Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. May 16, 2015; 7(5): 446-459
Published online May 16, 2015. doi: 10.4253/wjge.v7.i5.446
Published online May 16, 2015. doi: 10.4253/wjge.v7.i5.446
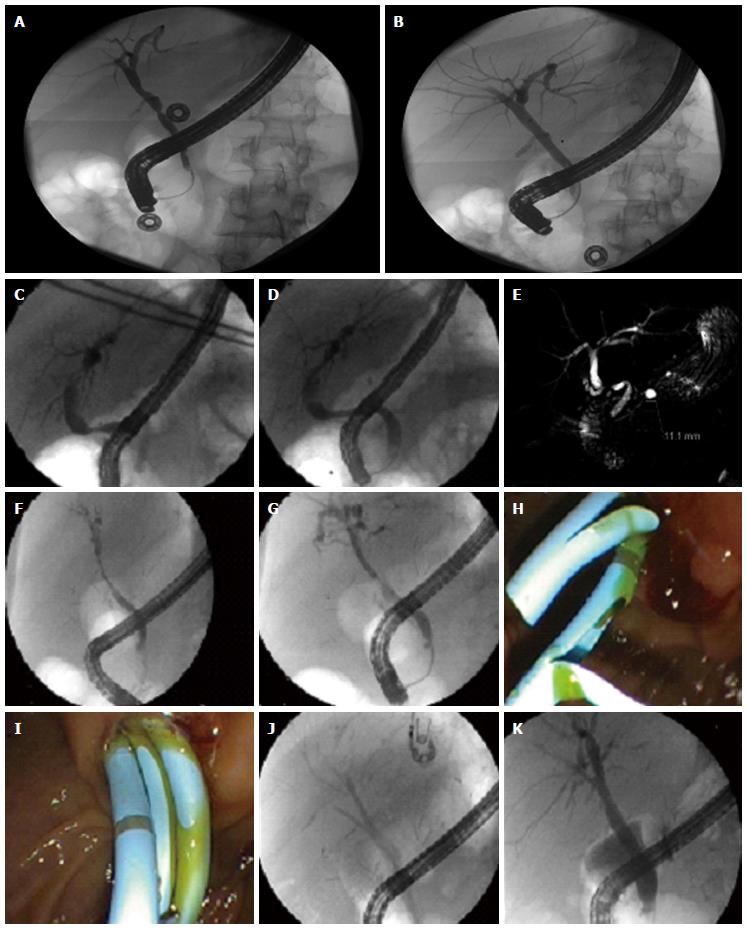
Figure 1 Different management strategies for biliary strictures.
A: Post-LT anastomotic biliary stricture (as seen on ERC); B: managed with balloon dilatation only; C: Post-LT anastomotic biliary stricture (as seen on ERC); D: Managed with balloon dilatation; E: MRCP image of the same stricture; F: Long segment biliary stricture due to global hypotension post-LT; G: Dilatation performed with biliary balloon; H: Followed by placement of two plastic stents; I: Due to inadequate effect with two stents, sequential therapy strategy adopted with placement of three stents; J: Fluoroscopic image of three stents in right posterior and anterior hepatic and left hepatic ducts; K: Final cholangiogram suggesting a much improved bile duct diameter. ERC: Endoscopic retrograde cholangiography; LT: Liver transplantation.
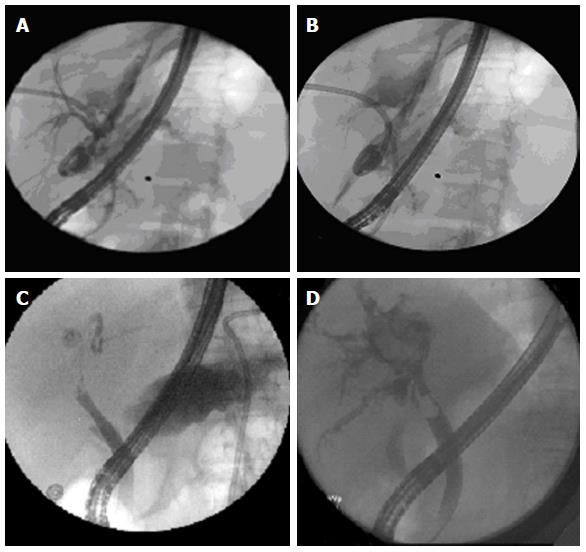
Figure 2 Diffuse non-anastomotic intra-hepatic biliary structuring seen in a donation after cardiac death liver transplant patient, not amenable to endoscopic therapy.
Figure 3 Management strategies for bile leak and biloma.
A: Bile leak from split surface of the liver in a patient with split-liver transplant; B: Managed successfully with endoscopic plastic stent placement; C: In a separate patient, bile leak successfully managed by placement of a fully covered metal stent; D: In yet another patient, intrahepatic biloma, which becomes apparent on occlusion cholangiogram.
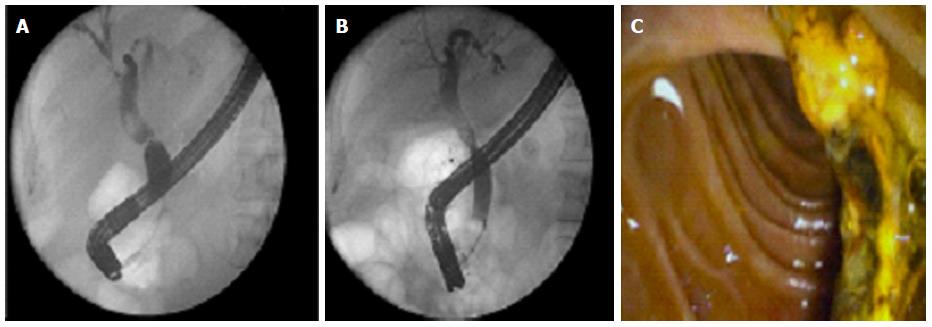
Figure 4 Management of common bile duct filling defects.
A: Common bile duct (CBD) filling defect seen proximal to mid-CBD stricture in a post-liver transplantation patient; B: Successful removal of stone after dilatation the stricture; C: Endoscopic image of successfully extracted stone and sludge in this case.
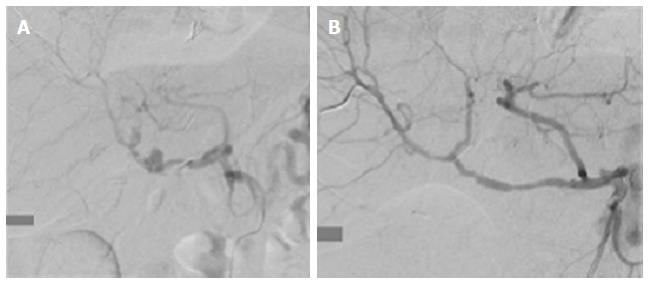
Figure 5 Rare cause of Hemobilia.
A: Hepatic artery pseudoaneurysm fistulizing to the common bile duct, resulting in hemobilia; B: Managed with intravascular stent placement by interventional radiology.
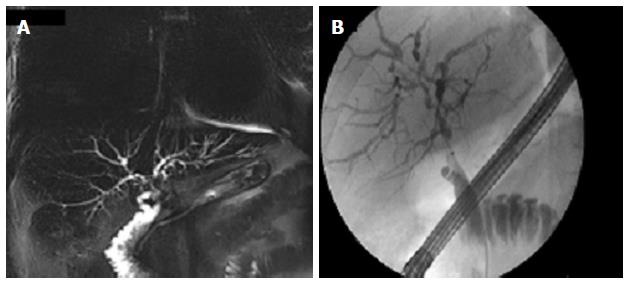
Figure 6 Don’t forget the native disease.
Recurrence of native disease can mimic biliary complications, hence appropriately investigated with magnetic resonance cholangiopancreatography (A) and/or endoscopic retrograde cholangiography (B). This patient was transplanted for primary sclerosing cholangitis, and had disease recurrence involving the intra-hepatics few years later.
- Citation: Girotra M, Soota K, Klair JS, Dang SM, Aduli F. Endoscopic management of post-liver transplant biliary complications. World J Gastrointest Endosc 2015; 7(5): 446-459
- URL: https://www.wjgnet.com/1948-5190/full/v7/i5/446.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i5.446