Published online May 16, 2025. doi: 10.4253/wjge.v17.i5.106690
Revised: April 2, 2025
Accepted: April 24, 2025
Published online: May 16, 2025
Processing time: 61 Days and 22.4 Hours
Relative changes in the prevalence of gastrointestinal (GI) diseases have been reported worldwide over the past decades. However, data on changing trends of upper GI diseases remain scarce in sub-Saharan Africa. This study examines the shifting patterns of upper GI endoscopic findings over 35 years in Ethiopia.
To analyze trends in upper GI endoscopic findings over two distinct time periods, 35 years apart, in Ethiopia.
We extracted findings from 8412 upper GI endoscopies performed between 2016 and 2024 at a tertiary referral center in Addis Ababa, Ethiopia. Patient characteri
Between the two study periods, the male-to-female ratio of patients undergoing upper GI endoscopy shifted from 2:1 to 1.4:1, while the median patient age increased from 36 to 40 years. The proportion of patients older than 50 years doubled (14.6% to 30.2%), and referrals from outside Addis Ababa increased from 33% to 57%. The pre
This study sheds light on critical epidemiological shifts in upper GI diseases in Ethiopia, with a decline in peptic ulcer disease and a rise in portal hypertensive lesions and malignancies which have important public health implications. These findings underscore the need for increased awareness, improved clinical practices, enhanced resource allocation, and expanded access to early diagnosis and treatment of prevailing conditions. Preventive strategies targeting immunization and treatment of viral hepatitis, schistosomiasis, and Helicobacter pylori infection are urgently needed.
Core Tip: This study analyzes changing trends in upper gastrointestinal endoscopic findings, comparing two distinct time periods over 35 years. We reviewed 18412 exams, focusing on varices, esophageal cancer, gastric cancer, and strictures. Our analysis highlights significant shifts in the prevalence and detection rates of these conditions, providing valuable insights into the evolution of gastrointestinal disease patterns and the impact of advancements in endoscopic technology.
- Citation: Roro GM, Annose RT, Gilja OH. Changing trends in upper gastrointestinal endoscopic findings in Ethiopia: A comparison of eighteen thousand exams across two periods. World J Gastrointest Endosc 2025; 17(5): 106690
- URL: https://www.wjgnet.com/1948-5190/full/v17/i5/106690.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i5.106690
The global burden of digestive diseases is significant, accounting for more than one-third of the overall disease burden in 2019[1]. This burden varies considerably based on age, sex, sociodemographic index, and geographical region[2]. While enteric infections remain the primary contributor to incidence and mortality, cirrhosis has the highest prevalence rate[1]. Disease prevalence shifts over time due to variations in sociodemographic index, environmental and lifestyle factors, and exposure to different etiologies or risk factors[1]. For instance, the prevalence of metabolic syndrome associated steatotic liver disease and alcohol-associated cirrhosis are rising in several regions of the world and predicted to be the leading cause of prevalent cirrhosis, liver transplantation and death over the coming years due to rapidly rising prevalence of obesity, type 2 diabetes and alcohol consumptions in those regions[2]. The decline in the prevalence of peptic ulcer disease (PUD) over the past 100 years parallels the decline in the prevalence of Helicobacter pylori (H. pylori). On the contrary, nonsteroidal anti-inflammatory drugs-related PUD is on the rise[3,4].
Reports from various countries indicate substantial changes in the prevalence of upper gastrointestinal (GI) diseases over time, driven by sociodemographic shifts and evolving risk factors[3-6]. Ethiopia has also witnessed significant transformations over the past three to four decades, including improved healthcare and sociodemographic conditions, increased life expectancy, enhanced diagnostic capacity, declining H. pylori prevalence, and previously reported high rates of schistosomiasis and chronic viral hepatitis[7-11]. These evolving health dynamics influence the relative pre
Tikur Anbessa Specialized Hospital is a tertiary referral and teaching hospital under Addis Ababa University. Its endoscopy center, which has provided GI endoscopy services for over 50 years[15], has experienced periodic service interruptions but remains a key institution for gastroenterology training in Ethiopia. Since 2014, the center has been training gastroenterologists and currently serves as the World Gastroenterology Organization endoscopy training center in the country. Patients are referred from across Ethiopia, and both diagnostic and therapeutic procedures are performed by senior gastroenterologists and GI fellows under faculty supervision. A computerized database was established in 2016 to document all GI endoscopy procedures systematically. This study aims to analyze individual patient data and aggregate patient characteristics, indications, and endoscopic diagnoses over two distinct time periods to identify trends and changes over time.
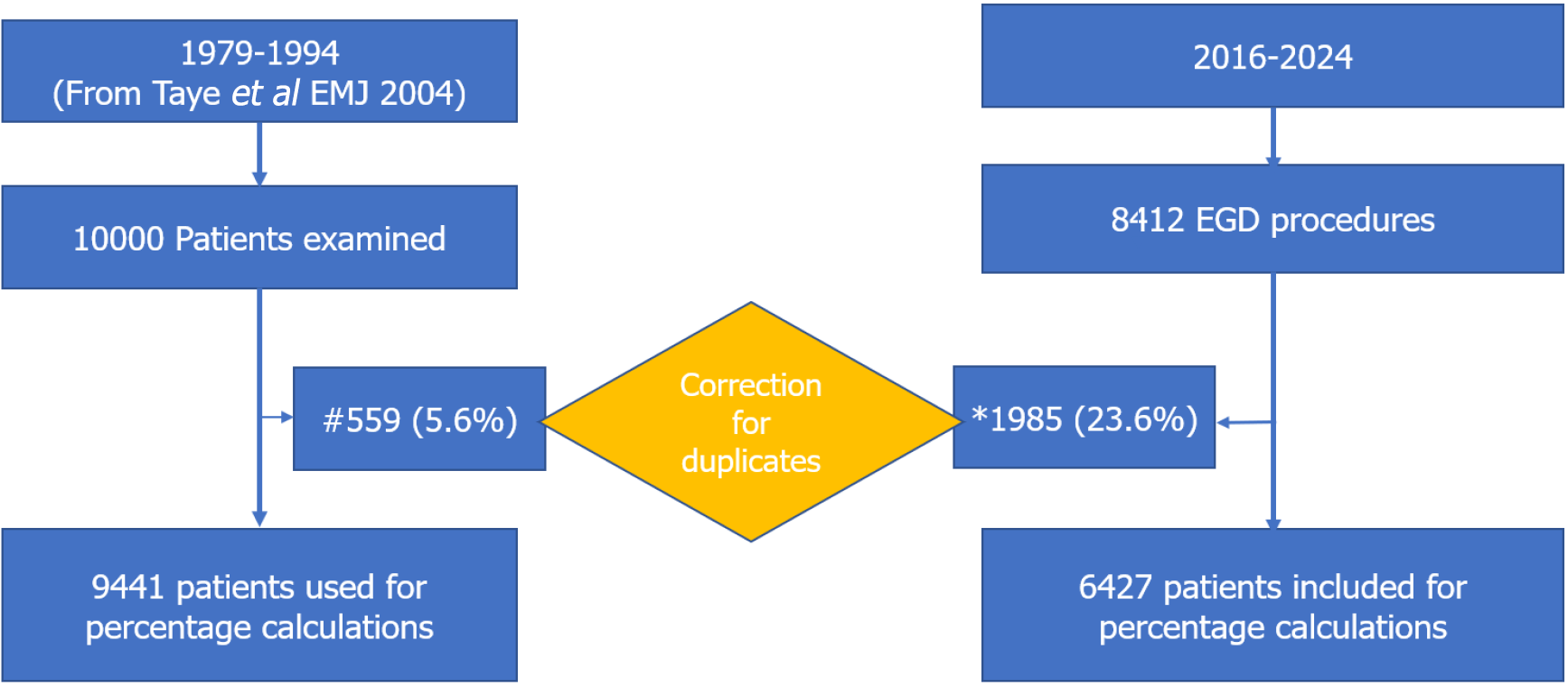
Records of patients who underwent upper GI endoscopy from 2016 to 2024 were extracted from the hospital’s database. The data was exported into Microsoft excel spread sheet and transferred into Stata 18. In patients with duplicate results due to multiple procedures done for the same patients with diagnosis or documented more than once due to multiple diagnosis in the same patient during a single procedure, only one major diagnosis is used for percentage calculation and comparison, to minimize chance of falsely inflating percentages of some diseases that inherently require repeat procedures. Typical examples were repeated variceal ligation after diagnosis of portal hypertension and multiple sessions of endoscopy for stricture dilatations which required an average of 1.6 procedures and 3.2 procedures per patient respectively. Patient demographic characteristics, indication for endoscopy and endoscopic diagnosis were analyzed using descriptive statistics, and presented tables and graphs. Data is available on request. These findings are compared to a similar report from the same endoscopy center published in 2004 in Ethiopian Medical Journal covering the time period from 1979-1994[15]. Percentage changes for the major upper GI findings were compared. The study is approved by the Institutional Review Board of the department of internal medicine, college of health sciences, Addis Ababa University.
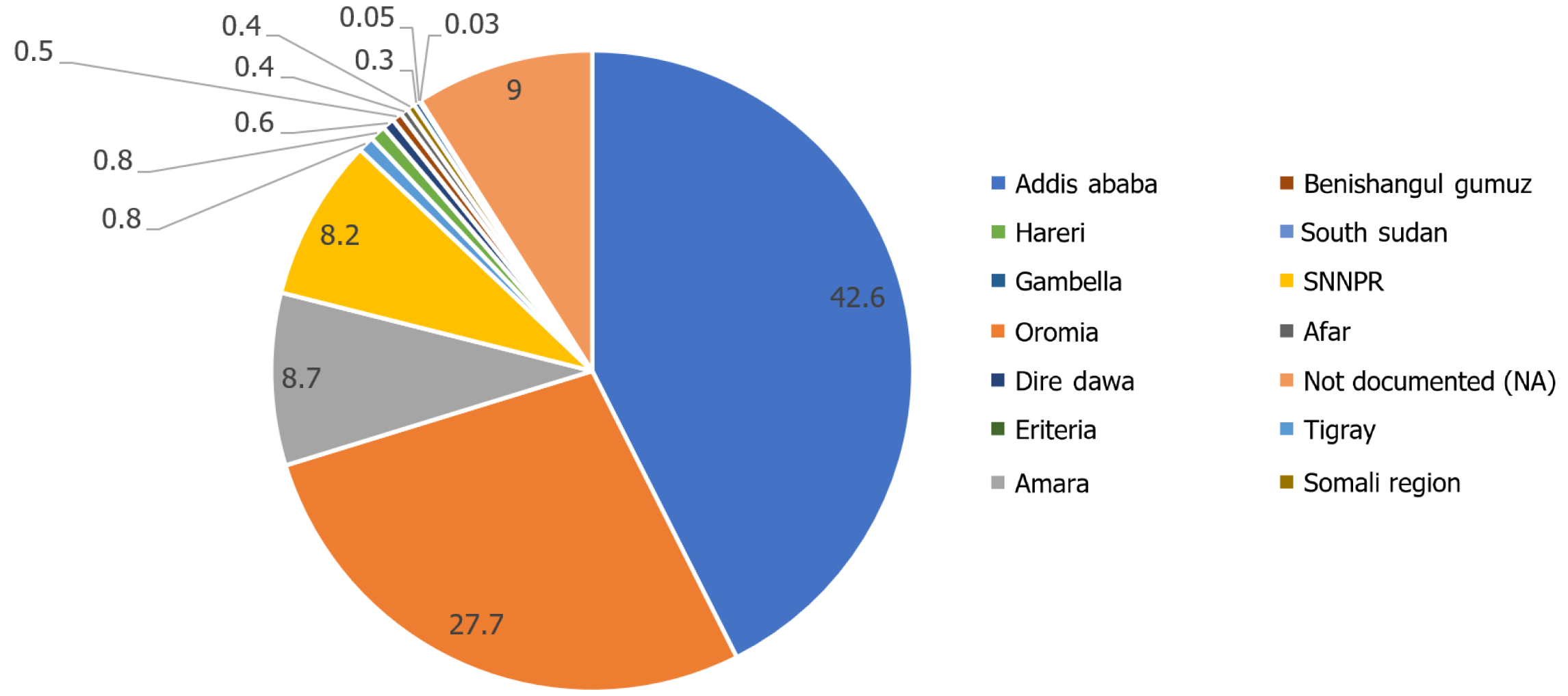
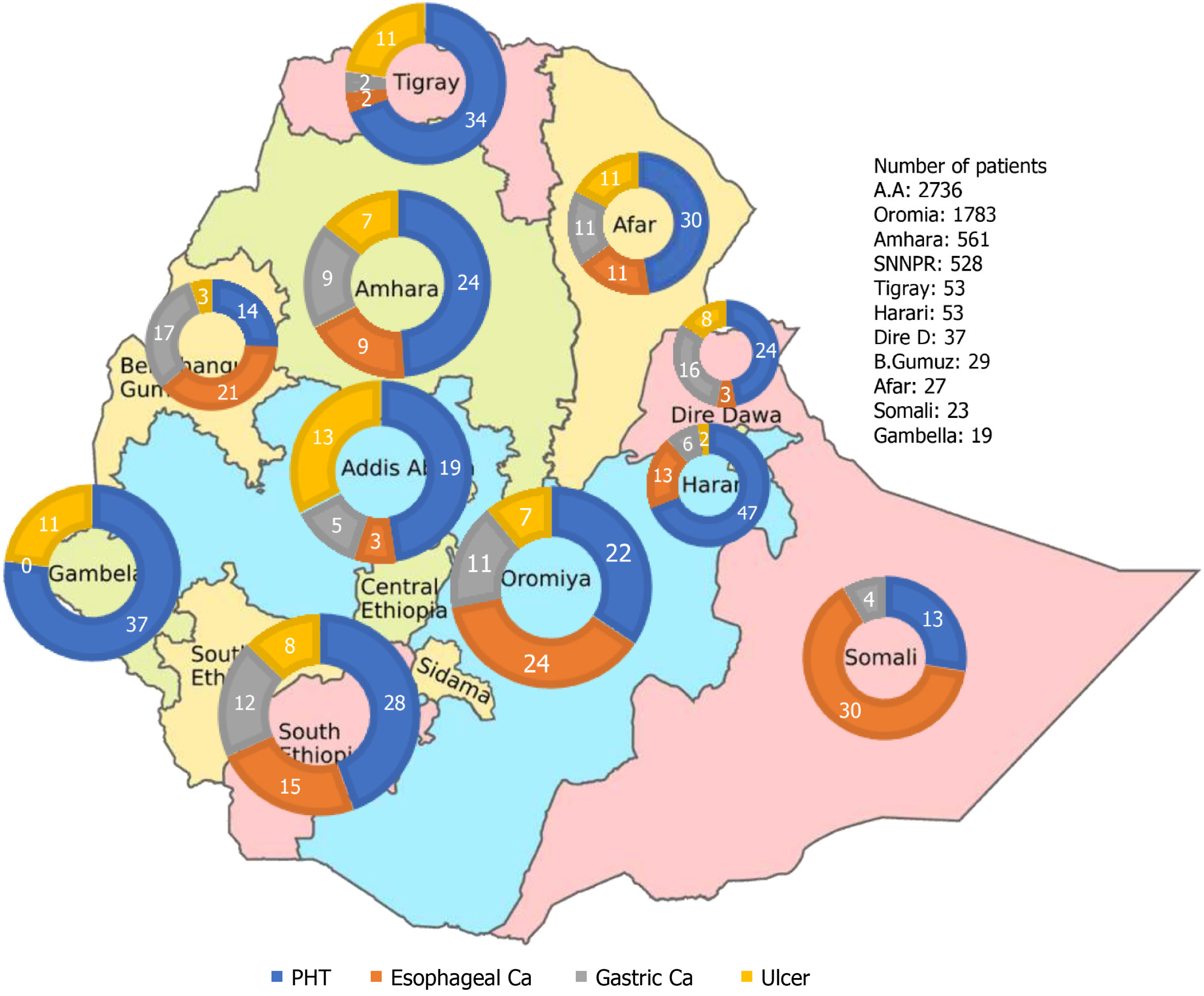
A total of 18412 upper GI endoscopy procedures were performed for 15868 patients during the two periods 1979-1994 and 2016-2024 (Figure 1). The male (65%) to female ratio was 2:1 during the 1979-1994 and currently is 1.4:1 (Table 1). The mean age was 36 (range: 5-96) and increased to 43 years (range: 3-100) and the proportion of patients age above 50 years increased from 14.6% to 32.6% over the two time periods. 67% of the patients evaluated during the initial period were from Addis Ababa while 57.4% of the current cohort came from all over the regions of Ethiopia and few patients from neighboring countries (Figure 2).
| 1979-1994[15] | 2016-2024 | |||||||
| Age | Male | Female | Total | Percent | Male | Female | Total | Percent |
| < 211 | 517 | 502 | 1019 | 10.2 | 327 | 229 | 556 | 8.7 |
| 21-30 | 1753 | 1200 | 2953 | 29.5 | 840 | 507 | 1347 | 21.0 |
| 31-40 | 1994 | 858 | 2852 | 28.5 | 666 | 534 | 1200 | 18.7 |
| 41-50 | 1243 | 477 | 1720 | 17.2 | 613 | 619 | 2132 | 19.2 |
| 51-60 | 633 | 304 | 937 | 9.4 | 603 | 519 | 1122 | 17.5 |
| 61-70 | 296 | 105 | 401 | 4.0 | 412 | 271 | 683 | 10.6 |
| > 702 | 73 | 45 | 118 | 1.2 | 187 | 100 | 287 | 4.5 |
| Total | 6509 (65) | 3491 (35) | 10000 | 100 | 3648 (57) | 2779 (43) | 6427 | 100 |
The most common indication was dyspepsia during both periods. Upper GI bleeding, screening for varices and dysphagia are other common indications for endoscopy. In the period 2016-2024 the average number of procedures per patient ratio is 1.3 overall and 3.2 procedures per patients with strictures, 1.6 for patients with gastroesophageal varices. After removing duplicated records, we used the corrected denominator number of patients (corrected n = 9441 and 6427) for percentage calculations for the two periods respectively (Table 2).
| Endoscopic findings | 1979-1994 (corrected n = 9441)[15] | 2016-2024 (corrected n = 6427) | ||||||
| Male | Female | Total | Percent | Male | Female | Total | Percent | |
| Ulcer diseases (DU + GU) | 2377 | 741 | 3118 | 33.0 | 328 | 147 | 475 | 7.4 |
| Duodenal luminal deformity (scar) and pyloric stenosis | 908 | 322 | 1230 | 13.0 | 102 | 36 | 138 | 2.1 |
| Gastroduodenitis1 | 635 | 338 | 973 | 10.3 | 483 | 424 | 907 | 14.1 |
| Gastroesophageal varices | 632 | 269 | 901 | 9.5 | 977 | 427 | 1404 | 21.8 |
| Gastric mass lesion | 160 | 98 | 258 | 2.7 | 284 | 207 | 491 | 7.6 |
| Esophagitis | 152 | 81 | 233 | 2.5 | 166 | 151 | 317 | 5.0 |
| Esophageal mass lesion | 52 | 34 | 86 | 0.9 | 335 | 385 | 720 | 11.2 |
| Hiatal hernia | 78 | 14 | 92 | 1.0 | 102 | 108 | 210 | 3.3 |
| Achalasia | 31 | 19 | 50 | 0.5 | 55 | 35 | 90 | 1.4 |
| stricture | 19 | 8 | 27 | 0.3 | 107 | 111 | 218 | 3.4 |
| Miscellaneous (others) | 146 | 75 | 221 | 2.3 | 202 | 177 | 379 | 6.0 |
| Normal | 1210 | 1042 | 2252 | 24.0 | 460 | 539 | 999 | 115.5 |
| Total | 6400 | 3041 | 9441 | 100 | 3648 | 2779 | 6427 | 100 |
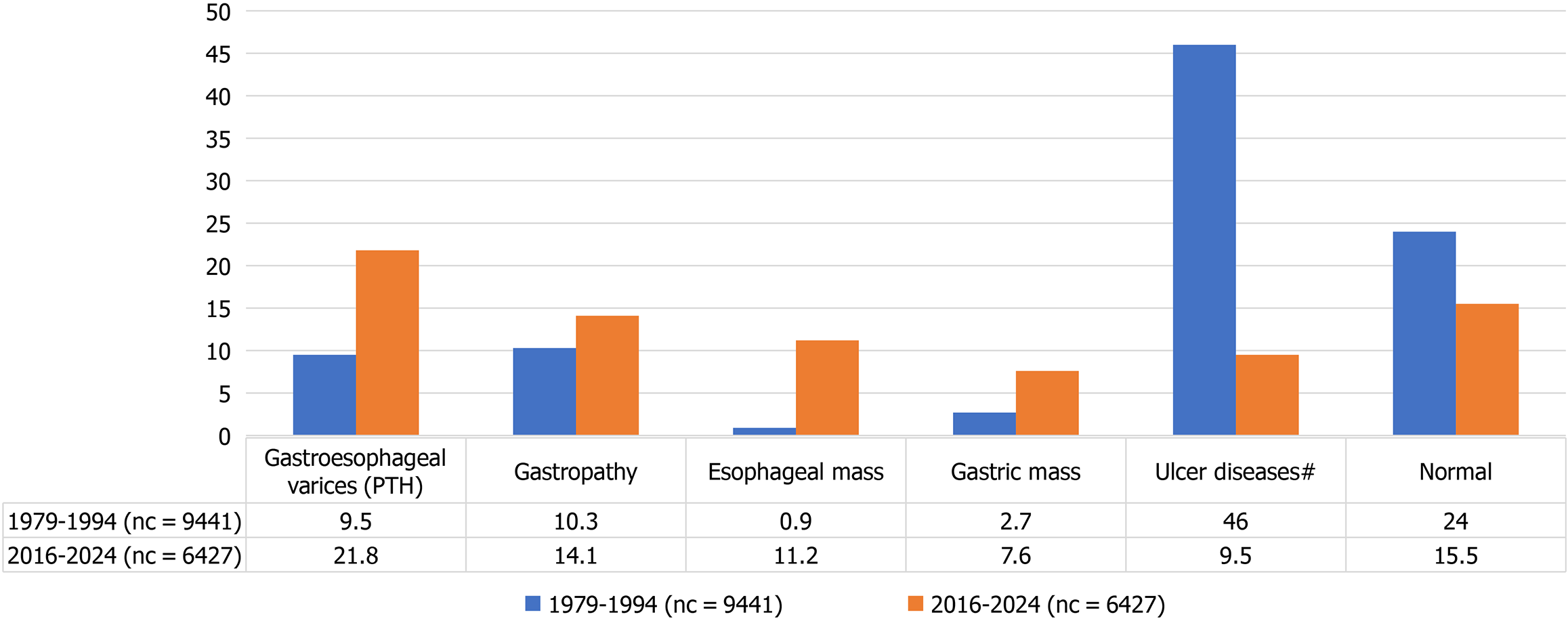
The most common endoscopic finding during the period 1979-1994 was ulcer diseases with duodenal ulcer of about 30% and chronic ulcer complications in additional 13% followed by gastroesophageal varices 9.5%. Ulcer diseases have declined dramatically to the current 7.4% while gastroesophageal varices have increased two-fold, currently at 21.8%. Gastroesophageal mass lesions were very rare with only 344/10000 (3.6%) of the total patients diagnosed during the 1979-1994. Esophageal mass lesions increased from less than 1% to the current 720/6427(11.1%) and gastric mass lesions increased from 2.7% to 491 (7.6%) (Table 3). Females are disproportionately affected by the mass lesions (Table 2).
| Diagnosis | Prevalence 1979-1994 | Prevalence 2016-2024 | P value |
| Esophageal mass lesion | 86/9441 (0.9) | 720/6427 (11.2) | 0.0000 |
| Ulcer diseases (DU + GU) | 3118/9441 (33.0) | 475/6427 (7.4) | 0.0000 |
| Gastroesophageal varices | 901/9441 (9.5) | 1404/6427 (21.8) | 0.0000 |
| Gastric mass lesion | 258/9441 (2.7) | 491/6427 (7.6) | 0.0000 |
| Hiatal hernia | 92/9441 (1.0) | 210/6427 (3.3) | 0.0000 |
| Achalasia | 50/9441 (0.5) | 90/6427 (1.4) | 0.0000 |
| Stricture | 27/9441 (0.3) | 218/6427 (3.4) | 0.0000 |
| Miscellaneous (others) | 221/9441 (2.3) | 379/6427 (5.9) | 0.0000 |
| Normal | 2252/9441 (23.9) | 999/6427 (15.5) | 0.0000 |
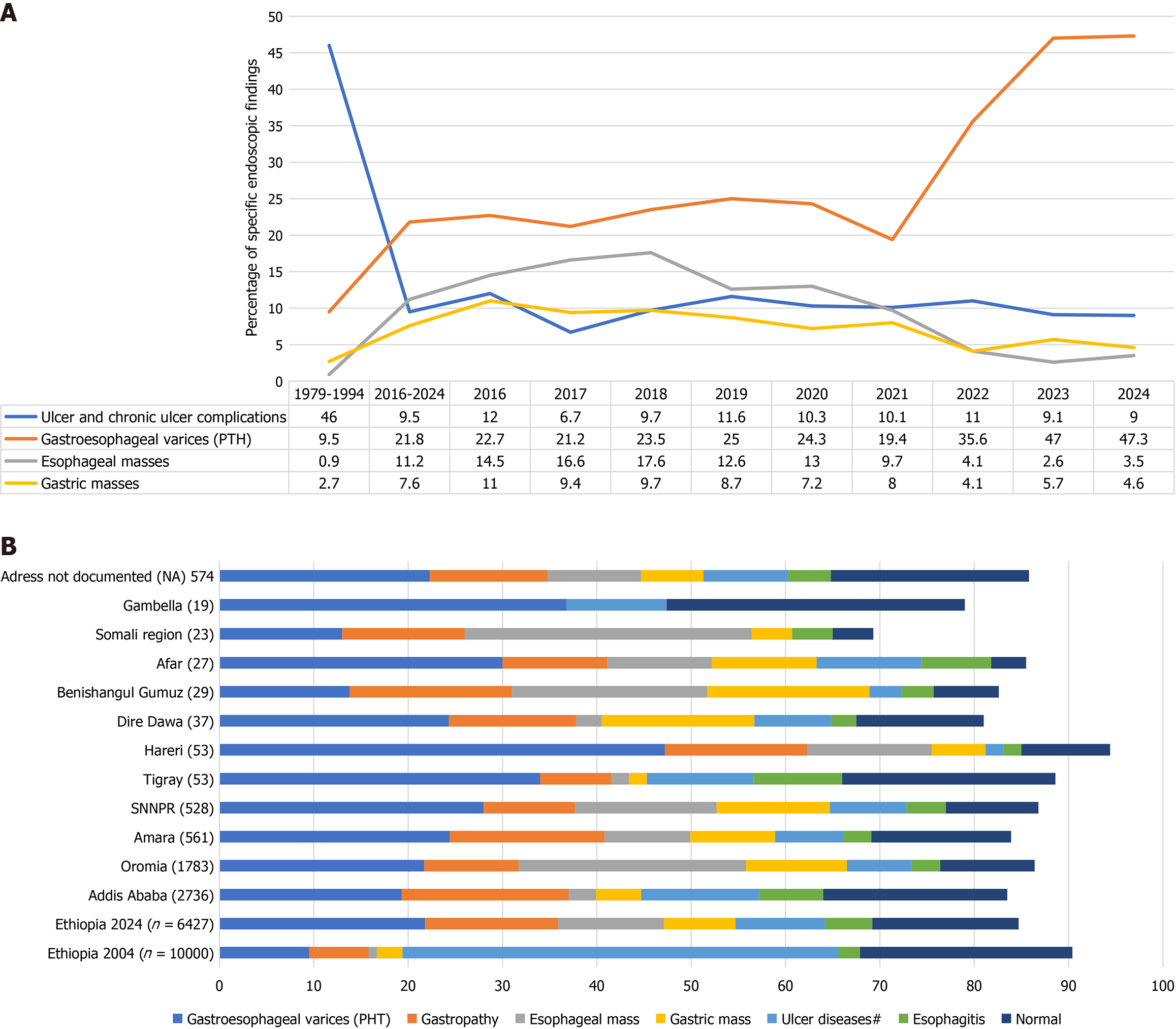
The proportion of patients diagnosed with gastritis (Gastropathy) has also increased (Figure 3). It is to be noted that the study published in 2004 and used as reference for this study described those lesions as acute gastritis and duodenitis reflecting association with H. pylori infections while the current documentation in the database used the term Gastropathy to emphasize most of these cases are patients with portal hypertension, matching the two prominent diagnosis in the two respective time periods. The proportions of patients with stricture, esophagitis, hiatal hernia and achalasia have also increased but the total numbers of patients with those diagnosis were limited. We also analyzed if the changes maintain consistent annual trend during the recent period compared to the aggregate percentages of the two periods. We found interesting changes over the time period (Figure 4A).
The proportion of patients with gastroesophageal varices has consistently increased and in 2024 almost half of the endoscopy procedures were done for either diagnosis or therapy of patients with portal hypertension. Ulcer diseases remained low ranging from 6.7%-12%. The proportion of patients with gastroesophageal masses has shown an initial increase reaching a maximum of 27.3% in 2018 and then a decreasing trend to about 8% since 2022 (Figure 4A). Analysis of the regional distribution of the major upper GI diseases also confirmed that portal hypertension and gastroesophageal masses dominate the picture in patients referred from most of the regions of Ethiopia. Portal hypertension and ulcers are more common than upper GI masses among patients from Addis Ababa, Tigray and Gambella (Figure 4B). Mass lesions and portal hypertension predominate in the other regions with the largest populations including Oromia (57%), Sothern Nations, Nationalities and Peoples’ Region (55%) and Amhara (42%) (Figure 5).
The scope of endoscopy services at our center has significantly expanded, evolving from primarily diagnostic procedures to include therapeutic interventions such as the treatment of bleeding lesions, stricture dilatation, foreign body removal, and stenting of stenotic lesions. Over the study period, the proportion of patients from regions outside Addis Ababa increased from 33% to 57.4%, with a notable rise in female beneficiaries from 35% to 43%. Historically, women in sub-Saharan Africa, including Ethiopia, have had limited access to healthcare due to cultural, financial, and logistical barriers[16,17] The increased utilization of endoscopy services by women in recent years may reflect improvements in healthcare accessibility, evolving sociocultural dynamics, and growing awareness of GI diseases. For instance, analysis of the nation-wide Community Health Program which was implemented since 2003, as part of primary health care services has revealed improvement in health knowledge, health care seeking and significant progress in many key health indicators in Ethiopia. It has also shown narrowing of the inequity among populations including between male and female as well as urban and rural[18].
A major finding of this study is the high prevalence of esophageal and gastric tumors among females, a pattern that contrasts with global trends. Esophageal tumors were identified in 14% of female patients compared to 9.2% of males, while gastric tumors were found in 7% of both genders. This represents a stark contrast to global data, where esophageal cancer is typically 2-3 times more common in men[19]. The median age for esophageal cancer in our study (54 years) is also younger than the African average[20]. These findings suggest that unique risk factors may be contributing to this pattern in Ethiopia, warranting further investigation into dietary, genetic, and environmental exposures.
We also observed a decline in PUD, aligning with global trends[3-6]. This decline correlates with a decrease in H. pylori prevalence, which has dropped from 64.4% in 1990-2000 to 42.9% in 2012-2017 in Ethiopia[9]. This reduction is attributed to improved sanitation, healthcare access, and early eradication strategies[7,9,18]. However, while duodenal ulcer cases have decreased, the incidence of gastric cancer has not followed the same trajectory. This is likely due to the long latency period between H. pylori infection and gastric malignancy, as the progression from chronic gastritis to intestinal metaplasia and adenocarcinoma can take decades[21]. This observation mirrors historical trends in Europe and Asia, where initial declines in H. pylori prevalence preceded a delayed reduction in gastric cancer incidence[3-6].
A regional disparity in upper GI malignancies was noted, with Oromia (35%), Somali (35%), Benishangul-Gumuz (38%), and Southern Nation Nationality People Region (27%) exhibiting the highest rates. Previous studies have identified Arsi and Bale zones of Oromia as esophageal cancer hotspots and our findings reaffirm these trends[22-23]. Interestingly, while Arsi remains a major contributor (20% of total cases), the proportion of patients from Bale has declined (3.3%), suggesting possible changes in healthcare access or referral patterns. The recent establishment of new endoscopy centers in regional hospitals may explain the relative decline in gastroesophageal tumor cases at our center since 2022, as patients are increasingly being diagnosed locally rather than referred to Addis Ababa[22].
