Published online Jun 15, 2000. doi: 10.3748/wjg.v6.i3.448
Revised: February 3, 2000
Accepted: February 26, 2000
Published online: June 15, 2000
- Citation: Hong DF, Gao M, Bryner U, Cai XJ, Mou YP. Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. World J Gastroenterol 2000; 6(3): 448-450
- URL: https://www.wjgnet.com/1007-9327/full/v6/i3/448.htm
- DOI: https://dx.doi.org/10.3748/wjg.v6.i3.448
The advent of laparoscopic cholecystectomy (LC) in the late 1980s gained widespr ead acceptance within a short period of time and has become the preferred treatment for symptomatic gallstones[1-7], but the management of coexisting gallbladder and common bile duct (CBD) stones has remained controversial because t he various strategies proposed have their limitations[8-12]. In fact, choledocholithiasis is found in 10%-15% of patients cholecystolithiasis, and most authors agree that at least 90% of CBD stones are secondary to those of the gallbladder, and that CBD stones must be extracted in timely manner in order to avoid consequent complications which would otherwise occur in at least 90% of patients[1-4]. This paper will introduce and evaluate a new approach of management of coexisting gallbladder and CBD stones-intraoperative endoscopic sphincterotomy (IOES).
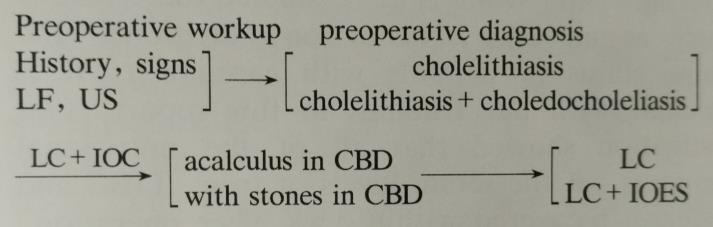
From December 1997 to August 1999, twenty-seven patients with cholelithiasis and CBD stones were treated by LC and IOES. Chole docholithiases were detected in 9 patients by preoperative ultrasonography and 18 routine intraoperativechol angiography (IOC). They were 5 males and 22 females. The youngest patient was 23 years old, the oldest being 74 years, averaging 50.3 years. The preoperative diagnoses are summarized in Table 1. All patients were treated according to a standard protocol(Figure 1).
| Preoperative diagnosis | NO. of patients |
| Acute cholecystitis with multiple gallstones | 3 |
| Chronic cholecystitis with multiple gallstones | 15 |
| Acute cholecystitis with multiple gallstones and CBDs | 3 |
| Chronic cholecystitis with multiple gallstones and CBDs | 6 |
LC was undertaken by the four trocar technique and IOC was performed according to the technique described by Alfred Cuschieri and Hong[1,2]. As soon as the CBD stones were confirmed, the endoscopist was expected on call. The patient lay in supine position, after deflating abdominal CO2, the endoscope (Olympus JF100 or a side-view JF100, JF140) was advanced into the duodenum. Once the position of ampulla of Vater was determined, EST was undertaken routinely. The size of sphincterotomy was about 0.8-1.5 cm. The CBD stones were extracted in different ways according to their size, shape and number. The small stones (less than 8 mm) were expelled into the duodenum with the help of surgeons by injecting normal saline through the cholangiogram catheter, medium sized stones (8-15 mm) were extracted with the basket (Olympus FG -23Q-1) or by a balloon (Wilson-cook EBL-12-200, EBL-8.5-200) monitored under fluoroscopy, large stones (more than 15 mm in diameter) were eliminated by basket or balloon after mechanical lithotripsy. After IOES and removal of CBD stones, the repeated IOC was performed to make sure that there were no retained CBD stones. The endoscope was withdrawn while aspirating the residual air. The LC was then completed.
The IOES was technically successful in 26 of 27 patients (96.30%) and the CBD stones were removed in all of these cases (100%). In 5 cases, the stones were expelled into the intestinal tract spontaneously, in 17 cases, extracted by basket or balloon and in 4 cases, removed after mechanical lithotripsy. The number of CBD stones ranged from 1 to 15, and the size of the stones varied from 3 mm to 16 mm. In one case, IOES failed because the sphincterome could not cannulate the ampulla of Vater due to stones impacted tightly the distal portion of CBD. Two cases were complicated with mild acute pancreatitis (7.69%) which resolved within 3 d and 7 d being fasted and intravenously supplemented fluid. No other complications occurred. There were no operative mortalities. The average operation time of LC combined with IOES was about 160 min (from 80 min to 210 min). All but 3 cases recovered uneventfully leaving bed and resuming food 8-4 h after LC and IOES. On e patient developed pneumothorax after LC procedure. In the other two cases recovery was delayed due to the complication of mild acute pancreatitis (mentioned above). The mean duration of hospital stay was 1 d to 26 d (3 d ± 1 d). The patient who had the pneumothorax was discharged on the 26th postoperative day.
It is well known that LC has become the primary method of treatment of symptomatic gallstones. Of the 500000 cholecystectomies performed annually in the United States, 85% of them are estimated now to be performed laparoscopically[13]. In China LC is also rapidly accepted. Likewise, the introduction of ERCP and EST in the 1970s rapidly revolutionized the management of CB D stones. Numerous series of cases have shown successful endoscopic clearance of the CBD stones in approximately 90% of patients, complications of EST occur in 5%-15%, most of these are minor, and the mortality is less than 1%. New instrumentation is being developed and improved continuouosly enabling the endoscopis t-surgeon to deal more and more successfully and creatively with a varity of in tra-abdominal conditions[4-6]. But the management of coexisting gallbladder and CBD stones is now more controversial than before, because many approaches to resolve this problem have their limitations besides the expense: and time (Table 2)[8-12].
| Methods | Shortcomings |
| Convert to open choledochostomy | loss of all advantages of minimally invasive surgery |
| Laparoscopic transcystic duct choledochoscopy | limited by cystic duct anatomy and risk associated with cystic duct dilation |
| Laparoscopic choledochostomy | Installation of T-tube and high technical demand |
| Preoperative ERCP and EST | hard to precisely predict preoperative CBD stones; if failed, subsequent operation should be considered |
| Postoperative ERCP and EST | If failed, another operation should be performed |
From May 1994 to November 1997, 1794 cases of LC and IOC were performed in our hospital. In about 7%-8% of patients with cholecystolithiasis[2,3], CBD stones were also found, we removed them by various methods such as converting to open choledochostomy, laparoscopic choledochostomy, laparoscopic choledochoscopy via cystic duct and postoperative EST. The results revealed that there was no best procedure for the patients, some shortcomings existed as shown in Table 2. Therefore, we employed a new approach of IOES from December 1997 to August 1999 to remove CBD stones identified at the time of LC.
The major advantages of combining LC and EST into one procedure are encouraging. The obvious benefit is that the patients have both problems solved at one session. But our 27 cases treated by LC combined with IOES only represent some o f the common bile duct explorations done at our hospital during this period due to the following reasons (among 1485 LC cases during this period). First, some surgeons in our department thought that IOES presents significant logistic difficulties in coordinating the necessary personnel and equipment. Second, it was thought that the supine position may increase the technical difficulty of EST[8-12]. But in our experience it is easier to remove the CBD stones by a combinati on of LC with IOES than by pre- or postoperative EST. The endoscopist gets benefit from general anesthesia. The surgeons can help the endoscopist to locate the proper position of the ampulla of Vater and irrigate the CBD by injecting normal saline through the cholangiography catheter. Small or fragmented stones can be washed out with normal saline irrigation. Medium or large sized stones in CBD c an be removed with the help of a basket or balloon and by lithotripsy. By deflating the peritoneal cavity of CO2, the endoscopist was able to insufflate the d uodenum adequately for performing IOES, after aspirating the gastrointestinal air, LC was more easily accomplished. From our study, IOES was successful in 26 (96.30%) of 27 patients and CBD stones were cleared in all of them (100%), only two cases were complicated with mild acute pancreatitis (7.69%) resolved within 3-7 d with intravenous fluid and fasting. No death occurred postoperatively. The case of pneumothorax after LC recovered by conservative management. The total operative time compares favorably with that of standard LC with CBD exploration in our hospital.
We recommend IOES as a valid alternative approach to the removal of CBD stones during LC. It has been safe and effective, and less traumatic to the patient than other intraoperative procedures or pre-or postoperative EST.
Dr. De-Fei Hong, graduated from Zhejiang University as a postgraduate in 1999, fellow of general surgery, major in hepato-biliary disease, having 14 papers published in international journal.
Edited by You DY and Ma JY
proofread by Sun SM
| 1. | Cuschieri A, Berci G, Paz-Partlow M, Nathanson LK, Sackier J. Laparoscopic Biliary Surgery. : Black Scientific Publications 1992; . |
| 2. | Hong DF, Li JD, Cai XJ, Wang YD, Wang XF, Wei Q, Yuan XM, Chen WJ, Li LB, Suong XY. The special role of routine intraoperative cholangiography in laparoscopic cholecystectomy. Zhonghua Gandan Waike Zazhi. 1998;4:101-103. |
| 3. | Cai X, Wang X, Hong D, Li L, Li J. [The application of intraoperative cholangiography in laparoscopic cholecystectomy]. Zhonghua Waike Zazhi. 1999;37:427-428. [PubMed] |
| 4. | Liu CL, Lai E CS, Lo CM, Chu KM, Fan ST, Wong J. Combined laparoscopic and endoscopic approach in patients with cholelithiasis and choledocholithiasis. Surgery. 1996;119:534-537. [PubMed] |
| 5. | Kullman E, Borch K, Lindström E, Svanvik J, Anderberg B. Management of bile duct stones in the era of laparoscopic cholecystectomy: appraisal of routine operative cholangiography and endoscopic treatment. Eur J Surg. 1996;162:873-880. [PubMed] |
| 6. | Gong JP, Zhou YB, Wang SG, Gu HG, He ZP. Effect of endoscopic retrograde cholangiopancreatography, endoscopic sphincterotomy in assisting laparoscopic cholec ystectomy for cholelithiasis. Zhonghua Xiaohua Neijing Zazhi. 1997;14:229-231. |
| 7. | Phillips EH, Carroll BJ, Pearlstein AR, Daykhovsky L, Fallas MJ. Laparoscopic choledochoscopy and extraction of common bile duct stones. World J Surg. 1993;17:22-28. [PubMed] |
| 8. | Deslandres E, Gagner M, Pomp A, Rheauit M, Leduc R, Clermont R, Gratton J, Bernard EJ. Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointes Endos. 1993;39:54-57. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Grieve DA, Merrett ND, Matthews AR, Wilson R. Left lateral laparoscopic cholecystectomy and its relevance to choledocholithiasis. Aust N Z J Surg. 1993;63:715-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Fitzgibbons RJ, Deeik RK, Martinez-Serna T. Eight years' experience with the use of a transcystic common bile duct duodenal double-lumen catheter for the treatment of choledocholithiasis. Surgery. 1998;124:699-705; discussion 705-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M. Laparo-endoscopic "rendezvous": a new technique in the choledocholithiasis treatment. Hepatogastroenterology. 1998;45:1430-1435. [PubMed] |
| 12. | Nakajima H, Okubo H, Masuko Y, Osawa S, Ogasawara K, Kambayashi M, Hata Y, Oku T, Takahashi T. Intraoperative endoscopic sphincterotomy during laparoscopic cholecystectomy. Endoscopy. 1996;28:264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Gholson CF, Dungan C, Neff G, Ferguson R, Favrot D, Nandy I, Banish P, Sittig K. Suspected biliary complications after laparoscopic and open cholecystectomy leading to endoscopic cholangiography: a retrospective comparison. Dig Dis Sci. 1998;43:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |