Published online Jun 15, 2002. doi: 10.3748/wjg.v8.i3.558
Revised: January 23, 2002
Accepted: March 7, 2002
Published online: June 15, 2002
AIM: Common bile duct microlithiasis (CBDM) is found in majority of patients with acute biliary pancreatitis (ABP) and no CBD stones in fluoroscopy during urgent ERCP. It is unclear, however, weather CBDM is a cause or the result of the disease. This prospective study was done to investigate the presence and density of CBDM in patients with ABP, when endoscopic retrograde cholangiopancreatography (ERCP) was done in different periods from the onset of the disease.
METHODS: One hundred fifty one consecutive patients with ABP and no CBDS on ERCP, performed as an urgent (< 24 h of admission) procedure, (101 - with gallbladder stones, 50 post-cholecystectomy patients), treated during last 4 years were prospectively included to the study. The presence and density of CBDM (cholesterol monohydrate crystals-CMCs and calcium bilirubinate granules-CBGs) in bile collected directly from common bile duct during ERCP was prospectively calculated according to Juniper and Burson criteria. High density of crystals was considered, when we found > 10 CMCs and/or > 25 clusters of CBGs on 1 slide.
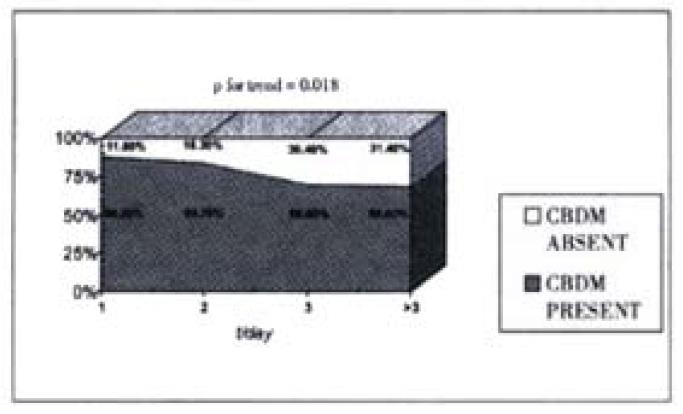
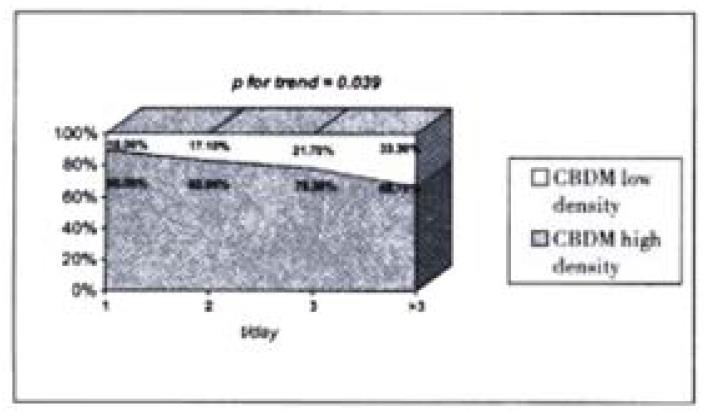
RESULTS: CBD microlithiasis was present in given number of patients: on d1-30/34 (88.2%), on d2-41/49 (83.7%), on d3-23/33 (69.6%), on d4-7-24/35 (68.6%) [P for trend = 0.018]. In patients with CBD microlithiasis the high density of crystals was observed in given number of patients:on d1-27/30 (90%), on d2-34/41 (82.9%), on d3-18/23 (78.3%), on d4-7-16/24 (66.7%) [P for trend = 0.039].
CONCLUSION: In patients with ABP and no CBDS on ERCP, CBD microlithiasis is observed in the majority of patients, especially during the first day of the disease. Density of CBD microlithiasis is the highest in the first day of the disease. This suggests that CBD microlithiasis can be the cause and not the result of ABP.
- Citation: Kohut M, Nowak A, Nowakowska-Dulawa E, Marek T. Presence and density of common bile duct microlithiasis in acute biliary pancreatitis. World J Gastroenterol 2002; 8(3): 558-561
- URL: https://www.wjgnet.com/1007-9327/full/v8/i3/558.htm
- DOI: https://dx.doi.org/10.3748/wjg.v8.i3.558
Some cases of acute biliary pancreatitis (ABP) are due to the biliary microcrystals (microlithiasis). The pathogenesis of acute pancreatitis (AP) produced by biliary crystals is unknown. It is probably related to the temporary impaction or migration of very small stones or clusters of crystals at the level of the ampoule of Vater. The mechanism of such pancreatitis is presumably the same as that when "normal size" biliary stones are impacted in the ampoule of Vater in the onset of the disease[1,2]. Literature on this problem started with simple case reports[3-5]. In the end of 1980’s and the beginning of 1990’s some larger series of patients with acute pancreatitis possibly associated with biliary sludge or microlithiasis were presented[1,6-10]. However, most of patients presented in these papers suffered from acute pancreatitis classified as so called "idiopathic" pancreatitis, as they do not bear gallbladder sludge, gallbladder stones and they did not have the history of cholecystectomy.
The methodology of these reports was based on the microscopic bile examination (MBE), which was a widely used technique in the diagnosis of gallstone disease before the advent of modern imaging procedures such as ultrasonography[11,12]. Almost all authors studied gallbladder bile obtained after stimulated gallbladder contractions via either blindly or endoscopicaly placed tube at the level of the papilla of Vater. Even in one of the best papers by Lee et al[6] the common bile duct bile has been investigated only in less than half of the patients. In the rest of cases the stimulated gallbladder bile was the matter of study. The minority of authors studied the bile obtained directly form the biliary tree on ERCP or via the T-tube placed in common bile duct during cholecystectomy with choledochotomy[13,14].
To our knowledge the study of common bile duct microlithiasis (CBDM) in patients with gallbladder stones or prior cholecystectomy and no CBD stones on ERCP is scanty[13,14]. In our previous paper we have found CBDM in vast majority of ABP cases (76%)[15]. One can argue, however, that the MBD microlithiasis can be the result and not the cause of the disease-CBD microlithiasis can be produced in the biliary tree due to the obstructed outflow of bile. This cholestasis can be related to the compression of distal common bile duct stone made by swollen pancreatic head during acute pancreatitis. Thus, we conducted the study of the presence and density of CBD microlithiasis in patients with ABP and no CBD stones on ERCP performed in the different periods from the onset of the disease. The aims of our work were to study the presence of CBD microlithiasis in different periods form the onset of the acute biliary pancreatitis, and the density of CBD mirolithiasis in patients with microlithiasis in different periods from the onset of acute biliary pancreatitis.
The study had been performed between September 1993 and January 1997 in the Department of Gastroenterology of the Silesian Academy of Medicine in Katowice, which is the reference centre for gastrointestinal diseases for approximately 4 million inhabitants area. Informed consent was obtained from all the subjects. Protocol of the study was approved by the local Ethics Committee in February 1993.
ERCP was done urgently-up to 24 hours of admission. Only patients with no more than 7 days from the onset of ABP were included to the study. We included patients with gallbladder stones or patients previously cholecystectomized. Patients without suspected biliary pathology [e.g. with pancreas divisum or with metabolic (hyperlipidaemia) acute pancreatitis] were excluded. Patients with alcoholic pancreatitis were also excluded. The diagnostic criteria for ABP were (both criteria must be present): (1) Typical clinical picture (epigastric pain), elevated levels of pancreatic enzymes (exceeding at least 3 times upper normal range), typical patterns of pancreatitis in abdominal imaging methods (ultrasonography, CT-scan), and (2) History of gallstones (e, g, cholecystectomy), positive laboratory criteria of biliary etiology of acute pancreatitis according to Goodman et al[16], gallstones on ultrasonography.
After the cannulation of the orifice of the ampoule of Vater was verified and the diagnostic catheter was placed in the common bile duct by injection of contrast medium (Meglumine diazotriacetas, Uropolinum, Polfa, Poland), the examiner confirmed that there were no "macroscopic" bile duct stones on fluoroscopy and X-ray films. Then the CBD bile was collected by manual suction through the standard ERCP catheters (Olympus and Boston Scientific companies) to the sterile syringe attached to the proximal end of the catheter. Approximately 5 mL of bile was achieved from every patient. All the following procedures were done in the sterile conditions. Immediately after the collection the bile sample was divided into two parts of the same volume. One part was examined immediately, while the second one was incubated in the temperature of 37 °C for 24 h. The presence of biliary microlithiasis was recorded as the combined result from both microscopic bile examinations. We established the diagnosis of CBD microlithiasis when at least we found crystals (immediately after incubation or on both microscopic bile examinations). The patients did not receive any antibiotic treatment prior to ERCP that can influence microscopic bile examination due to the drug precipitation in the bile.
The sample of bile was centrifuged 12000 r·min-1 for 10 min. Centrifugation enables to separate bile from the contrast medium we used during ERCP. The contrast medium floated over the bile after centrifugation. The sediment found on the bottom of the bile was than examined under direct and polarising light microscope, equipped with a heating stage. The same was done on the next day with the second portion of incubated bile. Three slides with bile sediment were examined for each sample. We prospectively used criteria of Juniper and Burson for counting crystals, as shown in Table 1[17]. Cholesterol monohydrate crystals (CMC) were identified on the basis of their rhomboid shape and their birefringence under cross-polarisation. Calcium bilirubinate granules (CBG) were identified on the basis of their reddish-brown colour and tendency to aggregate[17]. The number of crystals were graded as 1-4 when present and 0 when absent. Grades 1-4 corresponded to the grades specified by Juniper and Burson[17]. A positive result (at once, after incubation or both) for CMCs was taken if graded 1-4, and for CBGs if graded 3-4 (> 25 crystals per slide). The diagnosis of high density of crystals was done only if we have found > 10 CMCs and/or > 25 CBGs per one slide - as proposed by Juniper and Burson[17]. These criteria were derived directly from the original paper of Juniper and Burson, who discovered, that some cases with small number of calcium bilirubinate granules (graded 1 and 2, < 25 crystals per slide) were healthy and did not present cholelithiasis. All the bile samples were examined by one of the investigators, who were unaware of any clinical information.
| Number of crystals per one slide | Grading |
| < 10 | + |
| 10-25 | ++ |
| 25-40 | +++ |
| > 40 | ++++ |
The data were prospectively collected in the purpose-made data-base and analysed with the statistical package STATISTICA 5.0PL. The results are expressed as -x±s. Unpaired t Student tests (Fisher’s exact test-two-sided or Mann-Whitney’s test when needed) and chi-2 test when appropriate were used for statistical analyses. The level < 0, 05 was considered as statistically significant.
Demographic clinical and biochemical data of all the patients are shown in Table 2. The comparison of the characteristics of the patients with and without microlithiasis is given in the Table 3. There were no differences in the sex, mean age, the presence of gallbladder stones, mean BMI, mean levels of biochemical cholestasis (bilirubin, alkaline phosphatase and alanine transaminase) of patients in both subgroups. Presence and density of common bile duct microlithiasis (CBDM) in patients with acute biliary pancreatitis and no CBD stones on ERCP done in different periods from the onset of the disease are presented in Figure 1 and Figure 2, respectively. The results showed statistically significant decrease in the presence of microlithiasis, when the patient moved away from the onset of acute biliary pancreatitis. We observed also the fall in the presence of high density of microlithiasis. The highest density was in the first day of acute biliary pancreatitis, falling down in next days of the disease. These results also achieved the statistical significance.
| All cases | ||
| Number of patients | 151 | |
| Sex (M:F) | 49:102 | |
| Age (years) (-x±s) | 53.9 (± 15.7) | |
| Number of cases with gallbladder stones | 101 | |
| Number of cases with prior cholecystectomy | 50 | |
| Number of cases with Goodman’s criteria of | 129 | |
| ABP present (at least 1 criterion) | ||
| Ciochemical values (range, mean and SD) | Bilirubin (μmol·L-1) | 17-30654.57 (± 44.03) |
| Alkaline phosphatase (IU·L-1) | 57-556216.5 (± 115.3) | |
| Alanine transaminase (IU·L-1) | 16-1335351.2 (± 252.8) | |
| Feature | Microcrystals present (n = 118) | Microcrystals absent (n = 33) | P |
| Women | 91 | 11 | 0.066 |
| Men | 27 | 22 | 0.066 |
| Age [years] (mean) | 52.4 | 54.2 | 0.623 |
| Gallbladder stones present | 81 | 20 | 0.770 |
| BMI (mean) | 27.8 | 28.7 | 0.490 |
| Number of cases with Goodman’s criteria of ABP present (at least 1 criterion) | 106 | 23 | 0.670 |
| Bilirubin [(mol·L-1)] (mean) | 54.4 | 49.3 | 0.607 |
| Alkaline phosphatase [IU·L-1]](mean) | 213.7 | 178.9 | 0.148 |
| Alanine transaminase [IU·L-1]] (mean) | 350.4 | 383.4 | 0.577 |
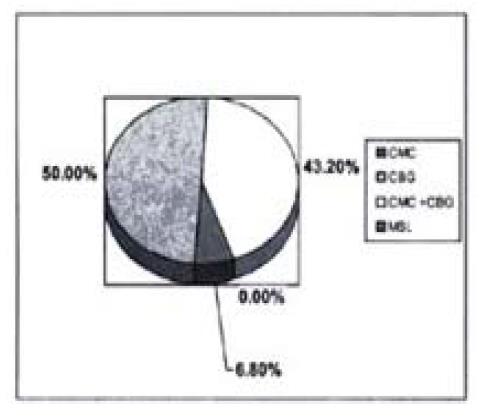
Results of microscopic bile examination (types of detected crystals) are shown in Figure 3. Calcium bilirubinate granules present alone (50% of cases with microlithiasis) were found the most frequently on MBE (Figure 3). CBGs together with CMCs were present in 43.2% cases with microlithiasis. Cholestrol monohydrate crystals were present alone only in 6.8% of patients with microlithiasis. We did not record any case of microspherolites.
Duodenal bile fractions was microscopically checked since decades in search for gallstone disease[11,12,17]. This method has shown the sensitivity and specificity around 70%-90%. The microscopic examination of stimulated gallbladder bile collected via the tube, placed either under radiological guidance or endoscope in the duodenum at the level of the papilla has been shown to be reliable in the diagnosis of gallstone disease as well[18,19]. Both methods of MBE had lost its attractivity after the advent of ultrasonographic examination of the gallbladder and bile ducts. However, the bile is still examined in some patients, especially with acute pancreatitis of uncertain origin[1,3,4-10]. Common bile duct bile has been microscopically examined in patients with endoscopically placed naso-biliary tube or surgically placed T-tube in CBD[13]. Sensitivity of 100% of such microscopic examination for CBD stones recognition was reported[13].
In another study common bile duct bile was obtained directly from the duct during ERCP[14]. We has shown the sensitivity of 85% in the diagnosis of choledocholithiasis[14] and the same methodology was used in this study.
Our study was designed to find out the presence and density of CBD microlithiasis in patients with acute biliary pancreatitis and no CBD stones on ERCP, when ERCP was done in different periods from the onset of the ABP. ABP was diagnosed according to the typical abdominal symptoms of acute pancreatitis, ultrasound and CT changes of pancreatic gland and the presence of gallbladder stones or prior cholecystectomy. All the patients presented also a significant (more than 2 × N) elevation of at least one of biochemical markers of cholestasis (alkaline phosphatase, alanine transaminase, and bilirubin).
ERCP is one of the diagnostic standards in choledocholithiasis. This method can give false (positive and negative) results, but the sensitivity and specificity of the method is believed to be above 90%-95%[20]. In this respect, we can exclude almost all cases with CBD stones during fluoroscopy with high confidence that our group of patients contains really no cases with CBD stones.
No one of the tested biochemical parameters achieved statistical significance as a marker of microcrystals (Table 2). Similar values of biochemical data in patients with or without microlithiasis can be explained by the finding of signs of recent stone passage through the papilla of Vater in some patients. Swollen papilla with enlarged (usually quite easy to cannulate) reddish orifice, sometimes with a drop of blood, were found on ERCP in some ABP patients, mostly without microlithiasis. In these patients elevated biochemical markers were seen, as in patients with microlithiasis and without recent passage signs. The absence of microlithiasis in patients with signs of recent passage of stone may be explained so called "flushing out" mechanism after decompression of bilio-pancreatic duct system. This deserves further studies.
Microcrystals within the biliary tree are present intermittently[19]. We observed very high percentage of microlithiasis in studied group of patients with ABP. This can be explained by the fact that majority of cases were admitted and ERCP performed on first three days of the disease. In previous studies, done few weeks or even months after the acute episode of acute pancreatitis, the percentage of cases with microlithiasis was lower[3-5,7-9,11,12,18].
The main idea behind our study was to exclude the biliary microlithiasis as the result of acute pancreatitis. The presented results confirmed our presumption, that the percentage of cases with microlithiasis falled down, when the beginning of the acute pancreatitis was becoming distant. The percentage of patients with high density of microlithiasis also falls down with time. We can speculate that the high density microlithiasis was potentially more harmful in the sense, that it can easily aggregate at the level of the orifice of the ampoule of Vater, leading to the obstruction of the outflow of pancreatic juice. It suggests, that microlithiasis is the cause and not the result of the acute pancreatitis.
Results of microscopic bile examinations, found in this study (Figure 3), confirm previous observation, that calcium bilirubinate granules (CBG) are more frequently found in patients with AP[1,6,7]. CBG were present alone (50%) or in association with CMC (43.2%) of all cases with microlithiasis. CMC were found alone in only 6.8% of cases. Previously CMCs were also less frequently found in endoscopically obtained duodenal bile, than in gallbladder bile in the same patient[21].
In our opinion one important etiopathogenetic conclusion comes from the study: microlithiasis can provoke acute biliary pancreatitis. Crystals can irritate the papilla, leading to inflammation of the papilla and obstructed outflow of pancreatic juice. If very high percentage of patients with microcrystals is present in the first day of ABP and if the high percentage of high density microlithiasis is also present in the first day of the disease, it seems logical to perform next step-the investigation of the influence of endoscopic sphincterotomy in such patients.
Edited by Pan BR and Zhang JZ
| 1. | Ros E, Navarro S, Bru C, Garcia-Pugés A, Valderrama R. Occult microlithiasis in 'idiopathic' acute pancreatitis: prevention of relapses by cholecystectomy or ursodeoxycholic acid therapy. Gastroenterology. 1991;101:1701-1709. [PubMed] |
| 2. | Acosta JM, Pellegrini CA, Skinner DB. Etiology and pathogenesis of acute biliary pancreatitis. Surgery. 1980;88:118-125. [PubMed] |
| 3. | Perrotta G, Pugliese G, Esposito R, Anselmucci W. [Acute pancreatitis in biliary microlithiasis: a study of the biliary sediment]. G Chir. 1989;10:646-648. [PubMed] |
| 4. | Block MA, Priest RJ. Acute pancreatitis related to grossly minute stones in a radiographically normal gallbladder. Am J Dig Dis. 1967;12:934-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Negro P, Flati G, Flati D, Porowska B, Tuscano D, Carboni M. Occult gallbladder microlithiasis causing acute recurrent pancreatitis. A report of three cases. Acta Chir Scand. 1984;150:503-506. [PubMed] |
| 6. | Lee SP, Nicholls JF, Park HZ. Biliary sludge as a cause of acute pancreatitis. N Engl J Med. 1992;326:589-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 311] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 7. | Neoptolemos JP, Davidson BR, Winder AF, Vallance D. Role of duodenal bile crystal analysis in the investigation of 'idiopathic' pancreatitis. Br J Surg. 1988;75:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Reyes López A, Miño Fugarolas G, Costán Rodero G, Pérez Rodríguez E, Montero Alvarez JL, Cabrera D. [Value of duodenal drainage in the etiologic diagnosis of acute pancreatitis]. Rev Esp Enferm Dig. 1993;83:363-366. [PubMed] |
| 9. | Bel FJ, Aparisi L, García-Tell G, Roselló JV, Rodrigo JM. [Biliary drainage in the diagnosis of microlithiasis. Value in acute idiopathic pancreatitis and in persistent pain in the right hypochondrium]. Rev Esp Enferm Dig. 1994;85:343-347. [PubMed] |
| 10. | Humbert P, Casals A, Boix J, Planas R, Morillas R, Barranco C, Villagrasa M. [Usefulness of microscopic study of the duodenal bile in the diagnosis of pancreatitis of unknown cause]. Rev Esp Enferm Apar Dig. 1989;75:471-474. [PubMed] |
| 11. | Lyon BBV. Diagnosis and treatment of diseases of the gallbladder and biliary ducts. J Am Med Assoc. 1919;73:980-986. [RCA] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Bockus HL, Shay H, Willard JM. Comparison of bile drainage and cholecystography in gallstone disease with special reference to bile microscopy. J Am Med Assoc. 1931;96:311-317. [RCA] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Agarwal DK, Choudhuri G, Saraswat VA, Negi TS. Utility of biliary microcrystal analysis in predicting composition of common bile duct stones. Scand J Gastroenterol. 1994;29:352-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Buscail L, Escourrou J, Delvaux M, Guimbaud R, Nicolet T, Frexinos J, Ribet A. Microscopic examination of bile directly collected during endoscopic cannulation of the papilla. Utility in patients with suspected microlithiasis. Dig Dis Sci. 1992;37:116-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Nowak A, Kohut M, Nowakowsa-Dulawa E, Marek TA, Kaczor R. Common bile duct microlithiasis in patients with acute biliary pancreatitis and no CBD stones on ERCP. Digestion. 1998;59:494. |
| 16. | Goodman AJ, Neoptolemos JP, Carr-Locke DL, Finlay DB, Fossard DP. Detection of gall stones after acute pancreatitis. Gut. 1985;26:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 71] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | JUNIPER K, BURSON EN. Biliary tract studies. II. The significance of biliary crystals. Gastroenterology. 1957;32:175-208; discussion, 208-11. [PubMed] |
| 18. | Abbas A, Baumann R, Schutz JF, Maillard D, Sondag D, Weill JP. [Cholesterol crystals and biliary lithiasis. Importance of the study of bile collected by duodenal intubation]. Gastroenterol Clin Biol. 1984;8:454-457. [PubMed] |
| 19. | Marks JW, Bonorris G. Intermittency of cholesterol crystals in duodenal bile from gallstone patients. Gastroenterology. 1984;87:622-627. [PubMed] |
| 20. | Prat F, Amouyal G, Amouyal G, Pelletier G, Choury AD, Buffet C, Etienne JP. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common bile duct lithiasis. Lancet. 1996;346:75-79. [RCA] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 168] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Janowitz P, Swobodnik W, Wechsler JG, Zöller A, Kuhn K, Ditschuneit H. Comparison of gall bladder bile and endoscopically obtained duodenal bile. Gut. 1990;31:1407-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 1.1] [Reference Citation Analysis (0)] |