Published online Jan 28, 2021. doi: 10.3748/wjg.v27.i4.371
Peer-review started: November 23, 2020
First decision: December 8, 2020
Revised: December 16, 2020
Accepted: January 8, 2021
Article in press: January 8, 2021
Published online: January 28, 2021
Processing time: 62 Days and 20.2 Hours
Duplication of the extrahepatic bile duct (DCBD) is an extremely rare congenital anomaly of the biliary system. There are five types of DCBD according to the latest classification. Among them, Type V is characterized by single drainage of the extrahepatic bile ducts. Reports on DCBD Type V are scarce.
A 77-year-old woman presented with recurrent epigastric pain but without fever or chills. Computed tomography revealed a dilated common bile duct (CBD) that harboured multiple choledocholithiasis. Endoscopic retrograde cholangio-pancreatography (ERCP) was performed, and the stones were extracted using a Dormia basket. She was discharged without any complications; however, she visited the emergency department a day after she was discharged due to epigastric pain and fever. Laboratory findings were suggestive of cholestasis. After urgent ERCP for stone removal, magnetic resonance cholangiopancrea-tography was performed to evaluate remnant choledocholithiasis. Magnetic resonance cholangiopancreatography revealed a DCBD Type Va and remnant choledocholithiasis in the right CBD. Both CBDs were accessed, and the stones were cleared successfully during a subsequent ERCP.
In this article, we report an extremely rare case of DCBD manifesting as recurrent pyogenic cholangitis. This case highlights the importance of recognizing DCBD because stones in the unrecognized bile duct could make the patient’s prognosis critical.
Core Tip: Double common bile duct (DCBD) is an extremely rare congenital biliary tract anomaly. We present herein, a rare case of DCBD manifesting as a recurrent pyogenic cholangitis. It is substantial to establish complete stone clearance during endoscopic retrograde cholangiopancreatography because residual stone is a probable risk factor for recurrent cholangitis. However, DCBD, an extremely rare anomaly, can completely mask the presence of remnant bile duct stones for biliary endoscopists. In this case, recurrent cholangitis, which occurred immediately after bile duct stone clearance was a clue to recognize DCBD. Although this is a rare condition, our case highlights the importance of recognizing DCBD because stones in the unrecognized bile duct could make the patient’s prognosis critical.
- Citation: Hwang JS, Ko SW. Duplication of the common bile duct manifesting as recurrent pyogenic cholangitis: A case report. World J Gastroenterol 2021; 27(4): 371-376
- URL: https://www.wjgnet.com/1007-9327/full/v27/i4/371.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i4.371
Double common bile duct (DCBD) is an extremely rare congenital anomaly of the biliary system. Morphological classification of this anomaly was modified by Choi et al[1] in 2007 by adding a Type V, which is characterized by single drainage of the extrahepatic bile ducts. Only 7 cases of DCBD Type V have been reported so far. Herein, we report a rare case of DCBD Type V in an elderly woman who presented with recurrent pyogenic cholangitis.
A 77-year-old woman presented to the outpatient department of our hospital complaining of recurrent epigastric pain.
Patient’s symptoms started a month ago with recurrent episodes, with no history of fever, chills, or vomiting.
The patient had a history of laparoscopic cholecystectomy for cholelithiasis 2 years earlier at another hospital. She had undergone endoscopic retrograde cholan-giopancreatography (ERCP) twice for choledocholithiasis before undergoing cholecystectomy.
The patient did not have a history of drinking or smoking. There was no remarkable family medical history.
Physical examination did not reveal tenderness or signs of peritoneal irrigation, and the bowel sounds were normal. At the outpatient clinic, her temperature was 36.7 °C, pulse rate was 70 beats/min, and blood pressure was 122/82 mm Hg.
Blood analysis showed normal complete blood cell count, liver function test and C-reactive protein.
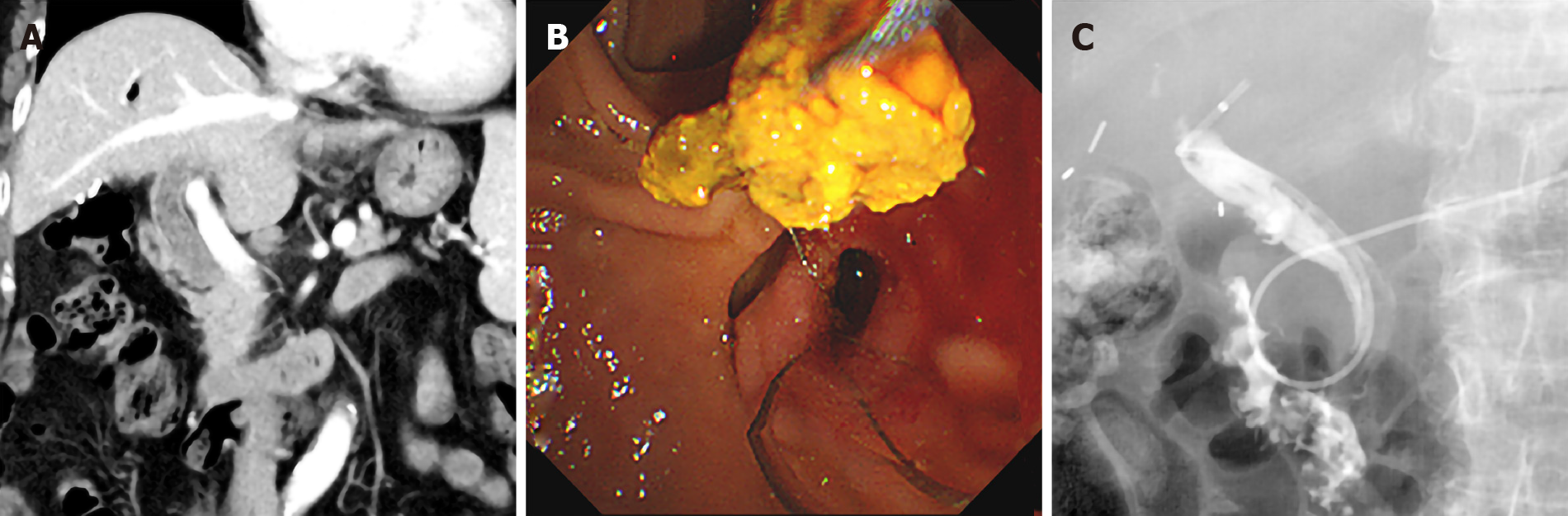
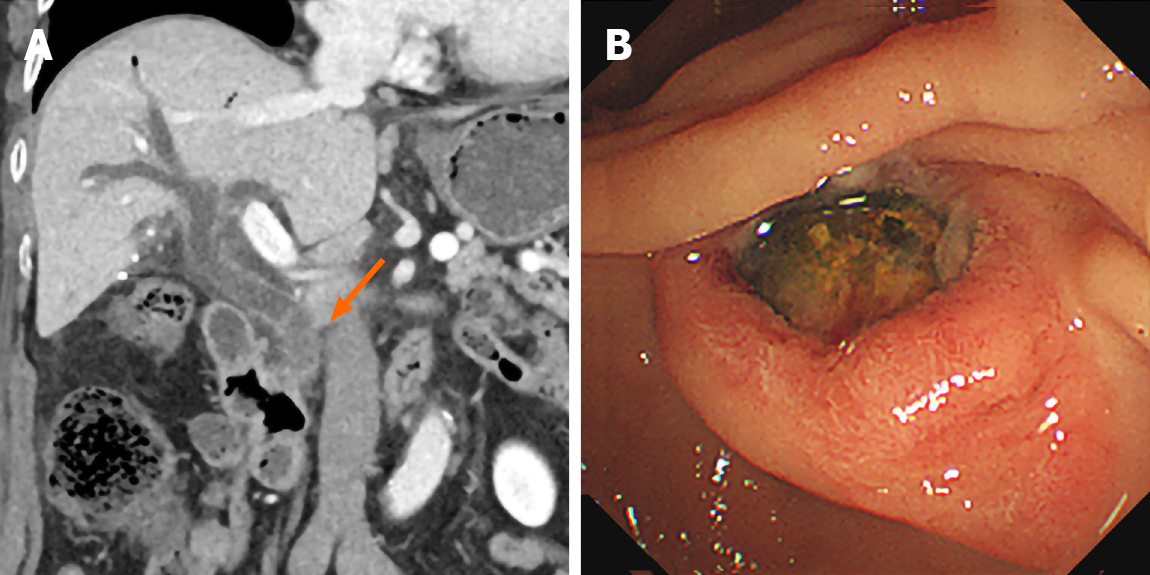
Computed tomography (CT) imaging revealed a dilated CBD that harboured multiple choledocholithiasis (Figure 1A). After admission, ERCP was subsequently performed, and the stones were extracted using a Dormia basket (MTW Endoskopie, Wesel, Germany) (Figure 1B) after endoscopic papillary balloon dilatation by a CRETM balloon dilatation catheters (Boston Scientific Corporation, Natick, MA, United States). A 5 Fr endoscopic nasobiliary drainage (ENBD) catheter (ENBD-5, Cook Medical, Bloomington, IN, United States) was inserted at the end of the procedure. A day after the ERCP, tubography via the ENBD catheter was performed to confirm the presence of residual stones in the bile duct. However, no definite filling defects were observed on tubography (Figure 1C). The patient was discharged without any complications of ERCP. A day after discharge, she visited the emergency department with complaints of severe epigastric pain and fever. Her temperature was 38.2 °C, pulse rate was 79 beats/min, and blood pressure was 149/85 mm Hg. Laboratory findings were suggestive of cholestasis [aspartate aminotransferase, 210 U/L (normal: 0–35 U/L); alanine aminotransferase, 134 U/L (0-35); alkaline phosphatase, 201 U/L (30-120); gamma glutamyl transferase, 184 U/L (9-64); total bilirubin, 2.77 mg/dL (0.3-1.2); direct bilirubin, 1.32 mg/dL (0-0.2); and C-reactive protein 6.91 mg/dL]. A CT scan demonstrated another dilated extrahepatic bile duct draining the right lobe of the liver, which also contained stones in the distal portion (Figure 2A). An urgent ERCP was performed as the stones were impacted at the ampulla (Figure 2B), and the stones with pus were retrieved using a balloon catheter (Escort II® Double Lumen Extraction Balloon, Cook Medical, Bloomington, IN, United States). A 10 Fr, 5 cm endoscopic retrograde biliary drainage tube (Cotton-Leung Biliary Stent, Cook Medical, Bloomington, IN, United States) was then placed in the CBD.
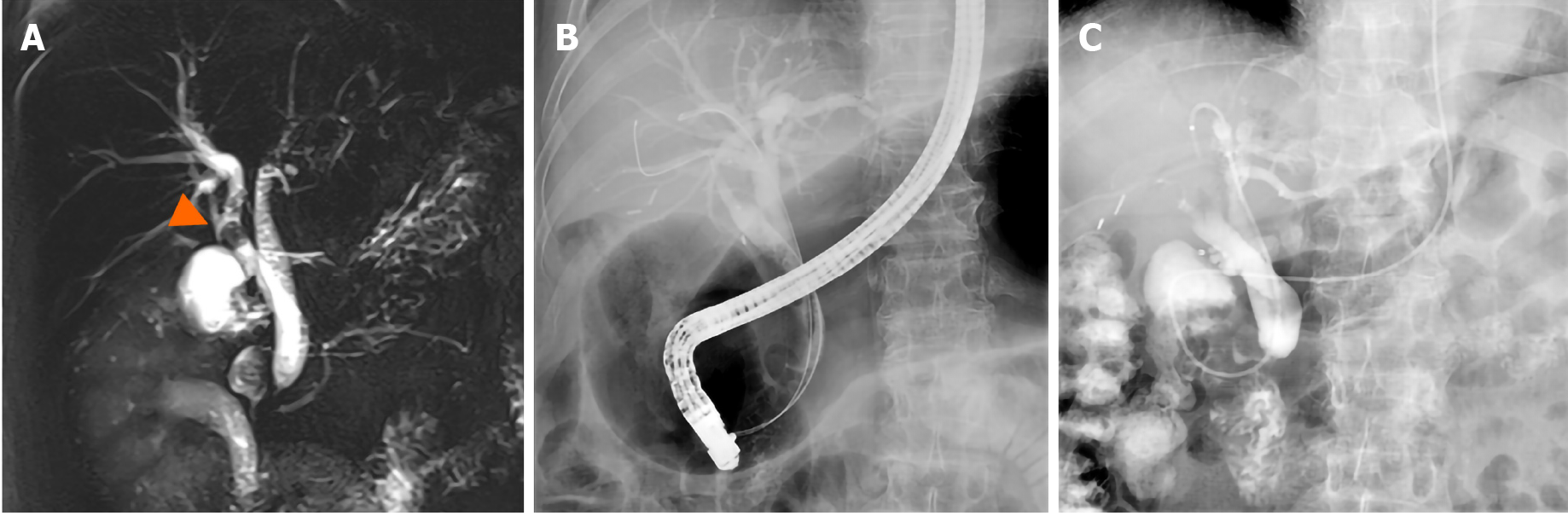
Magnetic resonance cholangiopancreatography (MRCP) was performed to evaluate the delicate structures of the CBD and to check for any remnant stones. MRCP revealed DCBD independently draining the left and right lobes of the liver, that created a short segment intrapancreatic CBD (Figure 3A) without a communicating channel, that was consistent with the DCBD Type Va as classified by Choi et al[1,2]. Residual choledocholithiasis was also noted in the right CBD. There was no evidence of anomalous union of the pancreaticobiliary duct on MRCP.
The final diagnosis was DCBD that manifested as recurrent pyogenic cholangitis due to the residual choledocholithiasis.
To remove the residual stones, subsequent ERCP was performed, and both CBDs were cannulated successfully under fluoroscopic guidance (Figure 3B). After stone removal, two ENBD tubes were placed separately in both bile ducts to achieve sufficient biliary drainage. Tubography was performed a day after ERCP and did not reveal any definite filling defects suggestive of residual stones in either CBD (Figure 3C).
The patient was discharged after resolution of cholangitis, and is being followed up for 9 mo after the procedure without recurrence of cholangitis.
DCBD is an extremely rare congenital anomaly of the biliary system. Since Vesarius first reported it in 1543, only 24 cases had been reported in the western literature until 1986[3]. However, cases of DCBD are reported more often in the eastern literature. A total of 47 patients reported in the Japanese literature were reviewed by Yamashita et al[4] in 2002; furthermore, Chen et al[5], reported 24 Chinese cases in 2014.
The mechanism of this biliary system anomaly is considered to be due to an abnormality during embryogenesis. The presence of two bile ducts is normal anatomically during early human embryogenesis[6]. However, failure of the second bile duct to regress results in the persistence of an accessory extrahepatic bile duct[1].
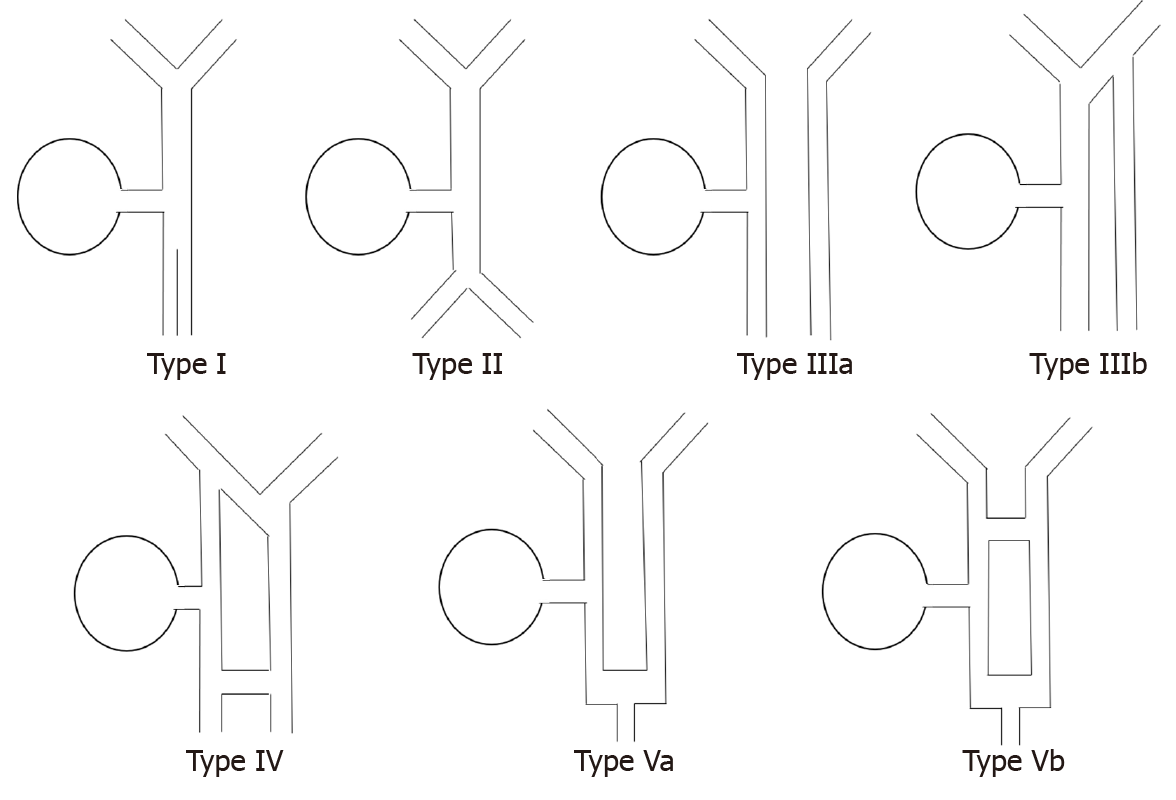
Morphological classification of this anomaly was first suggested by Goor et al[7]. Goor’s classification was revised by Saito et al[2], and recently Choi et al[1], modified it by adding a Type V, which is characterized by single drainage of the extrahepatic bile ducts. According to the classification by Choi et al[1], the types of DCBD are as follows: Type I, CBD divided by septum; Type II, CBD bifurcates at the distal end and drains into each opening independently; Type III, duplicated biliary drainage with (Type IIIa) or without (Type IIIb) intrahepatic communicating channels; Type IV, duplicated biliary drainage with one or more communicating channels; Type V, duplicated extrahepatic bile duct rejoined as a single drainage with (Type Va) or without (Type Vb) communicating channels (Figure 4). Our case corresponds to Type Va in the classification by Choi et al[1].
Very few cases of DCBD Type V have been reported. Ever since Choi et al[1] reported the first case of DCBD Type V, only 7 cases have been reported[8]. To the best of our knowledge, this patient is the eighth case of DCBD Type V to be reported. Among the previously reported cases, 5 cases were diagnosed with choledocholithiasis[3,8-11]. There were 2 cases[9,11] that had choledocholithiasis in both extrahepatic bile ducts; one underwent surgery as the stones were not completely removed using ERCP[11], and another case successfully underwent stone extraction in one session of ERCP[9]. In our case, the patient presented with recurrent pyogenic cholangitis because a DCBD was not initially suspected due to the rarity of the anomaly. Therefore, two sessions of ERCP were needed to remove all choledochal stones in this case.
MRCP is the examination of choice to evaluate the anatomy of the biliary tree and its variations[12]. It has several advantages over ERCP such as (1) non-invasiveness; (2) no radiation hazard; and (3) less operator dependence[13]. It also has advantages over CT; it does not require intravenous contrast media and provides comprehensive anatomy of the biliary tract in a single image due to its capability to acquire images in any desired plane[14]. As very few biliary endoscopists and radiologists have ever encountered DCBD even in high-volume centres[9], in this case, the right CBD was mistaken for a residual cystic duct on initial CT because the patient had already undergone cholecystectomy. However, the precise anatomy of CBD was clarified through MRCP, and this extremely rare congenital anomaly could be diagnosed. Therefore, MRCP should always be considered in patients with suspected biliary tract anomalies.
Despite the extremely rare nature of this condition, it is crucial to consider the possibility of this congenital anomaly. Goor et al[7] reported a case of inadvertent transection of the CBD during laparoscopic cholecystectomy because of the failure to recognize the presence of DCBD. It is substantial to establish complete stone clearance during ERCP, because residual stone is a probable risk factor for recurrent cholangitis[15]. Although we performed ENBD to confirm the residual stones, the stones in the ancillary bile duct were completely concealed because only one of the two CBDs was assessed during the index procedure. It may be quite challenging to access both bile ducts in a DCBD Type V because it shares a short segment of the draining duct. In a case reported by Kim et al[11], stones in the right CBD were extracted surgically owing to inadequate access to the right duct. Although only one duct was accessible initially in our case, we were able to successfully cannulate both bile ducts after recognizing DCBD.
We herein report an extremely rare case of duplication of the extrahepatic bile duct Type V associated with recurrent cholangitis. Although this condition is rare, it is very crucial for biliary endoscopists to be aware of this disease because choledocholithiasis in the unrecognized ancillary bile duct can significantly affect the prognosis of patients.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lin H S-Editor: Zhang L L-Editor: A P-Editor: Ma YJ
| 1. | Choi E, Byun JH, Park BJ, Lee MG. Duplication of the extrahepatic bile duct with anomalous union of the pancreaticobiliary ductal system revealed by MR cholangiopancreatography. Br J Radiol. 2007;80:e150-e154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Saito N, Nakano A, Arase M, Hiraoka T. [A case of duplication of the common bile duct with anomaly of the intrahepatic bile duct]. Nihon Geka Gakkai Zasshi. 1988;89:1296-1301. [PubMed] |
| 3. | Arora A, Sureka B, Kasana V, Patidar Y, Bansal K. Common bile duct duplication: the more the murkier. Saudi J Gastroenterol. 2015;21:51-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Yamashita K, Oka Y, Urakami A, Iwamoto S, Tsunoda T, Eto T. Double common bile duct: a case report and a review of the Japanese literature. Surgery. 2002;131:676-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Chen G, Wang H, Zhang L, Li Z, Bie P. Double common bile duct with choledochal cyst and cholelithiasis: report of a case. Surg Today. 2014;44:778-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Joo YE, Kim HS, Choi SK, Rew JS, Cho CK, Kim SJ. Congenital anomalous connection between the left intrahepatic bile duct and the stomach. J Gastroenterol. 2002;37:961-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Goor DA, Ebert PA. Anomalies of the biliary tree. Report of a repair of an accessory bile duct and review of the literature. Arch Surg. 1972;104:302-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 98] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 8. | Fan X, He L, Khadaroo PA, Zhou D, Lin H. Duplication of the extrahepatic bile duct: A case report and review of the literatures. Medicine (Baltimore). 2018;97:e9953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Chin JL, Sengupta S, Morrin MM, Murray FE, Patchett SE. Common bile duct duplication: double bile ducts, double trouble. Gastrointest Endosc. 2017;85:855-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Gupta V, Chandra A. Duplication of the extrahepatic bile duct. Congenit Anom (Kyoto). 2012;52:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Kim SW, Park DH, Shin HC, Kim IY, Park SH, Jung EJ, Kim CH. Duplication of the extrahepatic bile duct in association with choledocholithiasis as depicted by MDCT. Korean J Radiol. 2008;9:550-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Sureka B, Bansal K, Patidar Y, Arora A. Magnetic resonance cholangiographic evaluation of intrahepatic and extrahepatic bile duct variations. Indian J Radiol Imaging. 2016;26:22-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 13. | Hekimoglu K, Ustundag Y, Dusak A, Erdem Z, Karademir B, Aydemir S, Gundogdu S. MRCP vs. ERCP in the evaluation of biliary pathologies: review of current literature. J Dig Dis. 2008;9:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Petrescu I, Bratu AM, Petrescu S, Popa BV, Cristian D, Burcos T. CT vs. MRCP in choledocholithiasis jaundice. J Med Life. 2015;8:226-231. [PubMed] |
| 15. | Endo R, Satoh A, Tanaka Y, Shimoda F, Suzuki K, Takahashi K, Okata H, Hiramoto K, Kimura O, Asonuma S, Umemura K, Shimosegawa T. Saline Solution Irrigation of the Bile Duct after Stone Removal Reduces the Recurrence of Common Bile Duct Stones. Tohoku J Exp Med. 2020;250:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |