Published online Apr 16, 2012. doi: 10.4253/wjge.v4.i4.142
Revised: February 24, 2012
Accepted: March 30, 2012
Published online: April 16, 2012
Biliary fully covered self-expanding metal stents (FCSEMS) are now being used to treat several benign biliary conditions. Advantages include small predeployment and large postexpansion diameters in addition to an easy insertion technique. Lack of imbedding of the metal into the bile duct wall enables removability. In benign biliary strictures that usually require multiple procedures, despite the substantially higher cost of FCSEMS compared with plastic stents, the use of FCSEMS is offset by the reduced number of endoscopic retrograde cholangiopancreatography interventions required to achieve stricture resolution. In the same way, FCSEMS have also been employed to treat complex bile leaks, perforation and bleeding after endoscopic biliary sphincterotomy and as an aid to maintain permanent drainage tracts obtained by means of Endoscopic Ultrasound-guided biliary drainage. Good success rates have been achieved in all these conditions with an acceptable number of complications. FCSEMS were successfully removed in all patients. Comparative studies of FCSEMS and plastic stents are needed to demonstrate efficacy and cost-effectiveness
- Citation: García-Cano J. Use of fully covered self-expanding metal stents in benign biliary diseases. World J Gastrointest Endosc 2012; 4(4): 142-147
- URL: https://www.wjgnet.com/1948-5190/full/v4/i4/142.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i4.142
Biliary self-expanding metal stents (SEMS) have the advantage of being inserted undeployed with very small sizes and provide, when fully opened, large diameters for biliary drainage. However, their use in benign conditions has been very limited, mainly because of difficulty in their extraction.
Stent insertion and sphincterotomy by means of endoscopic retrograde cholangiopancreatography (ERCP) are the main techniques used to solve biliary obstruction. In 1982, the increase in diameter of the duodenoscope working channel, allowed the use of large bore (10 F or 3.3 mm) plastic stents[1]. Plastic stents are routinely used in benign biliary conditions to treat strictures of various etiologies[2], leaks[3], bile duct perforations[4] and in a temporary or permanent way for the management of common bile duct stones that have not been completely extracted after ERCP[5,6]. For years, improvements in technology have enabled the use of different materials to construct the so-called SEMS. It is well known that these stents are inserted undeployed with a diameter much smaller than they can reach after they are fully opened. As a consequence, a size well suited for biliary drainage up to 30 F or 10 mm, can be achieved with a simple insertion technique. However, until recently, most biliary SEMS were bare, that is, they had no coating material on the metal. For this reason, they soon embedded in body tissues and were difficult to remove after insertion[7].
Several SEMS have now been produced where the metal is coated with different materials. If the entire stent is covered, they are known as fully covered SEMS (FCSEMS). In general, this results in the stent not being trapped in the bile tissue with have the possibility of being extracted. Initial studies were carried out with partially covered SEMS (PCSEMS). In this model, about 5 mm in the upper and distal part of the stent are uncovered, whilst the rest of the stent is covered. When the extreme end is placed in the duodenal lumen, it has to be far enough out of the papilla to ensure the tissue does not grow through the uncovered mesh making extraction difficult[8]. It appears that, in general, the extraction of biliary PCSEMS are more technically demanding than removal of FCSEMS[9]. For this reason, in a recent study on post liver transplantation biliary strictures, a partially covered biliary Wallstent was left in place for only two months to allow easy extraction. In spite of short placement time, the authors concluded that removal was sometimes challenging[10].
Biliary FCSEMS have been more recently marketed than PCSEMS, therefore, there are fewer published reports. It is probable that outcomes in benign conditions will be similar with FCSEMS to those reported with PCSEMS with the advantage of easier removal.
Not all FCSEMS are available in all countries. These stents are intended for TTS insertion (through the working channel of a therapeutic duodenoscope or endoscope). There are other types for transhepatic placement (Table 1).
| Manufacterer | Model | Material | Deployed diameters (mm) and lengths (cm) |
| Boston scientific | Fully covered Wallflex | Platinol covered with permalume | 8 or 10 mm |
| 4, 6, 8 cm | |||
| Taewoong Medical | S-Type fully covered | Nitinol covered with silicone | 6, 8 or 10 mm |
| 4-15 cm | |||
| M.I. Tech | Hanarostent covered, with lasso or with anchoring flaps | Nitinol covered with silicone | 10 mm |
| 4-10 cm | |||
| Standard SciTech | Biliary covered Bonastent with flared ends | Nitinol covered with silicone | 10 mm |
| 4-10 cm | |||
| Ella-CS | Nitinella plus | Nitinol covered with silicone | 8 or 10 mm |
| 4-6-8-10 cm | |||
| ConMed | Gore viabil with or without holes and with fins | Nitinol covered with ePTFE/FEP (gore tex) | 8 or 10 mm |
| 4-6-8-10 cm |
For biliary FCSEMS insertion, a guidewire is previously placed beyond the location of the biliary problem (i.e., stricture) in the usual manner. The deployment mechanism is similar to most SEMS. The outer cover which maintains the folded stent is pulled back and the release begins in the distal part. Almost all packed stents have more length after deployment, this is called foreshortening. As the SEMS is opened, a progressive span reduction occurs and must be corrected continuously to ensure full opening takes place in the correct position and not entirely within the bile duct. The majority of them can be re-folded or re-sheathed completely after partial deployment of the stent has begun.
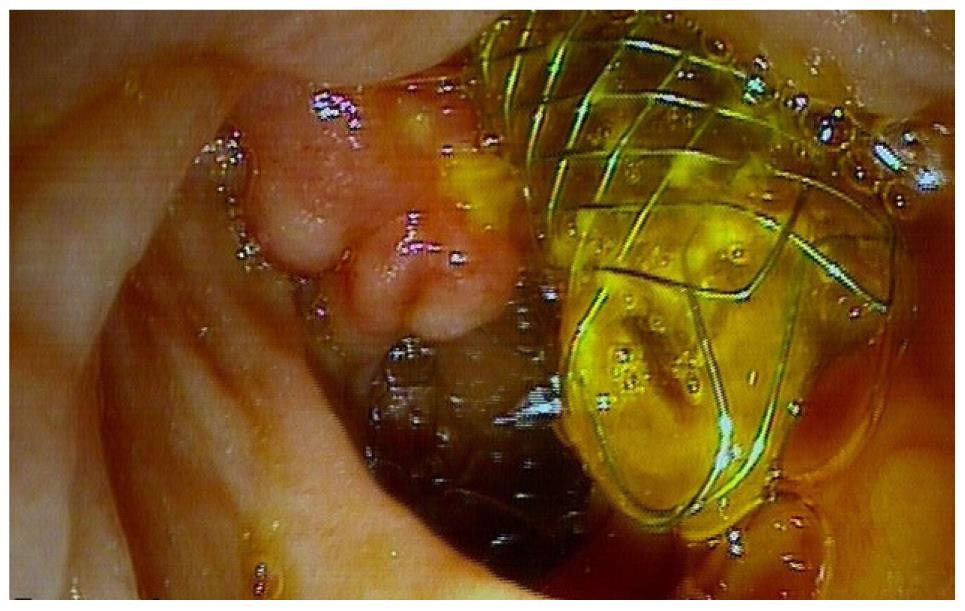
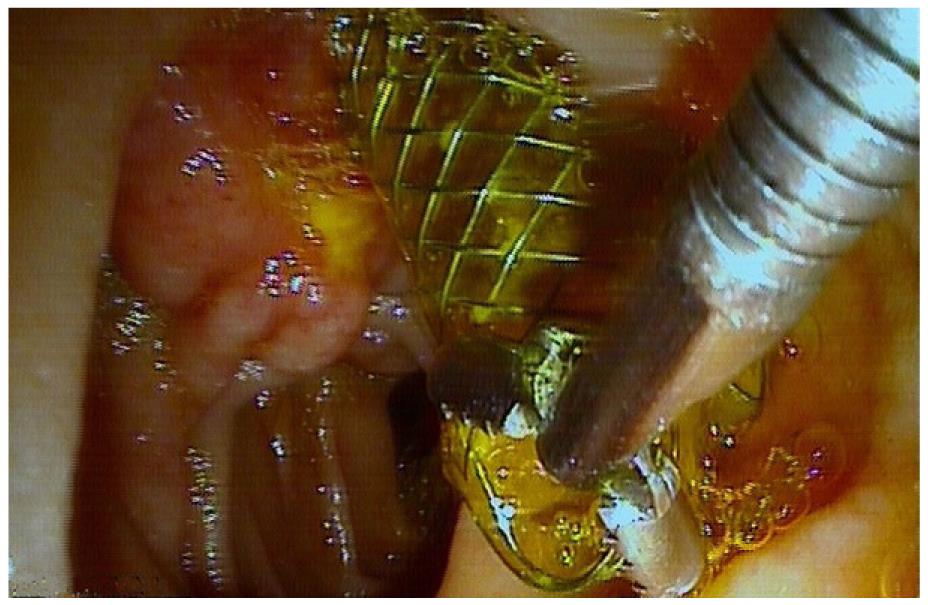
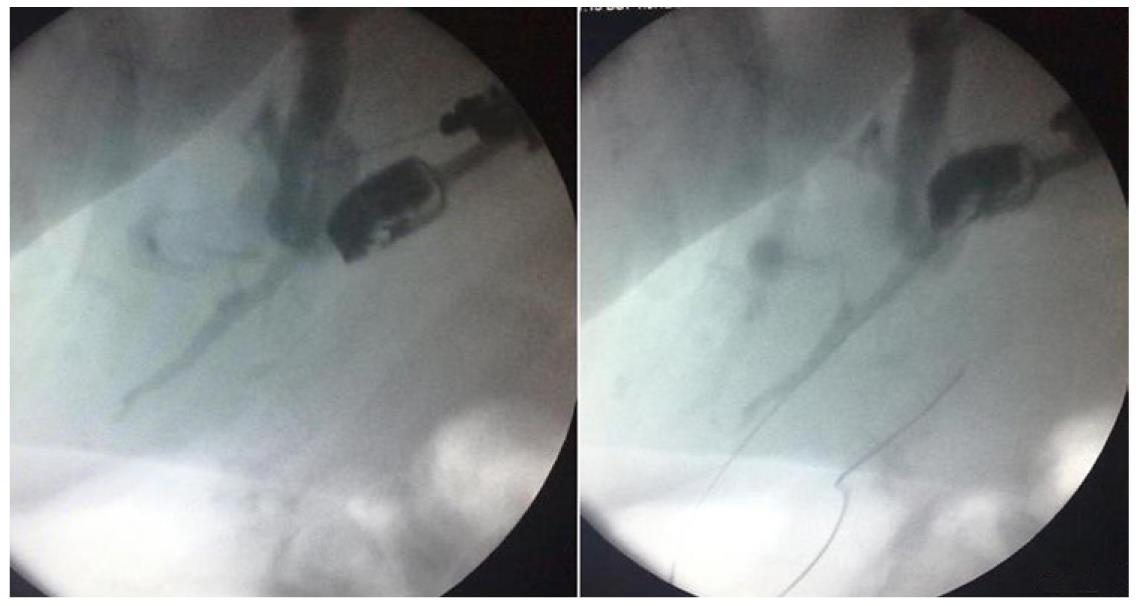
To facilitate extraction, the duodenal portion of the stent has to be placed into the duodenum more prominently than SEMS placed permanently in tumors. Some models have a distal strip or “lasso” for pulling out the stent. The Wallflex has a distal washer completely braided with the filamentary structure in a way that does not break when pulling it and facilitates its removal (Figures 1 and 2).
Care should be taken when the cystic duct opening is occluded by the stent, as cholecystitis can develop[11]. In the same way, if possible, a medium size sphincterotomy should be performed to facilitate pancreatic drainage. Upward migration into the bile duct makes extraction of the stent more challenging. Some FCSEMS with fins have been reported to injure the bile duct[12] and new bile duct strictures can develop in the upper part of the stent. An inferior rate of duodenal migration has been found with an anchoring flap FCSEMS compared with a model with flare ends. However, both FCSEMS were endoscopically retrieved without complications up to six months after insertion[13]. The ease of removal from the bile duct is one of the most important characteristics of FCSEMS in benign diseases. For instance, in one study, the fully covered Wallflex was extracted without difficulty after a mean of 119 d[14].
Until now the standard endoscopic treatment of benign biliary strictures (BBS) is progressive dilation with an increasing number of plastic stents. Bergman et al[15] achieved a long-term success rate (nine years of follow up) of 80% in postcholecystectomy BBS. They inserted two 10 Fr plastic stents during one year with exchange every three months. In similar patients, Costamagna et al[16] placed the maximum number of plastic stents (until four 10 Fr could be placed in the first ERCP) during a year with exchanges every three months and achieved a long-term success rate of 97.5% (Table 2).
| Treatment of benign biliary strictures |
| - Postcholecystectomy |
| - Post liver transplantation |
| - Chronic pancreatitis |
| - Papillary stenosis |
| - Bile duct stones and cholangitis |
| - Parasitic biliary infections |
| -Other forms of surgical biliary interventions and less frequent medical diseases such as primary sclerosing cholangitis or autoimmune pancreatitis |
| Treatment of biliary leaks |
| Sealing of papillary area perforations and bleeding after ERCP and biliary sphincterotomy |
| Extraction of biliary uncovered SEMS |
| EUS-guided biliary drainage |
Analogous protocols have been undertaken in postorthotopic liver transplantation BBS either anastomotic or non-anastomotic with good results[17,18], and in chronic pancreatitis[19] or in biliary sphincterotomy-associated distal common bile duct strictures[20].
Recently, FCSEMS have become commercially available and in some countries they have only received approval for malignant biliary strictures and not to treat BBS. Furthermore, as they have only been introduced in recent years there are few studies on their use compared with several other models of FCSEMS, and an even fewer number of studies comparing their efficacy with plastic stents, which still remain the standard for treatment of BBS[21]. Some studies on PCSEMS or FCSEMS in BBS are shown in Table 3[22-28].
| Author | No. ofpatients | Type ofstent | BBS etiology | Mean time to removal (mo) | Clinical success (%) |
| Cantu[22] | 14 | PCSEMS | CP | 21 | 37.50 |
| Kahaleh[23] | 79 | PCSEMS | CP/OLT/BS/IM/PS | 4 | 90 |
| Mahajan[24] | 44 | FCSEMS | CP/OLT/BS/IM/PS | 3.3 | 83 |
| Traina[25] | 16 | FCSEMS | OLT/LRLT | 2 | 81 |
| Park[13] | 43 | FCSEMS | CP/OLT/BS/PS | 6 | 84 |
| García- ano[26] | 14 | FCSEMS | IM/BS | 5.5 | 78.50 |
| Chaput[10] | 22 | PCSEMS | OLT | 2 | 52.60 |
| García-Pajares[27] | 22 | FCSEMS | OLT | 3.2 | 95.50 |
| Behm[28] | 22 | PCSEMS | CP | 5 | 72.70 |
However, FCSEMS are promising in the treatment of BBS for several reasons. It is technically difficult to place several stents during the initial endoscopic procedure due to the diameter of the stricture and the size of the bile duct below the stricture, whilst a single FCSEMS expands to a large diameter, equivalent to three 10 Fr stents and can remain in place for a prolonged period of time before removal. Plastic stents have a limited patency that requires frequent stent exchanges to prevent or manage stent occlusion. Although time to clinical occlusion appears to be prolonged when multiple stents are placed for BBS as compared to placement of a single stent[29], there remains a need for repeat procedures to replace stents until the endpoint of 1 year is reached. In addition, the small diameter delivery system of FCSEMS (8.5 Fr) allows placement without stricture dilation[30] enabling an easier endoscopic procedure.
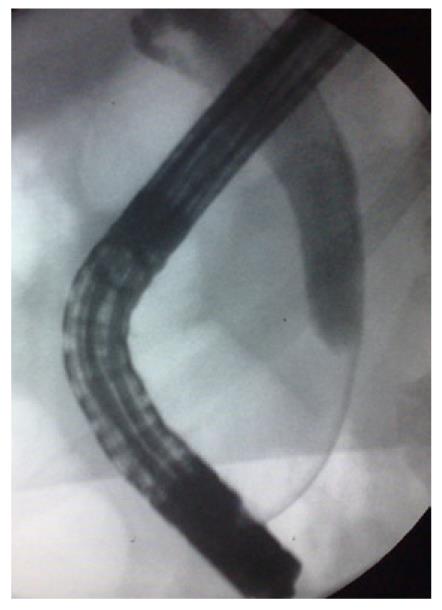
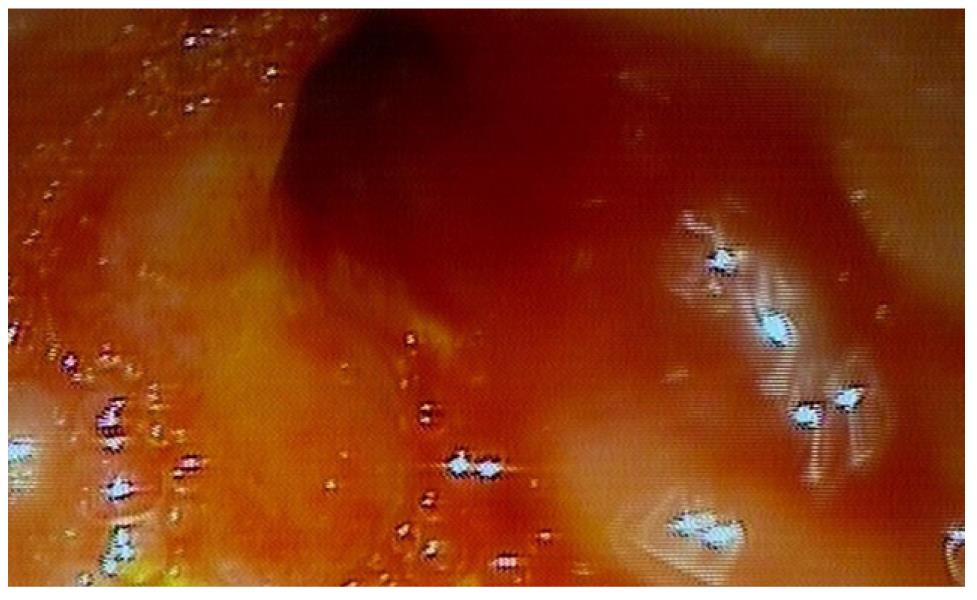
An example is shown in Figures 3 and 4. A papillary stenosis was successfully dilated with a single insertion of a FCSEMS during several months. In this way, despite the substantially higher cost of FCSEMS compared with plastic stents, this is offset by the number of procedures required to achieve stricture resolution.
Bile leaks typically occur following traumatic injury or surgical intervention, such as cholecystectomy, partial hepatic resection, and liver transplantation. A clinically significant postoperative bile leak occurs in 0.1%-0.5% of open cholecystectomies, 0.8%-2% of laparoscopic cholecystectomies, about 12% of cadaveric liver transplantations, and 6%-14% of hepatic resections[12]. ERCP has proved useful in treating BL by means of biliary sphincterotomy, stone extraction when present and plastic stent for nasobiliary drainage insertion[31]. These manoeuvres tend to divert flow away from the leak site. Stents can also bridge and seal the bile orifice responsible for the leak when it is present in the extrahepatic bile duct. Most leaks arise from the cystic duct stump, Luschka biliary branch or anastomosis in the bile duct.
Kahaleh et al[32] described the use of a 10 mm diameter Wallstent PCSEMS for the treatment of bile leaks following cholecystectomy (n = 15) and cadaveric liver transplantation (n = 1), in patients in whom conventional ERCP with stent placement had failed or who had co-morbidities that prevented multiple procedures. Although PCSEMS were effective in resolving bile leaks, they were unfortunately prone to migration and were difficult to remove after being in place for 6 mo, due to mucosal hyperplasia at the uncovered proximal end. In another study from Kahaleh’s group[12] concerning 13 patients with complex bile leaks, Viabil fully covered 10 mm diameter SEMS were placed. Complex leaks were defined as those that failed to close after endoscopic intervention with biliary sphincterotomy or plastic stent placement, bile leaks occurring after orthotopic liver transplantation (with or without surgical biliary stent placement), and complicated cholecystectomy with large bile leak. Successful resolution was achieved in all 13 patients. FCSEMS were removed in 11 at a mean of 156 d (range, 67-493 d). The other two patients died of unrelated causes before stent removal was attempted. No complications occurred following FCSEMS placement or removal. In five of the seven patients who underwent cholangioscopy at the time of stent removal, ulceration was seen where the anchoring fins were in contact with the bile duct. Easy removal and no biliary damage have been reported in a variety of biliary conditions (including an intrahepatic BL) treated with the Wallflex FCSEMS[33].
These are two feared complications of ERCP[34]. In both instances the FCSEMS has a mechanical compressive role. The covering allows the perforation to seal and to prevent fluid from leaking into the retroperitoneal space[26]. In haemorrhage the FCSEMS works by tamponading the bleeding site[35,36]. In both conditions, the stents are removed after several weeks.
FCSEMS can be used to induce pressure necrosis in the granulation tissue of uncovered SEMS when they require to be extracted and are embedded in the bile duct. For instance, if non-covered SEMS were inserted into benign strictures at a diagnostic stage which seemed neoplastic. This concept of “inducing pressure necrosis” with a FCSEMS on another uncovered SEMS was originally used to extract ultraflex SEMS from the esophagus[37]. Pérez-Miranda et al[38] first applied this method for the extraction of uncovered SEMS from the bile duct. This technique spread, and for example, an uncovered stent placed 1 year previously for a distal bile duct stricture from chronic pancreatitis, mistaken for pancreatic cancer, could be extracted after two FCSEMS were placed, the first for four months and the second for four weeks[39]. It is important that the FCSEMS diameter must be equal or superior to the non-covered SEMS to be extracted, otherwise, contact between them is not appropriate and pressure necrosis is not generated[26].
Endoscopic ultrasound allows transmural access to the bile duct (intra or extrahepatic) and subsequent contrast injection to provide ductal drainage under fluoroscopy using ERCP-based techniques[40]. This technique is known as endoscopic ultrasound cholangiopancreatography (EUSCP). As shown in Figure 5, the intrahepatic biliary tree is reached by means of a fine needle aspiration (FNA) device. The puncture in this case is made in the upper part of the stomach. Contrast medium is injected. Afterwards, several manoeuvres allow tract dilation and fistula formation between the stomach and the bile duct. A permanent drainage conduit can be maintained with a FCSEMS[41-44]. The puncture can also be made in the duodenal bulb or gastric antrum into the choledochus[45] or even in the gallbladder[45]. EUSCP has become an established salvage procedure after failed ERCP in the palliation of malignant biliary obstruction and facilitates bile duct drainage in benign conditions[46,47].
Technical developments have made FCSEMS possible and they are now widely available worldwide. In the majority of cases their removability is as easy as for plastic stents, although metallic materials, even covered, are always more prone to the formation of tissue hyperplasia than plastic material. For these reasons, six months is a reasonable time span to maintain, if necessary, FCSEMS in place before extraction. FCSEMS have recently been used for a variety of benign biliary disorders, although mostly for BBS. Potential advantages of FCSEMS over plastic stents are a reduction in the number of procedures and their complexity. Disadvantages include cost and potential complications. Randomized trials of plastic and FCSEMS are needed before these can be adopted in clinical practice for the treatment of benign biliary disorders. At present, it is necessary to individualize specific cases of benign biliary diseases necessitating stent drainage for the use of FCSEMS.
Peer reviewer: Everson Luiz de Almeida Artifon, MD, PhD, University of Sao Paulo School of Medicine, Rua Guimaraes Passos, 260-Apto 121 Vila Mariana-Sao Paulo-Sp-Brazil Zc-04107030, Brazil
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
| 1. | Huibregtse K, Tytgat GN. Palliative treatment of obstructive jaundice by transpapillary introduction of large bore bile duct endoprosthesis. Gut. 1982;23:371-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 130] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Costamagna G, Tringali A, Mutignani M, Perri V, Spada C, Pandolfi M, Galasso D. Endotherapy of postoperative biliary strictures with multiple stents: results after more than 10 years of follow-up. Gastrointest Endosc. 2010;72:551-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Germanidis G, Zavos C, Pilpilidis I, Paikos D, Papaziogas B. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc. 2008;22:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, Ott BJ, Farley DR, Farnell MB, Sarr MG. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007;142:448-54; discussion 454-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | García-Cano Lizcano J, González Martín JA, Taberna Arana L, Racionero M, Morillas Ariño MJ, Pérez Sola A. Plastic biliary stents in endoscopically irretrievable common bile duct stones. (Spanish). Revista de la Asociación Castellana de Aparato Digestivo (ACAD). 2003;19:3-6. |
| 6. | García-Cano Lizcano J, González Martín JA, Pérez Sola A, Morillas Ariño MJ. Success rate of complete extraction of common bile duct stones at first endoscopy attempt. Rev Esp Enferm Dig. 2002;94:340-350. [PubMed] |
| 7. | Dumonceau JM, Devière J, Delhaye M, Baize M, Cremer M. Plastic and metal stents for postoperative benign bile duct strictures: the best and the worst. Gastrointest Endosc. 1998;47:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Kahaleh M, Tokar J, Le T, Yeaton P. Removal of self-expandable metallic Wallstents. Gastrointest Endosc. 2004;60:640-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 110] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Ho H, Mahajan A, Gosain S, Jain A, Brock A, Rehan ME, Ellen K, Shami VM, Kahaleh M. Management of complications associated with partially covered biliary metal stents. Dig Dis Sci. 2010;55:516-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Chaput U, Scatton O, Bichard P, Ponchon T, Chryssostalis A, Gaudric M, Mangialavori L, Duchmann JC, Massault PP, Conti F. Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: a prospective, multicenter study. Gastrointest Endosc. 2010;72:1167-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | García-Cano J, Taberna-Arana L. Complications associated with the biliary fully covered Wallflex stent. Gastrointest Endosc. 2011;73:AB354. [DOI] [Full Text] |
| 12. | Wang AY, Ellen K, Berg CL, Schmitt TM, Kahaleh M. Fully covered self-expandable metallic stents in the management of complex biliary leaks: preliminary data - a case series. Endoscopy. 2009;41:781-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Park do H, Lee SS, Lee TH, Ryu CH, Kim HJ, Seo DW, Park SH, Lee SK, Kim MH, Kim SJ. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: a multicenter, prospective, comparative pilot study (with videos). Gastrointest Endosc. 2011;73:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | García-Cano J, Amao-Ruiz EJ, Taberna-Arana L. Treatment of benign distal biliary strictures with fully covered self-expanding metallic stents. Gastrointest Endosc. 2010;71:AB301. [DOI] [Full Text] |
| 15. | Bergman JJ, Burgemeister L, Bruno MJ, Rauws EA, Gouma DJ, Tytgat GN, Huibregtse K. Long-term follow-up after biliary stent placement for postoperative bile duct stenosis. Gastrointest Endosc. 2001;54:154-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 268] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 17. | Zoepf T, Maldonado-Lopez EJ, Hilgard P, Malago M, Broelsch CE, Treichel U, Gerken G. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006;12:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 142] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 18. | Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video). Gastrointest Endosc. 2010;71:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 19. | Catalano MF, Linder JD, George S, Alcocer E, Geenen JE. Treatment of symptomatic distal common bile duct stenosis secondary to chronic pancreatitis: comparison of single vs. multiple simultaneous stents. Gastrointest Endosc. 2004;60:945-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 118] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 20. | Pozsár J, Sahin P, László F, Topa L. Endoscopic treatment of sphincterotomy-associated distal common bile duct strictures by using sequential insertion of multiple plastic stents. Gastrointest Endosc. 2005;62:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | van Boeckel PG, Vleggaar FP, Siersema PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol. 2009;9:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 95] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 22. | Cantù P, Hookey LC, Morales A, Le Moine O, Devière J. The treatment of patients with symptomatic common bile duct stenosis secondary to chronic pancreatitis using partially covered metal stents: a pilot study. Endoscopy. 2005;37:735-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Kahaleh M, Behm B, Clarke BW, Brock A, Shami VM, De La Rue SA, Sundaram V, Tokar J, Adams RB, Yeaton P. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm? (with video). Gastrointest Endosc. 2008;67:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 164] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 24. | Mahajan A, Ho H, Sauer B, Phillips MS, Shami VM, Ellen K, Rehan M, Schmitt TM, Kahaleh M. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video). Gastrointest Endosc. 2009;70:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 25. | Traina M, Tarantino I, Barresi L, Volpes R, Gruttadauria S, Petridis I, Gridelli B. Efficacy and safety of fully covered self-expandable metallic stents in biliary complications after liver transplantation: a preliminary study. Liver Transpl. 2009;15:1493-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | García-Cano J, Taberna-Arana L, Jimeno-Ayllón C, Martínez-Fernández R, Serrano-Sánchez L, Reyes-Guevara AK, Viñuelas-Chicano M, Gómez-Ruiz CJ, Morillas-Ariño MJ, Pérez-García JI. Use of fully covered self-expanding metal stents for the management of benign biliary conditions. Rev Esp Enferm Dig. 2010;102:526-532. [PubMed] |
| 27. | García-Pajares F, Sánchez-Antolín G, Pelayo SL, Gómez de la Cuesta S, Herranz Bachiller MT, Pérez-Miranda M, de La Serna C, Vallecillo Sande MA, Alcaide N, Llames RV. Covered metal stents for the treatment of biliary complications after orthotopic liver transplantation. Transplant Proc. 2010;42:2966-2969. [PubMed] |
| 28. | Behm B, Brock A, Clarke BW, Ellen K, Northup PG, Dumonceau JM, Kahaleh M. Partially covered self-expandable metallic stents for benign biliary strictures due to chronic pancreatitis. Endoscopy. 2009;41:547-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Lawrence C, Romagnuolo J, Payne KM, Hawes RH, Cotton PB. Low symptomatic premature stent occlusion of multiple plastic stents for benign biliary strictures: comparing standard and prolonged stent change intervals. Gastrointest Endosc. 2010;72:558-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Baron TH. Covered self-expandable metal stents for benign biliary tract diseases. Curr Opin Gastroenterol. 2011;27:262-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 31. | Singh V, Singh G, Verma GR, Gupta R. Endoscopic management of postcholecystectomy biliary leakage. Hepatobiliary Pancreat Dis Int. 2010;9:409-413. [PubMed] |
| 32. | Kahaleh M, Sundaram V, Condron SL, De La Rue SA, Hall JD, Tokar J, Friel CM, Foley EF, Adams RB, Yeaton P. Temporary placement of covered self-expandable metallic stents in patients with biliary leak: midterm evaluation of a pilot study. Gastrointest Endosc. 2007;66:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | García-Cano J, Delgado-Torres V, Jimeno- Ayllón C. Initial experience with the new fully covered Wallflex® biliary stent used as a removable endoprosthesis in benign conditions. Endoscopy. 2009;41 (Suppl 1) A395. |
| 34. | García-Cano Lizcano J, González Martín JA, Morillas Ariño J, Pérez Sola A. Complications of endoscopic retrograde cholangiopancreatography. A study in a small ERCP unit. Rev Esp Enferm Dig. 2004;96:163-173. [PubMed] |
| 35. | Shah JN, Marson F, Binmoeller KF. Temporary self-expandable metal stent placement for treatment of post-sphincterotomy bleeding. Gastrointest Endosc. 2010;72:1274-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Itoi T, Yasuda I, Doi S, Mukai T, Kurihara T, Sofuni A. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011;43:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Evrard S, Le Moine O, Lazaraki G, Dormann A, El Nakadi I, Devière J. Self-expanding plastic stents for benign esophageal lesions. Gastrointest Endosc. 2004;60:894-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 141] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 38. | Pérez-Miranda M, González-Carro P, González-Huix F. Endoscopic removal of uncovered, partially and fully covered biliary SEMS: problems and salvage techniques. A GEPED Multicenter Descriptive Study. Gastrointest Endosc. 2008;67:AB93. [DOI] [Full Text] |
| 39. | Arias Dachary FJ, Chioccioli C, Deprez PH. Application of the "covered-stent-in-uncovered-stent" technique for easy and safe removal of embedded biliary uncovered SEMS with tissue ingrowth. Endoscopy. 2010;42 Suppl 2:E304-E305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 40. | Perez-Miranda M, de la Serna C, Diez-Redondo P, Vila JJ. Endosonography-guided cholangiopancreatography as a salvage drainage procedure for obstructed biliary and pancreatic ducts. World J Gastrointest Endosc. 2010;2:212-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Siddiqui AA, Sreenarasimhaiah J, Lara LF, Harford W, Lee C, Eloubeidi MA. Endoscopic ultrasound-guided transduodenal placement of a fully covered metal stent for palliative biliary drainage in patients with malignant biliary obstruction. Surg Endosc. 2011;25:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 42. | Park do H, Koo JE, Oh J, Lee YH, Moon SH, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided biliary drainage with one-step placement of a fully covered metal stent for malignant biliary obstruction: a prospective feasibility study. Am J Gastroenterol. 2009;104:2168-2174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 43. | Park do H, Song TJ, Eum J, Moon SH, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided hepaticogastrostomy with a fully covered metal stent as the biliary diversion technique for an occluded biliary metal stent after a failed ERCP (with videos). Gastrointest Endosc. 2010;71:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 44. | Nguyen-Tang T, Binmoeller KF, Sanchez-Yague A, Shah JN. Endoscopic ultrasound (EUS)-guided transhepatic anterograde self-expandable metal stent (SEMS) placement across malignant biliary obstruction. Endoscopy. 2010;42:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 45. | Artifon EL, Takada J, Okawa L, Moura EG, Sakai P. EUS-guided choledochoduodenostomy for biliary drainage in unresectable pancreatic cancer: a case series. JOP. 2010;11:597-600. [PubMed] |
| 46. | Kamata K, Kitano M, Kudo M, Imai H, Sakamoto H, Komaki T. Endoscopic ultrasound (EUS)-guided transluminal endoscopic removal of gallstones. Endoscopy. 2010;42 Suppl 2:E331-E332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Maranki J, Hernandez AJ, Arslan B, Jaffan AA, Angle JF, Shami VM, Kahaleh M. Interventional endoscopic ultrasound-guided cholangiography: long-term experience of an emerging alternative to percutaneous transhepatic cholangiography. Endoscopy. 2009;41:532-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |