Published online Feb 7, 2024. doi: 10.3748/wjg.v30.i5.499
Peer-review started: October 2, 2023
First decision: November 24, 2023
Revised: December 11, 2023
Accepted: January 12, 2024
Article in press: January 12, 2024
Published online: February 7, 2024
Processing time: 120 Days and 21.3 Hours
Superior mesenteric artery (SMA) syndrome is a rare cause of duodenal obstruction by extrinsic compression between the SMA and the aorta (SMA-Ao). Although the left lateral recumbent position is considered effective in the treatment of SMA syndrome, individual variations in the optimal patient position have been noted. In this report, we present two elderly cases of SMA syndrome that exhibited rapid recovery due to ultrasonographic dynamic evaluation of the optimal position for each patient.
Case 1: A 90-year-old man with nausea and vomiting. Following diagnosis of SMA syndrome by computed tomography (CT), ultrasonography (US) revealed the SMA-Ao distance in the supine position (4 mm), which slightly improved in the lateral position (5.7–7.0 mm) without the passage of duodenal contents. However, in the sitting position, the SMA-Ao distance was increased to 15 mm accompanied by improved content passage. Additionally, US indicated enhanced passage upon abdominal massage on the right side. By day 2, the patient could eat comfortably with the optimal position and massage. Case 2: An 87-year-old woman with vomiting. After the diagnosis of SMA syndrome and aspiration pneumonia by CT, dynamic US confirmed the optimal position (SMA-Ao distance was improved to 7 mm in forward-bent position, whereas it remained at 5 mm in the supine position). By day 7 when her pneumonia recovered, she could eat with the optimal position.
The optimal position for SMA syndrome varies among individuals. Dynamic US appears to be a valuable tool in improving patient outcomes.
Core tip: Superior mesenteric artery (SMA) syndrome is a rare cause of duodenal obstruction by extrinsic compression between the SMA and aorta. While the left lateral recumbent position has traditionally been recommended as conservative therapy for facilitating duodenal passage, recent studies have highlighted variations in the optimal position among patients. Here, we present two cases of SMA syndrome where rapid recovery was achieved through ultrasonographic dynamic evaluation of the individualized optimal positions. This pioneering report includes valuable images and a video of dynamic ultrasonography, contributing to improved prognosis by averting potentially life-threatening complications such as shock, pancreatitis, perforation, and hypokalemia.
- Citation: Hasegawa N, Oka A, Awoniyi M, Yoshida Y, Tobita H, Ishimura N, Ishihara S. Dynamic ultrasonography for optimizing treatment position in superior mesenteric artery syndrome: Two case reports and review of literature. World J Gastroenterol 2024; 30(5): 499-508
- URL: https://www.wjgnet.com/1007-9327/full/v30/i5/499.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i5.499
Superior mesenteric artery (SMA) syndrome is a rare cause of duodenal obstruction by extrinsic compression between the SMA and the aorta (SMA-Ao)[1-4]. Left untreated, it can lead to potentially lethal complications, including sudden death, shock, pancreatitis, gastric perforation, malnutrition and hypokalemia[5-9]. Hence, early diagnosis and treatments are imperative[10,11]. However, its nonspecific symptoms, such as nausea, appetite loss, and abdominal discomfort often lead to underdiagnosis in clinical practice[10-12]. Additionally, due to its rarity, therapeutic guidelines have not been established. While the left lateral recumbent position is generally considered to be effective in the treatment of SMA syndrome, literature on the optimal patient position is scarce[4,13-18]. Some reports suggest that the optimal position may not be limited to the lateral position but could include right recumbent and sitting positions, depending on the course of the SMA in relation to the aorta[14,15,17,18]. Therefore, the optimal position might differ for each patient, and we hypothesize that dynamic observation of the SMA-Ao distance by ultrasonography (US) is ideal to determine the optimal therapeutic position. Dynamic US has recently emerged as a valuable technique offering real-time and dynamic evaluation, as well as safe and quick access[19,20]. In this report, we present two cases of SMA syndrome that exhibited prompt recovery through ultrasonographic dynamic evaluation of the optimal position.
Case 1: A 90-year-old man arrived in the emergency department in our hospital with complaints of nausea, vomiting, and abdominal distention for several hours.
Case 2: An 87-year-old woman arrived in the emergency department in our hospital with complaints of nausea and recurrent vomiting.
Case 1: The patient had been treated with continuous positive airway pressure (CPAP) for sleep apnea syndrome since 2019. After CPAP therapy had started, he sometimes woke up with nausea and vomiting. During sleep, he remained mainly in the supine position because of CPAP. Several hours before his visit to our hospital in 2022, he received dental treatment in the supine position for 2 h, after which nausea and abdominal distension occurred.
Case 2: The patient had infectious diarrhea several months before coming to our hospital and lost 5 kg of body weight. The diarrhea recovered with conservative therapy. On the day coming to our hospital, she vomited frequently after dinner for several hours, then visited the emergency department in our hospital.
Case 1: The patient had undergone a right hemicolectomy for ascending colon cancer in 2009, with no recurrence. In the same year, he also underwent right ureteral reconstruction for right ureteral injury. Since 2019, he had been receiving CPAP therapy for mild sleep apnea syndrome. He had been on medications for hypertension, Alzheimer's disease, and paroxysmal atrial fibrillation since 2016.
Case 2: The patient had taken medication for hypertension.
Case 1: There was no significant personal and family history.
Case 2: There was no significant personal and family history.
Case 1: The patient was 166 cm in height and 52.0 kg in weight [body mass index (BMI), 18.9, there had been no body weight loss for several recent years]. The vital signs were normal: consciousness, clear; blood pressure, 146/66 mmHg; heart rate, 53 beats/min; body temperature, 36.4 °C; respiratory rate, 16 breaths/min. The saturation of percutaneous oxygen (SpO2) was 96% at room air. His abdomen was slightly distended with mild epigastric tenderness. There was no rebound tenderness. The abdominal sound was almost normal peristalsis. Surgical scars from right hemicolectomy were visible in the midline abdominal incision site for ascending colon cancer, located at the center and right of the abdomen.
Case 2: The patient was 161 cm in height and 42.4 kg in weight (BMI, 16.4). The vital signs were as follows: Cons
Case 1: Routine blood analyses showed no significant abnormalities: white blood cell (WBC) count, 5170 cells/µL; total bilirubin (TBil), 0.6 mg/dL; aspartate aminotransferase (AST), 20 IU/L; alanine aminotransferase (ALT), 13 IU/L; alkaline phosphatase (ALP), 66 IU/L; γ-glutamyl transpeptidase, 12 IU/L; serum amylase, 141 IU/L; blood urea nitrogen (BUN), 22.0 mg/dL; creatinine (Cr), 0.88 mg/dL; Na+/K+/Cl+ levels, 138/3.8/101 mmol/L; and C-reactive protein (CRP), 0.04 mg/dL. Blood pH was within the normal range (7.394).
Case 2: Elevated WBC count (8680 cells/µL) and CRP (3.59 mg/dL) indicated systemic inflammation. Elevated BUN (29.0 mg/dL) and Cr (1.29 mg/dL) indicated dehydration. Except for the elevated serum amylase (255 IU/L), other routine blood analyses were in normal range: TBil, 1.3 mg/dL; AST, 24 IU/L; ALT, 11 IU/L; ALP, 262 IU/L; Na+/K+/Cl+, 138/4.4/105 mmol/L. The blood pH was normal (7.366).
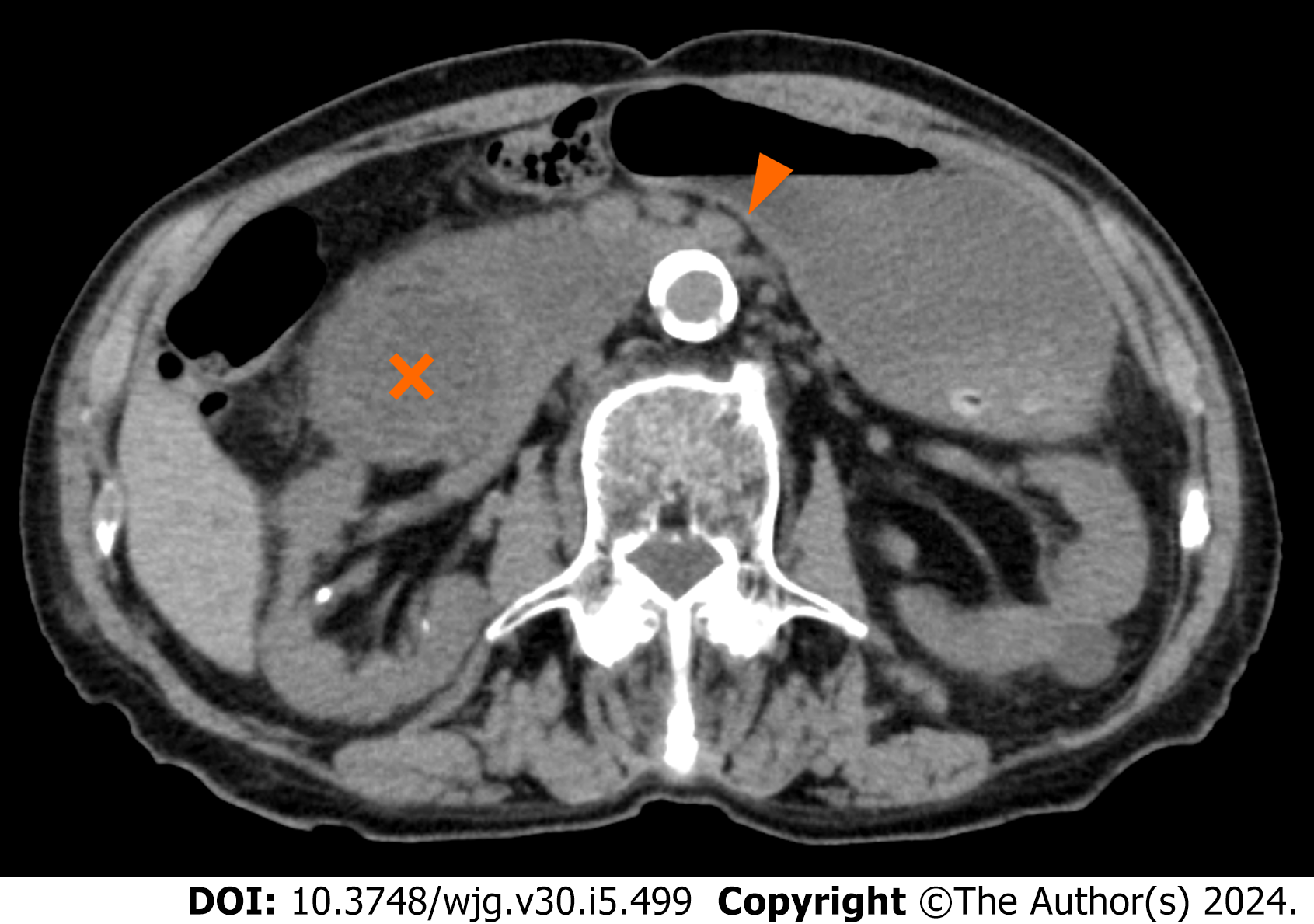
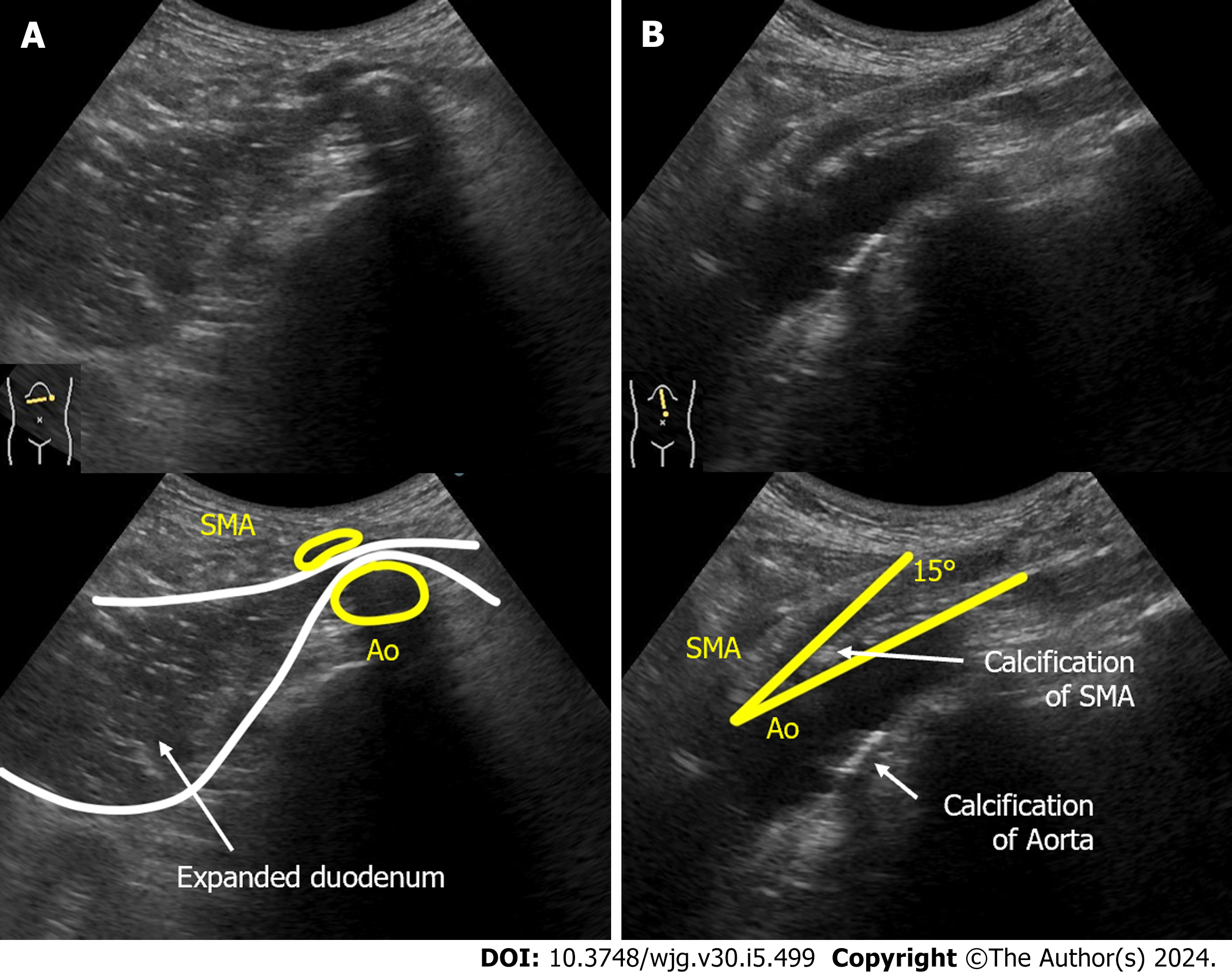
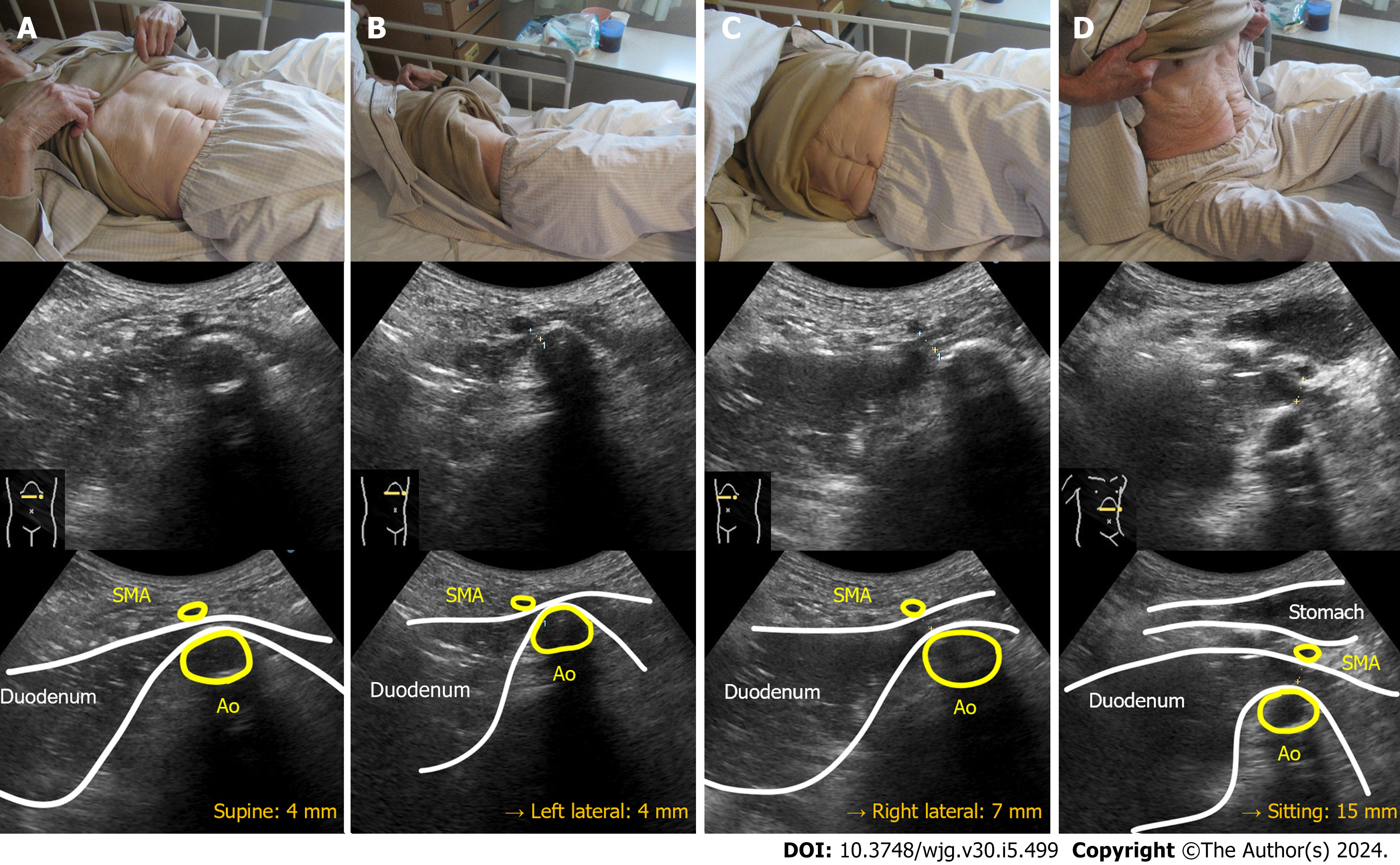
Case 1: Computed tomography (CT) demonstrated compression of the third portion of the duodenum between the SMA-Ao, as well as markedly dilated duodenum and stomach (Figure 1). Arteriosclerosis of the abdominal aorta and SMA was also observed. Abdominal US revealed that, in the supine position, the distance between SMA-Ao was shortened to 4 mm and the angle of SMA-Ao decreased to 15° (Figure 2). Additionally, real-time US observation showed no passage of contents through the SMA-Ao site, along with the to-and-fro sign at the oral side of this location (Video).
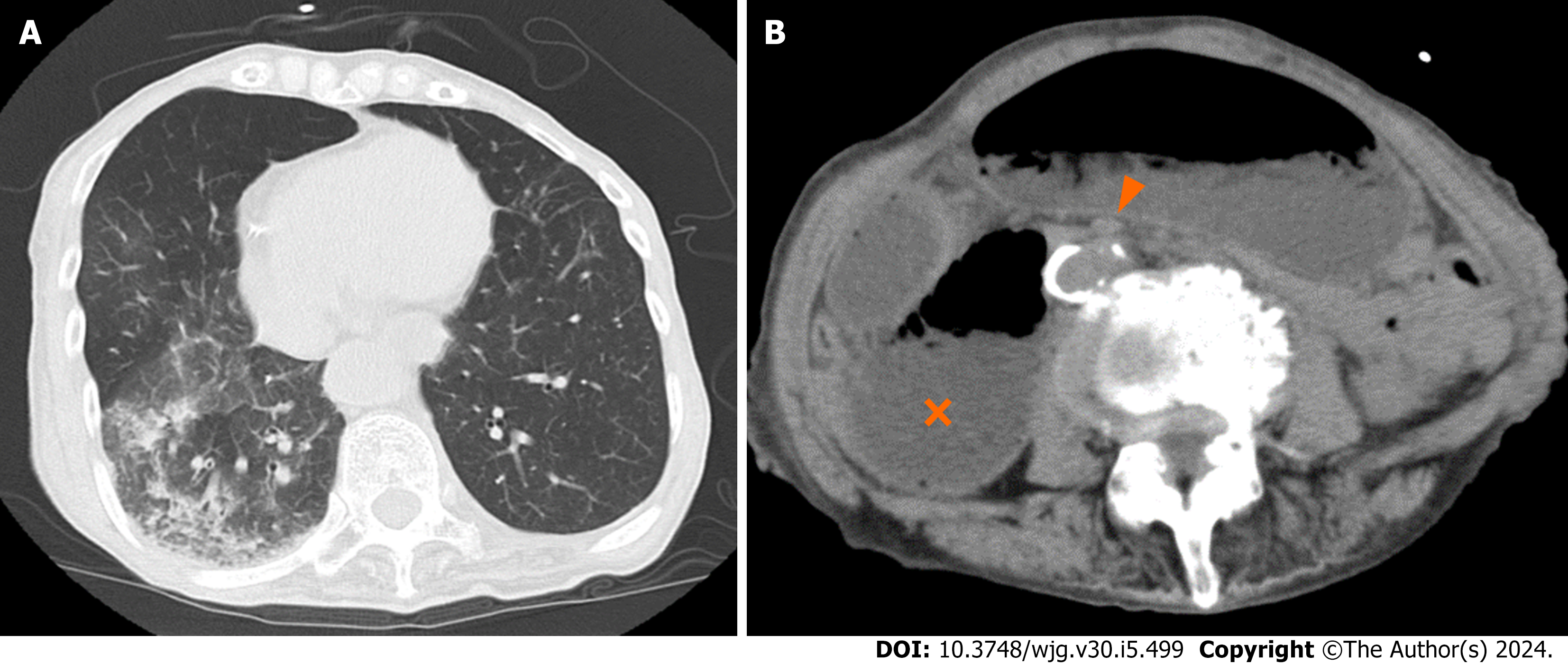
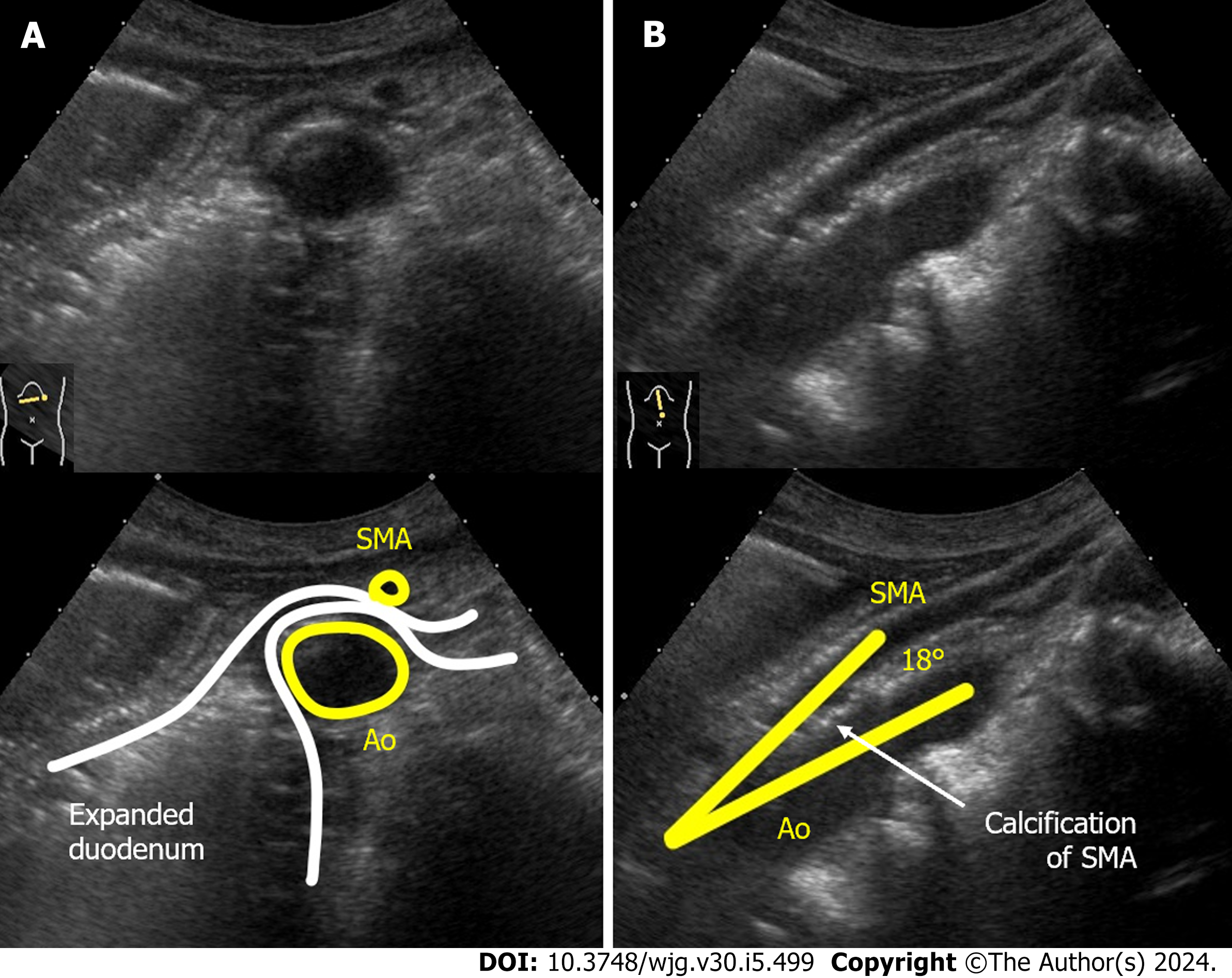
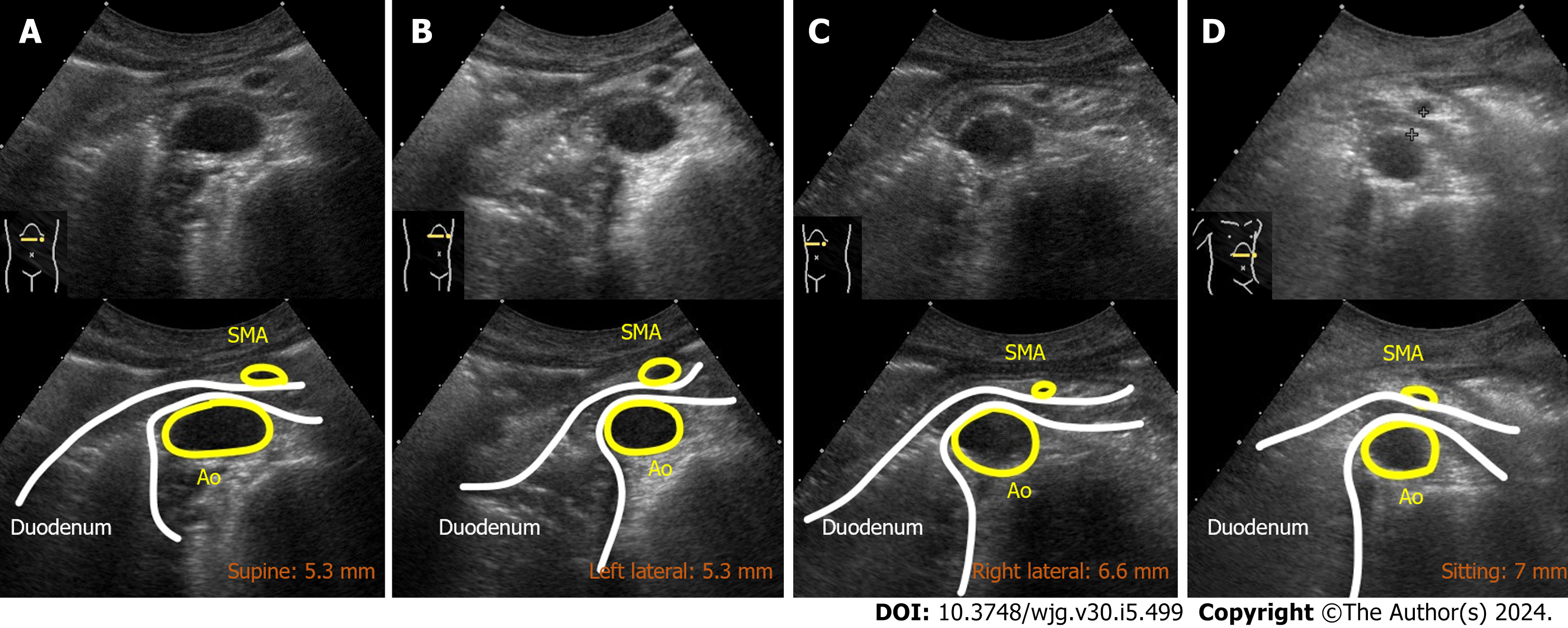
Case 2: CT showed a frosted shadow in the lower lobe of the right lung and compression of the third portion of the duodenum between SMA-Ao, as well as a markedly dilated duodenum and stomach (Figure 3). Arteriosclerosis of the abdominal aorta and SMA was also observed. US demonstrated the SMA-Ao distance was narrowed to 5 mm in the supine position without the passage of duodenal contents (Figure 4A). The angle of SMA-Ao decreased to 18° (Figure 4B).
Case 1: We performed a position change with dynamic observation using US (Figure 5). In the left lateral position, which is traditionally recommended for the patients with SMA syndrome, the SMA-Ao distance was 4 mm (no change compared to that in the supine position). In the right lateral position, US showed that the SMA-Ao distance increased to 7 mm and intestinal gas passed through the compression site of the duodenum. In the sitting position, SMA-Ao distance increased to 15 mm and gas and fluid content passed through the site. Real-time US revealed that pushing by hand on his right upper abdomen enhanced the passage of duodenal contents through the site (Video).
Case 2: Dynamic US with a change in body position revealed dynamic changes in the SMA-Ao distance, measuring 5.3 mm in the supine position, 5.3 mm in the left lateral position, 6.6 mm in the right lateral position, and 7.0 mm in the sitting position (Figure 6).
The final diagnosis was SMA syndrome based on the CT and US findings.
The final diagnosis was SMA syndrome with aspiration pneumonia as an SMA syndrome-related complication based on her medical history and CT and US findings.
On day 1 of hospitalization, fasting and peripheral venous nutrition started. Based on the findings of dynamic US, the patient kept his postprandial position in the right lateral or sitting as much as possible.
On the day 1 of hospitalization, fasting and peripheral venous nutrition started. Based on the findings of dynamic US, she was instructed to keep the optimal body position after a meal. Aspiration pneumonia was treated with intravenous antibiotics for 10 d.
By day 2, all of the patient’s symptoms had vanished, and US confirmed significant improvements in stomach and duodenal dilatation. Consequently, he could eat without recurrence. Upon discharge from the hospital on day 3, he was advised to maintain positions such as sitting or the right lateral position after meals, and also to assume the right-side supine position when using CPAP during sleep. He was also instructed to apply manual pressure (massage) to his right upper abdomen if he experienced any symptoms related to SMA syndrome. There have been no recurrences in the two years since the incident.
On day 7, the patients could start eating without recurrence. On day 32, she was discharged and there was no recurrence in the 12 years since the incident.
SMA syndrome (also known as Wilkie’s syndrome, cast syndrome, mesenteric duodenal obstruction, or aorto-mesenteric compass syndrome) is a rare duodenal obstruction caused by compression between the SMA-Ao[1,21]. Recent reviews indicate a wide age range of patients affected by SMA syndrome, with a notable increase in elderly patients[1,21]. Indeed, the present two patients were very old and required more prompt and careful management to avoid age-related complications, including aspiration pneumonia, functional decline, and malnutrition[22]. Fortunately, dynamic US could determine the optimal position for individualized duodenal passage, thus obviating the need for nasogastric tube placement, a common intervention for decompression and nutritional support in SMA syndrome[1-4]. However, nasogastric tubes can introduce additional complications, such as aspiration pneumonia and intestinal injuries[23,24].
The etiology of SMA syndrome might be different between younger and older patients[21]. In older patients (> 40 years), post-abdominal surgery emerges as the most common etiology, followed by weight loss. In contrast, younger patients (< 40 years) predominantly experience scoliosis-related cases, such as those following spinal fusion surgery and body casting, also accompanied by weight loss. Case 1 had multiple histories of abdominal surgery, suggesting surgical adhesion pulled on the mesentery or restricted the SMA mobility[1]. Furthermore, the presence of atherosclerosis affecting both the SMA and the Ao, as observed in both cases, might further impede SMA mobility[25,26]. Given these restrictions of the SMA mobility, confirming the SMA mobility by dynamic US should be helpful; or, the absence of SMA mobility could suggest early surgical intervention. CT is considered the gold standard for diagnosing SMA syndrome by visualizing duodenal compression by the SMA, along with dilation of the proximal duodenum and stomach[1,27]. Three-dimensional CT has emerged as a valuable tool for visualizing the anatomy of the SMA, Ao, and duodenum[28]. Under normal circumstances, the SMA-Ao angle and distance measure 38–65 and 10–33 mm, respectively[29-31]. The cutoff value was reported as 22 on the SMA-Ao angle and 8 mm distance with 42.8% sensitivity and 100% specificity[30]. While CT undoubtedly offers valuable and objective diagnostic information, it is typically performed in a single body position, usually supine. In contrast, US can potentially be conducted in various postures and provides dynamic assessments of luminal content and vascular movement. As demonstrated in this report, dynamic US is instrumental in identifying the most suitable position for facilitating luminal content passage. Historically, barium X-ray series were used for diagnosis and evaluation of luminal content passage in SMA syndrome[1,32]. However, due to the associated radiation exposure risks, US assessments offer a safer and more effective alternative for managing SMA syndrome. The diagnostic sensitivity of US for SMA syndrome has been validated in comparative studies with CT findings[30]. In addition, because it can be performed at the bedside, it can easily evaluate gastroduodenal dilatation and the distance between the SMA-Ao during follow-up. In light of these advantages, we believe dynamic US represents the most valuable tool for determining the optimal position for each patient with SMA syndrome. The absence of SMA movement, possibly due to calcification at the SMA root or post-abdominal surgery, could be indicative of the need for early surgical intervention[1]. While US findings may potentially be influenced by operator bias and interobserver variation, dynamic observation places greater emphasis on subjective focus compared to static images. To the best of our knowledge, this report constitutes the first documentation of dynamic US in SMA syndrome, complete with detailed images and a video. We anticipate that this report will be valuable for US practitioners aiming to enhance their understanding of SMA syndrome diagnosis.
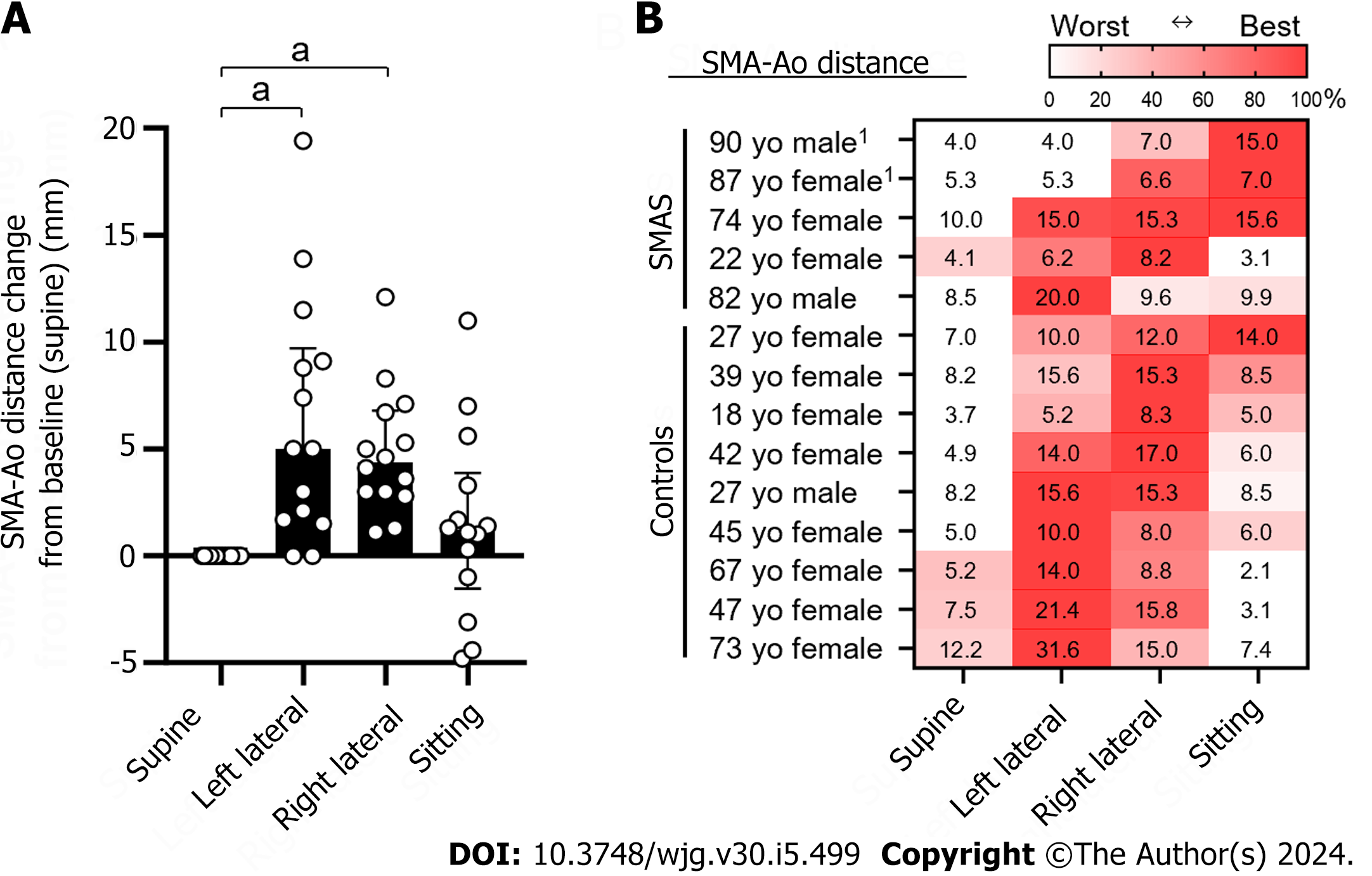
The treatment for SMA syndrome is initiated by conservative methods, such as gastric and duodenal decompression by postural change and/or nasogastric tube suction[22,33]. If the conservative treatment fails, surgery may be necessary[1,34]. Although it is believed that positioning the patient in the left lateral position is effective in the treatment of SMA syndrome, there is little evidence[13,16]. The optimal body position for each patient may vary because recent studies found a variation in the SMA position and movement[14,15,17]. Case 1 in our report demonstrated better content passage in the right lateral position than the left, corroborating the findings of Khan et al[15]. Miyata et al[17] reported a variation in position of SMA demonstrating that major position was the right side along with the aorta[17]. No study has reported the optimal position in SMA syndrome[1]. As such, we conducted an evaluation of the optimal body position in 14 individuals, including our two SMA syndrome cases and nine healthy controls, using abdominal US (Figure 7). In cases where duodenal detection proved challenging, subjects ingested 200 mL of water, modifying the drinking US test[35]. While the left lateral position, which is generally thought to be an optimal position, was significantly effective (long distance of SMA-Ao) as expected, the right lateral position was also significantly effective (Figure 7A). The best position varies from case to case: the left lateral position was effective in some cases while the right lateral recumbent position and the sitting position were more effective in other cases (Figure 7B). Further prospective cohort studies are warranted to explore the effectiveness of dynamic US in identifying ideal positions for SMA syndrome patients. Although recent surgical interventions for SMA syndrome have demonstrated safety and efficacy[1,36], surgery and anesthesia inherently pose risks to elderly patients, particularly those with pulmonary risk factors, as demonstrated by our cases[37]. Dynamic US offers a promising avenue to enhance the effectiveness of non-surgical treatments and prevent unnecessary surgical procedures.
We presented two cases of SMA syndrome in elderly patients in which US proved invaluable for determining optimal positioning. Given the variability of optimal body positions in SMA syndrome among patients, dynamic assessment of the optimal body position via bedside positioning using dynamic US emerged as a minimally invasive and effective option.
We thank Keiko Masuzaki and Yuriko Adachi for collecting references and Maki Watanabe for collaborating with the ethics committee.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Japanese Society of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Govindarajan KK, India S-Editor: Li L L-Editor: Kerr C P-Editor: Cai YX
| 1. | Oka A, Awoniyi M, Hasegawa N, Yoshida Y, Tobita H, Ishimura N, Ishihara S. Superior mesenteric artery syndrome: Diagnosis and management. World J Clin Cases. 2023;11:3369-3384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 40] [Article Influence: 20.0] [Reference Citation Analysis (9)] |
| 2. | Wilkie DPD. Chronic duodenal ileus. Am J Med Sci. 1927;173:643-648. [RCA] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 116] [Article Influence: 1.2] [Reference Citation Analysis (4)] |
| 3. | Hines JR, Gore RM, Ballantyne GH. Superior mesenteric artery syndrome. Diagnostic criteria and therapeutic approaches. Am J Surg. 1984;148:630-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 132] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Evarts CM. The cast syndrome. Report of a case after spinal fusion for scoliosis. Clin Orthop Relat Res. 1971;75:164-166. [PubMed] [DOI] [Full Text] |
| 5. | Murakami C, Irie W, Sasaki C, Nakamaru N, Sakamoto M, Nagato J, Satoh F. Extensive gastric necrosis secondary to acute gastric dilatation: A case report. Leg Med (Tokyo). 2019;36:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Mohammad Kazmin NE, Kamaruzaman L, Wong Z, Fong VK, Mohd R, Mustafar R. Acute Kidney Injury Caused by Superior Mesenteric Artery Syndrome. Case Rep Nephrol. 2020;2020:8364176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Petrosyan M, Estrada JJ, Giuliani S, Williams M, Rosen H, Mason RJ. Gastric perforation and pancreatitis manifesting after an inadvertent nissen fundoplication in a patient with superior mesenteric artery syndrome. Case Rep Med. 2009;2009:426162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Thieme ET, Postmus R. Superior mesenteric artery syndrome. Ann Surg. 1961;154:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Shajani-Yi Z, Lee HK, Cervinski MA. Hyponatremia, Hypokalemia, Hypochloremia, and Other Abnormalities. Clin Chem. 2016;62:898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Elbadaway MH. Chronic superior mesenteric artery syndrome in anorexia nervosa. Br J Psychiatry. 1992;160:552-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Mandarry MT, Zhao L, Zhang C, Wei ZQ. A comprehensive review of superior mesenteric artery syndrome. Eur Surg. 2010;42:229-236. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Kawanishi K, Shojima K, Nishimoto M, Abe H, Kakimoto T, Yasuda Y, Hara T, Kato J. Superior Mesenteric Artery Syndrome May Be Overlooked in Women with Functional Dyspepsia. Intern Med. 2017;56:2549-2554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Evarts CM, Winter RB, Hall JE. Vascular compression of the duodenum associated with the treatment of scoliosis. Review of the literature and report of eighteen cases. J Bone Joint Surg Am. 1971;53:431-44 passim. [PubMed] [DOI] [Full Text] |
| 14. | Dounas GD, Cundy TP, Smith ML, Gent R, Antoniou G, Sutherland LM, Cundy PJ. The coronal aorto-mesenteric orientation theory for post-operative nausea and vomiting following scoliosis surgery in children: a pilot study. ANZ J Surg. 2021;91:174-178. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Khan H, Al-Jabbari E, Shroff N, Barghash M, Shestopalov A, Bhargava P. Coexistence of superior mesenteric artery syndrome and nutcracker phenomenon. Radiol Case Rep. 2022;17:1927-1930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Neri S, Signorelli SS, Mondati E, Pulvirenti D, Campanile E, Di Pino L, Scuderi M, Giustolisi N, Di Prima P, Mauceri B, Abate G, Cilio D, Misseri M, Scuderi R. Ultrasound imaging in diagnosis of superior mesenteric artery syndrome. J Intern Med. 2005;257:346-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 113] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Miyata J, Eshak ES, Yoshioka T, Iso H. Movement of the superior mesenteric artery in patients with superior mesenteric artery syndrome: A case-reference study. Clin Anat. 2022;35:891-898. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Choi SH, Pfalzer FA Jr. Superior mesenteric artery syndrome. N Y State J Med. 1976;76:986-988. [PubMed] |
| 19. | Wu WT, Lin CY, Shu YC, Chen LR, Özçakar L, Chang KV. Subacromial Motion Metrics in Painful Shoulder Impingement: A Dynamic Quantitative Ultrasonography Analysis. Arch Phys Med Rehabil. 2023;104:260-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 20. | Shu YC, Lo YC, Chiu HC, Chen LR, Lin CY, Wu WT, Özçakar L, Chang KV. Deep learning algorithm for predicting subacromial motion trajectory: Dynamic shoulder ultrasound analysis. Ultrasonics. 2023;134:107057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 21. | Oka A, Hasegawa N, Yoshida Y, Tobita H, Awoniyi M, Ishimura N, Ishihara S. Ep129 superior mesenteric artery syndrome -a systematic review of 2,453 cases in the literature. Gastroenterology. 2023;164:S-1215. [DOI] [Full Text] |
| 22. | Merrett ND, Wilson RB, Cosman P, Biankin AV. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg. 2009;13:287-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 202] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 23. | McCann C, Cullis PS, McCabe AJ, Munro FD. Major complications of jejunal feeding in children. J Pediatr Surg. 2019;54:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Miura T, Nakamura J, Yamada S, Miura T, Yanagi M, Tani Y, Nishihara M, Takahashi T. A Fatal Aortoesophageal Fistula Caused by Critical Combination of Double Aortic Arch and Nasogastric Tube Insertion for Superior Mesenteric Artery Syndrome. Case Rep Gastroenterol. 2010;4:198-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Beita AKV, Whayne TF. The Superior Mesenteric Artery: From Syndrome in the Young to Vascular Atherosclerosis in the Old. Cardiovasc Hematol Agents Med Chem. 2019;17:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Kitaura K, Harima K. Superior mesenteric artery syndrome with vascular calcification in a maintenance hemodialysis patient. Clin Nephrol. 2009;71:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Lamba R, Tanner DT, Sekhon S, McGahan JP, Corwin MT, Lall CG. Multidetector CT of vascular compression syndromes in the abdomen and pelvis. Radiographics. 2014;34:93-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 28. | Raman SP, Neyman EG, Horton KM, Eckhauser FE, Fishman EK. Superior mesenteric artery syndrome: spectrum of CT findings with multiplanar reconstructions and 3-D imaging. Abdom Imaging. 2012;37:1079-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Hearn JB. Duodenal ileus; with reference to superior mesenteric artery compression. Md State Med J. 1965;14:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Unal B, Aktaş A, Kemal G, Bilgili Y, Güliter S, Daphan C, Aydinuraz K. Superior mesenteric artery syndrome: CT and ultrasonography findings. Diagn Interv Radiol. 2005;11:90-95. [PubMed] |
| 31. | Le D, Stirparo JJ, Magdaleno TF, Paulson CL, Roth KR. Point-of-care ultrasound findings in the diagnosis and management of Superior Mesenteric Artery (SMA) syndrome. Am J Emerg Med. 2022;55:233.e1-233.e4. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 32. | Hutchinson DT, Bassett GS. Superior mesenteric artery syndrome in pediatric orthopedic patients. Clin Orthop Relat Res. 1990;250-257. [PubMed] |
| 33. | Lee TH, Lee JS, Jo Y, Park KS, Cheon JH, Kim YS, Jang JY, Kang YW. Superior mesenteric artery syndrome: where do we stand today? J Gastrointest Surg. 2012;16:2203-2211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 34. | Shin MS, Kim JY. Optimal duration of medical treatment in superior mesenteric artery syndrome in children. J Korean Med Sci. 2013;28:1220-1225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Kato M, Nishida U, Nishida M, Hata T, Asaka R, Haneda M, Yamamoto K, Imai A, Yoshida T, Ono S, Shimizu Y, Asaka M. Pathophysiological classification of functional dyspepsia using a novel drinking-ultrasonography test. Digestion. 2010;82:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Pottorf BJ, Husain FA, Hollis HW Jr, Lin E. Laparoscopic management of duodenal obstruction resulting from superior mesenteric artery syndrome. JAMA Surg. 2014;149:1319-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 37. | Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 662] [Cited by in RCA: 749] [Article Influence: 41.6] [Reference Citation Analysis (0)] |