Published online Jul 27, 2010. doi: 10.4254/wjh.v2.i7.292
Revised: June 16, 2010
Accepted: June 23, 2010
Published online: July 27, 2010
Hemangiomas are the most frequent benign tumors of the liver. Most hemangiomas are asymptomatic and therefore largely diagnosed only in routine screening tests. Usually they are small and require no specific treatment. In some situations they can reach great dimensions, causing some discomfort to the patient. Resection of liver hemangioma is indicated in cases of great dimension tumors causing symptoms such as pain, nausea or bloating caused by compression of adjacent organs. We report a case of a rare giant hemangioma with rapid growth in short time: a 50 year old female reported to our institution with a 40 cm giant liver hemangioma and then underwent a left hepatectomy.
- Citation: Koszka AJ, Ferreira FG, Aquino CG, Ribeiro MA, Gallo AS, Aranzana EM, Szutan LA. Resection of a rapid-growing 40-cm giant liver hemangioma. World J Hepatol 2010; 2(7): 292-294
- URL: https://www.wjgnet.com/1948-5182/full/v2/i7/292.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i7.292
Hemangiomas are the most frequent benign tumors of the liver with an incidence ranging from 5% to 20% and women accounting for the largest part. Most hemangiomas are asymptomatic and therefore largely diagnosed only in routine screening tests. Usually they are small and require no specific treatment[1-5].
In some situations they can reach great dimensions, causing some discomfort to the patient. There is no consensus in the literature regarding the minimum size a hemangioma is considered as giant but in our service we use the limit of 10 cm. Rare cases of rupture followed by massive bleeding and Kassabach-Merrit’s syndrome with serious complications have been reported.
Resection of liver hemangioma is indicated in cases of great dimension tumors causing symptoms such as pain, nausea or bloating by compression of adjacent organs[6-9]. Resection is also advisable in a controversial diagnosis where malignancy cannot be fully eliminated[4-7].
We report a case of a rare giant hemangioma with rapid growth in a short time: a 50-year old female being monitored for 7 years since a liver hemangioma was incidentally diagnosed.
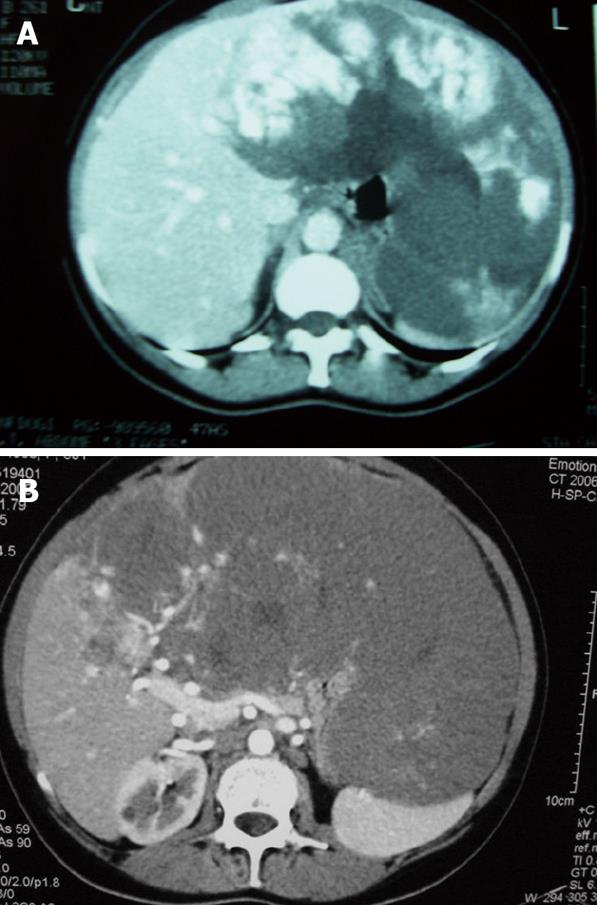
At that time, the lesion already measured 20 cm in its largest axis (Figure 1A). In the last 4 mo, she presented with symptoms such as a dry cough and in the last 2 mo, abdominal pain. CT scan evidenced an increase of 10 cm in the lesion in the left lobe with compression of the diaphragm, reaching 30 cm in its largest axis (Figure 1B).
An arterial embolization procedure was attempted in order to restrict the hemangioma growing. It brought no benefits but worsened the symptoms.
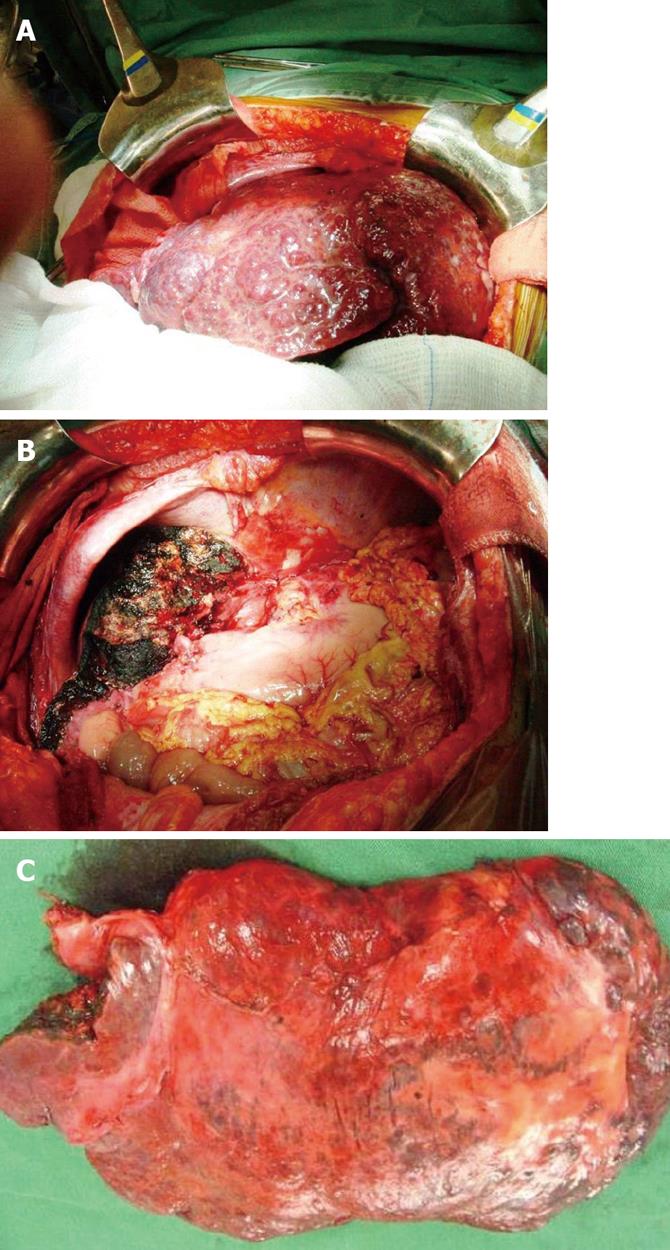
The patient then underwent a left hepatectomy. We usually access the abdominal cavity through a Chevron incision to perform hepatectomies. After liver mobilization was done, a great deformity in the vascular anatomy of the portal and supra hepatic veins was identified, mainly due to the compression caused by the huge hemangioma (Figure 2A). The left hepatic vein was involved by the tumor and had to be ligated. For a safe parenchymal transection, blood inflow and outflow control to the liver was performed. Pringle maneuver and the infra and supra hepatic vena cava were laced but not clamped. The liver transection was performed with kellyclasy and silkclasy[10] and hemostasis was achieved with cauterization. Figure 2B shows the final aspect of the resection. The anatomopathological findings confirmed the diagnosis of a 40 cm hemangioma in its largest axis (Figure 2C). The patient is now asymptomatic at 6 mo post-operation.
After a review of our patient database, we found that the number of diagnosed liver hemangiomas greater than 10 cm is very low. The few patients with giant hemangiomas do not present with any signs of tumor growing at follow up. Therefore, resection of liver hemangiomas is quite restricted in our service; the main argument against the resection is the need of submitting a patient with a benign disease to such a major surgery. Interestingly, this was the only report of a size changing hemangioma in our experience.
The literature shows that arterial embolization of the lesion to contain the tumor growth is not effective unless the hemangioma is a lesion with a clear arterial blood supply[11]. At first we assumed that this hemangioma could have an arterial supply that would justify such a rapid size enhancement. The arterial embolization was the initial therapeutic approach but unfortunately the procedure did not help and, due to necrosis, worsened the pain for the patient.
Discussions on resection of hemangiomas include procedures on the so-called giant tumors or in those that result in symptoms to the patient. Reports on surgery due to hemangioma growth are rare[6].
In this report, our attention is drawn to the speed of the hemangioma increase, leading to abdominal pain and cough due to diaphragm compression. In our service, we maintain clinical follow-up of hemangiomas in asymptomatic patients regardless the size. Nevertheless, due to the particular evolution of this case (rapid growth and the tumor necrosis as a consequence of the arterial embolization), we decided to carry out the resection despite the consequent complications involved in this kind of procedure.
Peer reviewers: Lars Mueller, MD, PhD, Pediatric Hematology/Oncology, Children's Hospital Boston, MA 02115, United States; Boon Hun Yong, Associate Professor, Department of Anaesthesiology, University of Hong Kong, Hong Kong, China
| 1. | Fu XH, Lai EC, Yao XP, Chu KJ, Cheng SQ, Shen F, Wu MC, Lau WY. Enucleation of liver hemangiomas: is there a difference in surgical outcomes for centrally or peripherally located lesions? Am J Surg. 2009;198:184-187. |
| 2. | Singh RK, Kapoor S, Sahni P, Chattopadhyay TK. Giant haemangioma of the liver: is enucleation better than resection? Ann R Coll Surg Engl. 2007;89:490-493. |
| 3. | Romano F, Messinesi G, Tana F, Uggeri F. Recurrent giant hemangioma causing severe respiratory distress. Dig Dis Sci. 2007;52:3526-3529. |
| 4. | Erdogan D, Busch OR, van Delden OM, Bennink RJ, ten Kate FJ, Gouma DJ, van Gulik TM. Management of liver hemangiomas according to size and symptoms. J Gastroenterol Hepatol. 2007;22:1953-1958. |
| 5. | Hazinedaroglu SM, Kayaoglu HA, Ali Yerdel M. Enucleation of centrally located giant hepatic hemangioma: report of two cases. Dig Dis Sci. 2006;51:1213-1217. |
| 6. | Herman P, Costa ML, Machado MA, Pugliese V, D’Albuquerque LA, Machado MC, Gama-Rodrigues JJ, Saad WA. Management of hepatic hemangiomas: a 14-year experience. J Gastrointest Surg. 2005;9:853-859. |
| 7. | Hamaloglu E, Altun H, Ozdemir A, Ozenc A. Giant liver hemangioma: therapy by enucleation or liver resection. World J Surg. 2005;29:890-893. |
| 8. | Demircan O, Demiryurek H, Yagmur O. Surgical approach to symptomatic giant cavernous hemangioma of the liver. Hepatogastroenterology. 2005;52:183-186. |
| 9. | Lerner SM, Hiatt JR, Salamandra J, Chen PW, Farmer DG, Ghobrial RM, Busuttil RW. Giant cavernous liver hemangiomas: effect of operative approach on outcome. Arch Surg. 2004;139:818-821; discussion 821-823. |
| 10. | Herman P, Machado MA, Machado MC. Silkclasy: a simple way for liver transection during anatomic hepatectomies. J Surg Oncol. 2007;95:86-89. |
| 11. | Vassiou K, Rountas H, Liakou P, Arvanitis D, Fezoulidis I, Tepetes K. Embolization of a giant hepatic hemangioma prior to urgent liver resection. Case report and review of the literature. Cardiovasc Intervent Radiol. 2007;30:800-802. |