Published online Dec 15, 2003. doi: 10.3748/wjg.v9.i12.2878
Revised: September 14, 2003
Accepted: October 7, 2003
Published online: December 15, 2003
We report a rare case of a postoperative pseudoaneurysm of the gastroduodenal artery following radical gastrectomy. Surgical trauma to the gastroduodenal artery during regional lymphadenectomy was considered the cause of the postoperative pseudoaneurysm. The pseudoaneurysm was successfully managed by ligating the bleeding vessel. We should consider the possibility of pseudoaneurysm formation in a patient with gastrointestinal bleeding in the postoperative period following radical gastrectomy with regional lymph node and perivascular lymphatic dissection.
- Citation: Kim DY, Joo JK, Ryu SY, Kim YJ, Kim SK, Jung YY. Pseudoaneurysm of gastroduodenal artery following radical gastrectomy for gastric carcinoma patients. World J Gastroenterol 2003; 9(12): 2878-2879
- URL: https://www.wjgnet.com/1007-9327/full/v9/i12/2878.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i12.2878
The causes of pseudoaneurysms include infection, trauma, and surgical procedures[1]. The development of pseudoaneurysms after upper abdominal surgery is rare, and most occur after biliary and pancreatic surgery[2-5]. There have been only a few reported cases of postoperative pseudoaneurysm of an artery following abdominal surgery. We recently encountered a patient with a ruptured pseudoaneurysm of the gastroduodenal artery following radical gastrectomy for gastric carcinoma.
A 73-year-old male was admitted with a two-month history of epigastric discomfort and weight loss. An upper gastrointestinal series, endoscopy, and abdominal CT scan suggested gastric carcinoma. The preoperative laboratory work-up was normal.
Laparotomy revealed an advanced gastric carcinoma involving the adjacent lymph nodes. No peritoneal dissemination or hepatic metastasis was found. The patient underwent a successful radical gastrectomy and the regional lymph nodes, and perivascular lymphatics surrounding the gastroduodenal artery were dissected.
Macroscopically, a curative resection was performed. Postoperative microscopic examination revealed poorly differentiated adenocarcinoma involving the serosal layer of the stomach, and metastasis in one of the twenty-eight lymph nodes dissected.
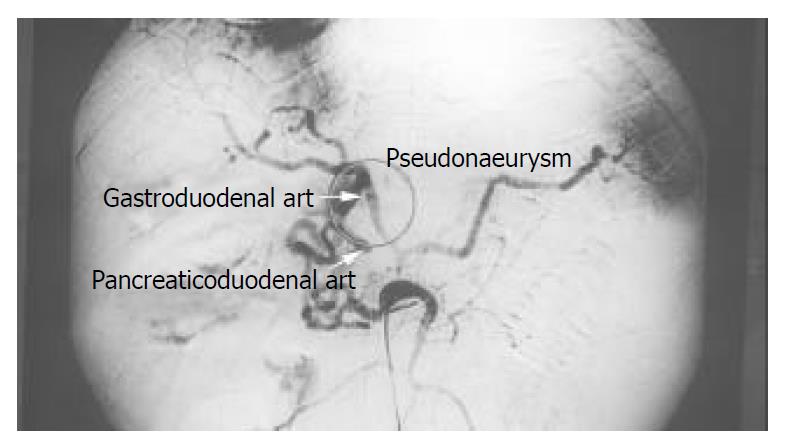
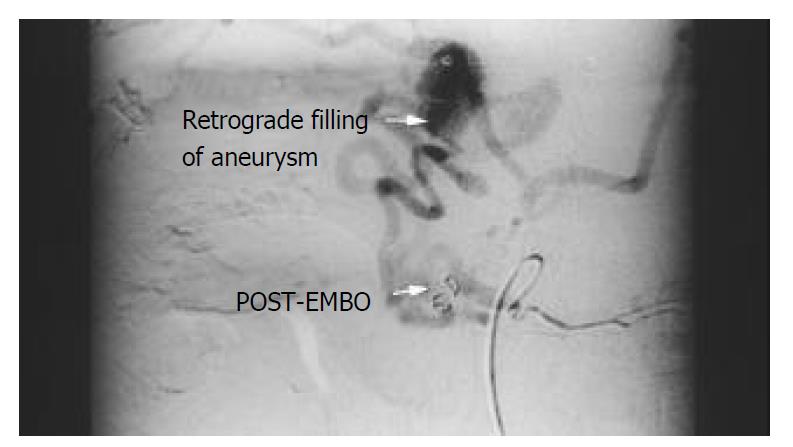
On postoperative day eight, a wound infection with moderate fever developed, and examination of the anastomotic site revealed no leakage. Twenty-five days after the operation, he suddenly developed abdominal distention with hypovolemic shock. A tentative diagnosis of hemoperitoneum was made and an emergency angiography was performed. An emergency celiac trunk arteriogram revealed a pseudoaneurysmal sac originating from the gastroduodenal artery (Figure 1). To obliterate the pseudoaneurysm transcatheter embolization with steel coils was attempted (Figure 2), but failed. We performed an emergent laparotomy. There was a large hematoma arou nd the gastrod ued enal artery . The gastroduodenal artery was allegedly ligated. The patient recovered and was discharged from the hospital two weeks later. He had no subsequent bleeding episodes and was doing well two months following discharge.
Pseudoaneurysms result from a variety of mechanisms, including infection, trauma, and surgical procedures[1]. All have in common disruption of arterial continuity with extravasation of blood into the surrounding tissues. This ultimately results in the formation of a fibrous tissue capsule that progressively enlarges due to the unrelenting arterial pressure[1]. Gastroduodenal artery aneurysms account for 1.5% of all splanchnic artery aneurysms, but the true incidence of postoperative pseudoaneurysm of the gastroduodenal artery is unknown[6]. Postoperative pseudoaneurysm formation is uncommon, but can follow surgical trauma during gastrointestinal surgery or perioperative local infection[2,7,8]. There is usually a history of massive bleeding and perioperative local infection when the pseudoaneurysm develops[2]. Our patient had a local wound infection and massive intra-abdominal bleeding.
Our review of the literature revealed no reported cases of postoperative pseudoaneurysm of the gastroduodenal artery following radical gastrectomy. We assumed that the pseudoaneurysm formation had been caused by a weakness in the arterial wall according to skeletonization resulting from lymphadenectomy.
When an intra-abdominal pseudoaneurysm is suspected, angiography is useful for determining the exact location of the pseudoaneurysm. In addition, it can save time and prevent the danger of an emergency laparotomy to locate the source of bleeding without angiography[9]. In our case, emergent angiography was performed after the episode of massive intra-abdominal bleeding and demonstrated a pseudoaneurysm arising from the gastroduodenal artery. Many authors[4,6,9-11] have recommended transcatheter occlusion or selective embolization as a useful method in high-risk patients. Basile et al[12], Bulut et al[13] and Furukawa et al[14], reported successful transcatheter arterial embolization in a patient who developed pseudoaneurysm after abdominal surgery. We tried transcatheter arterial embolization, but failed to control the bleeding.
Although it is impossible to know the true incidence of postoperative pseudoaneyrysm of the gastroduodenal artery, it may develop due to iatrogenic injury during surgery[4,15].
We should consider the possibility of pseudoaneurysm formation in a patient with inta-abdominal bleeding during the postoperative period following radical gastrectomy with regional lymph nodes and perivascular lymphatic dissection.
This report describes the successful management of a pseudoaneurysm of the gastroduodenal artery following radical gastrectomy, by ligation of the bleeding vessel.
Edited by Zhu LH
| 2. | Iseki J, Tada Y, Wada T, Nobori M. Hepatic artery aneurysm. Report of a case and review of the literature. Gastroenterol Jpn. 1983;18:84-92. [PubMed] |
| 3. | Tan M, Di Carlo A, Stein LA, Cantarovich M, Tchervenkov JI, Metrakos P. Pseudoaneurysm of the superior mesenteric artery after pancreas transplantation treated by endovascular stenting. Transplantation. 2001;72:336-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Sugimoto H, Kaneko T, Ishiguchi T, Takai K, Ohta T, Yagi Y, Inoue S, Takeda S, Nakao A. Delayed rupture of a pseudoaneurysm following pancreatoduodenectomy: report of a case. Surg Today. 2001;31:932-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Almogy G, Bloom A, Verstandig A, Eid A. Hepatic artery pseudoaneurysm after liver transplantation. A result of transhepatic biliary drainage for primary sclerosing cholangitis. Transpl Int. 2002;15:53-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Eckhauser FE, Stanley JC, Zelenock GB, Borlaza GS, Freier DT, Lindenauer SM. Gastroduodenal and pancreaticoduodenal artery aneurysms: a complication of pancreatitis causing spontaneous gastrointestinal hemorrhage. Surgery. 1980;88:335-344. [PubMed] |
| 7. | Kelley CJ, Hemingway AP, Mcpherson GA, Allison DJ, Blumgart LH. Non-surgical management of post-cholecystectomy haemobilia. Br J Surg. 1983;70:502-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Aranha GV, O'Neil S, Borge MA. Successful nonoperative management of bleeding hepatic artery pseudoaneurysm following pancreaticoduodenectomy. Dig Surg. 1999;16:528-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Stabile BE, Wilson SE, Debas HT. Reduced mortality from bleeding pseudocysts and pseudoaneurysms caused by pancreatitis. Arch Surg. 1983;118:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 165] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Kuno RC, Althaus SJ, Glickerman DJ. Direct percutaneous coil and ethanol embolization of a celiac artery pseudoaneurysm. J Vasc Interv Radiol. 1995;6:357-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Kitagawa T, Iriyama K, Azuma T, Yamakado K. Nonoperative treatment for a ruptured pseudoaneurysm of the celiac trunk: report of a case. Surg Today. 1997;27:1069-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Basile A, Boullosa-Seoane E, Dominguez-Viguera L, Certo A, Casal-Rivas M. Percutaneous embolization of a gastroduodenal artery aneurysm secondary to antrectomy and Roux en Y reconstruction. Radiol Med. 2002;104:374-377. [PubMed] |
| 13. | Bulut T, Yamaner S, Bugra D, Akyuz A, Acarli K, Poyanli A. False aneurysm of the hepatic artery after laparoscopic cholecystectomy. Acta Chir Belg. 2002;102:459-463. [PubMed] |
| 14. | Furukawa H, Kosuge T, Shimada K, Yamamoto J, Ushio K. Helical CT of the abdomen after pancreaticoduodenectomy: usefulness for detecting postoperative complications. Hepatogastroenterology. 1997;44:849-855. [PubMed] |
| 15. | Satoh H, Morisaki T, Kishikawa H. A case of a postoperative aneurysm of the common hepatic artery which ruptured into the remnant stomach after a radical gastrectomy. Jpn J Surg. 1989;19:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |