Copyright
©The Author(s) 2017.
World J Hepatol. Jan 28, 2017; 9(3): 131-138
Published online Jan 28, 2017. doi: 10.4254/wjh.v9.i3.131
Published online Jan 28, 2017. doi: 10.4254/wjh.v9.i3.131
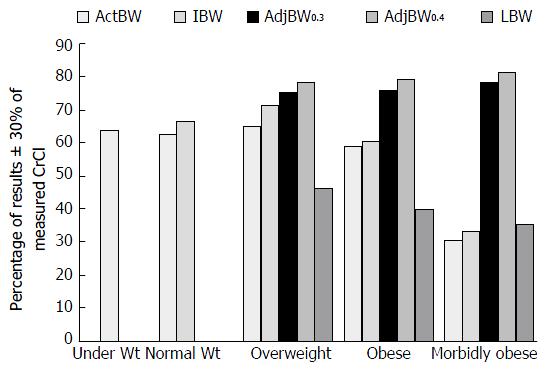
Figure 1 Impact of various body weights used in estimating creatinine clearance from Winter et al[1].
In patients with a BMI ≥ 25 kg/m2, using AdjBW0.4 was the most accurate weight to estimate CrCl when compared to a 24-h urine CrCl. Under Wt: BMI < 18.5 kg/m2; Normal Wt: BMI 18.5-24.9 kg/m2; Overweight: BMI 25-29.9 kg/m2; Obese: BMI 30-39.9 kg/m2; Morbidly obese: BMI ≥ 40 kg/m2; CrCl: Creatinine clearance; ActBW: Actual body weight; IBW: Ideal body weight; AdjBW: Adjusted body weight; LBW: Lean body weight; BMI: Body mass index.
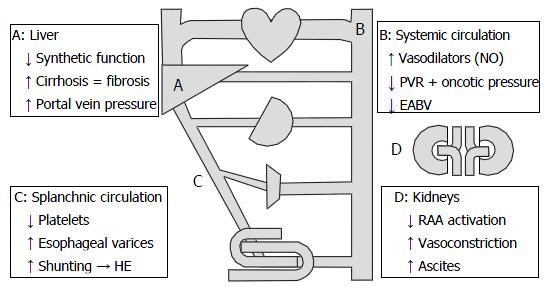
Figure 2 Systemic effects of cirrhosis.
Increased portal vein pressure results in vasodilation decreasing peripheral vascular resistance (PVR) and effective arterial blood volume (EABV). To compensate for this, increased renin-angiotensin-aldosterone (RAA) activation leads to sodium and fluid retention along with renal vasoconstriction and reduced glomerular filtration rate. Adopted with permission from Ho et al[27]. HE: Hepatic encephalopathy.
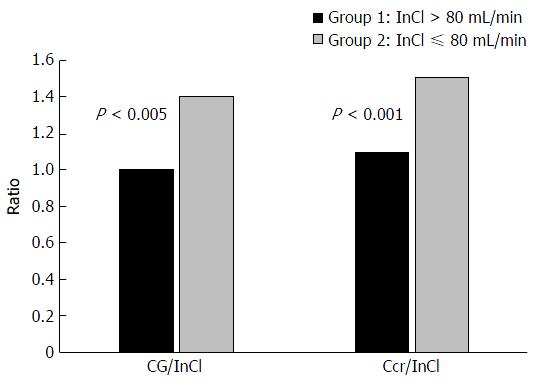
Figure 3 In cirrhotics, as renal function declines, conventional methods of estimating renal function are no longer accurate.
Both the Cockcroft-Gault (CG) equation and a 24-h urine creatinine clearance (Ccr) significantly overestimated true renal function as measured by inulin clearance (InCl) in cirrhotics with a baseline InCl ≤ 80 mL/min. The CG equation and Ccr were better estimates in those with a baseline InCl > 80 mL/min[33].
- Citation: Scappaticci GB, Regal RE. Cockcroft-Gault revisited: New de-liver-ance on recommendations for use in cirrhosis. World J Hepatol 2017; 9(3): 131-138
- URL: https://www.wjgnet.com/1948-5182/full/v9/i3/131.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i3.131