Published online Sep 25, 2015. doi: 10.4253/wjge.v7.i13.1103
Peer-review started: June 5, 2015
First decision: August 10, 2015
Revised: August 21, 2015
Accepted: September 1, 2015
Article in press: September 2, 2015
Published online: September 25, 2015
Processing time: 114 Days and 19.3 Hours
AIM: To determine the frequency of identification of the triradiate fold during colonoscopy and evaluate its reliability as a marker of caecal intubation.
METHODS: One hundred consecutive patients undergoing colonoscopy in a tertiary hospital colorectal unit from May to September 2013 were studied. Video documentation of the caecum was recorded and shown to consultant colorectal surgeons on the unit. Each reviewer was asked through a series of questions to independently identify the triradiate fold. The main outcome was the frequency of visualisation of the triradiate fold in the caecum.
RESULTS: The triradiate fold was seen on average in 18% of cases, but inter-observer agreement was poor. There were only four patients (4%) in which all reviewers agreed on the presence of a triradiate fold. In patients who had undergone previous appendicectomy, the appendiceal orifice was less frequently seen compared with patients who had not undergone appendicectomy.
CONCLUSION: The triradiate fold is infrequently seen during colonoscopy and is therefore an unreliable landmark of caecal intubation.
Core tip: The triradiate fold is often described as a major landmark of caecal intubation in colonoscopy, but its frequency of visualisation has not been previously documented. This study shows that identification of the triradiate fold is infrequent and its presence is subjective. Inclusion in guidelines or colonoscopy software programs as a sole marker of complete colonoscopy is questionable.
- Citation: Finlayson A, Chandra R, Hastie IA, Jones IT, Shedda S, Hong MKY, Yen A, Hayes IP. Triradiate caecal fold: Is it a useful landmark for caecal intubation in colonoscopy? World J Gastrointest Endosc 2015; 7(13): 1103-1106
- URL: https://www.wjgnet.com/1948-5190/full/v7/i13/1103.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i13.1103
Accurate assessment of the extent of colonoscopy relies on the identification and cognitive integration of several caecal landmarks to the trained endoscopist. These landmarks may include the ileocaecal valve, ileal mucosa, appendiceal orifice and caecal folds.
Of these many landmarks, the ileocaecal valve has been shown to be the single most reliable landmark, being viewed 98% of the time when caecal intubation had been confirmed with fluoroscopy[1]. The same study found the appendiceal orifice to be the second most reliable landmark. Others contend that the most accurate method to ensure caecal intubation is to enter the terminal ileum and confirm with a biopsy of ileal mucosa[2].
Various names and descriptions have been given to the folds in the caecum. The converging folds have been named the triradiate fold, Mercedes sign, crows-foot and caecal strap fold[2-5]. The term triradiate fold is used in many computerized colonoscopy databases and also by the Australian National Bowel cancer screening project as a landmark for caecal intubation with colonoscopy[6]. Last’s Anatomy textbook describes the three taenia of the colon converging at the base of the appendix[7]. However in practice, a clearly defined triradiate fold is not always seen at colonoscopy. We undertook this study to document how frequently a triradiate fold is seen at the caecal pole during colonoscopy.
This study was approved by the Melbourne Health Human Research Ethics Committee at the Royal Melbourne Hospital, Parkville, Australia. All consecutive patients undergoing colonoscopy from May to September 2013 either performed or supervised by two colorectal fellows were included in the study. Exclusion criteria were previous caecal resection, inadequate bowel preparation, technical issues with recording equipment and incomplete colonoscopies.
All colonoscopies were performed with an Olympus colonoscope. Once caecal intubation was reached, a short video was recorded on the Olympus Endobase® program. The caecal pole was thoroughly irrigated to adequately display the caecum. Caecal intubation was confirmed on collective visualisation of the ileocaecal valve, blind-ending caecal pole and appendiceal orifice when present. It was not routine in our institution to perform ileal intubation as a marker of complete colonoscopy unless clinically indicated. The videos were recorded in a standard fashion to give a panorama of the caecal pole including established landmarks of the appendiceal orifice and ileocaecal valve, and then zoomed in on the appendiceal orifice and surrounding folds.
All 100 videos were then edited using Corel Video Studio Pro® to delete unnecessary footage. The videos submitted for analysis included continuous footage so that each caecum was easily identifiable. The final length of edited videos ranged from 3 to 26 s. The shortest videos were those where all features of the caecum were very easily seen.
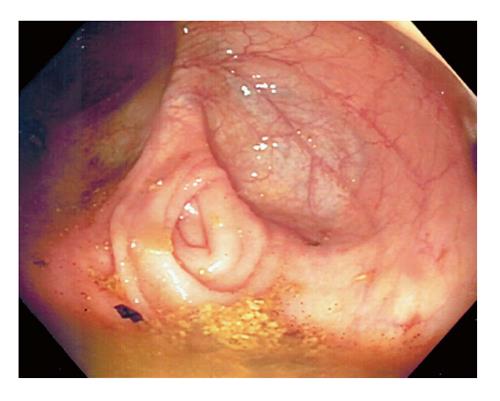
Each video was then shown to six consultant surgeons on the unit who then individually evaluated them. Prior to evaluation, a photograph of what we considered to be a triradiate fold was shown to all surgeons (Figure 1). A photograph showing an appendiceal orifice with no triradiate fold was also shown (Figure 2). For each video the following questions were asked:
Are you satisfied that this is a video of the caecum?
Can you identify the appendiceal orifice?
Is there a triradiate fold at the appendix orifice?
If the reviewer was not satisfied that the caecum was represented in the video, the remaining two questions were obsolete and not answered. Similarly if the appendiceal orifice could not be identified, no judgment could be made on the presence of a triradiate fold.
Statistical analysis was performed using Microsoft Excel®. Positive responses from the six reviewers were tallied for each of the 100 videos analysed and for each of the three questions asked. Individual and overall proportions of positive responses were calculated. Inter-rater reliability was measured using Conger’s kappa coefficient for multiple raters. The relationship between previous appendicectomy and visualisation of the appendiceal orifice was analysed using Fisher’s exact test on a 2 × 2 contingency table. Differences were considered significant when the probability was less than 0.05.
One hundred and thirty-four consecutive colonoscopies were either performed or supervised by two fellows. Of these 134 patients, 34 were excluded, leaving 100 colonoscopies for analysis. Of the patients excluded, 11 had a previous caecal resection, 14 had inadequate bowel preparation, 6 were incomplete colonoscopies and 3 had technical problems with the recording equipment. Of the 100 included patients, there were 43 males and 57 females with a mean age of 61 ± 15.8 years. The indications for their colonoscopies are given in Table 1.
| Indication | Number |
| Per rectal bleeding | 26 |
| Polyp follow up | 17 |
| Cancer follow up | 14 |
| Diverticulitis | 9 |
| Altered bowel habit | 9 |
| Abnormal imaging | 8 |
| Faecal occult blood test positive | 6 |
| Fistula investigation | 3 |
| Family history | 2 |
| Anaemia | 2 |
| Iron deficiency | 2 |
| Volvulus | 1 |
| Rectal prolapse | 1 |
A Conger’s Kappa coefficient for multiple raters was calculated to assess agreement between the answers to each of the three questions. This showed a strong agreement for each of the three questions, with coefficients of 0.93 for identification of the caecum, 0.79 for identification of the appendix and 0.81 for identification of the triradiate fold.
On average, the reviewers were satisfied the video depicted the caecum in 97% of cases. In those cases where the caecum was identified, the appendiceal orifice could be seen in 83%. In those cases where the appendix orifice was identified, a triradiate fold was seen in 18% (Table 2).
| Reviewer | Caecum | Appendiceal orifice | Triradiate fold | ||
| 1 | 99 | 76 | 77% | 13 | 17% |
| 2 | 95 | 79 | 83% | 17 | 22% |
| 3 | 96 | 76 | 79% | 13 | 17% |
| 4 | 93 | 89 | 96% | 18 | 20% |
| 5 | 100 | 89 | 89% | 11 | 12% |
| 6 | 97 | 73 | 75% | 13 | 18% |
| Average | 97 | 80 | 83% | 14 | 18% |
The Kappa coefficient for the triradiate fold was high due to strong agreement among observers about the non-visualization of the triradiate fold. In the smaller percentage of cases where the triradiate fold was identified, there was poor agreement among reviewers. There were only four patients in which all reviewers agreed on the presence of a triradiate fold. The appendiceal orifice was seen in 38 of 54 videos (70.4%) where the patient had undergone previous appendicectomy. When the patient had not undergone an appendicectomy the appendiceal orifice was seen in 444 of 527 videos (84.3%, P = 0.014).
Accurate identification of the caecum at colonoscopy relies heavily on visualising certain landmarks. The caecal folds have been previously suggested to be an unreliable landmark[8]. In this study we have demonstrated that a triradiate caecal fold is only seen 18% of the time when averaged across all observers. In cases where it was identified, there was poor inter-observer agreement.
Anatomically, the triradiate fold must be centred on the appendiceal orifice. Our study showed that the appendiceal orifice was less frequently seen in patients who had undergone previous appendicectomy. Elsewhere in the colon the intersection of haustral folds and a taenia coli may create a triradiate appearance that could be confused with the triradiate fold of the caecum.
This study is limited by its subjective design. The six consultants who analysed each video were aware of the study hypothesis, which may have influenced their response to the questions. However, they were not aware that all videos were of the caecum. Variables that may influence the identification of the caecal folds include the amount of insufflation. A large amount of inflation of the caecum may flatten the caecal folds, and thus a triradiate fold that may have been seen in a less distended caecum may have “disappeared” with inflation. Although this theory was not directly tested, we did not observe that inflation had any bearing on the visualization of a triradiate caecal fold through the process of recording, reviewing and editing the videos.
Photo documentation of caecal intubation has been recommended as routine practice although some studies have shown that still photography has poor reliability[9]. Video documentation has previously been shown to be superior to still photography in identifying the caecum to independent observers[3]. Our initial proposal was to use photo rather than video documentation. On review of the first still photographs taken it was our belief that a photograph alone was not sufficient to identify the caecum with certainty. The video however, gave greater detail and provided an accurate depiction of the caecum as demonstrated by the 97% agreement among reviewers. If caecal intubation documentation is to become a marker of quality and successful completion, video documentation appears to be a more reliable method.
This is the first study to look specifically at the triradiate caecal fold as a landmark during colonoscopy. The triradiate fold is an infrequently seen feature of the caecum and as such should not be relied upon to confirm caecal intubation.
We would like to thank the staff of the endoscopy suite at the Royal Melbourne Hospital for their assistance in the technical aspects of video recording.
Caecal landmarks are important for accurate assessment of the extent of colonoscopy. The triradiate fold in the caecum is referenced as a major landmark in some guidelines and endoscopy programs. This study was conducted to determine the frequency of identification of the triradiate fold.
Colonoscopy is a common investigation modality. Quality assurance has become a global focus. One quality measure in colonoscopy is completion rate. This study explores the role of visualisation of the triradiate fold as a marker of colonoscopy completion.
This is the first study that quantifies the rate of visualisation of the triradiate fold, and shows that it is infrequently seen.
The inclusion of the triradiate fold as a marker of colonoscopy completion in guidelines and endoscopy programs is questionable.
Triradiate fold is the appearance of three caecal folds converging upon the appendiceal orifice as seen at colonoscopy.
This is a very interesting, concise and “clever” paper. It is also written in excellent English, fluent and easy to read.
P- Reviewer: Ding XW, Giannopoulos GA, Slomiany BL, Sugimoto S S- Editor: Qiu S L- Editor: A E- Editor: Liu SQ
| 1. | Cirocco WC, Rusin LC. Confirmation of cecal intubation during colonoscopy. Dis Colon Rectum. 1995;38:402-406. [PubMed] |
| 2. | Clark , Rocker , Reddy , Aslam , Owen . Confirmation of complete colonoscopy without intubation of the ileum. Colorectal Dis. 1999;1:283-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Coe SG, Panjala C, Heckman MG, Patel M, Qumseya BJ, Wang YR, Dalton B, Tran P, Palmer W, Diehl N. Quality in colonoscopy reporting: an assessment of compliance and performance improvement. Dig Liver Dis. 2012;44:660-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Park HJ, Hong JH, Kim HS, Kim BR, Park SY, Jo KW, Kim JW. Predictive factors affecting cecal intubation failure in colonoscopy trainees. BMC Med Educ. 2013;13:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Rex DK. Still photography versus videotaping for documentation of cecal intubation: a prospective study. Gastrointest Endosc. 2000;51:451-459. [PubMed] |
| 6. | Australian Government Department of Health. National Bowel Cancer Screening Program. 2014;. |
| 7. | McMinn RM. Last’s Anatomy. London: Churchill Livingstone 2003; . |
| 8. | Maslekar S, Avery G, Duthie GS. Quality assurance in colonoscopy: role of endomucosal clips. Colorectal Dis. 2010;12:651-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Thuraisingam AI, Brown JL, Anderson JT. What are the sensitivity and specificity of endoscopic photographs in determining completion of colonoscopy? Results from an online questionnaire. Eur J Gastroenterol Hepatol. 2008;20:567-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |