Published online Aug 15, 1999. doi: 10.3748/wjg.v5.i4.353
Revised: May 3, 1999
Accepted: May 19, 1999
Published online: August 15, 1999
- Citation: Zhao WS, Zhi DS, Liu BP, Jiang W, Cong Z, Dong C. Stereotactic conformal radiotherapy of hepatic metastases: clinical analysis of 8 cases. World J Gastroenterol 1999; 5(4): 353-355
- URL: https://www.wjgnet.com/1007-9327/full/v5/i4/353.htm
- DOI: https://dx.doi.org/10.3748/wjg.v5.i4.353
It is always a routine to resect lesions of the body by surgery. Scientists have tried to obtain the same results without surgery, but failed. In recent years, with the development of multi-subject and high technology, lesions can be localized precisely with stereotactic technique. And with the help of computer and medical imaging technique, stereotactic conformal radiotherapy (SCR) has become a "no pain, no blood" surgery. At the same time, SCR is recognized globally, its therapeutic range has transferred from intracranial lesions to the lesions of extracranial sites of the body, and is expected to become an important method in conventional surgery. Therefore, it is called "surgery of the 21 century"[1]. From May 1997 to April 1998, we treated 8 cases of hepatic metastases with SCR and the results are reported below.
Eight patients (4 men and 4 women, 1-5 metastases/person) who received stereotactic high-dose radiation therapy for hepatic metastases (21 lesions) using an accelerator were included. Treatments were given from May 1997 to April 1998. The age ranged from 67 to 46 years (mean 55.4). Three cases had one lesion, 5 had more than one lesions (one case had 5 metastases). The maximal clinical target volume (CTV) was 232 cm3, and the minimal CTV 0.6 cm3. The majority of the patients had previously received treatment for various types of primary tumors. At the time of treatment most patients had one known lesion increased in size as assessed by repeated CT scanning. Biopsies for histopathological examinations were obtained from some patients during open surgery. The majority of the irradiated lesions were considered so typical for metastases.
Stereotactic conformal radiotherapy The stereotactic body-frame was used in treatment. For targets affected by the diaphragmatic motions due to breathing, a device was developed to minimize the motions to 1 cm or less[2]. The reproducible position of the patient in the frame was obtained by the vacuum pillow and two markers, chest and tibia marker respectively. These markers are set to predefined stereotactic coordinates, at which the markers should correspond to the tattoo-points on the skin over sternum and tibia to ensure a high reproducibility in the cranial-caudal direction.
Therapeutic technique Primarily, a positioning and drawing plan was worked out. A stereotactic system (including stereotactic setting and localization) was used for stereotactic radiotherapy (SRT) to improve the accuracy of localization and setting-up. A consecutive CT scan of 2 mm slice thickness was outlined manually on the computer screen in every horizontal CT-slice for patients with hepatic metastases. Target point and width of the collimator was calculated with specially designed computor programs. Beam′s eye view technique with digitally reconstructed radiographs from the transverse CT scans was adopted to design the 3-D treatment plan. The 3-D treatment planning is a conformal technique, using 6-8 non-coplanar stationary beams. On multi-leaf collimator, the shape of be am eye view was similar with the target in all directions. Patients were all treated with a liner accelerator (VARIAN Clinic 600C). The photon energies used were 6 Mev.
Dose distribution The dose planning was made on a 3-D system (Virtuos 2.8.0). Apart from dose distributions, the clinical target volume (CTV), planning target volume (PTV), and organs at risk volumes were also calculated. Several factors were taken into consideration when the dose/fraction was determined. These included size of the CTV, dose distribution with dose-volume histograms and radiation sensitivity of the surrounding normal tissues. In this series, the CTV of tumors ranged from 0.6 cm3 to 232 cm3 (mean 36.4 cm3), the prescribed dose (PD) was 4-6.5 Gy (mean 5.13 Gy). Treatments were given in 2-8 fractions. The total dose was 10-45 Gy/2-8 fractions.
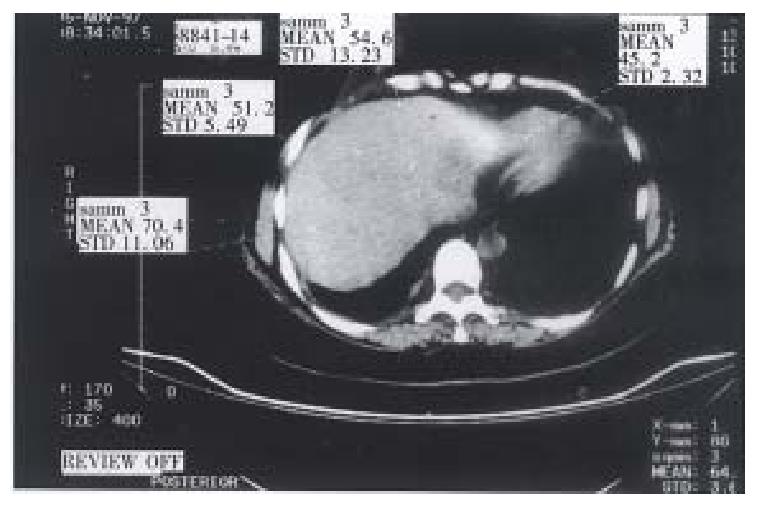
None of the patients died during SRT. Their condition was evaluated by Karnofsky Performance Standard (KPS), 20-90 before treatment (mean 58.75) and 30-100 after treatment. Very few, if any, complications could be ascribed to the SRT. Three (37.5%) patients developed slight fever (< 37.8 °C). WBC count and hepatic function had no distinct changes. During a follow-up period of 2-9 months, complete response (CR) was found in two cases (Figure 1, Figure 2), partial response (PR) in three cases, no change (NC) in two cases and progressed (PD) in one case. After SCR, 87.5% of tumors were controlled (62.5% of the tumors decreased in size or disappeared). Three patients died during the follow-up period, one died of bone metastases 303 months, one died of MSOF 1.5 months and one died of hepatic failure 2.3 months after treatment (Table 1).
| Patient No. | ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Sex (M/F) | M | M | F | F | F | M | F | M |
| Age (years) | 59 | 46 | 49 | 54 | 67 | 61 | 49 | 58 |
| Primary tumor | Colon | Lung | Breast | Breast | Preventriculus | Stomach | Breast | Cholecyst |
| Number of irradiated tumor | 1 | 3 | 1 | 4 | 2 | 5 | 4 | 1 |
| Volume of clinical | 34.5 | 1.9, 1.5 | 14.8 | 5.1, 0.6 | 18.4 | 232, 134.1 | 30.7, 11.6 | 120.3 |
| target (cm3) | 2.1 | 0.9, 0.9 | 16.7 | 75.2, 7.7, 23.7 | 3.3, 1.5 | |||
| Prescribed dose (Gy) | 5.00 | 4.50 | 5.00 | 5.00 | 5.00 | 4.00 | 6.00 | 6.50 |
| Number of fractions | 3 | 8 | 8 | 5 | 2 | 7 | 7 | 7 |
| KPS before treatment | 80 | 40 | 90 | 90 | 20 | 40 | 40 | 70 |
| KPS after treatment | 80 | 50 | 100 | 100 | 30 | 50 | 70 | 90 |
| Size of tumor after irradiation | NC | PD | CR | CR | NC | PR | PR | PR |
| Time period of follow-up | 8 | 4 | 6 | 6 | 2 | 3 | 3 | 2 |
| Time period after irradiation (months) | Unknown | 3.3 | 6 | 6 | 1.5 | 2.3 | 3 | 2 |
Most of all patients who receive SCR are advanced patients with tumor who underwent no surgery and conventional radiotherapy. Their prognosis is not well[3]. So SCR is a new method for late case of tumor.
In 1951, the term stereotactic radiosurgery was introduced by Leksell[4] who was a neurosurgeon in Karolinska Academy. In 1968, the first - knife of the world was developed successfully. It was an epochmaking event to neurosurgery and radiotherapy technique. Since the beginning of 1980, with the improvement of stereotactic system and collimator, stereotactic radiosurgery (X-knife)[5] has been performed to intracranial lesions with linear accelerator based radiosurgery, and soon the treatment extended from intracranial to extracranial tumors. For large and/or irregular lesions, linear accelerator, with circle and multi-leaf collimator was employed. The treatment can be achieved by a combination o f several non-coplanar rotational irradiations, each directed at the same point, thus representing a convergent beam irradiation technique. The 3-D treatment system demonstrates clinical superiority and flexibility to treatment planning.
Stereotactic radiotherapy is a system of 3-D treatment planning and radiotherapy-include hardware and software. X-knife software reconstructs radiograph from image data of CT, MRI and DSA. The 3-D treatment planning was designed by soft ware could be made standard or complex design based on these data from either single or multi-convergent. X-knife software can calculate radiation dose quickly and precisely. Dose-calculate formula is shown by dose-volume histograms (DVHs) on the screening display. Radiation dosage can be calculated by computer. Its important character is to deliver a highly focused radiation distribution to the target volume and to reduce the dose to surrounding normal tissues as much as possible[6].
Since SCR technique came into being, it has been used to treat intracranial lesions, primarily the AVM and intracranial tumors. In recent years, with the development of stereotactic technique for treatment of intracranial tumors, X-knife technique began to be applied to treat tumors of mediastinum, liver and retroperitoneal metastases in Karolinska Hospital in Sweden in 1993. Lax et al[7] created a method to treat abdominal malignant tumors with high-dose stereotactic radiotherapy.
In stereotactic radiotherapy, stereotactic technique (localization and setting- up) is used to improve localization accuracy and setting-up accuracy. The difference between SRT and SRS is, the conception of the former is fractional radiotherapy, the latter is single fraction. When the size of the tumor is large, either from radiobiology and radiophysiology or from clinic, SRT must be adopted instead of SRS[8]. Patients treated with SRT all obtained good therapeutic effects. The development of SCR technique will enrich the conventional surgery means. In tumor treatment, SCR will exert an indispensable effect. With the accumulation of clinical experience, SRT will play an important role in treatment of malignancies.
Dr. Wei-Sheng Zhao, male, born on 1946-04-19 in Tianjin City, graduated from Tianjin Medical University in 1970, now professor of surgery, majoring diagnosis and treatment of hepatic, gallbladder, thyroid and pancreatic diseases, having 38 papers published.
Edited by MA Jing-Yun
| 1. | Zhang J. Research and clinical practice of X knife. Shijie Yiliao Qijie. 1995;25-26. |
| 2. | Blomgren H, Lax I, Näslund I, Svanström R. Stereotactic high dose fraction radiation therapy of extracranial tumors using an accelerator. Clinical experience of the first thirty-one patients. Acta Oncol. 1995;34:861-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 656] [Cited by in RCA: 563] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 3. | Wu JP, Qiu FZ. Huang Jiasi Surgery. Vol 1, 5th ed. Beijing: Medical Publishing House 1992; 325-326. |
| 4. | Leksell DG. Stereotactic radiosurgery. Present status and future trends. Neurol Res. 1987;9:60-68. [PubMed] |
| 5. | Zhang KL, Xu T. Treatment of extracranial tumor with stereotactic radiosurgery and the biologic significance of fractional irradiation. Oncology, Foreign Medicine. 1996;23:325-326. |
| 6. | Chen BH. Stereotactic radioneurosurgery. Vol 1. Beijing: Beijing Publishing House 1994; 7. |
| 7. | Lax I, Blomgren H, Näslund I, Svanström R. Stereotactic radiotherapy of malignancies in the abdomen. Methodological aspects. Acta Oncol. 1994;33:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 374] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 8. | Hu YM, Gu XZ. Conformal radiotherapy: the development of irradiational technique. Chin J Radiol Tumors. 1997;6:8-11. |