Published online May 16, 2021. doi: 10.4253/wjge.v13.i5.115
Peer-review started: August 25, 2020
First decision: December 11, 2020
Revised: December 26, 2020
Accepted: April 7, 2021
Article in press: April 7, 2021
Published online: May 16, 2021
Processing time: 256 Days and 3.9 Hours
Obesity has evolved into a global pandemic. The prevalence of obesity and hypertension in eastern North Carolina are comparable, if not higher, than the national prevalence. In the United States, an estimated 34% of adults have hypertension, the most modifiable risk factor for heart disease and stroke. Lifestyle and pharmacological interventions often do not provide sustained weight loss in obese patients. Bariatric surgery offers an effective weight reduction with short-and long-term health improvements; however, a higher body mass index is associated with higher surgical morbidity and mortality, longer hospitalization, and increasing rates of 30-day readmission due to co-morbidities. Intragastric balloon may bridge a critical gap in the treatment of obesity. The objective of this paper is to showcase the impact of endoscopic bariatric therapy on blood pressure reduction.
To investigate the impact of intragastric balloon on blood pressure reduction.
A retrospective chart review was conducted from January 1, 2016 to January 31, 2019 of consecutive adults who received intragastric balloon therapy (IGBT) in a gastroenterology private practice in Eastern North Carolina. The balloon was introduced into the stomach under endoscopic guidance, and while in the region of the gastric body, inflation with saline was performed at increments of 50 mL until target volume between 500 to 650 mL of saline was attained depending on the patient's gastric capacity. No procedural complications were noted during endoscopic placement and removal of the balloon. A cohort study design was used for data analysis. A total of 172 patients had the Orbera® intragastric balloon placed. Of the 172 patients who had IGBT at baseline, 11 patients (6.4%) requested early balloon removal due to foreign body sensation (n = 1), and/or intolerable gastrointestinal adverse events (n = 10). The reported gastrointestinal adverse events were nausea, vomiting, abdominal pain, and diarrhea. Eventually, 6-mo follow-up data were available for only 140 patients. As a result, only the 140 available at the 6-mo follow-up were included in the analysis. Univariate, bivariate, and multivariate statistical analyses were performed. Specifically, scatterplots were created to show the relationship between weight and blood pressure, and paired two-sample t-test was carried out to determine if there was a significant reduction in weight before and after the IGBT. Multiple regressions were also performed to examine the association between participants’ total body weight and blood pressure. The outcome variables for the multiple regression were systolic and diastolic blood pressure measured as continuous variables. This was followed by logistic regression analyses to determine the association between total body weight and hypertension at 6-mo post-implantation. The outcome variables for the logistic regression were systolic blood pressure–non-hypertensive (140 mmHg or less) or hypertensive (greater than 140 mmHg), and diastolic blood pressure–non-hypertensive (90 mmHg or less) or hypertensive (greater than 90 mmHg). All authors had access to the study data and reviewed and approved the final manuscript. All statistical analyses were done using STATA 14®.
The study included 15% males and 85% females. 50% of the patients were white and just over 22% were non-white, and about 27% declined to give their race. The average baseline patients’ weight prior to IGBT was 231.61 Lbs. (SD = 46.53 Lbs.). However, the average patients’ weight after IGBT at the 6-mo follow-up was 203.88 Lbs. (SD = 41.04 Lbs.). Hence, on average, the percent total body weight loss at 6-mo is 11.97 after IGBT. The logistic regression performed revealed that weight (β = 0.0140, P < 0.000) and age (β = 0.0534, P < 0.000) are important factors in determining systolic blood pressure after IGBT. None of the other demographic characteristics or indicated comorbidities were found to be significant.
IGBT can be an effective short-term weight reduction modality with a relatively little risk of adverse event. Due to its improvement on systolic blood pressure, IGBT may help reduce cardiovascular risk.
Core Tip: Obesity is one of the leading causes of preventable life-years lost among Americans. Adults who have obesity compared with adults at a healthy weight have an increased risk of developing serious health conditions including hypertension. The treatment of hypertension in obesity is complicated by a high prevalence of resistant hypertension, as well as unpredictable hemodynamic effects of many medications. Weight loss stabilizes neurohormonal activity and causes clinically significant reductions in blood pressure. While lifestyle interventions can improve blood pressure, they fail to consistently yield sustained weight loss and have not demonstrated long-term benefits. Weight loss promotes dramatic declines in blood pressure and attenuation of long-term cardiovascular risk.
- Citation: Samuel GO, Lambert K, Asagbra E, Harvin G, Ibegbu E. Impact of intragastric balloon on blood pressure reduction: A retrospective study in Eastern North Carolina. World J Gastrointest Endosc 2021; 13(5): 115-124
- URL: https://www.wjgnet.com/1948-5190/full/v13/i5/115.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i5.115
Obesity with its associated devastating consequences has evolved into a global pandemic and a major health concern[1]. In the United States, an estimated 34% of adults have hypertension (approximately 8.7 million people), which is the most modifiable risk factor for heart disease and stroke[2]. Lifestyle interventions often do not provide sustained weight loss for people who are obese[2]. While 4.5%-11% total body weight loss can be achieved with pharmacological agents, some patients cannot achieve enough weight loss with lifestyle modifications and medication alone[3]. The pharmacological agents indicated for weight reduction often have limited data for long term effects or intolerable side effect profile[4]. Bariatric surgery is the most effective weight reduction intervention with short- and long-term health improvements; however, a higher body mass index is associated with higher surgical morbidity and mortality, longer hospitalization, and increasing rates of 30-d readmission due to co-morbidities[5-8]. In addition, risks may outweigh the benefits in those with a greater body mass index. While the mortality rates associated with bariatric surgery have decreased, the complication rates remain high with one meta-analysis citing a complication rate of 17% and a reoperation rate of 7%[9]. In addition, only 1% of patients eligible for bariatric surgery ultimately undergo the procedure[3]. Minimally invasive non-surgical options may bridge a critical gap in the treatment of obesity[10,11].
One of the most widely studied of the endoscopic bariatric therapies is Orbera, which is an intragastric balloon approved for a body mass index of 30-40 kg/m2[11]. It is a spherical silicone device, filled with saline, that is endoscopically implanted and removed with an approved indication of placement for six months[10,11]. It promotes weight loss by its effect as a space occupying device and altering gut hormones, however the mechanism is not quite clear[11]. One study showed that weight loss achieved with Orbera was 11.3% and excess weight loss measured was 25.4%[9]. Comorbidity improvement occurs at a 10% body weight reduction[1,12,13].
Limited studies have evaluated the efficacy of Orbera and its influence on co-morbidities. Genco et al[14] demonstrated in an Italian study significant improvement and resolution of pre-operative complications (hypertension, diabetes, respiratory disorders, osteoarthritis, and dyslipidemia) in 89.1% patients. There was a 44.8% resolution of hypertension; yet, there is an insufficient amount of data analyzing the association of weight loss with blood pressure reduction.
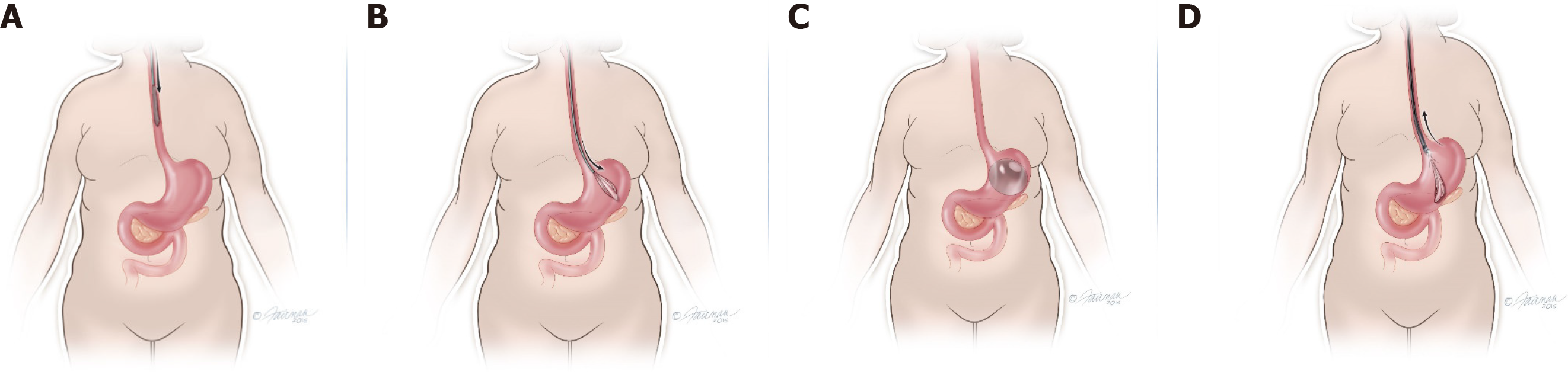
A retrospective chart review was conducted from January 1, 2016 to January 31, 2019 of consecutive adults who received intragastric balloon therapy (IGBT) in a gastroenterology private practice in Eastern North Carolina. The balloon was introduced into the stomach under endoscopic guidance, and while in the region of the gastric body, inflation with saline was performed at increments of 50 mL until target volume between 500 to 650 mL of saline was attained depending on the patient's gastric capacity (see Figure 1 for placement and removal of gastric balloon)[15]. No procedural complications were noted during endoscopic placement and removal of the balloon.
This study was exempt from institutional review board (IRB) review after institutional IRB review (UMCIRB 19-001002). The data collected consisted of patient demographics and other comorbidities. The patient demographic information collected included race, gender, age, and weight. Race was categorized in three groups-white, non-white, and not reported. The comorbidities considered in this study included hyperlipidemia, depression, coronary artery disease, cardiovascular disease, obstructive sleep apnea, and diabetes mellitus.
The unit of analysis was the patient, and the outcome of interest was hypertension. Both systolic and diastolic blood pressure were obtained to determine hypertension. All blood pressure measurements were assessed by a digital blood pressure machine (GE Dinamap Carescape V100 Vitals Monitor). This study examined the impact of weight reduction at baseline compared to 6-mo on hypertension. The cut-offs for systolic and diastolic blood pressures were 140 and 90 respectively. This allowed for the creation of binary outcome variables-hypertension and non-hypertension for both systolic and diastolic blood pressures.
A cohort study design was used for data analysis. A total of 172 patients had the Orbera intragastric balloon placed. Of the 172 patients who had IGBT at baseline, 11 patients (6.4%) requested early balloon removal due to foreign body sensation (n = 1), and/or intolerable gastrointestinal adverse events (n = 10). The reported gastrointestinal adverse events were nausea, vomiting, abdominal pain, and diarrhea. Eventually, 6-mo follow-up data were available for only 140 patients. As a result, only the 140 available at the 6-mo follow-up were included in the analysis. Univariate, bivariate, and multivariate statistical analyses were performed. Specifically, scatterplots were created to show the relationship between weight and blood pressure, and paired two-sample t-test was carried out to determine if there was a significant reduction in weight before and after the IGBT. Multiple regressions were also performed to examine the association between participants’ total body weight and blood pressure. The outcome variables for the multiple regression were systolic and diastolic blood pressure measured as continuous variables. This was followed by logistic regression analyses to determine the association between total body weight and hypertension at 6-mo post-implantation. The outcome variables for the logistic regression were systolic blood pressure (SBP)–non-hypertensive (140 mmHg or less) or hypertensive (greater than 140 mmHg), and diastolic blood pressure–non-hypertensive (90 mmHg or less) or hypertensive (greater than 90 mmHg). All authors had access to the study data and reviewed and approved the final manuscript. All statistical analyses were done using STATA 14®.
Of the 172 patients at baseline, follow-up data were available for only 140 patients at 6-mo. Table 1 shows the descriptive statistics for both patient demographic information and presence of comorbidities at baseline unless otherwise stated. The study included 15% males and 85% females. 50% of the patients were white and just over 22% were non-white, and about 27% declined to give their race. Additionally, a few patients were diagnosed with comorbidities including 12.86% patients with hyperlipidemia, 30% with depression, 2.86% with coronary artery disease, 5.71% with cardiovascular disease, 17.86% with obstructive sleep apnea, and 21.43% with Diabetes Mellitus.
| Variables | Description | Frequency | Percent (%) |
| Race distribution | White | 70 | 50.00 |
| Non-White | 32 | 22.86 | |
| Declined | 38 | 27.14 | |
| Gender distribution | Male | 21 | 15.00 |
| Female | 119 | 85.00 | |
| Age (in year) | mean (SD) | 45.56 (10.75) | |
| Weight in lbs. (At baseline) | mean (SD) | 231.61 (46.53) | |
| Weight in lbs. (At 6-mo) | mean (SD) | 203.88 (41.04) | |
| Systolic blood pressure (At baseline) | Non-hypertensive (140 or less) | 76 | 54.29 |
| Hypertensive (Greater than 140) | 64 | 45.71 | |
| Systolic blood pressure (At 6-mo) | Non-hypertensive (140 or less) | 110 | 78.57 |
| Hypertensive (Greater than 140) | 30 | 21.43 | |
| Diastolic blood pressure (At baseline) | Non-hypertensive (90 or less) | 123 | 87.86 |
| Hypertensive (Greater than 90) | 17 | 12.14 | |
| Diastolic blood pressure (At 6-mo) | Non-hypertensive (90 or less) | 125 | 89.29 |
| Hypertensive (Greater than 90) | 15 | 10.71 | |
| Has hyperlipidemia | No | 121 | 86.43 |
| Yes | 18 | 12.86 | |
| Missing | 1 | 0.71 | |
| Has depression | No | 97 | 69.29 |
| Yes | 42 | 30.00 | |
| Missing | 1 | 0.71 | |
| Has CAD | No | 136 | 97.14 |
| Yes | 4 | 2.86 | |
| Has CVD | No | 132 | 94.29 |
| Yes | 8 | 5.71 | |
| Has OSA | No | 115 | 82.14 |
| Yes | 25 | 17.86 | |
| Has diabetes mellitus | No | 110 | 78.57 |
| Yes | 30 | 21.43 | |
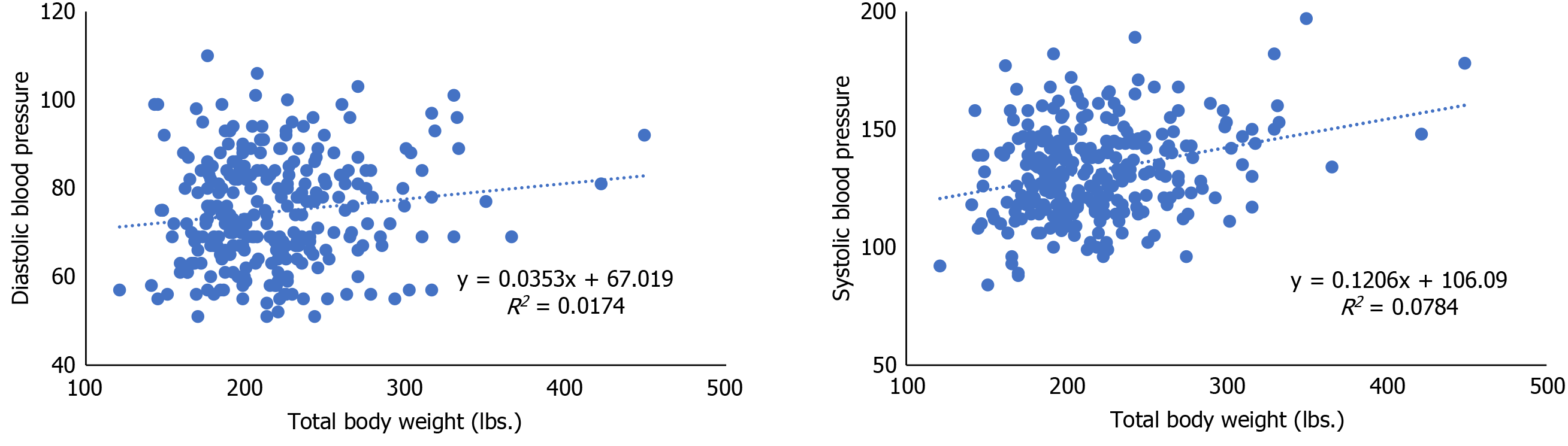
The average baseline patients’ weight prior to IGBT was 231.61 Lbs. (SD = 46.53 Lbs.). However, the average patients’ weight after IGBT at the 6-mo follow-up was 203.88 Lbs. (SD = 41.04 Lbs.). Hence, on average, the percent total body weight loss at 6-mo is 11.97 after IGBT. For comparison, a paired two-sample t-test was performed as shown in Table 2. The result reveals a statistically significant reduction in weight at the 6-mo follow-up after the IGBT. The scatterplot showing the relationship between total body weight and systolic and diastolic blood pressure is presented in Figure 2. The plots reveal a weak but positive correlation between total body weight and systolic blood pressure (r = 0.280), and total body weight and diastolic blood pressure (r = 0.132). Given the weak correlation, several cofounders were included in the multivariate analysis as presented below.
| Weight at baseline | Weight at 6-mo follow-up | |
| Mean | 231.61 | 203.88 |
| t-stat | 18.06 | |
| P value | 0.0000 |
This study further analyzed the relationship between weight loss and blood pressure using a multiple regression technique. The findings presented in Table 3 show that after controlling for other cofounders like comorbidities and patient demographic characteristics, weight is an important factor for predicting the systolic blood pressure of the study participants (β = 0.1350, P < 0.000). Conversely, it was revealed that weight was not significantly associated with the diastolic blood pressure of the study participants (β = 0.0295, P < 0.138).
The logistic regression performed revealed that weight (β = 0.0140, P < 0.000) and age (β = 0.0534, P < 0.000) are important factors in determining systolic blood pressure after IGBT. None of the other demographic characteristics or indicated comorbidities were found to be significant. The results specifically indicated that for every unit increase in weight, the log odds of SBP will increase by 1.4%. Also, for every unit increase in age, the log odds of SBP will increase by 5.34%. No variable included in the study however showed a significant association with diastolic blood pressure after IGBT. These results are presented in Table 4.
The intragastric balloon is used for those patients who have failed to achieve and maintain the weight loss with conservative measures or prefer a less invasive approach. In addition, it can have a significant role in the preoperative management of morbidly obese patients prior to bariatric surgery to reduce mortality and morbidity.
We observed an average loss of 11.97% from baseline weight at 6-mo post implantation, which is sufficient for comorbidity improvement. The present data indicate that Orbera® intragastric balloon significantly reduced weight, and systolic blood pressure at the time of balloon removal at 6-mo; although there was a decrease in diastolic blood pressure, it was not statistically significant. Furthermore, weight and age appear to be important factors in determining systolic blood pressure after intragastric balloon therapy. The weight reduction observed was analogous to other studies. Yorke et al[12] demonstrated a 15 kg and 5.9 ± 1.0 kg/m2 reduction post-implantation in a systematic review of 26 studies. Herve at al[16] demonstrated a 12 kg weight reduction at the time of balloon removal and 8.6 kg reduction at 1 year follow up. A Brazilian multicenter study also cited a significant weight reduction of 15.2 ± 10.5 kg, however, Ganesh et al[17] reported a 5.9 kg reduction after 6 mo[18]. While the intragastric balloon can induce short-term weight reduction, the weight loss sustainability is often difficult to achieve. Despite weight regain observed, Crea et al[19] reported improvement in metabolic syndrome and the sustained 10% body weight loss.
Obesity plays a key role in metabolic syndrome[20]. The development of hypertension in obesity involves multiple mechanisms such as insulin resistance, increased inflammatory markers, oxidative stress, the sympathetic nervous system, and the renin-angiotensin aldosterone system. The mentioned effects in the setting of obesity induce endothelial dysfunction thus contributing to elevated blood pressure[20]. While patients who undergo lifestyle interventions often have blood pressure improvement, its sustainability on weight loss is limited; therefore, it may fail to decrease long-term adverse cardiovascular effect[20]. While there are conflicting data regarding the influence of pharmacological agents for weight reduction on blood pressure improvement, there is evidence that bariatric surgery improves blood pressure by mechanisms such as decreasing plasma leptin and sympathetic nervous system activity[20]. Given the relatively new field of endoscopic bariatric therapies, there is limited data regarding the influence of intragastric balloon therapy on blood pressure. It is known that the intragastric balloon adopts the gastric restriction mechanism through the space-occupying design, while increasing post-prandial satiety and decreasing pre-prandial hunger. It has also been reported to alter hormone release, such as leptin and ghrelin, leading to weight loss; however, it appears to be a transitory affect[21,22].
Orbera has a relatively good safety profile with the commonest adverse events being abdominal pain, nausea, vomiting, and gastroesophageal reflux disease[8,12,23]. While there is a cited early balloon removal rate of 9%, in our study, there was a 6.4% early balloon removal rate due to intolerable gastrointestinal adverse events[9].
The study has several limitations. They include the retrospective analysis of a single-center analysis and the absence of a control group. The frequency of the other comorbidities may be an underestimate. In addition, the follow-up period was only at the six-month time period of balloon removal, and therefore, weight loss sustainability cannot be concluded.
IGBT can be an effective short-term weight reduction modality with a relatively little risk of adverse event. Due to its improvement on systolic blood pressure, IGBT may help reduce cardiovascular risk.
In the United States, about a third of adults have hypertension, which is the most modifiable risk factor for heart disease and stroke. The prevalence of obesity and hypertension in eastern North Carolina are comparable, with obesity being an established risk factor for hypertension. Lifestyle interventions and pharmacological agents often are not sufficient to achieve enough weight loss. Bariatric surgery offers the most effective weight reduction intervention, however patients with higher body mass index may have higher surgical morbidity and mortality, longer hospitalization, and high rates of 30-d readmission due to co-morbidities. Minimally invasive non-surgical options like the intragastric balloon may bridge a critical gap in the treatment of obesity.
The weight loss mechanism of the intragastric balloon therapy is restrictive, and this leads to weight reduction due to reduced food intake from early post-prandial satiety. Weight loss helps to lower the risk of potentially serious obesity-related health problems like heart disease, stroke, hypertension, diabetes and osteoarthritis. Aside from long-term health benefits, weight reduction is cost-effective and promotes substantial health-care cost savings.
Our study focused on the impact of intragastric balloon therapy (IGBT) on blood pressure reduction. IGBT leads to statistically significant weight and systolic blood pressure reduction at 6-mo. Also, the degree of weight reduction by IGBT is sufficient to effect improvement in comorbidities.
A retrospective chart review was conducted from January 1, 2016 to January 31, 2019 of consecutive adults who received IGBT in a gastroenterology private practice in eastern North Carolina. The balloon was introduced into the stomach under endoscopic guidance, and while in the region of the gastric body, inflation with saline was performed at increments of 50 mL until target volume between 500 to 650 mL of saline was attained depending on the patient's gastric capacity. No procedural complications were noted during endoscopic placement and removal of the balloon.
Of the 172 patients who had IGBT at baseline, 11 patients (6.4%) requested early balloon removal due to foreign body sensation (n = 1), and/or intolerable gastrointestinal adverse events (n = 10). The reported gastrointestinal adverse events were nausea, vomiting, abdominal pain, and diarrhea. Eventually, 6-mo follow-up data were available for only 140 patients. As a result, only the 140 available at the 6-mo follow-up were included in the analysis. Univariate, bivariate, and multivariate statistical analyses were performed. Specifically, scatterplots were created to show the relationship between weight and blood pressure, and paired two-sample t-test was carried out to determine if there was a significant reduction in weight before and after the IGBT. Multiple regressions were also performed to examine the association between participants’ total body weight and blood pressure. The outcome variables for the multiple regression were systolic and diastolic blood pressure measured as continuous variables. This was followed by logistic regression analyses to determine the association between total body weight and hypertension at 6-mo post-implantation. The outcome variables for the logistic regression were systolic blood pressure–non-hypertensive (140 mmHg or less) or hypertensive (greater than 140 mmHg), and diastolic blood pressure-non-hypertensive (90 mmHg or less) or hypertensive (greater than 90 mmHg). All authors had access to the study data and reviewed and approved the final manuscript. All statistical analyses were done using STATA 14®.
Weight is an important factor for predicting the systolic blood pressure of the study participants (β = 0.1350, P < 0.000). Conversely, weight was not significantly associated with the diastolic blood pressure of the study participants (β = 0.0295, P < 0.138). On average, the percent total body weight loss at 6-mo is 11.97 after IGBT. The logistic regression performed revealed that weight (β = 0.0140, P < 0.000) and age (β = 0.0534, P < 0.000) are important factors in determining systolic blood pressure after IGBT. The results specifically indicated that for every unit increase in weight, the log odds of SBP will increase by 1.4%. Also, for every unit increase in age, the log odds of SBP will increase by 5.34%.
IGBT can be an effective short-term weight reduction modality with a relatively little risk of adverse event. Due to its improvement on systolic blood pressure, IGBT may help reduce cardiovascular risk. Study limitations include the retrospective analysis of a single-center and the absence of a control group. In addition, the follow-up period was only at the six-month time period of balloon removal, and therefore, weight loss sustainability cannot be concluded.
IGBT engenders short-term weight reduction modality with a relatively little risk of adverse event. Its improvement on systolic blood pressure may help reduce cardiovascular risk.
Given the increasing global prevalence of obesity, it is envisioned that bariatric devices such as intragastric balloons will continue to evolve. Though intragastric balloons can bring about short-term morbidity/mortality benefits, the long-term benefits are questionable. Further studies will focus on promoting the long-term weight benefits of intragastric balloons.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Quadros LG, Hu B S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Fruh SM. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017;29:S3-S14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 392] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 2. | Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146-e603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6484] [Cited by in RCA: 6394] [Article Influence: 799.3] [Reference Citation Analysis (0)] |
| 3. | Saunders KH, Igel LI, Saumoy M, Sharaiha RZ, Aronne LJ. Devices and Endoscopic Bariatric Therapies for Obesity. Curr Obes Rep. 2018;7:162-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 666] [Article Influence: 74.0] [Reference Citation Analysis (0)] |
| 5. | Benaiges D, Más-Lorenzo A, Goday A, Ramon JM, Chillarón JJ, Pedro-Botet J, Flores-Le Roux JA. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21:11804-11814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 140] [Cited by in RCA: 150] [Article Influence: 15.0] [Reference Citation Analysis (4)] |
| 6. | Genco A, Cipriano M, Materia A, Bacci V, Maselli R, Musmeci L, Lorenzo M, Basso N. Laparoscopic sleeve gastrectomy vs intragastric balloon: a case-control study. Surg Endosc. 2009;23:1849-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Contival N, Menahem B, Gautier T, Le Roux Y, Alves A. Guiding the non-bariatric surgeon through complications of bariatric surgery. J Visc Surg. 2018;155:27-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Milone L, Strong V, Gagner M. Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI > or =50). Obes Surg. 2005;15:612-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 156] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Choi HS, Chun HJ. Recent Trends in Endoscopic Bariatric Therapies. Clin Endosc. 2017;50:11-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic Bariatric and Metabolic Therapies: New and Emerging Technologies. Gastroenterology. 2017;152:1791-1801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 105] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 11. | Goyal D, Watson RR. Endoscopic Bariatric Therapies. Curr Gastroenterol Rep. 2016;18:26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Yorke E, Switzer NJ, Reso A, Shi X, de Gara C, Birch D, Gill R, Karmali S. Intragastric Balloon for Management of Severe Obesity: a Systematic Review. Obes Surg. 2016;26:2248-2254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Ribeiro da Silva J, Proença L, Rodrigues A, Pinho R, Ponte A, Rodrigues J, Sousa M, Almeida R, Carvalho J. Intragastric Balloon for Obesity Treatment: Safety, Tolerance, and Efficacy. GE Port J Gastroenterol. 2018;25:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Genco A, Bruni T, Doldi SB, Forestieri P, Marino M, Busetto L, Giardiello C, Angrisani L, Pecchioli L, Stornelli P, Puglisi F, Alkilani M, Nigri A, Di Lorenzo N, Furbetta F, Cascardo A, Cipriano M, Lorenzo M, Basso N. BioEnterics Intragastric Balloon: The Italian Experience with 2,515 Patients. Obes Surg. 2005;15:1161-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 224] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 15. | Image Library. In: Illustrations [cited 22 March 2021]. Available from: http://apolloresource.wpengine.com/orbera/image-library/. |
| 16. | Herve J, Wahlen CH, Schaeken A, Dallemagne B, Dewandre JM, Markiewicz S, Monami B, Weerts J, Jehaes C. What becomes of patients one year after the intragastric balloon has been removed? Obes Surg. 2005;15:864-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Ganesh R, Rao AD, Baladas HG, Leese T. The Bioenteric Intragastric Balloon (BIB) as a treatment for obesity: poor results in Asian patients. Singapore Med J. 2007;48:227-231. [PubMed] |
| 18. | Sallet JA, Marchesini JB, Paiva DS, Komoto K, Pizani CE, Ribeiro ML, Miguel P, Ferraz AM, Sallet PC. Brazilian multicenter study of the intragastric balloon. Obes Surg. 2004;14:991-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Crea N, Pata G, Della Casa D, Minelli L, Maifredi G, Di Betta E, Mittempergher F. Improvement of metabolic syndrome following intragastric balloon: 1 year follow-up analysis. Obes Surg. 2009;19:1084-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Cohen JB. Hypertension in Obesity and the Impact of Weight Loss. Curr Cardiol Rep. 2017;19:98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 21. | Konopko-Zubrzycka M, Baniukiewicz A, Wróblewski E, Kowalska I, Zarzycki W, Górska M, Dabrowski A. The effect of intragastric balloon on plasma ghrelin, leptin, and adiponectin levels in patients with morbid obesity. J Clin Endocrinol Metab. 2009;94:1644-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Bazerbachi F, Vargas EJ, Abu Dayyeh BK. Endoscopic Bariatric Therapy: A Guide to the Intragastric Balloon. Am J Gastroenterol. 2019;114:1421-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 23. | Imaz I, Martínez-Cervell C, García-Alvarez EE, Sendra-Gutiérrez JM, González-Enríquez J. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 271] [Article Influence: 15.9] [Reference Citation Analysis (0)] |