Conversely, the proportion of patients with gastroesophageal varices has dramatically increased, a trend likely driven by portal hypertension due to chronic viral hepatitis (hepatitis B virus and hepatitis C virus) and schistosomiasis. Ethiopia has a moderate to high prevalence of chronic viral hepatitis, with hepatitis B virus affecting 7.4% and hepatitis C virus affecting 3.1% of the population[10]. Additionally, more than half of Ethiopia’s districts are schistosomiasis-endemic, with an estimated 37 million people at risk[11]. These infections are key contributors to portal hypertension, esophageal varices, and associated complications[24]. Our findings align with recent studies from Sudan and Zambia, where similar increases in esophageal varices and decreases in duodenal ulcer prevalence have been reported over the past four decades[12,13]. The observed rise in variceal cases at our center may also be influenced by referral bias, as regional hospitals are now capable of diagnosing malignancies but continue to send patients with portal hypertension-related complications to Addis Ababa for specialized care[22].
Given the shifting burden of upper GI diseases, targeted public health interventions are needed to improve early detection, enhance access to treatment, and prevent disease progression. Key recommendations include: (1) Expanding endoscopic services beyond referral hospitals to increase early detection of malignancies and portal hypertension-related complications; (2) Strengthening H. pylori eradication programs, given its established link to gastric cancer and significant impact of eradication on malignancy reduction across all base line risk of gastric cancer incidence from asymptomatic infection to atrophic gastritis and/or intestinal metaplasia and even after endoscopic removal of early gastric cancer[9,15,21]; (3) Increasing hepatitis B vaccination coverage and promoting the use of effective antiviral therapy to reduce chronic liver disease and prevent progression to portal hypertension[25,26]; (4) Enhancing schistosomiasis control measures, including mass drug administration and improved sanitation, to mitigate its contribution to periportal fibrosis and portal hypertension[11]; (5) Implementing gender-specific health education and economic empowerment initiatives to sustain the improvement in female healthcare access[17,18]; and (6) Improving blood transfusion safety and availability, particularly for managing variceal bleeding in patients with portal hypertension.
This study presents significant strengths in its effort to understand the evolving trends of upper GI diseases in Ethiopia over a 35-year period. With a large sample size of 18412 endoscopic exams and long-term comparisons, the study provides robust statistical power. The focus on Ethiopia, an understudied sub-Saharan African population, adds sub
However, we acknowledge certain limitations. Changes in endoscopic technology over the study period may have improved diagnostic accuracy, potentially influencing the observed trends. Despite efforts to harmonize evolving diagnostic criteria, minor inconsistencies may persist. Referral patterns over the study period may have changed; with our study likely representing more severe cases due to referral patterns, which may have influenced the reported trends. The possibility of subtle shifts influencing results cannot be entirely excluded. Furthermore, findings from Ethiopia may not be fully generalizable to other sub-Saharan African countries due to regional differences in healthcare systems and disease prevalence. Lastly, as with any long-term observational study, some residual bias from unmeasured confounding factors may exist. Despite these limitations, the study’s findings contribute meaningful knowledge to the understanding of upper GI disease trends and provide actionable insights for public health planning and clinical practice.
This study reveals a significant epidemiological shift from predominantly benign PUDs to more severe conditions such as portal hypertension and upper GI malignancies over the past three decades. The findings align with trends observed in Ethiopia, Sudan, and Zambia, suggesting broad regional changes in disease patterns due to risk factor modifications, evolving healthcare access, and lifestyle changes. Given these shifts, early detection programs, targeted screening strategies, and improved access to preventive and therapeutic interventions are urgently needed to reduce the growing burden of upper GI diseases in Ethiopia.
We extend our sincere gratitude to the staff and colleagues of the endoscopy unit for their meticulous documentation of patient records. Our heartfelt thanks also go to the staff and administration of the Gastroenterology unit for their invaluable assistance and active participation in this endeavor. We are deeply grateful to the patients. We acknowledge Professor Mark Topazian for his critical contributions in thoroughly refining the manuscript, ensuring its quality and clarity. Additionally, we express our profound appreciation to Dr. Amir Sultan for his exceptional efforts in establishing a functional computer database at our endoscopy center, which has been instrumental in providing reliable data for this work.
| 1. | Wang Y, Huang Y, Chase RC, Li T, Ramai D, Li S, Huang X, Antwi SO, Keaveny AP, Pang M. Global Burden of Digestive Diseases: A Systematic Analysis of the Global Burden of Diseases Study, 1990 to 2019. Gastroenterology. 2023;165:773-783.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 72] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 2. | Huang DQ, Terrault NA, Tacke F, Gluud LL, Arrese M, Bugianesi E, Loomba R. Global epidemiology of cirrhosis - aetiology, trends and predictions. Nat Rev Gastroenterol Hepatol. 2023;20:388-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 368] [Article Influence: 184.0] [Reference Citation Analysis (0)] |
| 3. | Musumba CO, Van Eker D, Jorgensen A, Pritchard M, Pirmohamed M. Changing trends in peptic ulcer disease: the rise of NSAID-induced and fall of H pylori-induced ulcers. Gut. 2011;60:A104-A105. [DOI] [Full Text] |
| 4. | Xie X, Ren K, Zhou Z, Dang C, Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol. 2022;22:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 101] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 5. | Roberts-Thomson IC. Rise and fall of peptic ulceration: A disease of civilization? J Gastroenterol Hepatol. 2018;33:1321-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Goh KL, Wong HT, Lim CH, Rosaida MS. Time trends in peptic ulcer, erosive reflux oesophagitis, gastric and oesophageal cancers in a multiracial Asian population. Aliment Pharmacol Ther. 2009;29:774-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | GBD 2019 Ethiopia Subnational-Level Disease Burden Initiative Collaborators. Progress in health among regions of Ethiopia, 1990-2019: a subnational country analysis for the Global Burden of Disease Study 2019. Lancet. 2022;399:1322-1335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 51] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 8. | Jembere GB, Cho Y, Jung M. Decomposition of Ethiopian life expectancy by age and cause of mortality; 1990-2015. PLoS One. 2018;13:e0204395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Melese A, Genet C, Zeleke B, Andualem T. Helicobacter pylori infections in Ethiopia; prevalence and associated factors: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Belyhun Y, Maier M, Mulu A, Diro E, Liebert UG. Hepatitis viruses in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2016;16:761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 11. | Leta GT, Mekete K, Wuletaw Y, Gebretsadik A, Sime H, Mekasha S, Woyessa A, Shafi O, Vercruysse J, Grimes JET, Gardiner I, French M, Levecke B, Drake L, Harrison W, Fenwick A. National mapping of soil-transmitted helminth and schistosome infections in Ethiopia. Parasit Vectors. 2020;13:437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | EI Shallaly GEHA, Ibrahim BAB, Mohamed Ahmed HEH, Elhajahmed MMI, Salih MME, Mohammed MFE, AOAli I. The change in upper gastrointestinal disease pattern in Sudan. Ann Gastroenterol Dig Syst. 2021;4:1047. |
| 13. | Kayamba V, Sinkala E, Mwanamakondo S, Soko R, Kawimbe B, Amadi B, Zulu I, Nzaisenga JB, Banda T, Mumbwe C, Phiri E, Munkonge P, Kelly P. Trends in upper gastrointestinal diagnosis over four decades in Lusaka, Zambia: a retrospective analysis of endoscopic findings. BMC Gastroenterol. 2015;15:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Argaw AM, Ethiopia SS, Lelisa G, Fisseha H, Mulugeta B. Indications and Findings of Upper Gastrointestinal Endoscopy at a Tertiary Hospital in Ethiopia: A Cross-Sectional Study. Clin Exp Gastroenterol. 2023;16:187-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Taye M, Kassa E, Mengesha B, Gemechu T, Tsega E. Upper gastrointestinal endoscopy: a review of 10,000 cases. Ethiop Med J. 2004;42:97-107. [PubMed] |
| 16. | Fentie EA, Asmamaw DB, Negash WD, Belachew TB, Amare Baykeda T, Addis B, Tamir TT, Wubante SM, Endawkie A, Zegeye AF, Kidie AA, Fetene SM. Spatial distribution and determinants of barriers of health care access among female youths in Ethiopia, a mixed effect and spatial analysis. Sci Rep. 2023;13:21517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 17. | Zegeye B, Adjei NK, Ahinkorah BO, Ameyaw EK, Budu E, Seidu A, Idriss-wheeler D, Yaya S. Barriers and Facilitators to Accessing Health Care Services among Married Women in Ethiopia: a Multi-level Analysis of the Ethiopia Demographic and Health Survey. Int J Transl Med Res Public Health. 2021;5:183-196. [DOI] [Full Text] |
| 18. | Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003-2018: successes and challenges toward universal coverage for primary healthcare services. Global Health. 2019;15:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 120] [Cited by in RCA: 232] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 19. | Liu CQ, Ma YL, Qin Q, Wang PH, Luo Y, Xu PF, Cui Y. Epidemiology of esophageal cancer in 2020 and projections to 2030 and 2040. Thorac Cancer. 2023;14:3-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 158] [Reference Citation Analysis (0)] |
| 20. | Asombang AW, Chishinga N, Nkhoma A, Chipaila J, Nsokolo B, Manda-Mapalo M, Montiero JFG, Banda L, Dua KS. Systematic review and meta-analysis of esophageal cancer in Africa: Epidemiology, risk factors, management and outcomes. World J Gastroenterol. 2019;25:4512-4533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (1)] |
| 21. | Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, Graham DY. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology. 2016;150:1113-1124.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 737] [Cited by in RCA: 674] [Article Influence: 74.9] [Reference Citation Analysis (0)] |
| 22. | Deybasso HA, Roba KT, Nega B, Belachew T. Clinico-Pathological Findings and Spatial Distributions of Esophageal Cancer in Arsi Zone, Oromia, Central Ethiopia. Cancer Manag Res. 2021;13:2755-2762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Zena D, Hisa F, Hurrisa Z, Kaso M. Patterns of upper gastrointestinal diseases among patients undergoing esophagogastroduodenoscopy at three hospitals in Asella town, Southeast Ethiopia. Sci Rep. 2024;14:24067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 24. | Tamarozzi F, Fittipaldo VA, Orth HM, Richter J, Buonfrate D, Riccardi N, Gobbi FG. Diagnosis and clinical management of hepatosplenic schistosomiasis: A scoping review of the literature. PLoS Negl Trop Dis. 2021;15:e0009191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Pattyn J, Hendrickx G, Vorsters A, Van Damme P. Hepatitis B Vaccines. J Infect Dis. 2021;224:S343-S351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 135] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 26. | Sinclair S 3rd, Shearen S, Ghobrial Y, Trad G, Abdul Basit S, Shih D, Ryan JK. Review of the Effects of Antiviral Therapy on Hepatitis B/C-Related Mortality and the Regression of Fibrosis. Viruses. 2024;16:1531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |