review started: October 7, 2016
First decision: November 10, 2016
Revised: December 5, 2016
Accepted: January 2, 2017
Article in press: January 3, 2016
Published online: February 16, 2017
Processing time: 132 Days and 16.8 Hours
Achalasia is generally accepted as a condition associated with an increased risk for developing esophageal squamous cell carcinoma. In our paper, we introduced an achalasia patient combined with synchronous early esophageal neoplasms. We performed a combination of concurrent endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM). No complications other than postoperative pain that needed morphine treatment for two days had occurred. Dysphagia was significantly improved. Neither reflux nor cough occurred. The short-term efficacy and safety of our case is favorable and suggests that concurrent ESD and POEM could be a treatment option to such patients.
Core tip: Achalasia is generally accepted as a condition associated with an increased risk for esophageal squamous cell carcinoma. However, cases of multiple synchronous neoplastic lesions in an achalasia patient had been rarely reported. In this paper, we performed a combination of concurrent endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM) on one patient suffering from esophageal achalasia for more than six years and esophageal neoplasia lesions for one month. The short-term efficacy and safety of our case is favorable and it suggests that concurrent ESD and POEM could be an option of treatment to this kind of patients.
- Citation: Shi S, Fu K, Dong XQ, Hao YJ, Li SL. Combination of concurrent endoscopic submucosal dissection and modified peroral endoscopic myotomy for an achalasia patient with synchronous early esophageal neoplasms. World J Gastrointest Endosc 2017; 9(2): 99-104
- URL: https://www.wjgnet.com/1948-5190/full/v9/i2/99.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i2.99
Peroral endoscopic myotomy (POEM) is used for treatment of achalasia as Endoscopic submucosal dissection (ESD) for treatment of early esophageal cancer. In this paper, we performed the two procedures on a patient suffering from esophageal achalasia for more than six years and early esophageal cancer for one month simultaneously. The symptoms of the patients relieved significantly while no intraoperative or postoperative complications occurred. The present report describes the safety and efficacy of the combination treatment of POEM and ESD for this kind of patients.
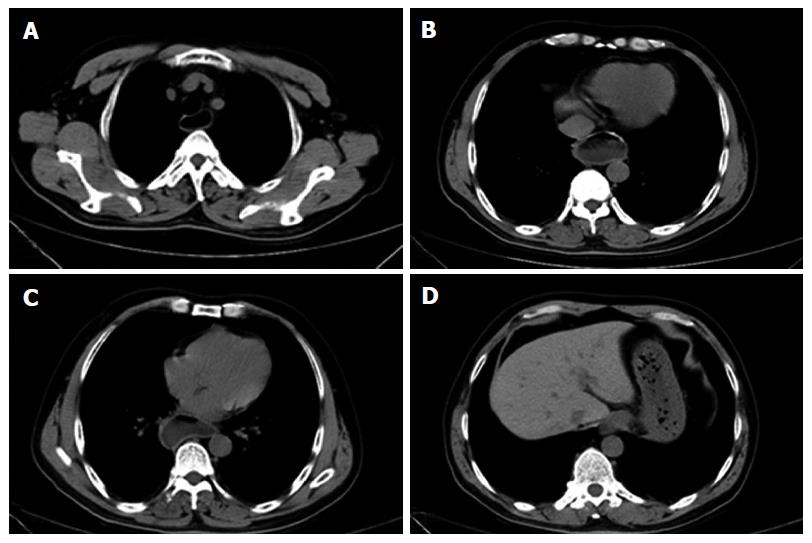
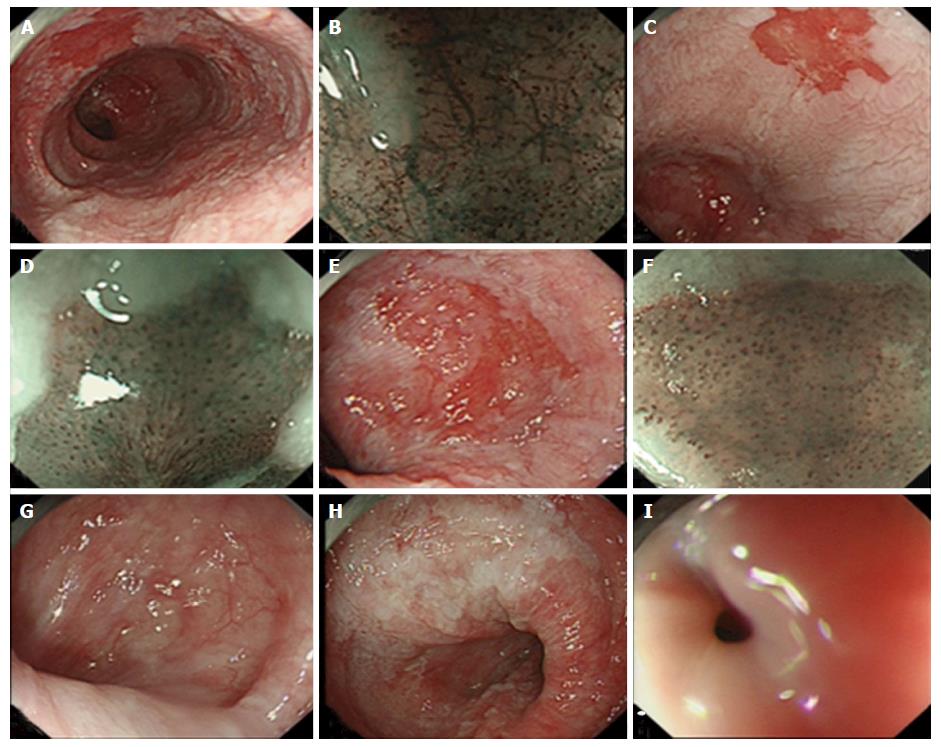
Before POEM, the patient was scored as Eckardt score 6 and Grade II. Chest computed tomography showed an obviously dilated esophageal cavity with large amount fluid retention in the lumen. The cardiac muscle layer was significantly thickened (Figure 1). Esophagogastroduodenoscopy also revealed significantly expanded esophageal lumen and remarkable fluid retention. After pumping the liquid and washing the lumen repeatedly, all of esophagus mucosa appeared edematous and turbid white. A reddish lesion (1.5 cm × 1.0 cm) was detected at 24 cm from the incisor. The lesion was identified as type IV of intra-epithelial papillary capillary loops (IPCLs) according to Inoue’s classification by narrow-band imaging with magnification and background colorization was also seen. Biopsy histopathology showed normal tissue with inflammation. Another lesion (1.0 cm × 0.8 cm) was detected at 32 cm and identified as IPCLs type V1, and the biopsy histopathology showed high-grade intraepithelial neoplasia. The third lesion (1.0 cm × 1.5 cm) was found at 34 cm disclosed type IV-V1 IPCLs, and analysis of the biopsy revealed low-grade intraepithelial neoplasia. The neoplastic lesions were located in the anterior wall of the esophagus. The esophageal lumen below 30 cm was distorted and dilated. The cardia was tightly closed and the resistance was significant (Figure 2). According to the endoscope and pathology funding, the patient was diagnosed with Sigmoid-type achalasia combined with neoplastic lesions.
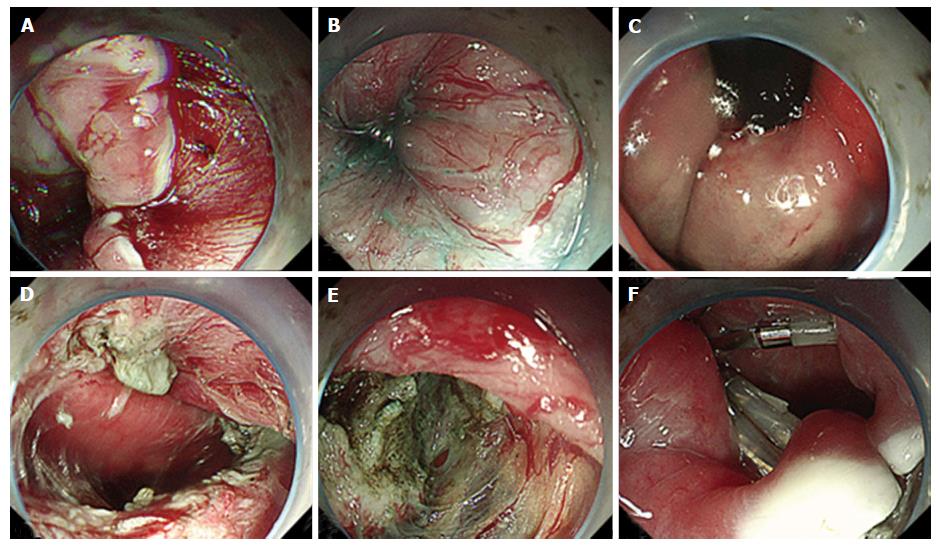
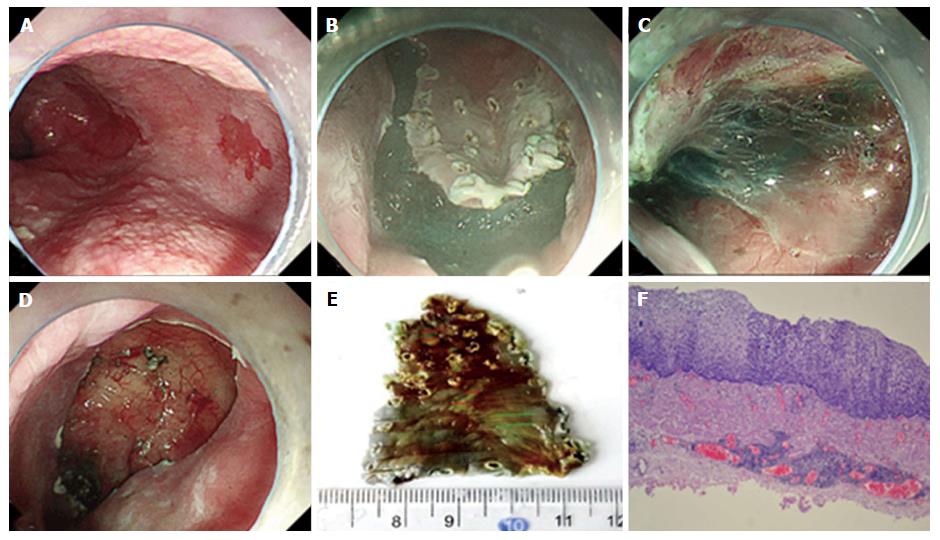
A combination treatment scheme of ESD and POEM was performed. The patient was fasted for over 24 h before procedure. Preoperative antibiotics were applied prophylactically. The patient was intubated and brought under intravenous anesthesia. Carbon dioxide insufflation was used throughout the procedure. First, ESD was conducted for both neoplastic lesions located at 32 cm and 34 cm. Immediately after ESD, a 2 cm longitudinal mucosal incision was made after submucosal injection at the opposite side wall of the ESD wound, the posterior wall. Meanwhile, a short-tunnel POEM surgery [about 35 cm from the esophagogastric junction (EGJ)] was performed; the muscularis propria was completely cut to 3 cm below the cardia. Owing to repeated injections of botulinum toxin and balloon dilatation, the submucosal tunnel creation was rather difficult. In the process of cutting the whole layer of muscularis propria, we found that the circular muscle of esophagus was obviously thickened (about 1 cm). We then exposed the esophageal fiber membrane and encountered the omentum in the cardia. After completing full-thickness myotomy, the entry site was closed using hemostatic clips (Figure 3). Subsequent histological evaluation combined with relevant immunohistochemistry produced a definitive diagnosis of high-grade intraepithelial neoplasia with a component of scattered low-grade intraepithelial neoplasia. The lateral and vertical margins were free (Figure 4). The patient was given liquid diet after 48 h of fasting. Because of the small perforation in the POEM, antibiotics were used to prevent infection. The patient felt severe pain and was given analgesic treatment. Two days later, the pain was relieved and pain medication was discontinued; three days later, the pain disappeared, antibiotics were stopped. Dysphagia was significantly improved. Neither reflux nor cough occurred. He was discharged 7 d later uneventfully. Two months after the procedures, the patient was largely asymptomatic with an increase of 3.5 kg body weight and was score as Eckardt 0. The Endoscopic examination showed the diameter of the esophageal lumen was significantly decreased. No food residual was found in the esophagus and the inflammatory mucosa turned normal. The ESD wounds healed completely. Gastroscope could pass through the EGJ without any resistance. Barium swallow examination showed that the emptying was smooth through the cardia. Due to the particularity of the patient, achalasia combined with neoplastic lesions, long time follow-up will be performed.
Esophageal achalasia is caused by esophageal neuromuscular dysfunction associated with lack of peristalsis of the esophagus, high pressure of lower esophageal sphincter and weakening response to the swallowing relaxation. Esophageal retention of foods and fluids, bacterial overgrowth, and impaired clearance of regurwhich is potentially associated with an increased risk of hyperplasia, dysplasia, and esophageal cancer[1-3]. Wychulis et al[4] have reported a 7-fold increased risk of esophageal squamous cell carcinomas in achalasia patients compared to the general population. However, cases of multiple synchronous neoplastic lesions in an achalasia patient had been rarely reported.
Tang et al[5] reported an achalasia patient with a small dysplastic lesion treated successfully with both of endoscopic mucosal resection (EMR) and POEM simultaneously. We performed ESD instead of EMR, as the size was larger than that of Tang’s case and ESD was more suitable than EMR for resection.
One reason we chose the posterior wall as the position of the mucosal incision of POEM is that it is safe and effective. Now this operation is used for a lot of POEM. The other reason is to avoid the impact of ESD wound and incision of POEM. During the procedure, the patient was left decubitus. As the esophagus was distorted obviously, it was difficult to ensure that the tunnel was not deviated and lost. Aiming for a straight tunnel, the position of liquid concentration and the circular muscle layer were used as references. The tunnel direction was viewed repeatedly in the esophageal lumen.
The reasons that we did not perform ESD and POEM separately were as follows: First, the patient would need to take the risks associated with two times of general anesthesia. In addition, if POEM was performed first, it would result in submucosal fibrosis which might make the subsequent ESD difficult. If ESD first, large amount of fluid retention in the sigmoid-type achalasia would prolong the mucosal healing and even cause unfavorable complication such as bleeding in delayed fashion or systemic infection. As the esophageal cavity was obviously dilated, there was enough luminal space for both ESD and POEM conducted at a time. Recently, modified POEM with shorter submucosal tunnel was confirmed to have good safety and excellent short-term efficacy for achalasia, even for the sigmoid-type[6,7]. Therefore, to reduce operation duration, we generated a short submucosal tunnel for POEM after ESD. Moreover, considering the risk of metachronous neoplasms, long submucosal tunnel creation would result in extensive submucosal fibrosis and would make further if needed ESDs much more difficult and dangerous. Before the ESD mucosal incision, saline was injected into the submucosal layer. The lifting sign was good. We estimated that the lesion had no significant adhesions; the extent of the lesion was not large. There was little risk of perforation during ESD. Even if there was a small perforation, it was also relatively safe to establish a tunnel opening on the contralateral mucosa in case of that the perforation was closed by hemostatic clips and esophageal lumen was remarkably dilated. Fortunately, according to the location of the neoplastic lesions and good physical condition of the patient, two procedures were successfully performed simultaneously.
This is the first case of an achalasia patient with synchronous early esophageal neoplasms treated by a combination of concurrent ESD and POEM. The short-term efficacy and safety of our case is favorable and suggests that concurrent ESD and POEM could be an option of treatment to this kind of patients. More cases, however, are warranted to show its safety and efficacy.
A 50-year-old male suffering from esophageal achalasia and synchronous early esophageal neoplasms was treated by a combination of concurrent endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
Esophageal achalasia, early esophageal neoplasms.
Carcinoma of gastric cardia, reflux esophagitis, angina pectoris.
All initial biochemical and hematological parameter results were within normal limits.
Chest computed tomography showed an obviously dilated esophageal cavity with large amount fluid retention in the lumen. The cardiac muscle layer was significantly thickened.
High-grade intraepithelial neoplasia.
Combination of concurrent endoscopic submucosal dissection and modified peroral endoscopic myotomy.
This is the authors’ first case of an achalasia patient with synchronous early esophageal neoplasms treated by a combination of concurrent ESD and POEM. This case confirmed that it’s safety and efficacy when there was no effect between the locations of the two operations.
This is the interesting case report describing combination of ESD and POEM for an achalasia patient with early esophageal neoplasms. As the authors mention, combination treatment of ESD and POEM seems to be effective in this case.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mangiavillano B, Niimi K S- Editor: Qi Y L- Editor: A E- Editor: Li D
| 1. | Richter JE. Oesophageal motility disorders. Lancet. 2001;358:823-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 180] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Loviscek LF, Cenoz MC, Badaloni AE, Agarinakazato O. Early cancer in achalasia. Dis Esophagus. 1998;11:239-247. [PubMed] |
| 3. | Leeuwenburgh I, Van Dekken H, Scholten P, Hansen BE, Haringsma J, Siersema PD, Kuipers EJ. Oesophagitis is common in patients with achalasia after pneumatic dilatation. Aliment Pharmacol Ther. 2006;23:1197-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Wychulis AR, Woolam GL, Andersen HA, Ellis FH. Achalasia and carcinoma of the esophagus. JAMA. 1971;215:1638-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Tang X, Ren Y, Jiang B, Gong W. Education and Imaging: Gastroenterology: Endoscopic mucosal resection for esophageal dysplasia in an achalasia patient followed by peroral endoscopic myotomy. J Gastroenterol Hepatol. 2015;30:1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Ma XB, Linghu EQ, Wang NJ, Wang XD,Du hong, Meng JY, Wang HB, Zhu J, Tang P, Huang QY, Zhao XW, Chai GQ, Kong JY, Qiu XY. The role of shorter submucosal tunnel POEM surgery in the treatment of LingIIc type. ZhongHua Qiang ing WaiKe Za hi. 2014;37-37. |
| 7. | Wang J, Tan N, Xiao Y, Chen J, Chen B, Ma Z, Zhang D, Chen M, Cui Y. Safety and efficacy of the modified peroral endoscopic myotomy with shorter myotomy for achalasia patients: a prospective study. Dis Esophagus. 2015;28:720-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |