Published online Feb 7, 2024. doi: 10.3748/wjg.v30.i5.440
Peer-review started: October 3, 2023
First decision: December 4, 2023
Revised: December 15, 2023
Accepted: January 11, 2024
Article in press: January 11, 2024
Published online: February 7, 2024
Processing time: 119 Days and 14.5 Hours
According to practice guidelines, endoscopic band ligation (EBL) and endoscopic tissue adhesive injection (TAI) are recommended for treating bleeding from esophagogastric varices. However, EBL and TAI are known to cause serious complications, such as hemorrhage from dislodged ligature rings caused by EBL and hemorrhage from operation-related ulcers resulting from TAI. However, the optimal therapy for mild to moderate type 1 gastric variceal hemorrhage (GOV1) has not been determined. Therefore, the aim of this study was to discover an individualized treatment for mild to moderate GOV1.
To compare the efficacy, safety and costs of EBL and TAI for the treatment of mild and moderate GOV1.
A clinical analysis of the data retrieved from patients with mild or moderate GOV1 gastric varices who were treated under endoscopy was also conducted. Patients were allocated to an EBL group or an endoscopic TAI group. The differences in the incidence of varicose relief, operative time, operation success rate, mortality rate within 6 wk, rebleeding rate, 6-wk operation-related ulcer healing rate, complication rate and average operation cost were compared between the two groups of patients.
The total effective rate of the two treatments was similar, but the efficacy of EBL (66.7%) was markedly better than that of TAI (39.2%) (P < 0.05). The operation success rate in both groups was 100%, and the 6-wk mortality rate in both groups was 0%. The average operative time (26 min) in the EBL group was significantly shorter than that in the TAI group (46 min) (P < 0.01). The rate of delayed postoperative rebleeding in the EBL group was significantly lower than that in the TAI group (11.8% vs 45.1%) (P < 0.01). At 6 wk after the operation, the healing rate of operation-related ulcers in the EBL group was 80.4%, which was significantly greater than that in the TAI group (35.3%) (P < 0.01). The incidence of postoperative complications in the two groups was similar. The average cost and other related economic factors were greater for the EBL than for the TAI (P < 0.01).
For mild to moderate GOV1, patients with EBL had a greater one-time varix eradication rate, a greater 6-wk operation-related ulcer healing rate, a lower delayed rebleeding rate and a lower cost than patients with TAI.
Core Tip: Endoscopic band ligation (EBL) and endoscopic tissue adhesive injection for the treatment of type 1 gastric variceal hemorrhage (GOV1) are often associated with various complications, which we believe are due to the lack of individualized treatment. Different treatment methods should be used for different degrees of varicose veins. Therefore, this study was based on mild to moderate GOV1 and explored individualized treatment. Ultimately, the use of EBL for mild to moderate GOV1 can achieve better outcomes and reduce both rebleeding rates and treatment costs.
-
Citation: Deng Y, Jiang Y, Jiang T, Chen L, Mou HJ, Tuo BG, Shi GQ. Evaluation of the efficacy and safety of endoscopic band ligation in the treatment of bleeding from mild to moderate gastric varices
type 1 . World J Gastroenterol 2024; 30(5): 440-449 - URL: https://www.wjgnet.com/1007-9327/full/v30/i5/440.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i5.440
Esophageal and gastric variceal bleeding (EGVB) is a common cause of death worldwide in patients with cirrhosis, a liver-related disease, with an incidence of approximately 5%-15%. The 6-wk mortality rate can reach 20%, and rebleeding rates can reach 60%, placing an enormous burden on the global economy[1,2]. The main endoscopic treatments for EGVB include endoscopic band ligation (EBL), endoscopic tissue adhesive injection (TAI) and endoscopic injection sclerotherapy (EIS)[3]. However, during the treatment of type 1 gastric variceal hemorrhage (GOV1), EBL, EIS and TAI can cause serious complications, such as hemorrhage from dislodged ligature rings caused by EBL and hemorrhage from operation-related ulcers resulting from TAI, which are major problems for patients and endoscopists. It is important to choose the appropriate treatment modality according to the type, morphology and severity of varicose veins to further improve the treatment efficacy and minimize the incidence of associated complications. However, there are no detailed recommendations in the guidelines or published literature, especially for GOV1. Currently, there is no consensus on the recommended endoscopic treatment for GOV1. Currently, most endoscopists use a “modified sandwich method” (lauromacrogol-tissue adhesive-lauromacrogol)[4], which is highly effective but has a high incidence of rebleeding in patients with mild-to-moderate GOV1[5,6]. Therefore, we stratified the risk factors for mild-to-moderate GOV1 and observed the efficacy, safety, and costs of EBL and TAI to provide more precise and individualized treatment.
Patients with mild-to-moderate GOV1 disease who visited Zunyi Medical University and Yinjiang Autonomous County People’s Hospital between January 2017 and December 2022 were selected. The inclusion criteria were as follows: (1) Patients diagnosed with cirrhotic decompensation with GOV1 based on their past medical history, clinical presentation and ancillary investigations[7]; (2) Patients who underwent primary or secondary prevention measures; (3) Patients who completed the 6-wk follow-up after endoscopic gastroscopy treatment; (4) Patients with mild-to-moderate GOV1 with gastric varices in the shape of a stripe and a diameter ≤ 10 mm; (5) Patients with no contraindications to endoscopy; (6) Those who had not undergone surgery or transjugular intrahepatic portosystemic shunt for portal hypertension; and (7) Patients and their families who were willing to cooperate with the treatment and signed a treatment consent form. The exclusion criteria were as follows: (1) Previous endoscopic treatment for gastric varices; (2) Lost to follow-up; (3) Severe comorbidities involving other organ systems; (4) Combined malignant tumors; and (5) Combined hepatic encephalopathies, disorders of consciousness, or other psychiatric-psychological disorders. The study protocol conformed to the ethical guidelines of the 1975 Helsinki Declaration and was approved by the Institutional Review Board.
Patient data, including age, sex, and disease etiology (chronic hepatitis B, chronic hepatitis C, alcoholic liver disease, autoimmune hepatitis, hepatitis B combined with alcohol consumption and others), were collected during hospitalization. The results of the radiographic examinations [diameter of gastric varices (mm) and diameter of portal vein (mm)] and Child-Pugh classification were collected at enrollment.
The classification of the gastric variceal size was similar to that of esophageal varices. Esophageal varices[8] were classified as mild gastric varices (G1): Rectilinear or slightly tortuous varices < 3 mm in diameter; moderate gastric varices (G2): Serpentine tortuous bulging varices 3-10 mm in diameter; and severe gastric varices (G3): Beaded, nodular or verrucous varices > 10 mm in diameter.
The following instruments were used: An electronic gastroscope (Olympus GIF-260), a disposable endoscopic injection needle (Poco, 25G), a multiband variceal ligator (Poco 7-ring ligature), N-butyl-2-cyanoacrylate (0.5 mL/pc; Beijing Fuaile Technology Development Co., Ltd., China), and lauromacrogol (10 mL/pc; Shaanxi Tianyu Pharmaceutical Co., Ltd., China).
Tests, including routine blood, coagulation, and biochemistry tests, as well as electrocardiogram and portal vein imaging, were completed on admission. The patient’s general condition was assessed, drugs were administered to suppress gastric acid and lower the portal pressure, and painless endoscopic treatment was administered once the patient’s vital signs had stabilized. All the procedures were performed by our team of doctors experienced in EGVB treatment.
In the EBL group, the lateral vein of the lesser curvature was ligated from the cardia toward the fundus of the stomach via a ligature via reverse endoscopy. TAI group: TAI treatment was performed using a “modified sandwich method” (lauromacrogol-tissue adhesive-lauromacrogol).
Both groups were treated for esophageal varices after the completion of GV treatment. The patients in both groups received proton pump inhibitors and vasoconstrictors. The TAI group received prophylactic antibiotics. The patients in both groups were followed up for at 6 wk after gastroscopy to judge the effectiveness of the varices eradication and to assess whether continuation of treatment was necessary. Patients in both groups were followed up at 3 months, 6 months and 1 year postoperatively at regular intervals. Depending on the effect of varices, the choice was made whether to repeat endoscopic treatment.
GOV1 efficacy is divided into three levels[9,10]: (1) Ineffective: No improvement in the varicose veins; (2) Effective: The condition of the varicose veins improved, indicated by less than 50% shrinkage; and (3) Markedly effective: The massed or nodular veins had changed to cords, had shrunk by more than 50% or had disappeared completely. Total effective rate = (number of effective cases + number of effective cases)/total number of cases × 100%.
Operation success was defined as the completion of EBL or TAI without uncontrollable bleeding intraoperatively or resulting in patient death. Operative time: The time from the start of the operation to the end of the operation, including the common time for treatment of gastric varices and esophageal varices. Six-week mortality[11]: Death within 6 wk after surgery.
Rebleeding: The reappearance of signs of upper gastrointestinal bleeding, such as vomiting blood, black stools, decreasing hemoglobin levels and shock, that recurs after the first bleeding has been controlled, with early rebleeding characterized as active bleeding within 6 wk after the bleeding had been controlled and late rebleeding characterized as active bleeding 6 wk after the bleeding had been controlled.
Six-week operation-related ulcer healing rate: Follow-up gastroscopy was performed 6 wk after surgery to observe the healing of the ulcer after EBL or TAI. The ulcer was considered healed if a fibrous scar was formed; otherwise, it was not healed. Adverse events included abdominal pain, infection, ectopic embolism, and perforation.
The following were summarized: The average number of hospitalizations, average length of hospitalizations, average total cost of hospitalization, average number of operations and average operation cost.
Microsoft Excel 2016 and SPSS 26.0 were used for statistical analysis in this study. Normally distributed data are expressed as the mean ± SD, quantitative data with a skewed distribution are described by the median, and count data are expressed as the rate. A t-test was used to compare differences between the groups; nonnormally distributed measures and rank data were compared using the Mann-Whitney U test or Wilcoxon rank sum test, and count data were compared using the χ2 test and Fisher’s test. The test level was P < 0.05.
According to the inclusion and exclusion criteria, a total of 151 patients were included, including 57 patients in the EBL group and 94 patients in the TAI group. The control variables used were sex, age, etiology, Child-Pugh classification, gastric variceal diameter, and portal vein diameter, and propensity score matching was performed using SPSS software. Then, 51 pairs of 102 patients were matched to the EBL group and the TAI group. The sex, age, etiology, Child-Pugh classification, gastric variceal diameter, and portal vein diameter of the two groups of patients were compared after matching. The differences between the two groups were not statistically significant (P > 0.05) (Table 1).
| EBL group (n = 50) | TAI group (n = 50) | χ2/t/U | P value | |
| Sex, n (%) | ||||
| Male | 45 (88.2) | 43 (84.3) | / | 0.4871 |
| Female | 6 (11.8) | 8 (15.7) | ||
| Age (yr, mean ± SD) | 52.78 ± 8.50 | 52.92 ± 9.65 | 0.076 | 0.9392 |
| Causes of disease, n (%) | 3.744 | 0.6301 | ||
| Hepatitis B liver cirrhosis | 28 (54.9) | 26 (51.0) | ||
| alcoholic cirrhosis | 11 (21.6) | 13 (25.5) | ||
| Hepatitis C cirrhosis | 6 (11.7) | 2 (3.9) | ||
| Autoimmune liver cirrhosis | 1 (2.0) | 3 (5.9) | ||
| Hepatitis B liver cirrhosis with alcoholic cirrhosis | 4 (7.8) | 6 (11.7) | ||
| Other cause | 1 (2.0) | 1 (2.0) | ||
| Child-Pugh classification, n (%) | -0.377 | 0.7063 | ||
| A | 11 (21.6) | 10 (19.6) | ||
| B | 37 (72.6) | 37 (72.6) | ||
| C | 3 (5.8) | 4 (7.8) | ||
| Diameter of gastric varices (mm) | 15.0 | 14.0 | -1.459 | 0.1353 |
| Diameter of the portal vein (mm) | 8.0 | 9.0 | -1.280 | 0.2003 |
Gastroscopy was performed again 6 wk after the operation to observe if there was relief of the gastric varices after endoscopic treatment in the two groups. The difference in the total effective rate between the EBL group (96.1%) and the TAI group (94.1%) was not statistically significant (P > 0.05). However, the percentage of patients in the EBL group (66.7%) was significantly greater than that in the TAI group (39.2%) (χ2 = 7.713, P < 0.05) (Table 2).
Comparison of the operative time, operation success rate and 6-wk mortality: Both groups of patients successfully completed endoscopic treatment, and there was no intraoperative bleeding that was difficult to control or that led to patient death. The operation success rate of the two groups was 100%. Additionally, there were no deaths for any reason in the two groups of patients 6 wk after the operation. The average operative time in the EBL group (26 min) was significantly shorter than that in the TAI group (46 min) (P < 0.01) (Table 3).
| Operative time (min) | Operative success rate, n (%) | Week mortality, n (%) | |
| EBL group | 26 | 51 (100) | 0 (0) |
| TAI group | 46 | 51 (100) | 0 (0) |
| Z | -8.721 | / | / |
| P value | < 0.0011 | / | / |
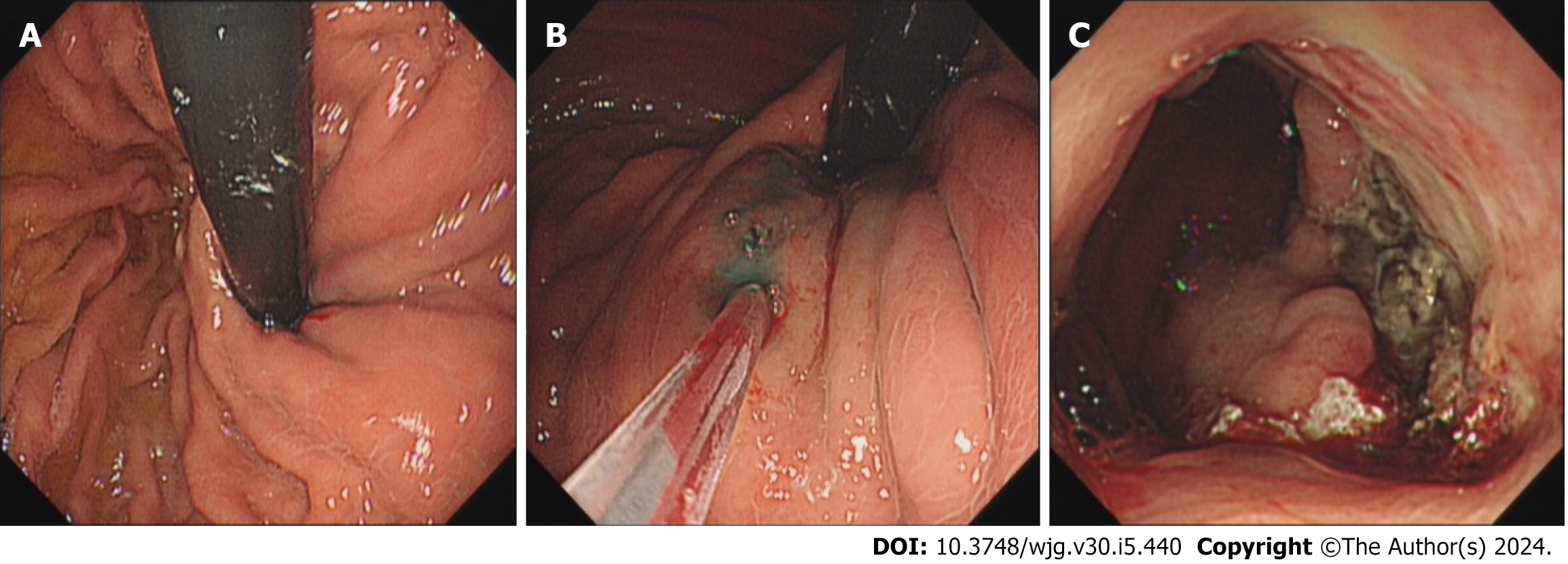
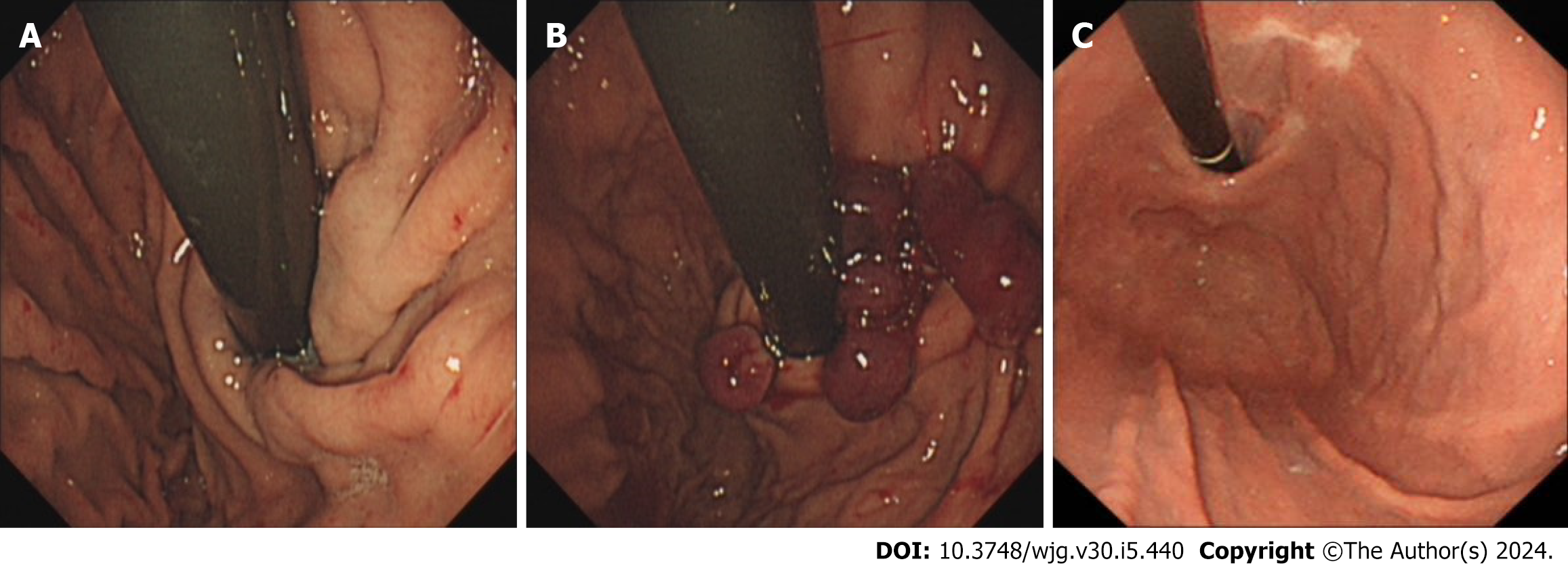
Comparison of the 6-wk operation-related ulcer healing rate: After surgery, gastroscopy revealed that the healing rate of the ulcers that developed after dislodgement of the ligature ring in the EBL group reached 80.4%, which was significantly greater than the healing rate of the glue-draining ulcers in the TAI group (35.3%). The difference between the two groups was statistically significant (P < 0.01) (Table 4). Many TAI patients presented with glue-draining ulcers and bleeding (Figure 1); however, most EBL patients had healed ulcers (Figure 2).
| Healed | Non-healed | |
| EBL group | 41 (80.4) | 10 (19.6) |
| TAI group | 18 (35.3) | 33 (64.7) |
| χ2 | 21.268 | |
| P value | < 0.001 | |
Comparison of the postoperative rebleeding rates: Patients in both groups were followed up for 1 year after successful endoscopic treatment to focus on rebleeding. The rate of early postoperative rebleeding (within 6 wk after surgery) was slightly lower in the EBL group (7.8%) than in the TAI group (13.7%), but the difference was not statistically significant (P > 0.05). The rate of late postoperative rebleeding (from 6 wk postoperatively to 1 year) was significantly lower in the EBL group (11.8%) than in the TAI group (45.1%) (P < 0.01) (Table 5).
| Early rebleeding rate | Delayed rebleeding rate | |
| EBL group | 4 (7.8) | 6 (11.8) |
| TAI group | 7 (13.7) | 23 (45.1) |
| χ2 | 0.917 | 13.924 |
| P value | 0.338 | < 0.001 |
Comparison of adverse events: The rates of postoperative abdominal pain and infection were similar between the two groups, but the difference was not statistically significant (P > 0.05). No heterotopic embolism or perforation occurred in either group (Table 6).
Follow-up economic indices such as the number of hospitalizations, the total number of days of hospitalization, the total cost of hospitalization, the number of surgeries, the cost of surgical materials and other economic indicators were significantly lower in the two groups one year after the operation in the EBL group than in the TAI group (P < 0.01) (Table 7).
| Average number of hospitalizations (No.) | Average length of hospitalizations (d) | Average total cost of hospitalization (Yuan) | Average number of operations (No.) | Average operation cost (Yuan) | |
| EBL group | 2.00 | 13.00 | 32128.60 | 2.00 | 1680.00 |
| TAI group | 3.00 | 19.00 | 69380.75 | 3.00 | 6548.80 |
| Z | 3.596 | 3.894 | 6.134 | 3.631 | 8.855 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
In liver cirrhosis, increased intrahepatic vascular resistance to portal flow increases the portal pressure and leads to portal hypertension. Once portal hypertension develops, it influences extrahepatic vascular beds in the splanchnic and systemic circulations, causing collateral vessel formation and arterial vasodilation. This process helps to increase blood flow into the portal vein, which exacerbates portal hypertension and eventually aids in the development of hyperdynamic circulatory syndrome. As a result, esophageal varices or ascites develop. Gastric varices are present in 5%-33% of patients with portal hypertension. Gastric varices usually bleed more severely than ruptured esophageal varices, and the mortality rate can reach 45%[1].
Based on Sarin’s classification, gastric varices can be classified as GOV1, GOV2, isolated gastric varices type 1 (IGV1) or IGV2. GOV1 is the most common type of gastric varices, accounting for 75%[12] of all gastric varices. GOV2 and IGV1 tend to have varices that have thicker diameters and are continuously exposed to gastric acid and pepsin; thus, TAI is recognized as the treatment of choice, as it has high success rates in hemostasis and one-time varicose vein eradication[13]. GOV1 is characterized by the presence of gastric varices that appear with esophageal varices and extend 2-5 cm below the gastroesophageal junction. The shape of these lesions is similar to that of esophageal varices, and they may appear tortuous, nodular or tumorous in shape. There is no uniform standard for the endoscopic treatment of GOV1. Currently, most endoscopists choose endoscopic TAI, while a few endoscopists use EBL. Recently, a few studies had analyzed and compared the clinical application of EBL and TAI for removing GOV1, but the conclusions have not been consistent. Several studies have shown that there is no statistically significant difference between EBL and TAI in the treatment of GOV1 in terms of acute hemostasis, variceal elimination or risk of rebleeding, but the complication rate of EBL is lower[14]. Several studies have shown that EBL is superior to TAI in terms of reducing the incidence of late rebleeding in patients with acute GOV1[15]. It has also been suggested that TAI is more favorable than EBL because of its significantly reduced rebleeding rate, significantly increased survival time, high hemostasis and survival rate[16-19]. We believe that the inconsistency of the results of the current study compared to other studies may be related to the fact that none of the other studies stratified the risks of the procedures for the study population, and none of them analyzed indicators such as diameter, morphology, or severity of gastric varices. Moreover, all of their studies involved emergency bleeding rather than primary or secondary bleeding prevention. Therefore, these studies failed to individualize the choice of regimen, which led to different results.
Therefore, we stratified the risk of GOV1 and developed different treatment programs. For high-tension, nodular or tumorous varicose veins with a diameter greater than 1 cm (severe), precise puncture and precise endoscopic injection are feasible; therefore, TAI can achieve very good outcomes. For this kind of varicose vein, if EBL is chosen, incomplete ligation and insufficient vessel occlusion are likely to occur. In contrast, the risk of rebleeding is high[20]. Therefore, it is appropriate to choose the TAI for GOV1. However, for striated varicose veins (mild to moderate) with a diameter less than 1 cm, precise puncture and precise endoscopic injection are difficult because of the low vascular tone. Therefore, rebleeding is characterized by bleeding from a draining ulcer that can develop as a result of TAI[21,22]. On the basis of our clinical findings, EBLs prevent bleeding from glue-draining ulcers. Therefore, our retrospective study compared endoscopic reverse body ligation and TAI for the treatment of mild to moderate GOV1. Our study included patients who were subjected to secondary or primary prophylaxis and did not include only emergency patients.
EBL is a procedure in which the gastroscope enters the fundus of the stomach and then reverses the body to fully expose the fundus, and a ligature ring is used to ligate the varicose vein inside the clear cap at the front of the inhalation endoscope so that tissue necrosis occurs at the site of the ligature and a thrombus forms to block the varicose vein within 24 to 48 h. The ligature ring eventually detaches and leaves an ulcer, which heals and leaves a fibrous scar, creating a lasting interruption of the blood flow in the vein[23].
Therefore, this study compared the efficacy, safety and cost of endoscopic reverse body ligation and TAI for the treatment of mild and moderate GOV1 gastric varices: (1) Efficacy: The total effective rates of EBL and TAI were similar, but the effective rate of EBL was better than that of TAI. These findings suggest that both EBL and TAI have similar overall efficacy rates, but EBL has a greater rate of effective one-time varicose vein eradication than does TAI. Because of the small diameter of the gastric varices selected for this study and the choice of intensive multiple ring ligation during treatment, the varices could be fully occluded at one time, and the risk of recurrence of residual varices could be reduced; (2) Safety: The data of this study showed that the patients in both the EBL group and the TAI group successfully completed the endoscopic surgery, and none of them had uncontrollable intraoperative bleeding or died. Both EBL and TAI are feasible, safe and effective for the treatment of mild to moderate GOV1. However, the average operative time of EBL was significantly shorter than that of TAI. This finding indicates that performing EBL is easier for endoscopists. EBL can fully expose the gastric fundus to expand the surgical window more openly and clearly locate the varicose vein, which is favorable for surgical operation. Complete ligation under direct vision can be achieved due to the clear visibility of the surgical field, ensuring a safe operation. The early postoperative rebleeding rate in the EBL group was slightly lower than that in the TAI group. The rate of late rebleeding in the postoperative period after surgery for EBL was significantly lower than that in the postoperative period after TAI. A 6-wk postoperative review of patients treated with gastroscopy showed that the healing rate of ulcers after dislodged ligature rings in the EBL group was significantly greater than the glue-draining ulcers in the TAI group. This is because shallow ulcers tend to form after detachment of the ligature ring, and most of the ulcers heal into a fibrous scar within 6 wk. However, after injection of the tissue adhesive, due to poor precision, the tissue glue tends to leak into the submucosa, which results in the formation of a long-lasting and deep glue-discharging ulcer that tends to remain unhealed and bleeds repeatedly even after 6 wk. This is the reason why the rate of delayed rebleeding after surgery was significantly lower in the EBL group than in the TAI group. The rate of postoperative complications was similar between the two groups, which shows that there is no increased risk of treatment with EBL; and (3) Cost: The number of hospitalizations, total number of days of hospitalization, total cost of hospitalization, number of surgeries, and cost of surgical materials in the EBL group were lower than those in the TAI group. The cost of consumables used in the EBL group was lower than that used in the TAI group because the EBL group had higher rates of effective one-time varicose vein eradication and procedure-related ulcer healing at 6 wk postoperatively but a lower rebleeding rate. Therefore, this approach has a significantly lower health care cost and a considerably lighter financial burden on the patient’s family and the country.
In conclusion, for mild to moderate GOV1, endoscopic reverse body ligation is safer, more effective, more economical and easier to perform than TAI, thus confirming that this approach is beneficial for patients and is worthy of clinical application. EBL is a better treatment for gastric varices in patients with mild or moderate GOV1.
During the treatment of type 1 gastric variceal hemorrhage (GOV1), endoscopic band ligation (EBL), endoscopic tissue adhesive injection (TAI) and endoscopic injection sclerotherapy can cause serious complications. Therefore, individualized treatment is urgently needed.
The optimal individualized therapy for patients with mild or moderate GOV1 has yet to be identified. It is important to choose the appropriate treatment modality according to the type, morphology and severity of varicose veins to further improve the treatment efficacy and minimize the incidence of associated complications. Thus, this new treatment will greatly reduce patient suffering.
We focused on comparing the differences between the EBL and TAI treatments. This study provides new ideas for the treatment of mild and moderate GOV1.
This retrospective study compared the efficacy, safety and costs of EBL and TAI. A detailed comparison of the varicose-relief rate, operative time, operation success rate, mortality rate within 6 wk, rebleeding rate, 6-wk operation-related ulcer healing rate, complication rate and average operation cost was performed.
EBL has a higher one-time varix eradication rate, a higher 6-wk operation-related ulcer healing rate, a lower delayed rebleeding rate and a lower cost than TAI for mild to moderate GOV1.
This study provides a new method for the treatment of mild to moderate GOV1:EBL.
EBL has a higher one-time varix eradication rate, higher 6-wk operation-related ulcer healing rate, lower delayed rebleeding rate and lower cost than TAI for mild to moderate GOV1.
Our research team will expand the sample size and study the treatment of different levels of gastric varices in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Christodoulidis G, Greece; Popovic DD, Serbia S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Kim DH, Cho E, Jun CH, Son DJ, Lee MJ, Park CH, Cho SB, Park SY, Kim HS, Choi SK, Rew JS. Risk Factors and On-site Rescue Treatments for Endoscopic Variceal Ligation Failure. Korean J Gastroenterol. 2018;72:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 2. | Ginès P, Krag A, Abraldes JG, Solà E, Fabrellas N, Kamath PS. Liver cirrhosis. Lancet. 2021;398:1359-1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 856] [Article Influence: 214.0] [Reference Citation Analysis (1)] |
| 3. | Gralnek IM, Camus Duboc M, Garcia-Pagan JC, Fuccio L, Karstensen JG, Hucl T, Jovanovic I, Awadie H, Hernandez-Gea V, Tantau M, Ebigbo A, Ibrahim M, Vlachogiannakos J, Burgmans MC, Rosasco R, Triantafyllou K. Endoscopic diagnosis and management of esophagogastric variceal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:1094-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 4. | Zeng XQ, Ma LL, Tseng YJ, Chen J, Cui CX, Luo TC, Wang J, Chen SY. Endoscopic cyanoacrylate injection with or without lauromacrogol for gastric varices: A randomized pilot study. J Gastroenterol Hepatol. 2017;32:631-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Nakayama S, Murashima N. Extrusion of Glue Cast after Sclerotherapy. Intern Med. 2015;54:2781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Cheng LF, Wang ZQ, Li CZ, Lin W, Yeo AE, Jin B. Low incidence of complications from endoscopic gastric variceal obturation with butyl cyanoacrylate. Clin Gastroenterol Hepatol. 2010;8:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 7. | Smith A, Baumgartner K, Bositis C. Cirrhosis: Diagnosis and Management. Am Fam Physician. 2019;100:759-770. [PubMed] |
| 8. | Beppu K, Inokuchi K, Koyanagi N, Nakayama S, Sakata H, Kitano S, Kobayashi M. Prediction of variceal hemorrhage by esophageal endoscopy. Gastrointest Endosc. 1981;27:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 553] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, Austin A, Ferguson JW, Olliff SP, Hudson M, Christie JM; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64:1680-1704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 416] [Article Influence: 41.6] [Reference Citation Analysis (2)] |
| 10. | Wani ZA, Bhat RA, Bhadoria AS, Maiwall R, Choudhury A. Gastric varices: Classification, endoscopic and ultrasonographic management. J Res Med Sci. 2015;20:1200-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1440] [Article Influence: 180.0] [Reference Citation Analysis (3)] |
| 12. | Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244-1249. [PubMed] |
| 13. | Jakab SS, Garcia-Tsao G. Screening and Surveillance of Varices in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2019;17:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Chang DF, Mei ZC, He S, Guo JJ, Deng L. [Clinical efficacy of endoscopic gastric variceal ligation vs. gastric variceal obliteration in treating type 1 gastroesophageal varices bleeding]. J Chongqing Medical University. 2021;46:252-256. [DOI] [Full Text] |
| 15. | Hong HJ, Jun CH, Lee du H, Cho EA, Park SY, Cho SB, Park CH, Joo YE, Kim H, Choi SK, Rew JS. Comparison of Endoscopic Variceal Ligation and Endoscopic Variceal Obliteration in Patients with GOV1 Bleeding. Chonnam Med J. 2013;49:14-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Park SJ, Kim YK, Seo YS, Park SW, Lee HA, Kim TH, Suh SJ, Jung YK, Kim JH, An H, Yim HJ, Jang JY, Yeon JE, Byun KS. Cyanoacrylate injection versus band ligation for bleeding from cardiac varices along the lesser curvature of the stomach. Clin Mol Hepatol. 2016;22:487-494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Tan PC, Hou MC, Lin HC, Liu TT, Lee FY, Chang FY, Lee SD. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology. 2006;43:690-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 227] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 18. | Lo GH, Lin CW, Perng DS, Chang CY, Lee CT, Hsu CY, Wang HM, Lin HC. A retrospective comparative study of histoacryl injection and banding ligation in the treatment of acute type 1 gastric variceal hemorrhage. Scand J Gastroenterol. 2013;48:1198-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Qiao W, Ren Y, Bai Y, Liu S, Zhang Q, Zhi F. Cyanoacrylate Injection Versus Band Ligation in the Endoscopic Management of Acute Gastric Variceal Bleeding: Meta-Analysis of Randomized, Controlled Studies Based on the PRISMA Statement. Medicine (Baltimore). 2015;94:e1725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Garcia-Pagán JC, Barrufet M, Cardenas A, Escorsell A. Management of gastric varices. Clin Gastroenterol Hepatol. 2014;12:919-28.e1; quiz e51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 21. | Hu Z, Zhang D, Swai J, Liu T, Liu S. Risk of rebleeding from gastroesophageal varices after initial treatment with cyanoacrylate; a systematic review and pooled analysis. BMC Gastroenterol. 2020;20:181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Nakazawa M, Imai Y, Sugawara K, Uchida Y, Saitoh Y, Fujii Y, Uchiya H, Ando S, Nakayama N, Tomiya T, Mochida S. Long-term outcomes of patients with cirrhosis presenting with bleeding gastric varices. PLoS One. 2022;17:e0264359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Nelms DW, Pelaez CA. The Acute Upper Gastrointestinal Bleed. Surg Clin North Am. 2018;98:1047-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |