Published online Nov 25, 2015. doi: 10.4253/wjge.v7.i17.1257
Peer-review started: April 30, 2015
First decision: July 26, 2015
Revised: October 2, 2015
Accepted: October 16, 2015
Article in press: October 19, 2015
Published online: November 25, 2015
Processing time: 211 Days and 8.4 Hours
Portal hypertensive duodenopathy (PHD) is a recognized, but uncommon finding of portal hypertension in cirrhotic patients. Lesions associated with PHD include erythema, erosions, ulcers, telangiectasia, exaggerated villous pattern and duodenal varices. However, duodenal polyposis as a manifestation of PHD is rare. We report a case of a 52-year-old man who underwent esophagogastroduodenoscopy and was found with multiple small duodenal polyps ranging in size from 1-8 mm. Biopsy of the representative polyps revealed polypoid fragments of duodenal mucosa with villiform hyperplasia lined by reactive duodenal/gastric foveolar epithelium and underlying lamina propria showed proliferating ectatic and congested capillaries. The features were diagnostic of polyps arising in the setting of PHD.
Core tip: Duodenal polyposis secondary to portal hypertensive duodenopathy (PHD) is rare. We report a case of PHD presenting as polyposis.
- Citation: Gurung A, Jaffe PE, Zhang X. Duodenal polyposis secondary to portal hypertensive duodenopathy. World J Gastrointest Endosc 2015; 7(17): 1257-1261
- URL: https://www.wjgnet.com/1948-5190/full/v7/i17/1257.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i17.1257
Portal hypertensive duodenopathy (PHD) is a recognized, but uncommon finding of portal hypertension in cirrhotic patients. While other associations of portal hypertension such as portal hypertensive gastropathy and portal hypertensive colopathy have been described and studied, data concerning duodenal alterations is relatively scarce. The lesions described in PHD include erythema, erosions, ulcers, telangiectasia, exaggerated villous pattern and duodenal varices[1]. Recently, there have been emerging reports of polyps as a manifestation of PHD[2-5]. Herein, we report a patient with duodenal polyposis secondary to portal hypertension, review the literature and describe the spectrum of histopathologic changes.
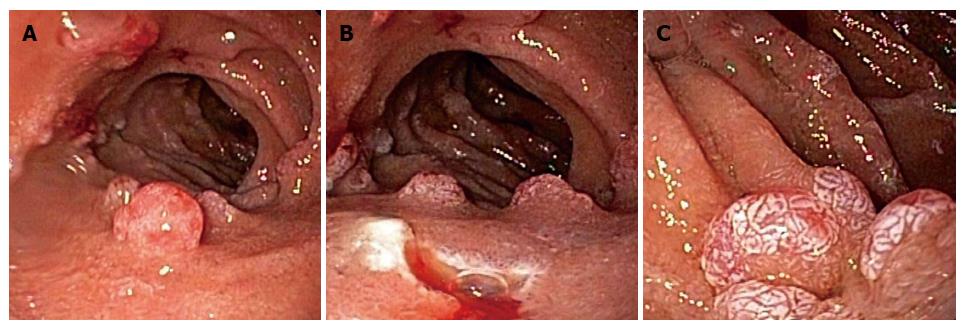
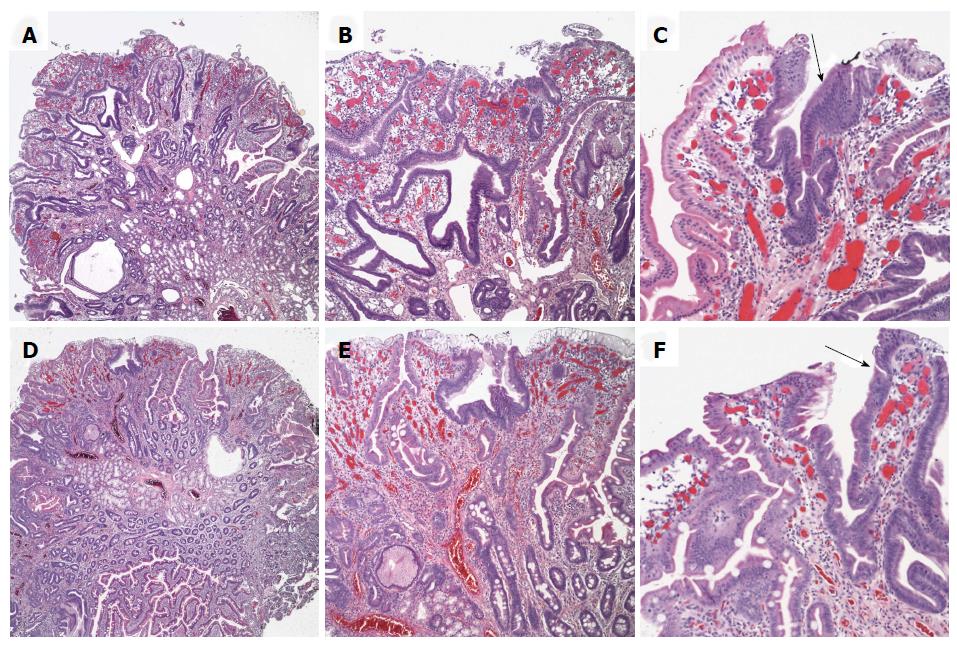
A 52-year-old man with compensated alcoholic cirrhosis presented for follow up esophagogastroduodenoscopy. Past medical history includes remote T1N0 colon cancer (status post right hemicolectomy 4 years), low-grade gastrointestinal blood loss, iron deficiency anemia, gastric antral vascular ectasia, portal hypertensive gastropathy and hypertension. He was diagnosed with cirrhosis 13 years ago when he presented with jaundice and ascites and had a recent history of hepatic encephalopathy. Abdominal U/S and magnetic resonance imaging showed a large heterogenous liver, recanalization of the umbilical vein, splenomegaly, splenorenal shunt, additional collateral vessels inferior to the left renal vein and scattered renal cysts. Endoscopy revealed numerous small 1-2 mm polyps extending from the duodenal bulb to the second portion of the duodenum. The three largest polyps included a 6 mm polyp in the mid duodenal bulb (Figures 1A and B), 8 mm polyp distal to this along the anterior wall, and 8 mm polyp in the second part of the duodenum (Figure 1C). The esophagus was normal and no esophageal varices were noted. The stomach showed diffuse “snake skin” appearance, an area of friable mucosa with a polypoid appearance and surface erosions in the antrum and pre-pyloric area with spontaneous oozing of blood. The three duodenal largest polyps were biopsied and histologic examination revealed polypoid fragments of duodenal mucosa with villiform hyperplasia lined by reactive duodenal and gastric foveolar epithelium. The underlying lamina propria showed proliferating ectatic and congested capillaries (Figures 2A and B, D and E). The findings were diagnostic of multiple portal hypertensive duodenal polyps.
Common gastrointestinal tract manifestations of portal hypertension include esophageal/gastric/anorectal varices and gastric antral vascular ectasia. In addition, less common features include portal hypertensive gastropathy[6-8], congestive jejunopathy[9,10], portal colopathy[11,12] and PHD[1,13]. PHD is commonly defined as the appearance of patchy or diffuse congestion of the duodenal mucosa associated with friability, erosions or ulcerations[14,15]. The prevalence of PHD in cirrhotic patients with portal hypertension ranges from 8.4%[16] to 51.4%[1]. The lesions described in PHD include erythema, erosions, ulcers, telangiectasia, exaggerated villous pattern and duodenal varices[1]. Coexistence of severe gastropathy and higher hepatic venous pressure gradients are more frequent in PHD patients and features of PHD have been reported to disappear after liver transplantation[16].
Duodenal polyps as a manifestation of PHD, an uncommon event, have been reported previously (summarized in Table 1). These include an ulcerated solitary 3 cm polyp in the descending duodenum[3], multiple sessile polyps in the first portion of the duodenum[2] and a recent report documenting two to “several” duodenal or jejuno-ileal polypoid lesions ranging in size from < 5 mm to 15 mm in 5 patients[4]. The spectrum of histopathologic findings in the polyps includes the presence of numerous capillaries with vascular ectasia/congestion/thrombi as well as fibrosis and smooth muscle proliferation. In addition gastric foveolar metaplasia, reactive atypia and ulceration may be seen. Devadason et al[5] reported “duodenal capillary hemagiomatous polyps” in 3 pediatric patients (aged 1, 4 and 6 years old). All these 3 patients presented with multiple duodenal polyps in either the 1st or 2nd portion of the duodenum in the setting of extrahepatic portal venous obstruction. Polyps were biopsied in two patients, both of which demonstrated lobular capillary proliferation within the polyps[5]. Although they favored the term “duodenal capillary hemagiomatous polyps”, it appears from their description, as well as accompanying image, that the polyps they described share similar morphological features to the polyps in our case and other reported polyps in the setting of PHD.
| Ref. | Age (yr)/gender | Location(s) | Number/sizes of polyps | Pathologic findings | Etiology of portal hypertension |
| Current report | 52/M | Duodenal bulb to second portion | Greater than 7, majority 1-2 mm, largest 8 mm | Villiform hyperplasia of reactive intestinal and gastric foveolar epithelium, proliferating ectatic and congested lamina propria vessels | Alcoholic cirrhosis |
| Pillai et al[2] | 55/M | 1st portion of duodenum | “multiple sessile polyps”, sizes NS | Polypoid muocsa lined by small intestinal and gastric foveolar type epithelium with ectatic capillaries, fibrosis and smooth muscle proliferation of lamina propria | Alcoholic cirrhosis |
| Zeitoun et al[3] | 70/M | 2nd portion of duodenum | Single polyp, 3 cm | Numerous thick-walled capillaries with vascular ectasia in lamina propria | Alcoholic cirrhosis |
| 1Lemmers et al[4] | 50/F | Jueuno-ileal | “Several”, > 5 mm | Lamina propria vascular dilation and thrombi without epithelial atypia | Hepatitis C cirrhosis |
| 73/M | Jejunal | Two “bumps”, < 5 mm | Not biopsied | Cryptogenic cirrhosis | |
| 67/M | Duodenal | “Several”, 5 mm | Lamina propria vascular dilation and inflammation with epithelial atypia and ulceration | Alcoholic cirrhosis | |
| 74/F | Antral/duodenal | “Several”, 15 mm | Lamina propria vascular dilation and epithelium with crenellated glands | Hepatitis C cirrhosis | |
| 66/F | Duodenal/jejuno-ileal | “Several”, 5/< 5 mm | Not biopsied | Cryptogenic cirrhosis | |
| Devadason et al[5] | 6 yr/M | 1st and 2nd portion of duodenum | “polyps”, sizes NS | Lobular capillary proliferation in a hemagiomatous pattern in lamina propria | EHPVO |
| 4 yr/F | 2nd portion of duodenum | “numerous”, sizes NS | Lobular capillary proliferation in a hemagiomatous pattern in lamina propria | EHPVO | |
| 1 yr/F | 2nd portion of duodenum | “polyps”, sizes NS | Polyp not biopsied, mucosa adjacent to polyp with ecatsia and congestion of lamina propria with smooth muscle hypertrophy | EHPVO |
To date, including our case, there are 11 documented reports of polyps associated with PHD (Table 1). There is no gender predilection (6 male and 5 female), the ages of patients ranges from 1 to 73 years and in the majority of cases (10/11), multiple polyps are seen. The etiology of portal hypertension in adult patients include alcoholic cirrhosis (37.5%, 3/8), hepatitis C cirrhosis (25%, 2/8) and cryptogenic cirrhosis (37.5%, 3/8), while extrahepatic portal venous obstruction accounts for all cases in the pediatric population (100%, 3/3).
Histologically, the PHD associated polyp surface- and crypt-lining epithelium may focally show cells with mucin depletion and contain slightly pencillate nuclei with mild hyperchromasia (Figures 2C and F). These features may mimic duodenal adenomatous polyp, a precancerous lesion in the duodenum. Our current case was previously diagnosed as “duodenal adenomas” at an outside institution. The initial diagnosis of duodenal adenoma in our patient’s prior biopsy highlights the challenges that the reactive atypia may pose during histological evaluation. The differential diagnosis of polypoid lesions in the duodenum is diverse (Table 2) and we limit our discussion to more commonly seen and lesions with similar histologically features to PHD associated polyps. While duodenal adenomas with low-grade dysplasia (which are histologically similar to those seen in the colon) are typically composed of mucin depleted cells with hyperchromatic pencillate nuclei, compared to the reactive atypia seen in polyps associated with PHD, nuclei show a greater degree of enlargement, hyperchromasia and stratification. PHD polyps differ from duodenal hamartomatous polyps seen in Peutz-Jegher syndrome as polyps in the latter typically show disorganized mucosa with thick arborizing smooth muscle fibers of the muscularis mucosa. Although there may be histologic overlap between Juvenile polyps, inflammatory bowel disease (IBD) associated inflammatory polyps and PHD associated polyps, Juvenile polyps are characterized by dilated mucin filled crypts, while IBD associated polyps tend to have prominent glandular architectural distortion in the background of IBD.
| Primary | Epithelial |
| Duodenal adenoma/adenocarcinoma | |
| Ampullary adenoma/adenocarcinoma | |
| Hyperplasia, heterotopias, ectopias, inflammatory | |
| Brunners gland hyperplasia/hamartoma | |
| Gastric/pancreatic hetertopia/ectopia | |
| IBD associated inflammatory pseudopolyps | |
| Inflammatory fibroid polyp | |
| Peutz Jegher polyps | |
| Juvenile polyps (JPS or PTEN associated) | |
| Cronkhite-Canada syndrome polyps | |
| Neuroendocrine/neural | |
| Neuroendocrine tumors | |
| Mixed adenocarcinoma neuroendocrine carcinoma | |
| Gangliocytic paranglioma | |
| Neurofibroma | |
| Ganglioneuroma | |
| Schwannoma | |
| Perinerioma | |
| Mesenchymal | |
| Gastrointestinal stromal tumor | |
| Leiomyoma | |
| Lipoma | |
| Hemangioma | |
| Granular cell tumor | |
| Kaposi sarcoma | |
| Lymphoid | |
| Lymphoid hyperplasia | |
| B and T cell lymphomas | |
| Secondary | Metastases |
| Miscellaneous | Malakoplakia, mucosal prolapse related, lymphangiectasia, xanthoma |
In summary, duodenal polyps secondary to PHD is uncommon. With our case, the total number of patients reported in the literature to date is 11. The finding of multiple polyps in a patient with portal hypertension should raise suspicion for this entity and careful histopathologic examination is necessary to render the appropriate diagnosis.
A 52-year-old man with compensated alcoholic cirrhosis presented for follow up esophagogastroduodenoscopy and multiple duodenal polyps were found.
Cirrhosis and duodenal polyps.
Duodenal adenomatous polyp, polyposis syndrome, duodenal pancreatic or gastric ectopia, or other benign neoplasms.
Endoscopy revealed numerous small 1-2 mm polyps extending from the duodenal bulb to the second portion of the duodenum. The three largest polyps included a 6 mm polyp in the mid duodenal bulb, 8 mm polyp distal to this along the anterior wall, and 8 mm polyp in the second part of the duodenum.
Portal hypertensive duodenal polyps.
Duodenal polyps as a manifestation of portal hypertensive duodenopthy (PHD), an uncommon event, have been reported previously. The prevalence of PHD in cirrhotic patients with portal hypertension ranges from 8.4% to 51.4%. However, manifestation as multiple duodenal polyps is rare.
Portal hypertensive duodenal polyps are seen in patients with cirrhosis and portal hypertension. The spectrum of histopathologic findings in the polyps includes the presence of numerous capillaries with vascular ectasia/congestion/thrombi as well as fibrosis and smooth muscle proliferation. In addition gastric foveolar metaplasia, reactive atypia and ulceration may be seen.
PHD is a recognized, but uncommon finding of portal hypertension in cirrhotic patients. Multiple duodenal polyps can be an endoscopic finding of PHD.
The authors reported a 52-year-old patient with cirrhosis and portal hypertension who underwent endoscopy and was found with multiple portal hypertensive duodenal polyps. This is an interesting case report and literature review. It is very well written with excellent images. The article highlights the clinical characteristics of PHD and provides information about differential diagnosis of portal hypertensive duodenal polyps.
P- Reviewer: Therapondos G, Thandassery RB S- Editor: Gong XM L- Editor: A E- Editor: Jiao XK
| 1. | Barakat M, Mostafa M, Mahran Z, Soliman AG. Portal hypertensive duodenopathy: clinical, endoscopic, and histopathologic profiles. Am J Gastroenterol. 2007;102:2793-2802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Pillai SB, Ram Ganesh VR, Mohanakrishnan A, Nirmala V. Portal duodenopathy presenting as polyposis. Indian J Pathol Microbiol. 2010;53:558-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Zeitoun JD, Chryssostalis A, Terris B, Prat F, Gaudric M, Chaussade S. Portal hypertensive duodenal polyp: a case report. World J Gastroenterol. 2007;13:1451-1452. [PubMed] |
| 4. | Lemmers A, Evrard S, Demetter P, Verset G, Gossum AV, Adler M, Devière J, Moine OL. Gastrointestinal polypoid lesions: a poorly known endoscopic feature of portal hypertension. United European Gastroenterol J. 2014;2:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Devadason D, Murphy MS, Brown R, Wilson D, McKiernan PJ. Duodenal capillary hemangiomatous polyps: a novel manifestation of extrahepatic portal hypertension? J Pediatr Gastroenterol Nutr. 2007;45:114-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | McCormack TT, Sims J, Eyre-Brook I, Kennedy H, Goepel J, Johnson AG, Triger DR. Gastric lesions in portal hypertension: inflammatory gastritis or congestive gastropathy? Gut. 1985;26:1226-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 380] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Qureshi K, Al-Osaimi AM. Approach to the management of portal hypertensive gastropathy and gastric antral vascular ectasia. Gastroenterol Clin North Am. 2014;43:835-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Zardi EM, Ghittoni G, Margiotta D, Viera FT, Di Matteo F, Rossi S. Portal hypertensive gastropathy in cirrhotics without varices: a case-control study. Eur J Gastroenterol Hepatol. 2015;27:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Nagral AS, Joshi AS, Bhatia SJ, Abraham P, Mistry FP, Vora IM. Congestive jejunopathy in portal hypertension. Gut. 1993;34:694-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Desai N, Desai D, Pethe V, Deodhar KP, Sawant P, Nanivadekar S. Portal hypertensive jejunopathy: a case control study. Indian J Gastroenterol. 2004;23:99-101. [PubMed] |
| 11. | Kozarek RA, Botoman VA, Bredfeldt JE, Roach JM, Patterson DJ, Ball TJ. Portal colopathy: prospective study of colonoscopy in patients with portal hypertension. Gastroenterology. 1991;101:1192-1197. [PubMed] |
| 12. | Urrunaga NH, Rockey DC. Portal hypertensive gastropathy and colopathy. Clin Liver Dis. 2014;18:389-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Vigneri S, Termini R, Piraino A, Scialabba A, Bovero E, Pisciotta G, Fontana N. The duodenum in liver cirrhosis: endoscopic, morphological and clinical findings. Endoscopy. 1991;23:210-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Gupta R, Saraswat VA, Kumar M, Naik SR, Pandey R. Frequency and factors influencing portal hypertensive gastropathy and duodenopathy in cirrhotic portal hypertension. J Gastroenterol Hepatol. 1996;11:728-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K. Duodenal erosions, a common and distinctive feature of portal hypertensive duodenopathy. Am J Gastroenterol. 2002;97:867-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Menchén L, Ripoll C, Marín-Jiménez I, Colón A, Gómez-Camarero J, González-Asanza C, Menchén P, Cos E, Bañares R. Prevalence of portal hypertensive duodenopathy in cirrhosis: clinical and haemodynamic features. Eur J Gastroenterol Hepatol. 2006;18:649-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |