Published online Dec 15, 2003. doi: 10.3748/wjg.v9.i12.2866
Revised: April 16, 2003
Accepted: May 21, 2003
Published online: December 15, 2003
AIM: Angiogenesis is an important step in the growth of solid malignant tumors. A number of angiogenic factors have been found such as transforming growth factorβ1 (TGF-β1) and vascular endothelial growth factor (VEGF). However, the roles of TGFβ1 and VEGF in gastrointestinal carcinogenesis are still unclear. This study was to investigate the expressions of TGF-β1 and VEGF in gastrointestinal tract malignant tumors, as well as their association with microvessel density (MVD). At the same time, we also observed the localization of TGF-β1 and its receptor CD105 in gastric malignant tumors.
METHODS: The expressions of TGF-β1 and CD105 were detected in 55 fresh specimens of gastric carcinoma and VEGF and CD105 in 44 fresh specimens of colorectal carcinoma by immunohistochemical staining (S-ABC). TGF-β1 and CD105 in 55 gastric carcinoma tissues on the same slide were detected by using double-stain Immunohistochemistry (DS-ABC).
RESULTS: Among the 55 cases of gastric carcinoma tissues, 30 were positive for TGF-β1 (54.55%). The MVD of TGF-β1 strong positive group (++~+++ 23.22 ± 5.8) was significantly higher than that of weak positive group (+17.56 ± 7.2) and negative group (-17.46 ± 3.9) (q = 4.5, q = 5.3207, respectively, P < 0.01). In the areas of high expression of TGF-β1, MVD and the expression of CD105 were also high. Among the 44 cases of colonic carcinoma tissues, 26 were positive for VEGF (59.1%). The expressions of both VEGF and CD105 (MVD) were related with the depth of invasion (F = 5.438, P < 0.05; F = 4.168, P = 0.05), lymph node metastasis (F = 10.311, P < 0.01; F = 20.282, P < 0.01) and Dukes stage (F = 6.196, P < 0.01; F = 10.274, P < 0.01), but not with histological grade (F = 0.487, P > 0.05). There was a significant correlation between the expression of VEGF and CD105 (MVD) (r = 0.720, P < 0.01).
CONCLUSION: Over-expression of TGF-β1 and VEGF acts as stimulating factors of angiogenesis in gastrointestinal tumors. CD105, as a receptor of TGF-β1, can regulate the biological effect of TGF-β1 in tumor angiogenesis. MVD marked by CD105 is more suitable for detecting newborn blood vessels.
- Citation: Yu JX, Zhang XT, Liao YQ, Zhang QY, Chen H, Lin M, Kumar S. Relationship between expression of CD105 and growth factors in malignant tumors of gastrointestinal tract and its significance. World J Gastroenterol 2003; 9(12): 2866-2869
- URL: https://www.wjgnet.com/1007-9327/full/v9/i12/2866.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i12.2866
Angiogenesis occurs in diverse physiological and pathological situations and particularly in tumour growth. The development of a new blood vessel is a complex phenomenon and the result of a sequence of events, among which the release of growth factors of interstitial cells is the most important step. At present, many growth factors have been identified including transforming growth factor (TGF)-β1 and endothelial cell growth factor (VEGF). TGF-β1 is a potent inhibitor of endothelial cells (EC) proliferation and migration in vitro and an angiogenesis promoter in vivo. It has aroused much interests in study of the relationship between TGF-β1 and angiogenesis. In this research, we used CD105, a new EC marker, to count the intratumor microvessel density (MVD), and to detect the expression of TGF-β1 in 55 gastric carcinoma tissues. Because CD105 is one of the receptors of TGF-β1, we hoped to find out the biological effect of TGF-β1 by studying the relationship between the ligand and the receptor. We also detected the expression of VEGF and CD105 (MVD) in 44 colorectal carcinoma tissues and analyzed the effect of VEGF in angiogenesis of colorectal carcinoma tissues. Furthermore we demonstrated the confidence level and superiority of CD105 in studying tumor angiogenesis.
Two groups of patients were chosen and examined. Group A: Fifty-five specimens of freshly resected malignant gastric tissues were collected from 55 patients with gastric carcinoma (median age 57.65 ± 5.3 years, range 29-77 years) who were operated in Qingdao Municipal Hospital and the Affiliated Hospital of Medical College, Qingdao University (Shandong, China) from October 2000 to April 2001. Four cases were well-differentiated adenocarcinoma, nine moderately-differentiated adenocarcinoma and forty-two poorly-differentiated adenocarcinoma. Among the 55 cases, 36 cases had lymph node metastasis and five cases had distant metastasis. Normal tissue samples located at least 8 cm away from the margins of cancers, and 51 normal gastric tissue samples were frozen in liquid nitrogen. Group B: Forty-four freshly resected malignant intestinal tissue samples were collected from 44 patients with intestinal carcinoma (median age 62.5 ± 6.2 years, range 31-79 years) who were operated in Qingdao Municipal Hospital and the Affiliated Hospital of Medical College, Qingdao University from July 2001 to March 2002. The group included one case of well-differentiated adenocarcinoma, thirty-eight cases of moderately-differentiated adenocarcinoma and five cases of poorly-differentiated adenocarcinoma. Among the 44 tumor patients, 20 cases had lymph node metastasis. 20 normal intestinal tissue samples taken at least 8 cm away from the margins of cancers were frozen in liquid nitrogen.
None of the patients in groups A and B received any chemotherapy or radiation therapy prior to surgery. Fresh tissue samples were collected within 4 hours after resection. The pathological diagnosis was made on the basis of the size, infiltrating depth, histological grade, lymph node and distant metastasis. The grading standard was in accordance with “Practical and surgical pathology”(Chen-Zhong Nian, published by ShangHai Medical University, first edition). Written informed consent was obtained from each patient.
Immunohistochemistry Biopsy specimens were snap frozen in liquid nitrogen and serial cryostat sections were cut into 7 μm thick. Paraffin-embedded sections were cut into 4 μm thick. Immunohistochemical staining (S-ABC) and immunohistochemical double staining (DS-ABC) were performed in accordance with the introduction of the kit. PBS was used as the negative controls instead of Mab.
Identification of immunohistochemical staining results TGF-β1/VEGF staining was classified into four grades. +++, most carcinoma cells were stained with a very strong intensity, and distributed in clusters. ++, a large number of carcinoma cells were stained with a moderate intensity, and distributed in clusters occasionally. +, a few carcinoma cells were stained with a slight intensity. -, no staining of carcinoma cells.
Counting of MVD in carcinoma tissues was in accordance with Weidner’s standards with a minor modification. The slide was searched for the hot spots rich in vessels, which were located in or near the area of tumor tissues under a low power microscope (100×). MVD was counted under a high power (400×) or low power (100×) microscope according to the standards that any stained endothelial cell or cells were identified as an independent vessel. These vessels must be clearly separated from each other. However, apparent vasa or vasa with red blood cells could be regarded as vessels. Five different HP vision fields were chosen on each of the slides, and the stained vessels were counted simultaneously by two doctors under a multi-ocular len microscope. The results were averaged, which was the relative value of the amount of vessels per unit area.
The relation between MVD and expression of TGF-β1 was studied with analysis of variance and Q-test. The analysis of variance and χ2-test were used for statistical analysis of the relation between MVD and expression of VEGF.
Among the 55 specimens in group A, 30 were positively stained and 25 negatively stained, with a positive rate of 54.55%. TGF-β1 was mainly existed in cytoplasms of carcinoma cells. In the 51 specimens of normal gastric tissues, TGF-β1 was mainly expressed in gastric mucosa epithelial cells.
Among the 44 cases in group B, 26 were positively stained and 18 negatively stained, with a positive rate of 59.1%. VEGF was mainly existed in cytoplasms of colorectal carcinoma cells.
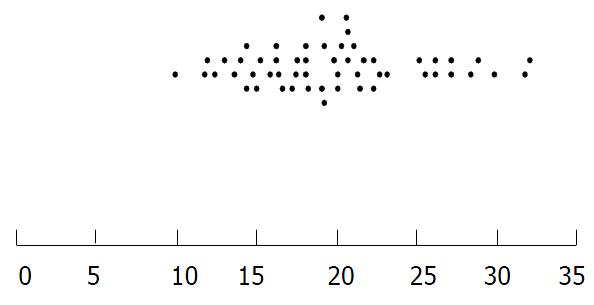
In both group A and group B CD105 was mainly expressed in cytoplasms and plasmalemma of newborn endothelial cells in cryostat section. CD105 was weakly expressed or absent in native blood vessels with thick walls and large lumina. MVD of gastric carcinoma tissues is listed in Figure 1.
When the gastric carcinoma tissues were double stained for CD105 and TGF-β1 in one cryostat section, TGF-β1 was highly expressed and so was CD105 in the same area. It was also found that newborn vessels were present around carcinoma nests whereas TGF-β1 was observed mainly in cytoplasms of carcinoma cells. The relation between MVD and TGF-β1 is shown in Table 1. Analysis of variance and Q-test were used to analyze the difference of MVD counting among the three different TGF-β1 staining groups. It showed that MVD of TGF-β1 strong positive group was significantly higher than weak positive group and negative group, and the MVD between the two groups of TGF-β1 staining weak positive “+”and negative “-” had no significant difference.
Analysis of variance showed the expression of VEGF was correlated with infiltrating depth (F = 5.438, P < 0.05), lymph node metastasis (F = 10.311, P < 0.01) and Duke’s staging (F = 6.196, P < 0.01), but had no relation with histological stage (F = 0.487, P > 0.05). MVD was correlated with infiltrating depth (F = 4.168, P = 0.05), lymph nodes metastasis (F = 20.282, P < 0.01) and Duke’s staging (F = 10.274, P < 0.01), but had no relation with histological stage (F = 0.006, P > 0.05), (Table 2).
| Clinical pathological parameters | Cases (n) | VEGF | Px value | MVD (CD105) | P value |
| Histological grade | |||||
| Well differentiation | 1 | 18.50 | 143.1 | ||
| Moderate differentiation | 38 | 22.28 ± 14.49 | > 0.05 | 144.8 ± 31.9 | > 0.05 |
| Poor differentiation | 5 | 21.89 ± 14.44 | 146.4 ± 47.4 | ||
| Infiltrating depth | |||||
| Serous membrane (-) | 5 | 9.37 ± 4.79 | < 0.05 | 119.0 ± 17.2 | = 0.05 |
| Serous membrane (+) | 39 | 22.55 ± 12.32 | 150.0 ± 32.7 | ||
| Lymph node metastasis | |||||
| (-) | 24 | 14.76 ± 9.62 | < 0.01 | 126.3 ± 20.8 | < 0.01 |
| (+) | 20 | 27.31 ± 12.17 | 167.7 ± 30.3 | ||
| Dukes stage | |||||
| A | 3 | 9.37 ± 4.79 | < 0.01 | 119.0 ± 17.2 | < 0.01 |
| B | 16 | 17.00 ± 10.37 | 129.3 ± 22.1 | ||
| C and D | 25 | 27.31 ± 12.16 | 167.7 ± 30.3 |
Angiogenesis refers to the formation of new blood vessels from native blood vessels, which is essential for the unrestricted growth and metastasis of solid tumors[1]. Thus, highly hyperplastic microvessels are usually recognized as a marker of malignant tumor development. At present, many growth factors have been identified including TGF-β1 and VEGF. These factors could be paracrined by tumor cells[2]. However, the potential roles of these factors, especially TGF-β1, are not clearly known.
Human TGF-β is a large family consisting of 3 isomers: TGF-β1, TGF-β2 and TGF-β3. TGF-β1, the most widely studied protein of the three TGF-β isomers, derived from a 390-amino acid precursor cleaved to produce a 112-amino acid carboxy-terminal peptide, is the predominant form in humans. TGF-β1 influences the proliferation rate of many cell types, acting as a growth inhibitor in most but not all cases. In addition, TGF-β1 controls the processes of epithelial cell differentiation. In normal cells, TGF-β1 generally enhances adhesion through increased matrix production and decreased proteolysis. Resistance to the negative growth regulating properties of TGF-β1 has been observed in epithelial and mesenchymal tumors. In addition to a stimulator of angiogenesis, TGF-β1 also influences the growth of tumor cells directly or indirectly. Tumor cells can escape the inhibiting effect of TGF-β1 on normal cells at post- transcription level, receptor level or post-receptor level. When tumor cells are insensitive, TGF-β1 also can promote tumor metastasis through enhancing angiogenesis, adjusting the character of matrix, or adjusting the body’s immune response to tumor growth. TGF-β1 seems to affect tumor angiogenesis and play an important role in tumor progression in non-small cell lung carcinoma and lung adenocarcinoma. A significant correlation between TGF-β1 protein level and prognosis was detected by multivariate analysis[3]. Maehara[4] found that TGF-β1 was closely related to the invasion and metastasis of gastric cancer, and production of TGF-β1 in the tumor did not contribute to the total amount of TGF-β1 in the blood circulation. TGF-β1 might be associated with tumor progression by modulating angiogenesis in colorectal cancer and it could be used as a possible biomarker[5].
In the present study, 55 cases of gastric carcinoma tissues were stained for TGF-β1. 54.55% of these tissues were positively stained including 21 strong positive cases “+++~++”, 9 positive cases “+”, 25 negative cases “-”. MVD between the two groups of “+” and “-” staining had no significant difference (P > 0.05), but MVD of the group of “+++~++” was significantly higher than the groups of “+” and “-” (P < 0.01). Therefore, we propose that overexpression of TGF-β1 be positively correlated with MVD in tumors and one of the bio-effects of TGF-β1 act as a stimulating factor of angiogenesis in vivo. In our other studies, TGF-β1 was highly expressed in gastric carcinoma tissues with lymph node metastasis and distant metastasis.
TGF-β1 exerts its functions through binding its receptors. Receptors for TGF-β family include type I, type II, type III and CD105. CD105 could act as an auxiliary protein in the ligand-receptor compound and regulate the function of TGF-β1[6]. It has been found to mainly localize in vascular endothelial cells in normal or tumor tissues. Calabro[7] detected soluble TGF-β1 and CD105 (sCD105) in hematopoietic malignancies, and showed that high levels of sCD105 were present in myeloid malignancies characterized by a high cellular proliferation rate, and suggested that an altered balance between sCD105 and sTGF-β1 might favor disease progression and clinical complications.
In this study we used double staining to detect the expression of CD105 and TGF-β1 in one gastric carcinoma section, and found that CD105 was highly expressed around these cancer cells with more TGF-β1.
VEGF, also named vascular permeability factor, can specifically direct to endothelial cells and is one of the most important factors to induce, up-regulate and migrate angiogenesis. VEGF is a kind of dimer glycoproteins, with a molecular weight of 34-50 kD. VEGF specifically promotes the mitosis and proliferation of endothelial cells by paracrine. Furthermore, VEGF can induce angiogenesis, increase the permeability of vessels and stimulate endothelial cells to produce protease and other low molecule proteins. In addition, VEGF can significantly prolong the life span of endothelial cells, increasing the mitosis to 15-20 fold. Further studies showed VEGF could improve the function of vesicles in endothelial cells, thus increasing the permeability of vessels, which facilities tumor cells to invade the vessels and distant migration. Therefore, VEGF can effectively promote angiogenesis and maintain its existence.
Kaio[8] found that lymph node metastasis and VEGF expression were significant risk factors in advanced colorectal carcinoma patients. Song[9] noticed VEGF was closely related to gastric carcinoma angiogenesis, and involved in tumor progression and lymph node metastasis. Some other studies showed that high VEGF expression or high MVD would indicate a poor prognosis in breast carcinoma patients[10] or high VEGF could be a marker of metastasis and invasion in squamous cell carcinomas[11]. In our study, VEGF and MVD marked by CD105 were highly expressed in colorectal carcinoma tissues. The expression of VEGF and MVD in colorectal carcinoma tissues was closely related to infiltrating depth, lymph node metastasis and Duke’s staging but not related to histological staging. These observations suggested that the expression of VEGF and MVD in colorectal carcinoma tissues was important in monitoring tumor invasion, lymph node metastasis and Duke’s staging.
Our previous correlation analysis showed that the expression of VEGF was positively related to MVD, further proving the causality of VEGF and MVD, i.e., VEGF could stimulate angiogenesis through paracrine in colorectal carcinoma tissues and thus promoting the growth, infiltration and metastasis of tumors.
Newborn blood vessels have their own construction features. For example, the new vessels in tumor tissues do not further differentiate or rebuild corresponding arteries and veins, which means that newborn vessels have no smooth muscle and cannot contract. Newborn vessels in tumors are highly winded, sinusoid and slender. Functionally, blood stream in new vessels is irregular, tending to result in thrombosis or hemorrhage spontaneously. In this case, tumor cells invade into new vessels and are carried to other organs, continuing to grow and become a metastasis. The more the newborn blood vessels are, the greater the possibilities of metastasis are. Because of the important effects of newborn vessels, great attention has been paid to the studies of angiogenesis.
While counting newborn blood vessels, most researchers selected several normal endothelial cell markers, such as CD31, CD34 and von Willerbrand (vWF). VWF, a factor VIII related antigen (VIII-RA), is a kind of EC marker that exists on EC of normal tissues. Many experiments showed that VIII-RA mainly existed in completely mature vessels, and the chapter restricts its utilization in angiogenesis of tumor tissues. CD31, a member of cell adhesion molecules, often participates in the adhesiveness of platelets in inflammation and wound. Parums pointed out that anti-CD31 monoclonal antibody could also bind normal blood vessels. CD34 is a transmembrane glycoprotein with a MW of 110 kD, and can express on endothelial cells. Ewoto[12] found that it was difficult to identify native or newborn vessels by using CD34. For this reason, CD34 is not an ideal marker of endothelial cells in the research of newborn vessels. Because of the heterogeneity of endothelial cells, the markers of normal endothelial cells are apparently unfit for the studies of angiogenesis in tumor tissues.
CD105, also called endoglin, is a new kind of cell adhesion molecules, first found by Quackenbush in pre-B cell line HOON[13]. CD105 mainly locates in EC and has become a new marker of EC[14]. CD105 is an endothelial homodimeric membrane antigen with 633 amino acid residues and its molecular mass is 180 kD. The gene of CD105 is located on 9q34, which is the target gene of HHT-I. Therefore, the expression of CD105 in EC showed it was highly related to the structure and function of EC[15]. Although CD105 can express in normal vessels, many studies showed CD105 could be detected more easily and reacted more strongly in tissues with angiogenesis.
Mab E9, a new murine anti-human monoclonal antibody, was produced by the Experimental Pathology Institute, Manchester University in early 1990’s. It belongs to immunoglobulin G (IgG). Mab E9 does not react with large vessels but with microvessels in tumor tissues strongly. The series of responses of Mab E9 showed its uniqueness from other antibodies. Wang stained the vessels in breast carcinoma tissues with antibody Mab5.6E (anti-CD31) and Mab E9 (anti-CD105), and found blood vessels in or around tumor tissues stained intensely for Mab E9, whereas the same blood vessels were either weakly positive or did not stain at all for CD31. Furthermore, in most cases, unlike Mab 5.6E, Mab E9 failed to stain (a) some apparently normal blood vessels in tumor tissues and (b) a few apparently normal blood vessels in normal tissues were entrapped within a tumor mass. In several normal breast tissues, Mab E9 alone stained only a proportion of blood vessels (-20%) that were positive for Mab 5.6E. Kumar stained CD34 and CD105 in series cryostat sections with Mab QBEND-10 and Mab E9, and found there was no relation between the two groups of MVD. The group of MVD marked with CD34 was only related to the size of tumors, while the group marked with CD105 could be the independent prognostic marker for patients with breast cancer. Further observation showed, in the same sites the native vessels were CD34 stained, and the newborn vessels were CD105 stained[16].
Because of the heterogeneity of endothelial cells, the markers of normal endothelial cells are apparently unfit for the studies of angiogenesis in tumor tissues. The growth of tumors includes not only the increase of blood vessels in number but also the change of protein molecules in structure of ECs. An ideal EC marker for angiogenesis should detect the newborn vessel quality as well as its quantity. Only in this way can we improve the sensitivity and credibility in detecting angiogenesis. From the above, it is reasonably believed that CD105 is a better marker of angiogenesis compared with CD34, CD31 and VIII-RA. Mab E9 increases the credibility in detecting angiogenesis. In our study, we used Mab E9 to stain MVD in malignant tumors of the gastrointestinal tract, so the credibility was high. We were able to prevent the possibility of mistaking native vessels for newborn vessels.
Edited by Zhu LH and Wang XL
| 1. | Griffioen AW, Molema G. Angiogenesis: potentials for pharmacologic intervention in the treatment of cancer, cardiovascular diseases, and chronic inflammation. Pharmacol Rev. 2000;52:237-268. [PubMed] |
| 2. | de Jong JS, van Diest PJ, van der Valk P, Baak JP. Expression of growth factors, growth-inhibiting factors, and their receptors in invasive breast cancer. II: Correlations with proliferation and angiogenesis. J Pathol. 1998;184:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Hasegawa Y, Takanashi S, Kanehira Y, Tsushima T, Imai T, Okumura K. Transforming growth factor-beta1 level correlates with angiogenesis, tumor progression, and prognosis in patients with nonsmall cell lung carcinoma. Cancer. 2001;91:964-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Maehara Y, Kakeji Y, Kabashima A, Emi Y, Watanabe A, Akazawa K, Baba H, Kohnoe S, Sugimachi K. Role of transforming growth factor-beta 1 in invasion and metastasis in gastric carcinoma. J Clin Oncol. 1999;17:607-614. [PubMed] |
| 5. | Xiong B, Gong LL, Zhang F, Hu MB, Yuan HY. TGF beta1 expression and angiogenesis in colorectal cancer tissue. World J Gastroenterol. 2002;8:496-498. [PubMed] |
| 6. | Li C, Hampson IN, Hampson L, Kumar P, Bernabeu C, Kumar S. CD105 antagonizes the inhibitory signaling of transforming growth factor beta1 on human vascular endothelial cells. FASEB J. 2000;14:55-64. [PubMed] |
| 7. | Calabrò L, Fonsatti E, Bellomo G, Alonci A, Colizzi F, Sigalotti L, Altomonte M, Musolino C, Maio M. Differential levels of soluble endoglin (CD105) in myeloid malignancies. J Cell Physiol. 2003;194:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Kaio E, Tanaka S, Kitadai Y, Sumii M, Yoshihara M, Haruma K, Chayama K. Clinical significance of angiogenic factor expression at the deepest invasive site of advanced colorectal carcinoma. Oncology. 2003;64:61-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Song ZJ, Gong P, Wu YE. Relationship between the expression of iNOS,VEGF,tumor angiogenesis and gastric cancer. World J Gastroenterol. 2002;8:591-595. [PubMed] |
| 10. | Li HJ, Jing J, Zhao YB, Zhu JQ, Zhang SY, Shi ZD. [Tumor angiogenesis in node-negative breast carcinoma]. Ai Zheng. 2002;21:75-78. [PubMed] |
| 11. | Sauter ER, Nesbit M, Watson JC, Klein-Szanto A, Litwin S, Herlyn M. Vascular endothelial growth factor is a marker of tumor invasion and metastasis in squamous cell carcinomas of the head and neck. Clin Cancer Res. 1999;5:775-782. [PubMed] |
| 12. | Emoto M, Iwasaki H, Mimura K, Kawarabayashi T, Kikuchi M. Differences in the angiogenesis of benign and malignant ovarian tumors, demonstrated by analyses of color Doppler ultrasound, immunohistochemistry, and microvessel density. Cancer. 1997;80:899-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Fonsatti E, Del Vecchio L, Altomonte M, Sigalotti L, Nicotra MR, Coral S, Natali PG, Maio M. Endoglin: An accessory component of the TGF-beta-binding receptor-complex with diagnostic, prognostic, and bioimmunotherapeutic potential in human malignancies. J Cell Physiol. 2001;188:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 126] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Miller DW, Graulich W, Karges B, Stahl S, Ernst M, Ramaswamy A, Sedlacek HH, Müller R, Adamkiewicz J. Elevated expression of endoglin, a component of the TGF-beta-receptor complex, correlates with proliferation of tumor endothelial cells. Int J Cancer. 1999;81:568-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Bodey B, Bodey B, Siegel SE, Kaiser HE. Over-expression of endoglin (CD105): a marker of breast carcinoma-induced neo-vascularization. Anticancer Res. 1998;18:3621-3628. [PubMed] |
| 16. | Kumar S, Ghellal A, Li C, Byrne G, Haboubi N, Wang JM, Bundred N. Breast carcinoma: vascular density determined using CD105 antibody correlates with tumor prognosis. Cancer Res. 1999;59:856-861. [PubMed] |