Published online Oct 15, 2003. doi: 10.3748/wjg.v9.i10.2313
Revised: July 25, 2003
Accepted: August 2, 2003
Published online: October 15, 2003
AIM: Capsule endoscopy has demonstrated its clinical utility in the evaluation of small bowel pathology in several Western studies. In this prospective study, we aimed to determine the clinical utility, safety and tolerability of capsule endoscopy in the evaluation of suspected small bowel disease in an urban Southeast Asian population.
METHODS: We used the given (M2A) capsule endoscopy system in 16 consecutive patients with suspected small bowel pathology. In 9 patients the indication was obscure gastrointestinal bleeding, while in 6 patients it was to determine the extent of small bowel involvement in Crohn’s disease. One patient underwent capsule endoscopy for evaluation of chronic abdominal pain. Patient’s tolerability to the procedure was evaluated by standardized questionnaires and all patients were reviewed at one week to ensure that the capsule had been excreted without any adverse events.
RESULTS: Abnormal findings were present in 8 patients (50%). The cause of obscure gastrointestinal bleeding was determined in 5 out of 9 patients. Findings included 2 cases of angiodysplasia, 2 cases of jejunal ulcers and 1 case of both angiodysplasia and jejunal ulcer. One patient had small bowel erosions and foci of erythema of doubtful significance. Ileal lesions were diagnosed in 2 out of 6 patients with Crohn’s disease. Capsule endoscopy was well tolerated by all patients. One patient with Crohn’s disease had a complication of capsule retention due to terminal ileum stricture. The capsule eventually passed out spontaneously after 1 month.
CONCLUSION: Our study, which represented the first Asian series, further confirms the diagnostic utility, safety and tolerability of wireless capsule endoscopy.
- Citation: Ang TL, Fock KM, Ng TM, Teo EK, Tan YL. Clinical utility, safety and tolerability of capsule endoscopy in urban Southeast Asian population. World J Gastroenterol 2003; 9(10): 2313-2316
- URL: https://www.wjgnet.com/1007-9327/full/v9/i10/2313.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i10.2313
Small bowel imaging is important in the evaluation of obscure gastrointestinal bleeding[1], inflammatory disease of the small bowel[2] and tumours. The main methods of small bowel imaging have been either enteroscopy or small bowel barium studies in the evaluation of luminal pathology. Angiography is a diagnostic option in the context of suspected small intestinal bleeding. Push enteroscopy allows examination of only 80 to 120 cm of the small bowel beyond the ligament of Treitz, while intra-operative enteroscopy requires general anesthesia and laparotomy. Small bowel series and enteroclysis have limited sensitivity, and in particular, could not detect flat lesions such as angiodysplasia[3].
Wireless capsule endoscopy was first reported by Iddan et al[4] in 2000, and it represents a major advancement in the imaging of the small intestine. It is able to capture video-images of the mucosal surface of the entire length of the small intestine directly, and has been reported to be virtually pain-free since it is essentially propelled forward through the gastrointestinal tract by peristalsis, without the need for any air-insufflation.
Thus far all published data on the use of capsule endoscopy have been from Western countries, with only 2 case reports on its use from India. One was a case of ileal angiodysplasia[5] while another was that of small intestine tuberculosis[6].
In this prospective study, we aimed to determine the clinical utility, safety and tolerability of capsule endoscopy in the evaluation of suspected small bowel disease in an urban Southeast Asian population.
Consecutive patients with suspected small bowel pathology seen at the Division of Gastroenterology, Changi General Hospital, Singapore, were recruited. Indications for capsule endoscopy included obscure gastrointestinal bleeding, assessment of extent of small intestine involvement in Crohn’s disease, evaluation of chronic abdominal pain and assessment for small bowel pathology in the presence of malabsorption. Patients with the following conditions were excluded from the study: pregnant subjects, suspected small bowel obstruction, presence of cardiac pacemaker, subjects expected to undergo MRI examination before elimination of capsule and subjects with swallowing difficulty. The study was approved by the Hospital Ethics Committee. Informed consent was obtained from all patients before commencement of the study.
The given diagnostic imaging system is comprised of the 26 mm by 11 mm M2A® capsule which contains a miniscule color video-camera equipped with a localization feature, a data recorder which is a portable, battery operated external receiving/recording unit that receives data transmitted by the capsule and subsequently allows data downloading, the Rapid® Workstation, a modified personal computer which has been designed for storage, processing and presentation of captured images as well as generation of reports. The technical details have previously been described in an earlier paper[7].
After a 12-hour fast, subjects underwent capsule examination with the M2A® capsule according to the standard procedure. Briefly it involved attaching 8 sensory arrays to the abdomen based on a standard template. These arrays were then attached to the portable battery powered data recorder. The capsule was swallowed and subjects were advised that fluids were allowed after 2 hours and light snack after 4 hours. Subjects were then allowed to go home. After 8 hours, the subject returned and the equipment was removed and the data were downloaded into the Rapid® Workstation and the images were analyzed using the proprietary software. The subjects were asked to look for the capsule in the feces. They were also reviewed again at 1 week for any complications and to ensure that the capsule had passed out. If excretion of the capsule was not noticed by the subject, an abdominal X-ray would be done.
All subjects were asked about tolerability of the procedure in the following areas using a standardised questionnaire, which included ease of swallowing, pain or discomfort experienced during the procedure, pain or discomfort experienced after the procedure, overall tolerability of the procedure, and overall convenience of the procedure. The subjects were also evaluated at one week after procedure for any adverse events such as pain, nausea,vomiting and capsule impaction or retention.
Two gastroenterologists (Drs Tay-Meng Ng and Tiing-Leong Ang) reviewed the capsule images independently and reported on the findings. Questionable findings were discussed. Positive findings were defined as detected abnormalities that were potentially related to the presenting problem.
During the period from mid February to May 2003, 16 consecutive patients with suspected small bowel pathology and no contraindication to capsule endoscopy were recruited. Their mean age was 55.6 years (range: 19 to 82 years) with a male to female ratio of 9:7. Table 1 summarizes the patient profile, indication for capsule endoscopy and the results of the study.
| SN. | Age/sex | Indication for capsule endoscopy | Results of capsule endoscopy |
| 1 | 66/male | Extent of small bowel involvement in Crohn’s disease | Erythema in terminal ileum |
| 2 | 30/male | Extent of small bowel involvement in Crohn’s disease | Edematous small bowel |
| 3 | 62/female | Obscure gastrointestinal blood loss | Small bowel angiodysplasia |
| 4 | 39/male | Extent of small bowel involvement in Crohn’s disease | Ulcers and strictures in ileum |
| 5 | 28/male | Extent of small bowel involvement in Crohn’s disease | Normal small bowel |
| 6 | 74/female | Extent of small bowel involvement in Crohn’s disease | Gastric erosions; normal small bowel |
| 7 | 62/male | Obscure gastrointestinal blood loss | Gastric erosion; normal small bowel |
| 8 | 69/male | Obscure gastrointestinal blood loss | Jejunal ulcer; small bowel angiodysplasia |
| 9 | 59/female | Obscure gastrointestinal blood loss | Mild gastritis and duodenitis; normal small bowel |
| 10 | 82/female | Obscure gastrointestinal blood loss | Gastritis; small bowel angiodysplasia |
| 11 | 54/female | Extent of small bowel involvement in Crohn’s disease | Normal small bowel |
| 12 | 69/male | Evaluation for small intestine pathology in context | Normal small bowel |
| of chronic abdominal pain | |||
| 13 | 71/female | Obscure gastrointestinal blood loss | Jejunal ulcer |
| 14 | 66/female | Obscure gastrointestinal blood loss | Bleeding jejunal ulcer |
| 15 | 46/male | Obscure gastrointestinal blood loss | Normal small bowel |
| 16 | 19/male | Obscure gastrointestinal blood loss | Small bowel erosions and foci of erythema |
Nine patients had obscure gastrointestinal bleeding, having presented with anaemia and melaena. All underwent both gastroscopy and colonoscopy. These investigations did not reveal significant pathology that could have accounted for the bleeding. Push enteroscopy was done in 2 of these patients, and small bowel series were done in another 4. Apart from small bowel diverticula seen on small bowel series in one patient, the rest of the small bowel imaging were normal.
Six patients were diagnosed to have Crohn’s disease on the basis of characteristic clinical, endoscopic and histologic features. Capsule endoscopy was performed to determine the extent of small bowel involvement in these patients.
One patient had a problem of recurrent abdominal pain and capsule endoscopy was performed to exclude any small intestine pathology after previous endoscopies did not reveal any significant lesions.
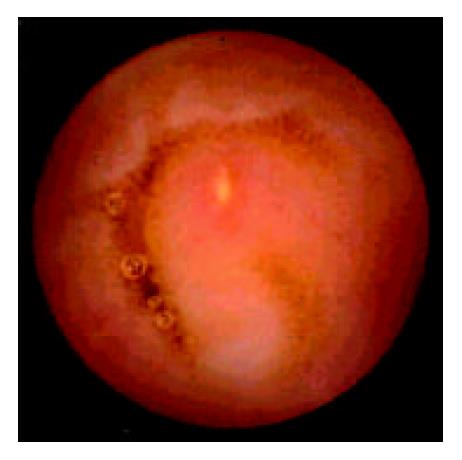
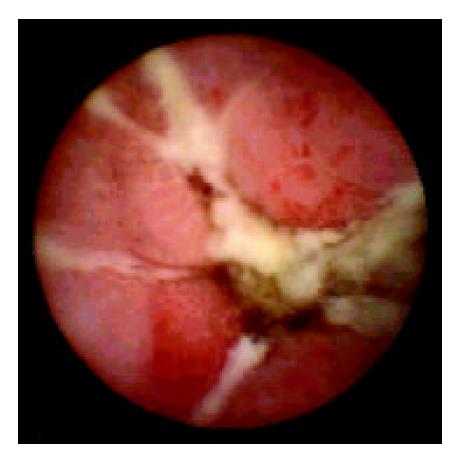
Among the 9 patients with obscure gastrointestinal bleeding, capsule endoscopy was able to diagnose a clinically significant pathology in 5 of them (55.6%). Two patients had jejunal ulcers (Figure 1). Two patients had angiodysplasia while the last patient had both angiodysplasia and jejunal ulcer. It was felt that the jejunal ulcers could have been related to NSAID usage. A sixth patient had the finding of small bowel erosions and foci of erythema, but the authors felt that these lesions could not have accounted for the gastrointestinal bleeding. Among the 6 patients with Crohn’s disease, capsule endoscopy revealed small bowel pathology in 2 cases. One patient had multiple ileal ulcers and strictures (Figure 2) while the other had erythema in the terminal ileum. These abnormalities were not detected by small bowel barium studies done prior to capsule endoscopy. Overall, abnormalities were present in 50% (8/16) of the subjects.
All the patients rated the procedure as comfortable and very convenient. Despite the size of the capsule being larger than most tablets, all the patients described swallowing as very easy. There was no complaint of pain or discomfort during or after the procedure. However, 2 of the patients commented on the weight of the portable recorder/battery pack.
The capsule was excreted in all the patients without any ill effects. One patient had retention of capsule beyond one week without developing any obstructive symptoms. It took 31 d before the capsule was noted to have passed out spontaneously. This was the patient with Crohn’s disease who had ileal ulcer and stricture. In fact, an attempt was made to retrieve it endoscopically at one week but it was unsuccessful. It was then decided to follow up the patient and wait for spontaneous passage of the capsule as he had remained asymptomatic throughout, rather then subject him to surgery. For the remaining 15 patients, the capsule was excreted within a week, six of these patients actually did not notice the passage of the capsule, but an abdominal X-ray done at one week proved that the capsule had not been retained.
Our study, which represented the first Asian series, further confirmed the diagnostic utility, safety and tolerability of wireless capsule endoscopy. In our series, it was able to reveal significant small intestine pathology in 43.8% (7/16) of the patients. In particular, for obscure gastrointestinal bleeding, it was able to reveal the cause in 55.6% of the patients. It was remarkably well tolerated, and apart from one patient with delayed capsule excretion, there were no complications. This complication highlighted the need to be vigilant towards the possibility of intestinal obstruction when considering the use of capsule endoscopy.
In a prospective study of 20 patients, Costamagna et al[7] confirmed the superiority of capsule endoscopy over small bowel radiographs in the diagnosis of suspected small bowel disease. Capsule endoscopy was able to detect abnormalities in 17 out of 20 patients, compared to 3 out of 20 using barium studies. Similarly, Scapa[8] in another prospective study found that among 35 patients with suspected small intestine pathology but normal small bowel series, capsule endoscopy was able to detect clinically significant small intestine pathology in 63% of (22/35) patients.
For the evaluation of obscure gastrointestinal bleeding, our results were comparable to other published data. Scapa[8] was able to find a source of bleeding in 75% (15/20) of his patients with obscure gastrointestinal bleeding. Lewis[9] had a positive yield of 55% (11/20) in the evaluation of obscure gastrointestinal bleeding with capsule endoscopy. Ell[10] detected a definite source in 66% of his patients.
For the diagnosis of Crohn’s disease, Fireman[11], Eliakim[12] and Herrerias[13] have demonstrated the clinical utility of capsule endoscopy in diagnosis as well as in assessment of the extent of disease. It was particularly relevant where conventional endoscopic and radiological techniques have not identified pathological findings but clinical suspicion based on symptoms and laboratory tests was strong. In our series, only 33% of the patients with Crohn’s disease had abnormal findings on capsule endoscopy. This probably simply reflected the actual prevalence of small bowel involvement in our series, rather than under-diagnosis, since alternative imagings, such as barium studies when done, did not reveal any small bowel lesions either. In addition it was recognized that about 1/3 of patients with Crohn’s disease had ileocolic disease, about 1/3 had colonic disease and about 1/3 had small bowel disease[14]. An important point to note was that one patient actually had ileal stricture that led to delayed excretion of the capsule. In this case, the presence of small bowel stricture was not suspected, as the patient did not have any clinical evidence of small bowel obstruction. It is therefore suggested that if Crohn’s disease is a diagnostic consideration, then small bowel series or enema should precede the use of capsule endoscopy in order to minimize the risk of capsule retention. It is also worth noting that despite the stricture, the capsule was able to pass out without any ill effect after 31 d. Therefore in the absence of any signs or symptoms of capsule impaction or obstruction, a conservative approach may be adopted, with the use of high dose steroid to reduce the inflammation and oedema so as to facilitate the passage of the capsule, as occurred in this patient with Crohn’s stricture.
Possible complications and limitations exist with any procedure, and capsule endoscopy is no exception, in spite of the high diagnostic yield. The key complication is that of capsule retention proximal to a stricture, and a 5% retention rate has been reported, with the need for surgery in less than 1% of patients[15]. Another concern is delayed passage of capsule due to slow transit time, resulting in capsule recording terminating before it has passed to the caecum, and hence incomplete data acquisition. Other limitations included difficulty in determining the exact site of the abnormality in the small bowel, inability to take tissue biopsy, problem of visual clarity due to intestinal fluids and long viewing time of the video, which could take up to 2 hours[7]. It is also costly, with the estimated cost of each capsule being greater than the cost of undergoing colonoscopy in the Singapore context. Thus it is likely that its use would remain selective, being reserved for situations when endoscopy or other imaging modalities have failed to achieve a definite diagnosis. These would include the investigation of obscure gastrointestinal bleeding, and in the context where clinical suspicion for Crohn’s disease is strong but the results of all other tests have been equivocal.
In conclusion, our study affirms the diagnostic utility and safety of capsule endoscopy in clinical practice. It has the promise to become a leading method in the evaluation of small bowel pathology, but limitations and the issue of cost need to be addressed.
Servicom Medical (Singapore) Pte Ltd: For provision of M2A® Capsules (Given Imaging Limited, Yoqneam, Israel)) for the study.
Edited by Wang XL
| 1. | Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000;118:201-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 321] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 2. | Gay GJ, Delmotte JS. Enteroscopy in small intestinal inflammatory diseases. Gastrointest Endosc Clin N Am. 1999;9:115-123. [PubMed] |
| 3. | Nolan DJ, Traill ZC. The current role of the barium examination of the small intestine. Clin Radiol. 1997;52:809-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1994] [Cited by in RCA: 1384] [Article Influence: 55.4] [Reference Citation Analysis (1)] |
| 5. | Nagral A, Nisar P, Nagral S, Maydeo A, Sampat M, Borkar D. Capsule endoscopy diagnosis of ileal anglodysplasia. Indian J Gastroenterol. 2003;22:64-65. [PubMed] |
| 6. | Reddy DN, Sriram PV, Rao GV, Reddy DB. Capsule endoscopy appearances of small-bowel tuberculosis. Endoscopy. 2003;35:99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 565] [Cited by in RCA: 517] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 8. | Scapa E, Jacob H, Lewkowicz S, Migdal M, Gat D, Gluckhovski A, Gutmann N, Fireman Z. Initial experience of wireless-capsule endoscopy for evaluating occult gastrointestinal bleeding and suspected small bowel pathology. Am J Gastroenterol. 2002;97:2776-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 194] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 9. | Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest Endosc. 2002;56:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 326] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 10. | Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 408] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 11. | Fireman Z, Mahajna E, Broide E, Shapiro M, Fich L, Sternberg A, Kopelman Y, Scapa E. Diagnosing small bowel Crohn's disease with wireless capsule endoscopy. Gut. 2003;52:390-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 271] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 12. | Eliakim R, Fischer D, Suissa A. Wireless capsule endoscopy is a superior diagnostic tool in comparision to barium follow-through and computerized tomography in patients with sus-pected Crohn's disease. Eur J Gastroenterol Hepatol. 2003;15:363-367. [RCA] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 169] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 13. | Carucci LR, Levine MS. Radiographic imaging of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:93-117, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Herrerías JM, Caunedo A, Rodríguez-Téllez M, Pellicer F, Herrerías JM. Capsule endoscopy in patients with suspected Crohn's disease and negative endoscopy. Endoscopy. 2003;35:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Cave DR. Wireless video capsule endoscopy. Clinical Perspec-tives Gastroenterol. 2002;5:203-207. |