Published online Jul 28, 2022. doi: 10.3748/wjg.v28.i28.3595
Peer-review started: February 14, 2022
First decision: April 5, 2022
Revised: June 26, 2022
Accepted: June 26, 2022
Article in press: June 26, 2022
Published online: July 28, 2022
Processing time: 162 Days and 10.2 Hours
Hepatocellular carcinoma (HCC) is among the most common cancers and it is a major cause of cancer-related deaths. Non-alcoholic fatty liver disease (NAFLD) affects approximately one fourth of individuals worldwide and it is becoming one of the most important causes of HCC. The pathogenic mechanisms leading to NAFLD-related HCC are complex and not completely understood. However, metabolic, fibrogenic, oncogenic, inflammatory and immunological pathways seem to be involved. First-line therapy of advanced HCC has recently undergone major changes, since the combination of atezolizumab and bevacizumab was proven to increase survival when compared to sorafenib. Other immune-oncology drugs are also demonstrating promising results in patients with advanced HCC when compared to traditional systemic therapy. However, initial studies raised concerns that the advantages of immunotherapy might depend on the underlying liver disease, which seems to be particularly important in NAFLD-related HCC, as these tumors might not benefit from it. This article will review the mechanisms of NAFLD-related hepatocarcinogenesis, with an emphasis on its immune aspects, the efficacy of traditional systemic therapy for advanced NAFLD-related HCC, and the most recent data on the role of immunotherapy for this specific group of patients, showing that the management of this condition should be individualized and that a general recommendation cannot be made at this time.
Core Tip: Non-alcoholic fatty liver disease (NAFLD) is an important cause of hepatocellular carcinoma (HCC). While the treatment of advanced HCC has recently undergone a revolution led by immunotherapy, concerns have been raised that NAFLD-related HCC might not respond well to these new therapies. This review will approach the pathophysiology of NAFLD-related liver cancer, the evidence on traditional systemic treatments and the most recent data on immunotherapy for this particular group of patients, showing that the management of this condition should be individualized.
- Citation: Mattos ÂZ, Debes JD, Vogel A, Arrese M, Revelo X, Pase THS, Manica M, Mattos AA. Non-alcoholic fatty liver disease-related hepatocellular carcinoma: Is there a role for immunotherapy? . World J Gastroenterol 2022; 28(28): 3595-3607
- URL: https://www.wjgnet.com/1007-9327/full/v28/i28/3595.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i28.3595
The incidence of liver cancer worldwide was 11.6/100000 individuals in 2020 and its mortality rate reached 10.7/100000 in the same year, making it the sixth most common cancer and the second cause of cancer-related mortality[1]. Furthermore, it is estimated that its incidence rate will continue to increase until 2030[2]. Hepatocellular carcinoma (HCC) is by far the most common among primary liver cancers[3,4].
Non-alcoholic fatty liver disease (NAFLD) has a striking prevalence of 25% worldwide[5], which highlights its relevance as an underlying cause of HCC[6]. In the year of 2019, for instance, NAFLD was estimated to be associated with 36300 new cases of HCC, as well as with 34700 HCC-related deaths[7]. As it would be expected, the burden of NAFLD as a cause of HCC seems to be growing. It is estimated that the age-standardized incidence rate of NAFLD-related liver cancer will raise from 0.92 to 1.18/100000 individuals between 2018 and 2030[2]. Moreover, while a multinational cohort study demonstrated that NAFLD was responsible for 9% of HCC cases followed between 2005 and 2015 in South America (an area with high prevalence of NAFLD)[8], the same group verified that it was responsible for 34% of cases followed between 2019 and 2020[9].
Cirrhosis in general predisposes to HCC, and the annual incidence of HCC in patients with NAFLD-related cirrhosis ranges between 0.5% and 2.6%[10-13]. However, some specific mechanisms associated with NAFLD, which will be further discussed in this article, also allow for the development of HCC in the absence of cirrhosis, making NAFLD itself etiologically associated to hepatocarcinogenesis[6,14-16]. According to a meta-analysis, approximately 38% of NAFLD-related HCCs would develop in non-cirrhotic settings[17]. Still, it must be highlighted that the risk of developing HCC is much lower in patients with NAFLD who do not have cirrhosis than in those with NAFLD-related cirrhosis, as it has been recently shown in another meta-analysis (incidence of 0.03 vs 3.78/100 person-years)[18].
Significant progress has been recently made in the treatment of advanced HCC, when immunotherapy was proven superior to the systemic therapy used for over a decade[19,20]. Table 1 shows a summary of the most important randomized controlled trials on systemic therapy for advanced HCC.
| Ref. | Interventions | Mechanisms of action | Main results |
| Llovet et al[57] | Sorafenib × placebo | TKI × placebo | Increased OS with sorafenib |
| Cheng et al[56] | Sorafenib × placebo | TKI × placebo | Increased OS with sorafenib |
| Bruix1 et al[59] | Regorafenib × placebo | TKI × placebo | Increased OS with regorafenib |
| Kudo et al[61] | Lenvatinib × sorafenib | TKI × TKI | Non-inferior OS |
| Abou-Alfa2 et al[58] | Cabozantinib × placebo | TKI × placebo | Increased OS with cabozantinib |
| Zhu1,3 et al[60] | Ramucirumab × placebo | Anti-VEGF receptor 2 × placebo | Increased OS with ramucirumab |
| Yau et al[73] | Nivolumab × sorafenib | Anti-PD-1 × TKI | No increase in OS4 |
| Finn1 et al[74] | Pembrolizumab × placebo | Anti-PD-L1 × placebo | No increase in OS4 |
| Finn et al[19] | Atezolizumab + bevacizumab × sorafenib | Anti-PD-L1 + anti-VEGF × TKI | Increased OS with atezolizumab + bevacizumab |
| Kelley et al[79] | Atezolizumab + cabozantinib × sorafenib × cabozantinib | Anti-PD-L1 + TKI × TKI × TKI | No increase in OS4 |
| Abou-Alfa et al[82] | Tremelimumab + durvalumab × durvalumab × sorafenib | Anti-CTLA-4 + anti-PD-L1 × anti-PD-L1 × TKI | Increased OS with tremelimumab + durvalumab (× sorafenib). Non-inferior OS with durvalumab (× sorafenib) |
Nevertheless, initial studies raised concerns that the advantages of immunotherapy might depend on the underlying liver disease, and that patients with NAFLD-related HCC might benefit less from it[21,22]. Considering the epidemiological importance of NAFLD-related HCC, this article aims to review the mechanisms behind NAFLD-related hepatocarcinogenesis, with an emphasis on its immune aspects, the knowledge gathered over the years on the efficacy of traditional systemic therapy for advanced NAFLD-related HCC, and the most up-to-date evidence on the role of immunotherapy for this specific group of patients.
The underlying pathogenic mechanisms leading to NAFLD-related HCC are complex and not completely understood[10,23,24]. Metabolic dysfunction as well as inflammatory, fibrogenic and oncogenic pathways are involved, which are in turn modulated by a myriad of factors. These include, among others, genetic and epigenetic changes, different degrees of dysregulation of multiorgan metabolic and endocrine signaling, altered immunologic responses and changes in gut microbiota[24,25].
A disturbed systemic metabolic milieu characterized mainly by insulin resistance and a low-grade inflammatory state seems to be a key in promoting carcinogenesis in a fat-laden liver. Both type 2 diabetes and obesity are known risk factors for NAFLD-related HCC, which may act additively with other metabolic syndrome traits (i.e., dyslipidemia and hypertension) in increasing the risk of HCC development[25,26]. However, the precise molecular mechanisms underpinning the connection between metabolic dysfunction and HCC remain incompletely understood. Metabolic dysfunction-related changes in lipid metabolism (including uncontrolled lipolysis in adipose tissue leading to fatty acid overflow towards the liver and stimulation of hepatic de novo lipogenesis) lead to hepatocyte lipid overload that, in turn, triggers some compensatory adaptations such as downregulation of carnitine palmitoyltransferase 2, which may promote hepatocarcinogenesis. Accumulation of acylcarnitine has been suggested as a potential mechanism in this regard[27]. Also, changes in sterol regulatory element-binding proteins transcription factors, key regulators of sterol and fatty acid biosynthesis, may contribute through interaction with tumor suppressor genes such as p53[28].
Importantly, lipid overload also leads to the occurrence of oxidative stress, endoplasmic reticulum stress, mitochondrial dysfunction, cell injury and cell death, all triggering inflammatory responses and activating fibrogenic processes[29]. Moreover, numerous signaling pathways are also dysregulated, including activation of interleukin (IL)-6/Janus kinase/signal transducer and activator of transcription (STAT) pathway and insulin-like growth factor, among others[30].
Of note, in the setting of a chronic inflammatory microenvironment, death of hepatocytes by different mechanisms (necrosis, apoptosis, pyroptosis and other forms of the cell death) determines a compensatory hepatocyte proliferation. This proliferative response is associated with genetic and epigenetic changes that play a pivotal role in hepatocarcinogenesis. Among these genetic changes, different studies have identified mutations in the telomerase reverse transcriptase promoter, p53 gene and wingless-related integration site (Wnt)/β-catenin signaling pathway genes as the most consistent genetic changes during HCC development[26]. Finally, epigenetic modifications have been shown to be involved in HCC progression in the context of NAFLD. A broad range of changes in chromatin remodeling, histone alterations, DNA methylation, and noncoding RNA expression has been described and reviewed recently[31]. Such processes have diagnostic, prognostic, and therapeutic implications[32].
Experimental evidence generated in mouse models and some human data strongly suggest that altered gut microbiota may be an important contributing factor to HCC development in the setting of NAFLD/nonalcoholic steatohepatitis (NASH)[33]. The occurrence of dysbiosis is common in NAFLD/NASH, as well as in its commonly associated comorbidities, such as obesity and type 2 diabetes. Nevertheless, although microbiome changes have been characterized in different studies involving subjects with NASH or NAFLD-related cirrhosis, there is considerable variability across different reports, and only few studies have focused specifically on NAFLD-related HCC. Ponziani et al[34] showed that cirrhotic NAFLD-related HCC patients had a microbiome profile enriched in Bacteroides and Ruminococcaceae compared to patients with NAFLD-related cirrhosis without HCC[34]. This microbiota profile was associated with increased levels of some circulating proinflammatory cytokines. However, it remains unclear if this is just an epiphenomenon or has pathogenetic relevance.
Mechanistically, dysbiosis leads to altered intestinal permeability, which in turn contributes to hepatic inflammation via toll-like receptor 4 (TLR4) stimulation by bacterial derived products. Sustained hepatic inflammation triggered by this pathway can then contribute to hepatocarcinogenesis through multiple mechanisms[23]. Consistent with this proposed mechanism, TLR4 ablation has been shown to prevent HCC development in NASH models[35]. Additionally, changes in gut microbiota critically influence bile acid metabolism. Thus, animals fed with a NASH-promoting diet exhibit a change in their bile acid pool composition, which become enriched in secondary bile acids, particularly deoxycholic acid[33]. Moreover, microbiome changes may induce the transition of hepatic stellate cells (HSCs) in the stroma into a senescence-associated secretory phenotype, which are cells associated with suppression of antitumor immunity[36].
Specific genetic polymorphisms that influence NAFLD susceptibility and severity, such as patatin-like phospholipase domain containing protein 3 (PNPLA3), transmembrane 6 superfamily member 2 and membrane bound O-acetyltransferase domain containing 7, have been linked to a higher risk for NAFLD-related HCC[26]. Of these polymorphisms, the I148M variant of PNPLA3 is one of striking relevance in HCC development[37]. Carriage of this variant critically influences triacylglycerol remodeling in hepatocytes, and recent evidence shows that it also influences fibrogenesis and carcinogenesis by impairing retinol release from HSCs[38].
NAFLD-related HCC generally emerges in the setting of cirrhosis, but may arise also in a non-cirrhotic liver. Some pathways have been shown to play a role in this scenario. Increased STAT-3 signaling has been shown to be associated to the development of HCC independently of NASH and fibrosis. Also, disruption of circadian homeostasis has been shown to be related to HCC development independently of cirrhosis[39].
In summary, pathobiological mechanisms of hepatocarcinogenesis result from a complex interaction of the above-mentioned factors leading to uncontrolled proliferative responses, dysregulation of DNA-damage-response pathways, activation of survival signaling, angiogenesis, evasion of immune surveillance, genomic instability and ultimately to cancer development. It is likely that, in NAFLD patients, mechanisms leading to HCC vary from one subject to another given the heterogenous population grouped under the acronym[40]. Precision medicine approaches based on advanced biomarkers may help identify those at higher risk of developing HCC in order to include them in surveillance programs or, once diagnosed, may allow treatment with targeted therapies.
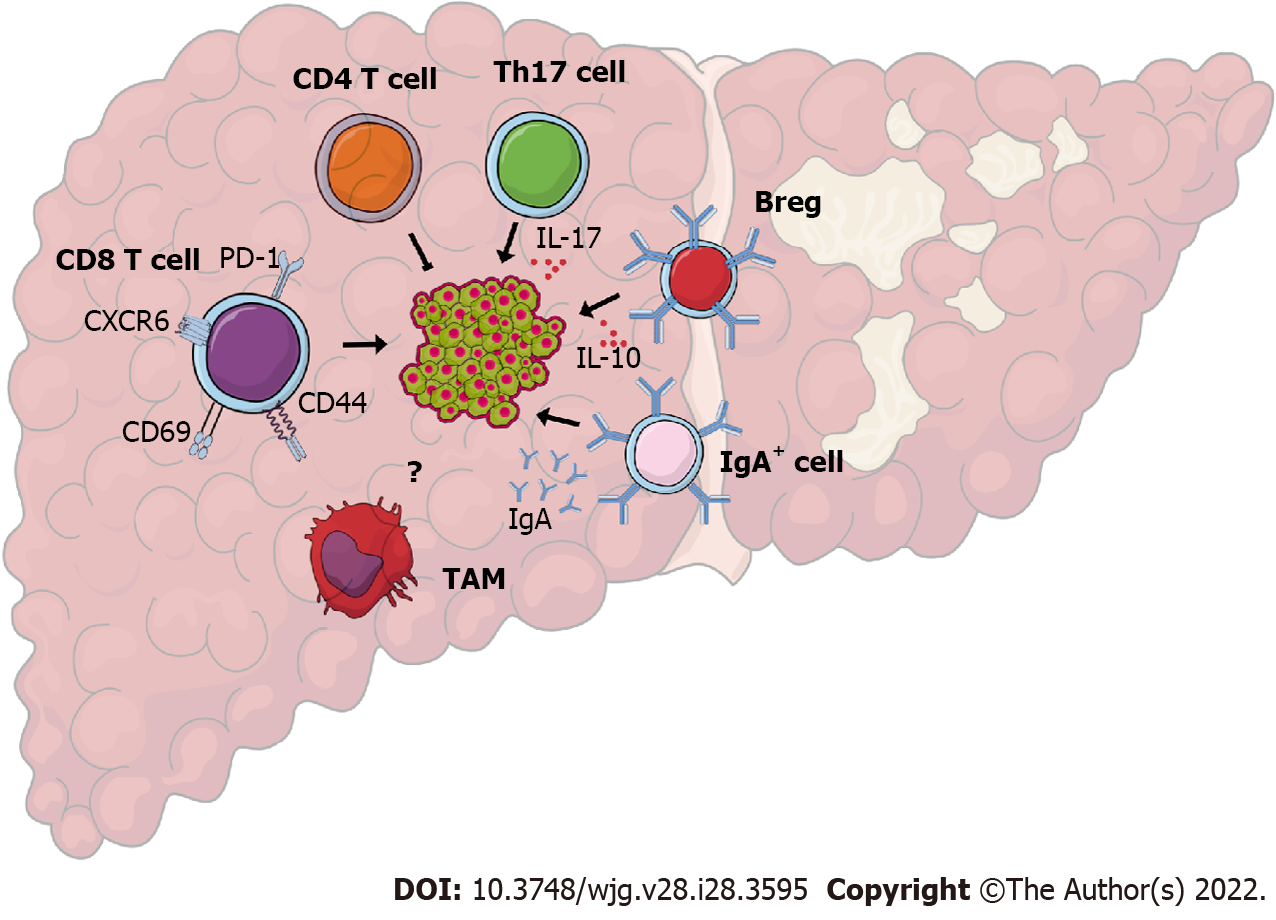
Emerging evidence suggests that the chronic inflammatory process of NAFLD and NASH sets the basis for the development of HCC[41]. In addition, there seems to be a role for innate and adaptive immune cells in the pathogenesis of NAFLD-related HCC (Figure 1). However, the immune mechanisms that are specific to NAFLD as the underlying cause of HCC are largely unclear. For example, numerous studies have demonstrated the critical involvement of hepatic macrophages, including resident Kupffer cells and recruited monocyte-derived macrophages in the pathogenesis of NASH[42]. The activation of Kupffer cells is crucial for tumor development in the early stage of chemical-induced carcinogenesis[43] and tumor-associated macrophages play a prominent role in promoting HCC once a primary tumor is established[44]. Nevertheless, the role of hepatic macrophages in NAFLD-related HCC has not been investigated yet.
Regarding the role of adaptive immunity as a central player in the progression of NAFLD-related HCC, several reports have shown increased recruitment of adaptive immune cells such as T and B lymphocytes into the liver of these patients. For instance, whole-exome sequencing of livers from patients with NAFLD-related HCC shows enrichment of gene signatures associated with T lymphocytes suggesting increased hepatic T cell accumulation[45]. Notably, studies show that HCC cases from NAFLD-related cirrhosis display features of immune exhaustion, indicating a state of dysfunction likely due to stimulation by tumor antigens[45].
Experimental murine models of NAFLD-related HCC have shed light on the potential mechanisms by which T cells regulate HCC development. In a mouse model of NAFLD-related HCC that recapitulates metabolic disease, intrahepatic CD8 T cells become activated and express CD44 and CD69, suggesting that they can directly induce liver damage through interactions with hepatocytes[46]. Indeed, genetic ablation of CD8 T cells in this mouse model ameliorates liver damage, NASH, and HCC development, suggesting that CD8 T cells directly instigate disease progression[46]. The increased T cell infiltration in NAFLD-related HCC has been attributed to the inactivation of T cell protein tyrosine phosphatase in hepatocytes and increased expression of T cell chemoattractants[47]. Mechanistically, NASH programs CD8 T cells to acquire an activated exhausted phenotype and express increased levels of programmed cell death protein 1 (PD-1) in response to metabolic signals as well as to IL-15, instigating their non-specific killing of hepatocytes and disease progression[48]. In addition to exhaustion markers, NASH-derived PD-1 positive CD8 T cells express high levels of effector function molecules such as tumor necrosis factor α, interferon γ, and granzyme[21]. The increased activity of exhausted PD-1 positive CD8 T cells in the NASH liver is not limited to accelerating liver damage but can result in impaired immune surveillance and subsequent HCC[21].
In contrast to the accumulation of CD8 T cells, lipid dysregulation has been shown to cause a loss of CD4 T cells in tumor-free and tumor-bearing environments in the liver of mice with NASH induced by a methionine and choline-deficient L-amino acid-defined diet[49]. Importantly, depletion of total CD4 T cells promoted hepatic carcinogenesis in a MYC oncogene model of HCC, suggesting that the overall function of CD4 T cells is to provide antitumor immunity[49]. However, nutrient overload induces a subset of CD4 T cells known as T helper-17 cells that produce large amounts of IL-17A to promote tumorigenesis in NAFLD-related HCC[50]. Overall, these findings suggest that the exhaustion of hepatic CD8 T cells and the loss of CD4 T cells in NASH compromise the hepatic antitumor surveillance and increase the susceptibility to HCC.
In addition to T cells, emerging evidence suggests that immunoglobulin A (IgA)-producing B cells play a critical role in the progression of NAFLD-related HCC. In humans, the number of tumor-infiltrating B cells correlates with tumor progression[51]. Likewise, patients with HCC that have fewer tumor-infiltrating plasma cells present a better prognosis[52]. Feeding a high fat diet to major urinary protein-urokinase-type plasminogen activator transgenic mice, a reliable model of NAFLD-related HCC, instigates IgA-producing cells to interfere with the protective role of anti-tumor cytotoxic CD8 T cells[53]. The IgA positive B cells inhibit the activity of CD8 T cells through the expression of programmed death-ligand 1 (PD-L1) and the production of the immunosuppressive cytokine IL-10[53]. Regulatory B cells, a subset of B cells, can also inhibit anti-tumor immunity through IL-10 production and promote HCC growth through direct interactions with the tumor cells[54]. As B cells promote NAFLD through the production of pro-inflammatory cytokines and regulation of intrahepatic T cells in NASH[55], future studies are needed to clarify the precise role of liver B cells in NAFLD-related HCC.
Systemic therapy for HCC is relatively young in comparison to other cancers, becoming available only after 2007, with the arrival of sorafenib, a multikinase inhibitor that showed improved survival against placebo in both the SHARP and Asia-Pacific trials[56,57]. For 10 years, sorafenib was the only available systemic therapy for HCC, until the field expanded significantly over the last 5 years with trials showing benefit from regorafenib, lenvatinib, cabozantinib and ramucirumab[58-61]. All of these studies were performed on HCCs from multiple etiologies, but primarily viral hepatitis-related tumors. Recently, attention has shifted to the importance of HCC etiology as a predictor of response to systemic therapy. This issue has been most evident in HCC immunotherapy, but potentially applies to other systemic therapies as well.
NAFLD-related HCC represents a unique conundrum for systemic therapy, as metabolic issues beyond that of HCC may play a role[62]. Individuals with NAFLD-related HCC are more likely to be obese, and are more likely to be on hormone-related medications, both of which could affect the pharmacokinetics of systemic therapy. Indeed, a small study showed that patients on sorafenib who were receiving metformin for diabetes mellitus had worse survival than those on insulin, regardless of the cause of HCC[63].
Due to the temporal dynamics of HCC systemic therapy in the last 15 years, most of the available data is from sorafenib studies. Sorafenib is known to perform best when used in patients with viral hepatitis-related HCC, particularly hepatitis C infection. However, most studies addressed hepatitis C vs alcohol-related HCC, or viral hepatitis vs other causes of HCC, clouding the understanding of the role of sorafenib in NAFLD-related HCC specifically[64-66]. An international study, presented only in abstract form, found similar overall survival (OS) in patients treated with sorafenib with NAFLD-related HCC vs other causes [hazard ratio (HR): 0.94, 95% confidence interval (CI): 0.76-1.16, P = 0.57]. However, the NAFLD portion of the study included only 187 patients (3.5% of the total cohort), and further details are awaited with the full peer-reviewed version[67]. A recent retrospective subgroup analysis including 483 NAFLD-related HCC patients treated with sorafenib also found no significant difference in univariate analysis of survival between NAFLD and other etiologies (10.2 mo vs 12.3 mo; HR: 1.06; 95%CI: 0.83-1.34, P = 0.63)[68].
Information on NAFLD-related HCC for other non-immune forms of systemic therapy remains rather elusive, although very recent studies are shedding some light on the field. The initial trials for regorafenib (RESORCE), cabozantinib (CELESTIAL) and ramucirumab (REACH-2) included very limited numbers of patients with NAFLD-related HCC (6.6%, 9.3% and 7.9% respectively), and most subgroup analyses did not specifically evaluate NAFLD-related HCC[58-60]. The CELESTIAL trial for cabozantinib indicated benefit of the drug across all subgroups of etiologic factors and found no difference for OS between viral hepatitis-related HCC and other etiologies (HR: 0.76, 95%CI: 0.63-0.92 vs HR: 0.72, 95%CI: 0.54-0.96). However, the “other etiologies” group included all non-viral hepatitis-related tumors, with the NASH proportion conforming 43 patients. Also, this trial evaluated cabozantinib as second line therapy[58].
More recently, retrospective studies have evaluated lenvatinib in NAFLD-related HCC, suggesting an advantage for this multikinase inhibitor in this group of patients. A multicenter analysis of 236 NAFLD-related HCCs treated with lenvatinib (19% of the entire cohort) found a better OS for NAFLD-related HCC compared to other etiologies (22.2 mo vs 15.1 mo, HR: 0.69, 95%CI: 0.56-0.85, P = 0.0006)[68]. A Japanese study (also retrospective) of lenvatinib in unresectable tumors involving 103 NAFLD-related HCCs found no difference in OS compared to other etiologies, but the progression free survival (PFS) was better in the NAFLD group (median 9.3 mo vs 7.5 mo, P = 0.01)[69]. Furthermore, the retrospective multicenter ELEVATOR study, in which 200 patients were treated with lenvatinib, observed a similar survival in patients with viral and non-viral (NASH and alcoholic steatohepatitis) related HCC[70].
This early evidence suggests that sorafenib or cabozantinib are not particularly better (or worse) for NAFLD-related HCC, and that the use of lenvatinib might pose an advantage, with no specific data, so far, for regorafenib. Nevertheless, it should be noted that better studies are needed in order to draw significant conclusions.
In recent years, besides several tyrosine kinase inhibitors and a monoclonal antibody against vascular endothelial growth factor (VEGF) receptor-2 being added to the treatment armamentarium, immunotherapy with immune checkpoint blockers has been extensively investigated in patients with HCC[71]. Nivolumab, pembrolizumab, and the combination of nivolumab plus ipilimumab have been approved by the United States Food and Drug Administration (FDA) based on very promising phase II studies[72], but nivolumab and pembrolizumab failed to reach their primary endpoints in subsequent phase III trials in first- and second-line, respectively[73,74].
Overexpression of VEGF has been associated with liver cancer development and progression, and small phase II studies have shown modest anti-tumor efficacy of bevacizumab as monotherapy in advanced HCC[75]. In addition to the antiangiogenic effects, there is increasing evidence that anti-VEGF therapies may enhance the efficacy of anti-PD-1 and anti-PD-L1 by reversing VEGF-mediated immunosuppression and promoting T-cell infiltration in tumors[76]. Based on these observations, the PD-L1 inhibitor atezolizumab was evaluated together with the VEGF inhibitor bevacizumab in the phase III IMbrave150 study. The combination significantly improved all efficacy endpoints with a statistically significant and clinically meaningful survival benefit compared to sorafenib[19,77]. Side effect profiles of the drugs were in line with their respective mechanism of action and no new safety signals were observed. Additionally, patient-reported outcomes revealed that deteriorations in quality of life were significantly delayed in the combination arm compared to the sorafenib arm[78]. The combination has been approved by the FDA and by the European Medicines Agency (EMA), and it is currently regarded as the standard of care in first-line therapy of advanced HCC.
In the COSMIC-312 trial, in which 837 patients with HCC were randomized to be treated with atezolizumab plus cabozantinib, sorafenib in monotherapy or cabozantinib in monotherapy (2:1:1), PFS was 6.8 mo for the group receiving combination therapy, compared to 4.2 mo for the group under sorafenib (HR: 0.63, 95%CI: 0.44-0.91, P = 0.0012). Regarding OS, an interim analysis did not demonstrate a significant difference between combination treatment and monotherapy with sorafenib (HR: 0.90, 95%CI: 0.69-1.18, P = 0.438). Finally, the interim analysis on the comparison between cabozantinib and sorafenib showed a tendency favoring cabozantinib regarding PFS (HR: 0.71, 95%CI: 0.51-1.01)[79].
Two antibodies against cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) have been investigated in advanced HCC. The combination of nivolumab and ipilimumab has already shown improved OS in HCC patients in the phase I/II CheckMate040 study[80,81]. The pure immune-oncology (IO) combination achieved a high overall response rate with a promising OS of almost 23 mo. The most common immune related adverse events were rash, hepatitis, and adrenal insufficiency. Based on these results, the FDA approved nivolumab plus ipilimumab as second-line treatment for patients with advanced HCC previously treated with sorafenib. Currently, the checkmate 9DW study evaluates the efficacy of nivolumab plus ipilimumab compared to sorafenib or lenvatinib as first-line therapy.
Similar to ipilimumab, tremelimumab has also been studied as an anti-CTLA-4 antibody in HCC. Based on promising phase II data, the combination of durvalumab and tremelimumab was compared with durvalumab in monotherapy or sorafenib in monotherapy as first-line therapy for unresectable HCC in the HIMALAYA trial. Regarding the comparison between combination therapy and monotherapy with sorafenib, there was a significant improvement in OS favoring combination therapy (16.4 mo vs 13.8 mo, HR: 0.78, 95%CI: 0.65-0.92, P = 0.0035), and durvalumab plus tremelimumab may be approved by the FDA and EMA in the near future as an additional option for first-line treatment in HCC. Finally, monotherapy with durvalumab was noninferior to sorafenib regarding OS (HR: 0.86, 95%CI: 0.73-1.03)[82].
A very recent study suggested that clinicians might need to consider the underlying liver disease for treatment selection in HCC. Pfister et al[21] provided provocative preclinical and limited clinical evidence that patients with NAFLD-related HCC may benefit less from immune checkpoint inhibition than patients with viral hepatitis-related HCC. Regarding preclinical data, authors evaluated immunotherapy in mice with NAFLD-related HCC. Despite the hepatic abundance of PD-1 positive CD8 T cells with features of exhaustion and effector functions in mice with NASH, which might be suggestive of a good response to immunotherapy, none of the pre-existing tumors regressed with treatment, and there was evidence indicating that immunotherapy could even play a role in hepatocarcinogenesis in mice with NASH. In the same publication, a meta-analysis of three randomized controlled phase III trials failed to demonstrate evidence of survival improvement for patients with non-viral hepatitis-related HCC receiving immunotherapy. The authors also investigated a cohort of 130 HCC cases, in which 13 were NAFLD-related and had OS after immunotherapy of 5.4 mo, significantly lower than that of patients with HCCs related to other causes of liver disease (11.0 mo, P = 0.023). Finally, authors validated these findings in yet another cohort of 118 individuals with HCC, in which 11 were NAFLD-related and had OS of 8.8 mo, while patients with HCC related to other causes of liver disease had OS of 17.7 mo (P = 0.034)[21]. Nevertheless, important remarks on this study have been made in an editorial, which highlighted that patients with NASH were not separated from those with other non-viral hepatitis etiologies of liver disease in the meta-analysis presented in the paper, and that the small number of patients evaluated in the cohorts must be kept in mind when considering their results[83].
In the same line, both the Checkmate-459 and the IMBrave150 trials found that HR for OS was worse in patients with non-viral hepatitis-related HCC compared with patients with viral hepatitis-related cancer. However, neither study distinguished between patients with NASH and alcoholic steatohepatitis. In addition, it should be noted that the poor HRs in the non-viral hepatitis group were not solely due to the shorter survival in the IO arm, but also to a surprisingly long survival in the sorafenib arm of both trials[19,84]. Similarly, in the COSMIC-312 trial, when a subgroup analysis on etiology of the underlying liver disease was performed, the benefit of atezolizumab plus cabozantinib on PFS seemed to be driven by the hepatitis B-related HCC group, and there was no significant difference between combination therapy and sorafenib for patients with non-viral hepatitis related-HCC (HR: 0.92, 95%CI: 0.60-1.41)[79].
Another recent meta-analysis of randomized controlled trials helped fuel this debate, when it also demonstrated that immune checkpoint inhibitors were significantly more effective for viral hepatitis-related HCCs than for tumors associated with other kinds of liver disease. On the other hand, the etiology of liver disease did not seem to interfere with the efficacy of tyrosine-kinase inhibitors or anti-VEGF therapies[22].
In contrast to these observations, underlying liver disease (viral hepatitis vs alcohol vs NASH) did not significantly impact PFS and OS in a recent real-world cohort treated with atezolizumab and bevacizumab[85]. Moreover, in the HIMALAYA trial, the benefit of the combination of durvalumab and tremelimumab on OS persisted in the subgroup analysis in patients with non-viral hepatitis related-HCC (HR: 0.74, 95%CI: 0.57-0.95)[82].
Perhaps the decision to start immunotherapy might be guided by prognostic biomarkers, rather than solely by the etiology of liver disease. Several predictive biomarkers for immunotherapy response have been proposed, including PD-L1 expression[86] and evidence of activated Wnt/β-catenin signaling[87], but currently no validated biomarker exists to guide treatment decisions in HCC patients undergoing immunotherapy. The recently proposed CRAFITY score (C reactive protein and alpha-fetoprotein in ImmunoTherapY) may be an easy-to-use tool to predict outcomes of patients undergoing immunotherapy for HCC, regardless of Child-Pugh class and performance status[88].
As the field moves forward, and with early evidence suggesting a potential decreased response of NAFLD-related HCC to immunotherapy, studies of non-immune systemic therapy for this group of patients should become more frequent and more robust. Moreover, randomized controlled trials evaluating immunotherapy in this particular group of patients are of the utmost importance. Multiple issues should be taken into account in such studies, including the strict definition of NAFLD, metabolic associated fatty liver disease or NASH, the heterogeneity of this group which includes lean NAFLD, NAFLD related to metabolic syndrome and others, as well as the impact of other co-morbidities and medication profiles.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Federação Brasileira De Gastroenterologia.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghoneim S, United States; Marchesini G, Italy S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | World Health Organization. Global Cancer Observatory-GLOBOCAN 2020. [cited 14 February 2022]. Available from: https://gco.iarc.fr/. |
| 2. | Liu Z, Xu K, Jiang Y, Cai N, Fan J, Mao X, Suo C, Jin L, Zhang T, Chen X. Global trend of aetiology-based primary liver cancer incidence from 1990 to 2030: a modelling study. Int J Epidemiol. 2021;50:128-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 3. | McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of Hepatocellular Carcinoma. Hepatology. 2021;73 Suppl 1:4-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 820] [Cited by in RCA: 1344] [Article Influence: 336.0] [Reference Citation Analysis (1)] |
| 4. | Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, Bray F. Global Burden of 5 Major Types of Gastrointestinal Cancer. Gastroenterology. 2020;159:335-349.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 857] [Cited by in RCA: 1231] [Article Influence: 246.2] [Reference Citation Analysis (0)] |
| 5. | Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5322] [Cited by in RCA: 7541] [Article Influence: 837.9] [Reference Citation Analysis (0)] |
| 6. | Anstee QM, Reeves HL, Kotsiliti E, Govaere O, Heikenwalder M. From NASH to HCC: current concepts and future challenges. Nat Rev Gastroenterol Hepatol. 2019;16:411-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 814] [Cited by in RCA: 965] [Article Influence: 160.8] [Reference Citation Analysis (0)] |
| 7. | GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11327] [Cited by in RCA: 9637] [Article Influence: 1927.4] [Reference Citation Analysis (35)] |
| 8. | Debes JD, Chan AJ, Balderramo D, Kikuchi L, Gonzalez Ballerga E, Prieto JE, Tapias M, Idrovo V, Davalos MB, Cairo F, Barreyro FJ, Paredes S, Hernandez N, Avendaño K, Diaz Ferrer J, Yang JD, Carrera E, Garcia JA, Mattos AZ, Hirsch BS, Gonçalves PT, Carrilho FJ, Roberts LR. Hepatocellular carcinoma in South America: Evaluation of risk factors, demographics and therapy. Liver Int. 2018;38:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 9. | Farah M, Diaz Ferrer J, Baca EL, Mattos A, Arrese M, Prieto Ortiz JE, Balderramo D, Carrera E, Boonstra A, Debes JD. Changing epidemiology of hepatocellular carcinoma in South America: a report from the ESCALON Network. Hepatology. 2021;74 Suppl 1:681A. |
| 10. | Banini BA, Sanyal AJ. NAFLD-related HCC. Adv Cancer Res. 2021;149:143-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972-1978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 893] [Cited by in RCA: 965] [Article Influence: 64.3] [Reference Citation Analysis (1)] |
| 12. | Yatsuji S, Hashimoto E, Tobari M, Taniai M, Tokushige K, Shiratori K. Clinical features and outcomes of cirrhosis due to non-alcoholic steatohepatitis compared with cirrhosis caused by chronic hepatitis C. J Gastroenterol Hepatol. 2009;24:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 239] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 13. | Amarapurkar DN, Dharod M, Gautam S, Patel N. Risk of development of hepatocellular carcinoma in patients with NASH-related cirrhosis. Trop Gastroenterol. 2013;34:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Levrero M, Zucman-Rossi J. Mechanisms of HBV-induced hepatocellular carcinoma. J Hepatol. 2016;64:S84-S101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 710] [Article Influence: 78.9] [Reference Citation Analysis (0)] |
| 15. | Geh D, Manas DM, Reeves HL. Hepatocellular carcinoma in non-alcoholic fatty liver disease-a review of an emerging challenge facing clinicians. Hepatobiliary Surg Nutr. 2021;10:59-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 16. | Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2066] [Cited by in RCA: 3173] [Article Influence: 528.8] [Reference Citation Analysis (37)] |
| 17. | Stine JG, Wentworth BJ, Zimmet A, Rinella ME, Loomba R, Caldwell SH, Argo CK. Systematic review with meta-analysis: risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment Pharmacol Ther. 2018;48:696-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 260] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 18. | Orci LA, Sanduzzi-Zamparelli M, Caballol B, Sapena V, Colucci N, Torres F, Bruix J, Reig M, Toso C. Incidence of Hepatocellular Carcinoma in Patients With Nonalcoholic Fatty Liver Disease: A Systematic Review, Meta-analysis, and Meta-regression. Clin Gastroenterol Hepatol. 2022;20:283-292.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 129] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 19. | Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Xu DZ, Hernandez S, Liu J, Huang C, Mulla S, Wang Y, Lim HY, Zhu AX, Cheng AL; IMbrave150 Investigators. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020;382:1894-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2542] [Cited by in RCA: 4698] [Article Influence: 939.6] [Reference Citation Analysis (2)] |
| 20. | Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, Kelley RK, Galle PR, Mazzaferro V, Salem R, Sangro B, Singal AG, Vogel A, Fuster J, Ayuso C, Bruix J. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol. 2022;76:681-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1904] [Cited by in RCA: 2612] [Article Influence: 870.7] [Reference Citation Analysis (59)] |
| 21. | Pfister D, Núñez NG, Pinyol R, Govaere O, Pinter M, Szydlowska M, Gupta R, Qiu M, Deczkowska A, Weiner A, Müller F, Sinha A, Friebel E, Engleitner T, Lenggenhager D, Moncsek A, Heide D, Stirm K, Kosla J, Kotsiliti E, Leone V, Dudek M, Yousuf S, Inverso D, Singh I, Teijeiro A, Castet F, Montironi C, Haber PK, Tiniakos D, Bedossa P, Cockell S, Younes R, Vacca M, Marra F, Schattenberg JM, Allison M, Bugianesi E, Ratziu V, Pressiani T, D'Alessio A, Personeni N, Rimassa L, Daly AK, Scheiner B, Pomej K, Kirstein MM, Vogel A, Peck-Radosavljevic M, Hucke F, Finkelmeier F, Waidmann O, Trojan J, Schulze K, Wege H, Koch S, Weinmann A, Bueter M, Rössler F, Siebenhüner A, De Dosso S, Mallm JP, Umansky V, Jugold M, Luedde T, Schietinger A, Schirmacher P, Emu B, Augustin HG, Billeter A, Müller-Stich B, Kikuchi H, Duda DG, Kütting F, Waldschmidt DT, Ebert MP, Rahbari N, Mei HE, Schulz AR, Ringelhan M, Malek N, Spahn S, Bitzer M, Ruiz de Galarreta M, Lujambio A, Dufour JF, Marron TU, Kaseb A, Kudo M, Huang YH, Djouder N, Wolter K, Zender L, Marche PN, Decaens T, Pinato DJ, Rad R, Mertens JC, Weber A, Unger K, Meissner F, Roth S, Jilkova ZM, Claassen M, Anstee QM, Amit I, Knolle P, Becher B, Llovet JM, Heikenwalder M. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592:450-456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 845] [Article Influence: 211.3] [Reference Citation Analysis (1)] |
| 22. | Haber PK, Puigvehí M, Castet F, Lourdusamy V, Montal R, Tabrizian P, Buckstein M, Kim E, Villanueva A, Schwartz M, Llovet JM. Evidence-Based Management of Hepatocellular Carcinoma: Systematic Review and Meta-analysis of Randomized Controlled Trials (2002-2020). Gastroenterology. 2021;161:879-898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 158] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 23. | Shetty K, Chen J, Shin JH, Jogunoori W, Mishra L. Pathogenesis of hepatocellular carcinoma development in non alcoholic fatty liver disease. Curr Hepatol Rep. 2015;14:119-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Kanda T, Goto T, Hirotsu Y, Masuzaki R, Moriyama M, Omata M. Molecular Mechanisms: Connections between Nonalcoholic Fatty Liver Disease, Steatohepatitis and Hepatocellular Carcinoma. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 25. | Wegermann K, Hyun J, Diehl AM. Molecular Mechanisms Linking Nonalcoholic Steatohepatitis to Cancer. Clin Liver Dis (Hoboken). 2021;17:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Valenti L, Pedica F, Colombo M. Distinctive features of hepatocellular carcinoma in non-alcoholic fatty liver disease. Dig Liver Dis. 2022;54:154-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 27. | Fujiwara N, Nakagawa H, Enooku K, Kudo Y, Hayata Y, Nakatsuka T, Tanaka Y, Tateishi R, Hikiba Y, Misumi K, Tanaka M, Hayashi A, Shibahara J, Fukayama M, Arita J, Hasegawa K, Hirschfield H, Hoshida Y, Hirata Y, Otsuka M, Tateishi K, Koike K. CPT2 downregulation adapts HCC to lipid-rich environment and promotes carcinogenesis via acylcarnitine accumulation in obesity. Gut. 2018;67:1493-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 153] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 28. | Wu H, Ng R, Chen X, Steer CJ, Song G. MicroRNA-21 is a potential link between non-alcoholic fatty liver disease and hepatocellular carcinoma via modulation of the HBP1-p53-Srebp1c pathway. Gut. 2016;65:1850-1860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 160] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 29. | Schuster S, Cabrera D, Arrese M, Feldstein AE. Triggering and resolution of inflammation in NASH. Nat Rev Gastroenterol Hepatol. 2018;15:349-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 665] [Article Influence: 95.0] [Reference Citation Analysis (0)] |
| 30. | Garcia-Lezana T, Lopez-Canovas JL, Villanueva A. Signaling pathways in hepatocellular carcinoma. Adv Cancer Res. 2021;149:63-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 31. | Nagaraju GP, Dariya B, Kasa P, Peela S, El-Rayes BF. Epigenetics in hepatocellular carcinoma. Semin Cancer Biol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 177] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 32. | Geh D, Anstee QM, Reeves HL. NAFLD-Associated HCC: Progress and Opportunities. J Hepatocell Carcinoma. 2021;8:223-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Akkız H. The Gut Microbiome and Hepatocellular Carcinoma. J Gastrointest Cancer. 2021;52:1314-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 34. | Ponziani FR, Bhoori S, Castelli C, Putignani L, Rivoltini L, Del Chierico F, Sanguinetti M, Morelli D, Paroni Sterbini F, Petito V, Reddel S, Calvani R, Camisaschi C, Picca A, Tuccitto A, Gasbarrini A, Pompili M, Mazzaferro V. Hepatocellular Carcinoma Is Associated With Gut Microbiota Profile and Inflammation in Nonalcoholic Fatty Liver Disease. Hepatology. 2019;69:107-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 474] [Article Influence: 79.0] [Reference Citation Analysis (1)] |
| 35. | Miura K, Ishioka M, Minami S, Horie Y, Ohshima S, Goto T, Ohnishi H. Toll-like Receptor 4 on Macrophage Promotes the Development of Steatohepatitis-related Hepatocellular Carcinoma in Mice. J Biol Chem. 2016;291:11504-11517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, Iwakura Y, Oshima K, Morita H, Hattori M, Honda K, Ishikawa Y, Hara E, Ohtani N. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1318] [Cited by in RCA: 1651] [Article Influence: 137.6] [Reference Citation Analysis (0)] |
| 37. | Liu YL, Patman GL, Leathart JB, Piguet AC, Burt AD, Dufour JF, Day CP, Daly AK, Reeves HL, Anstee QM. Carriage of the PNPLA3 rs738409 C >G polymorphism confers an increased risk of non-alcoholic fatty liver disease associated hepatocellular carcinoma. J Hepatol. 2014;61:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 414] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 38. | Bruschi FV, Claudel T, Tardelli M, Caligiuri A, Stulnig TM, Marra F, Trauner M. The PNPLA3 I148M variant modulates the fibrogenic phenotype of human hepatic stellate cells. Hepatology. 2017;65:1875-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 193] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 39. | Kettner NM, Voicu H, Finegold MJ, Coarfa C, Sreekumar A, Putluri N, Katchy CA, Lee C, Moore DD, Fu L. Circadian Homeostasis of Liver Metabolism Suppresses Hepatocarcinogenesis. Cancer Cell. 2016;30:909-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 368] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 40. | Arrese M, Arab JP, Barrera F, Kaufmann B, Valenti L, Feldstein AE. Insights into Nonalcoholic Fatty-Liver Disease Heterogeneity. Semin Liver Dis. 2021;41:421-434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 41. | Giraud J, Chalopin D, Blanc JF, Saleh M. Hepatocellular Carcinoma Immune Landscape and the Potential of Immunotherapies. Front Immunol. 2021;12:655697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 142] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 42. | Krenkel O, Tacke F. Liver macrophages in tissue homeostasis and disease. Nat Rev Immunol. 2017;17:306-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 621] [Cited by in RCA: 1004] [Article Influence: 125.5] [Reference Citation Analysis (0)] |
| 43. | Wu J, Li J, Salcedo R, Mivechi NF, Trinchieri G, Horuzsko A. The proinflammatory myeloid cell receptor TREM-1 controls Kupffer cell activation and development of hepatocellular carcinoma. Cancer Res. 2012;72:3977-3986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 198] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 44. | Noy R, Pollard JW. Tumor-associated macrophages: from mechanisms to therapy. Immunity. 2014;41:49-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2889] [Cited by in RCA: 3071] [Article Influence: 279.2] [Reference Citation Analysis (0)] |
| 45. | Pinyol R, Torrecilla S, Wang H, Montironi C, Piqué-Gili M, Torres-Martin M, Wei-Qiang L, Willoughby CE, Ramadori P, Andreu-Oller C, Taik P, Lee YA, Moeini A, Peix J, Faure-Dupuy S, Riedl T, Schuehle S, Oliveira CP, Alves VA, Boffetta P, Lachenmayer A, Roessler S, Minguez B, Schirmacher P, Dufour JF, Thung SN, Reeves HL, Carrilho FJ, Chang C, Uzilov AV, Heikenwalder M, Sanyal A, Friedman SL, Sia D, Llovet JM. Molecular characterisation of hepatocellular carcinoma in patients with non-alcoholic steatohepatitis. J Hepatol. 2021;75:865-878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 145] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 46. | Wolf MJ, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, Ringelhan M, Simonavicius N, Egger M, Wohlleber D, Lorentzen A, Einer C, Schulz S, Clavel T, Protzer U, Thiele C, Zischka H, Moch H, Tschöp M, Tumanov AV, Haller D, Unger K, Karin M, Kopf M, Knolle P, Weber A, Heikenwalder M. Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 2014;26:549-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 547] [Article Influence: 49.7] [Reference Citation Analysis (0)] |
| 47. | Grohmann M, Wiede F, Dodd GT, Gurzov EN, Ooi GJ, Butt T, Rasmiena AA, Kaur S, Gulati T, Goh PK, Treloar AE, Archer S, Brown WA, Muller M, Watt MJ, Ohara O, McLean CA, Tiganis T. Obesity Drives STAT-1-Dependent NASH and STAT-3-Dependent HCC. Cell. 2018;175:1289-1306.e20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 286] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 48. | Dudek M, Pfister D, Donakonda S, Filpe P, Schneider A, Laschinger M, Hartmann D, Hüser N, Meiser P, Bayerl F, Inverso D, Wigger J, Sebode M, Öllinger R, Rad R, Hegenbarth S, Anton M, Guillot A, Bowman A, Heide D, Müller F, Ramadori P, Leone V, Garcia-Caceres C, Gruber T, Seifert G, Kabat AM, Mallm JP, Reider S, Effenberger M, Roth S, Billeter AT, Müller-Stich B, Pearce EJ, Koch-Nolte F, Käser R, Tilg H, Thimme R, Boettler T, Tacke F, Dufour JF, Haller D, Murray PJ, Heeren R, Zehn D, Böttcher JP, Heikenwälder M, Knolle PA. Auto-aggressive CXCR6+ CD8 T cells cause liver immune pathology in NASH. Nature. 2021;592:444-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 320] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 49. | Ma C, Kesarwala AH, Eggert T, Medina-Echeverz J, Kleiner DE, Jin P, Stroncek DF, Terabe M, Kapoor V, ElGindi M, Han M, Thornton AM, Zhang H, Egger M, Luo J, Felsher DW, McVicar DW, Weber A, Heikenwalder M, Greten TF. NAFLD causes selective CD4(+) T lymphocyte loss and promotes hepatocarcinogenesis. Nature. 2016;531:253-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 589] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 50. | Gomes AL, Teijeiro A, Burén S, Tummala KS, Yilmaz M, Waisman A, Theurillat JP, Perna C, Djouder N. Metabolic Inflammation-Associated IL-17A Causes Non-alcoholic Steatohepatitis and Hepatocellular Carcinoma. Cancer Cell. 2016;30:161-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 311] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 51. | Faggioli F, Palagano E, Di Tommaso L, Donadon M, Marrella V, Recordati C, Mantero S, Villa A, Vezzoni P, Cassani B. B lymphocytes limit senescence-driven fibrosis resolution and favor hepatocarcinogenesis in mouse liver injury. Hepatology. 2018;67:1970-1985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 52. | Zhang S, Liu Z, Wu D, Chen L, Xie L. Single-Cell RNA-Seq Analysis Reveals Microenvironmental Infiltration of Plasma Cells and Hepatocytic Prognostic Markers in HCC With Cirrhosis. Front Oncol. 2020;10:596318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 53. | Shalapour S, Lin XJ, Bastian IN, Brain J, Burt AD, Aksenov AA, Vrbanac AF, Li W, Perkins A, Matsutani T, Zhong Z, Dhar D, Navas-Molina JA, Xu J, Loomba R, Downes M, Yu RT, Evans RM, Dorrestein PC, Knight R, Benner C, Anstee QM, Karin M. Inflammation-induced IgA+ cells dismantle anti-liver cancer immunity. Nature. 2017;551:340-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 425] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 54. | Shao Y, Lo CM, Ling CC, Liu XB, Ng KT, Chu AC, Ma YY, Li CX, Fan ST, Man K. Regulatory B cells accelerate hepatocellular carcinoma progression via CD40/CD154 signaling pathway. Cancer Lett. 2014;355:264-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 55. | Barrow F, Khan S, Fredrickson G, Wang H, Dietsche K, Parthiban P, Robert S, Kaiser T, Winer S, Herman A, Adeyi O, Mouzaki M, Khoruts A, Hogquist KA, Staley C, Winer DA, Revelo XS. Microbiota-Driven Activation of Intrahepatic B Cells Aggravates NASH Through Innate and Adaptive Signaling. Hepatology. 2021;74:704-722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 134] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 56. | Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 4652] [Article Influence: 273.6] [Reference Citation Analysis (0)] |
| 57. | Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9016] [Cited by in RCA: 10270] [Article Influence: 604.1] [Reference Citation Analysis (2)] |
| 58. | Abou-Alfa GK, Meyer T, Cheng AL, El-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen Y, Park JW, Blanc JF, Bolondi L, Klümpen HJ, Chan SL, Zagonel V, Pressiani T, Ryu MH, Venook AP, Hessel C, Borgman-Hagey AE, Schwab G, Kelley RK. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N Engl J Med. 2018;379:54-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1630] [Cited by in RCA: 1769] [Article Influence: 252.7] [Reference Citation Analysis (0)] |
| 59. | Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G; RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2160] [Cited by in RCA: 2714] [Article Influence: 339.3] [Reference Citation Analysis (0)] |
| 60. | Zhu AX, Kang YK, Yen CJ, Finn RS, Galle PR, Llovet JM, Assenat E, Brandi G, Pracht M, Lim HY, Rau KM, Motomura K, Ohno I, Merle P, Daniele B, Shin DB, Gerken G, Borg C, Hiriart JB, Okusaka T, Morimoto M, Hsu Y, Abada PB, Kudo M; REACH-2 study investigators. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:282-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1027] [Cited by in RCA: 1249] [Article Influence: 208.2] [Reference Citation Analysis (0)] |
| 61. | Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib vs sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3128] [Cited by in RCA: 3827] [Article Influence: 546.7] [Reference Citation Analysis (1)] |
| 62. | Foerster F, Gairing SJ, Müller L, Galle PR. NAFLD-driven HCC: Safety and efficacy of current and emerging treatment options. J Hepatol. 2022;76:446-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 173] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 63. | Casadei Gardini A, Faloppi L, De Matteis S, Foschi FG, Silvestris N, Tovoli F, Palmieri V, Marisi G, Brunetti O, Vespasiani-Gentilucci U, Perrone G, Valgiusti M, Granato AM, Ercolani G, Negrini G, Tamburini E, Aprile G, Passardi A, Santini D, Cascinu S, Frassineti GL, Scartozzi M. Metformin and insulin impact on clinical outcome in patients with advanced hepatocellular carcinoma receiving sorafenib: Validation study and biological rationale. Eur J Cancer. 2017;86:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 64. | Bruix J, Cheng AL, Meinhardt G, Nakajima K, De Sanctis Y, Llovet J. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: Analysis of two phase III studies. J Hepatol. 2017;67:999-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 453] [Article Influence: 56.6] [Reference Citation Analysis (0)] |
| 65. | Bruix J, Raoul JL, Sherman M, Mazzaferro V, Bolondi L, Craxi A, Galle PR, Santoro A, Beaugrand M, Sangiovanni A, Porta C, Gerken G, Marrero JA, Nadel A, Shan M, Moscovici M, Voliotis D, Llovet JM. Efficacy and safety of sorafenib in patients with advanced hepatocellular carcinoma: subanalyses of a phase III trial. J Hepatol. 2012;57:821-829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 664] [Cited by in RCA: 654] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 66. | Leathers JS, Balderramo D, Prieto J, Diehl F, Gonzalez-Ballerga E, Ferreiro MR, Carrera E, Barreyro F, Diaz-Ferrer J, Singh D, Mattos AZ, Carrilho F, Debes JD. Sorafenib for Treatment of Hepatocellular Carcinoma: A Survival Analysis From the South American Liver Research Network. J Clin Gastroenterol. 2019;53:464-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 67. | Howell J, Samani A, Mannan B, Hajiev S, Aval LM, Abdelmalak R, Tam VC, Bettinger D, Thimme R, Taddei TH, Kaplan DE, Seidensticker M, Sharma R. Impact of NAFLD on clinical outcomes in hepatocellular carcinoma treated with sorafenib: An international cohort study. J Clin Oncol. 2021;39 Suppl 3:289. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 68. | Rimini M, Kudo M, Tada T, Shigeo S, Kang W, Suda G, Jefremow A, Burgio V, Iavarone M, Tortora R, Marra F, Lonardi S, Tamburini E, Piscaglia F, Masi G, Cabibbo G, Foschi FG, Silletta M, Kumada T, Iwamoto H, Aoki T, Goh MJ, Sakamoto N, Siebler J, Hiraoka A, Niizeki T, Ueshima K, Sho T, Atsukawa M, Hirooka M, Tsuji K, Ishikawa T, Takaguchi K, Kariyama K, Itobayashi E, Tajiri K, Shimada N, Shibata H, Ochi H, Yasuda S, Toyoda H, Fukunishi S, Ohama H, Kawata K, Tani J, Nakamura S, Nouso K, Tsutsui A, Nagano T, Takaaki T, Itokawa N, Okubo T, Arai T, Imai M, Joko K, Koizumi Y, Hiasa Y, Cucchetti A, Ratti F, Aldrighetti L, Cascinu S, Casadei-Gardini A. Nonalcoholic steatohepatitis in hepatocarcinoma: new insights about its prognostic role in patients treated with lenvatinib. ESMO Open. 2021;6:100330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 69. | Hiraoka A, Kumada T, Tada T, Tani J, Kariyama K, Fukunishi S, Atsukawa M, Hirooka M, Tsuji K, Ishikawa T, Takaguchi K, Itobayashi E, Tajiri K, Shimada N, Shibata H, Ochi H, Kawata K, Yasuda S, Toyoda H, Aoki T, Tanaka T, Ohama H, Nouso K, Tsutsui A, Nagano T, Itokawa N, Arai T, Okubo T, Imai M, Koizumi Y, Nakamura S, Joko K, Hiasa Y, Kudo M; Real-life Practice Experts for HCC (RELPEC) Study Group and HCC 48 Group (hepatocellular carcinoma experts from 48 clinics in Japan). Efficacy of lenvatinib for unresectable hepatocellular carcinoma based on background liver disease etiology: multi-center retrospective study. Sci Rep. 2021;11:16663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 70. | Welland S, Leyh C, Finkelmeier F, Jefremow A, Shmanko K, Gonzalez-Carmona MA, Kandulski A, Jeliazkova P, Best J, Fründt TW, Djanani A, Pangerl M, Maieron A, Greil R, Fricke C, Sookthai D, Günther R, Schmiderer A, Wege H, Venerito M, Ehmer U, Müller M, Strassburg CP, Weinmann A, Siebler J, Waidmann O, Lange CM, Saborowski A, Vogel A. Real-World Data for Lenvatinib in Hepatocellular Carcinoma (ELEVATOR): A retrospective multicenter study. Liver Cancer. 2022;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 71. | Vogel A, Martinelli E; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org; ESMO Guidelines Committee. Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO Clinical Practice Guidelines. Ann Oncol. 2021;32:801-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 297] [Article Influence: 74.3] [Reference Citation Analysis (1)] |
| 72. | Díaz-González Á, Sanduzzi-Zamparelli M, da Fonseca LG, Di Costanzo GG, Alves R, Iavarone M, Leal C, Sacco R, Matilla AM, Hernández-Guerra M, Aballay Soteras G, Wörns MA, Pinter M, Varela M, Ladekarl M, Chagas AL, Mínguez B, Arenas JI, Granito A, Sánchez-Torrijos Y, Rojas Á, Rodríguez de Lope C, Alvares-da-Silva MR, Pascual S, Rimassa L, Lledó JL, Huertas C, Sangro B, Giannini EG, Delgado M, Vergara M, Perelló C, Lue A, Sala M, Gallego A, Coll S, Hernáez T, Piñero F, Pereira G, França A, Marín J, Anders M, Mello V, Lozano M, Nault JC, Menéndez J, García Juárez I, Bruix J, Reig M. International and multicenter real-world study of sorafenib-treated patients with hepatocellular carcinoma under dialysis. Liver Int. 2020;40:1467-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 73. | Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, Kudo M, Harding JJ, Merle P, Rosmorduc O, Wyrwicz L, Schott E, Choo SP, Kelley RK, Sieghart W, Assenat E, Zaucha R, Furuse J, Abou-Alfa GK, El-Khoueiry AB, Melero I, Begic D, Chen G, Neely J, Wisniewski T, Tschaika M, Sangro B. Nivolumab vs sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022;23:77-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 744] [Article Influence: 186.0] [Reference Citation Analysis (0)] |
| 74. | Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, Breder V, Edeline J, Chao Y, Ogasawara S, Yau T, Garrido M, Chan SL, Knox J, Daniele B, Ebbinghaus SW, Chen E, Siegel AB, Zhu AX, Cheng AL; KEYNOTE-240 investigators. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2020;38:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1365] [Cited by in RCA: 1341] [Article Influence: 268.2] [Reference Citation Analysis (0)] |
| 75. | Siegel AB, Cohen EI, Ocean A, Lehrer D, Goldenberg A, Knox JJ, Chen H, Clark-Garvey S, Weinberg A, Mandeli J, Christos P, Mazumdar M, Popa E, Brown RS Jr, Rafii S, Schwartz JD. Phase II trial evaluating the clinical and biologic effects of bevacizumab in unresectable hepatocellular carcinoma. J Clin Oncol. 2008;26:2992-2998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 395] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 76. | Hughes PE, Caenepeel S, Wu LC. Targeted Therapy and Checkpoint Immunotherapy Combinations for the Treatment of Cancer. Trends Immunol. 2016;37:462-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 217] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 77. | Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Lim HY, Kudo M, Breder VV, Merle P, Kaseb AO, Li D, Verret W, Shao H, Liu J, Li L, Zhu AX, Cheng AL. IMbrave150: Updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J Clin Oncol. 2021;39 Suppl 3:267. [RCA] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 78. | Galle PR, Finn RS, Qin S, Ikeda M, Zhu AX, Kim TY, Kudo M, Breder V, Merle P, Kaseb A, Li D, Mulla S, Verret W, Xu DZ, Hernandez S, Ding B, Liu J, Huang C, Lim HY, Cheng AL, Ducreux M. Patient-reported outcomes with atezolizumab plus bevacizumab vs sorafenib in patients with unresectable hepatocellular carcinoma (IMbrave150): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22:991-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 236] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 79. | Kelley R, Yau T, Cheng A, Kaseb A, Qin A, Zhu AX, Chan S, Sukeepaisarnjaroen W, Breder V, Verset G, Gane E, Borbath I, Gomez Rangel JD, Merle P, Benzaghou FM, Banerjee K, Hazra S, Fawcett J, Rimassa L. Cabozantinib (C) plus atezolizumab (A) vs sorafenib (S) as first-line systemic treatment for advanced hepatocellular carcinoma (aHCC): Results from the randomized phase III COSMIC-312 trial. Ann Oncol. 2022;33:114-116. [RCA] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 60] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 80. | El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492-2502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3278] [Cited by in RCA: 3310] [Article Influence: 413.8] [Reference Citation Analysis (1)] |
| 81. | Yau T, Kang YK, Kim TY, El-Khoueiry AB, Santoro A, Sangro B, Melero I, Kudo M, Hou MM, Matilla A, Tovoli F, Knox JJ, Ruth He A, El-Rayes BF, Acosta-Rivera M, Lim HY, Neely J, Shen Y, Wisniewski T, Anderson J, Hsu C. Efficacy and Safety of Nivolumab Plus Ipilimumab in Patients With Advanced Hepatocellular Carcinoma Previously Treated With Sorafenib: The CheckMate 040 Randomized Clinical Trial. JAMA Oncol. 2020;6:e204564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 908] [Cited by in RCA: 970] [Article Influence: 194.0] [Reference Citation Analysis (0)] |
| 82. | Abou-Alfa G, Chan S, Kudo M, Lau G, Kelley RK, Furuse J, Sukeepaisarnjaroen W, Kang YK, Dao TV, De Toni EN, Rimassa L, Breder VV, Vasilyev A, Heurgue A, Tam V, Mody K, Thungappa SC, He P, Negro A, Sangro B. Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (pts) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. J Clin Oncol. 2022;40 Suppl 4:379. |
| 83. | Kelley RK, Greten TF. Hepatocellular Carcinoma - Origins and Outcomes. N Engl J Med. 2021;385:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 84. | Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, Kudo M, Han KH, Harding JJ, Merle P, Rosmorduc O, Wyrwicz L, Schott E, Choo SP, Kelley RK, Begic D, Chen G, Neely J, Anderson J, Sangro B. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann Oncol. 2019;30 Suppl 5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 433] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 85. | de Castro T, Jochheim LS, Bathon M, Welland S, Scheiner B, Shmanko K, Roessler D, Ben Khaled N, Jeschke M, Ludwig JM, Marquardt JU, Weinmann A, Pinter M, Lange CM, Vogel A, Saborowski A. Atezolizumab and bevacizumab in patients with advanced hepatocellular carcinoma with impaired liver function and prior systemic therapy: a real-world experience. Ther Adv Med Oncol. 2022;14:17588359221080298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 86. | Sangro B, Melero I, Wadhawan S, Finn RS, Abou-Alfa GK, Cheng AL, Yau T, Furuse J, Park JW, Boyd Z, Tang HT, Shen Y, Tschaika M, Neely J, El-Khoueiry A. Association of inflammatory biomarkers with clinical outcomes in nivolumab-treated patients with advanced hepatocellular carcinoma. J Hepatol. 2020;73:1460-1469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 309] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 87. | Sia D, Jiao Y, Martinez-Quetglas I, Kuchuk O, Villacorta-Martin C, Castro de Moura M, Putra J, Camprecios G, Bassaganyas L, Akers N, Losic B, Waxman S, Thung SN, Mazzaferro V, Esteller M, Friedman SL, Schwartz M, Villanueva A, Llovet JM. Identification of an Immune-specific Class of Hepatocellular Carcinoma, Based on Molecular Features. Gastroenterology. 2017;153:812-826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 690] [Cited by in RCA: 663] [Article Influence: 82.9] [Reference Citation Analysis (0)] |
| 88. | Scheiner B, Pomej K, Kirstein MM, Hucke F, Finkelmeier F, Waidmann O, Himmelsbach V, Schulze K, von Felden J, Fründt TW, Stadler M, Heinzl H, Shmanko K, Spahn S, Radu P, Siebenhüner AR, Mertens JC, Rahbari NN, Kütting F, Waldschmidt DT, Ebert MP, Teufel A, De Dosso S, Pinato DJ, Pressiani T, Meischl T, Balcar L, Müller C, Mandorfer M, Reiberger T, Trauner M, Personeni N, Rimassa L, Bitzer M, Trojan J, Weinmann A, Wege H, Dufour JF, Peck-Radosavljevic M, Vogel A, Pinter M. Prognosis of patients with hepatocellular carcinoma treated with immunotherapy - development and validation of the CRAFITY score. J Hepatol. 2022;76:353-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 187] [Article Influence: 62.3] [Reference Citation Analysis (0)] |