Published online Sep 28, 2019. doi: 10.3748/wjg.v25.i36.5423
Peer-review started: June 10, 2019
First decision: July 21, 2019
Revised: August 5, 2019
Accepted: August 19, 2019
Article in press: August 19, 2019
Published online: September 28, 2019
Processing time: 112 Days and 18.4 Hours
The impact of a chronic disease such as inflammatory bowel disease (IBD) on sexual functioning and body image can significantly impair the quality of life of patients. This review considers the sexual and fertility aspects of IBD patients and their daily management. Modern IBD healthcare management should include appropriate communication on sexuality and consider psychological, physiological, and biological issues. Patients with IBD have less children than the general population, and voluntary childlessness is frequent. The most influential factors reported by IBD patients who experience fertility alteration are psychological and surgery-related problems. Pregnancy is a major concern for patients, and any pregnancy for IBD patients should be closely followed-up to keep the chronic disease in a quiescent state. Preconceptional consultation is of great help.
Core tip: The impact of inflammatory bowel diseases on sexual and fertility is of major concern for inflammatory bowel disease (IBD) patients. Quality of life of IBD patients can be impaired and their management remains challenging. Communication and counseling are crucial aspects in the management of all IBD patients and should be implemented in IBD centers.
- Citation: Leenhardt R, Rivière P, Papazian P, Nion-Larmurier I, Girard G, Laharie D, Marteau P. Sexual health and fertility for individuals with inflammatory bowel disease. World J Gastroenterol 2019; 25(36): 5423-5433
- URL: https://www.wjgnet.com/1007-9327/full/v25/i36/5423.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i36.5423
Crohn’s disease (CD) and ulcerative colitis (UC) have a high burden on a patient’s quality of life (QoL)[1]. QoL and patient-related outcomes are the treatment targets for managing patients who are suffering from inflammatory bowel disease (IBD)[2]. Sexual health is a main determinant of QoL and is negatively impacted in patients with IBD[3,4]. IBD patients expect more open listening and better information from care providers[5]. Fertility can be affected by IBD[6], and voluntary childlessness is more frequent in IBD patients than in the general population, sometimes because of improper medical knowledge and/or communication[7].
In this review, we summarize the knowledge on the impact of IBD on sexual health and fertility and what gastroenterologists should do to better meet patients’ expectations regarding these often-neglected topics.
An electronic search of the literature was conducted using MEDLINE (PubMed). The search was restricted to English language. The search strategy used the following MeSH and text words: “Sexual dysfunction”, “Inflammatory Bowel disease”, “Fertility”, “Psychological”, “Crohn’s Disease” and “Ulcerative colitis”.
Sexual health is defined by the World Health Organization as “a state of physical, emotional, mental and social wellbeing in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity”[8]. Sexual health has five dimensions: physical, emotional, social, mental, and spiritual. Along with body image, it is an important aspect of psychosocial functioning and has a significant impact on overall QoL[9].
Assessing sexual function is a quantitative approach toward sexual health that considers the domains of desire, arousal, orgasm and satisfaction, erectile function for men, and lubrication and pain for women. Specific questionnaires on sexual function have been designed and validated in healthy men and women and in diseased populations. The most used auto-questionnaires are the Female Sexual Function Index (FSFI) for women[10] and the International Index Erectile Function (IIEF) for men[11]. Within these questionnaires, sexual dysfunction has been defined as an FSFI score below 26.55 and IIEF score below 42.9. There is no specific tool for IBD patients, but some QoL questionnaires designed for these patients include questions on sexual health[12-14].
Body image and intimacy are some of the major concerns of IBD patients but rarely are spontaneously expressed[15]. In the IMPACT study, a wide-ranging European study including 4990 IBD patients recruited by patients’ associations, 40% reported that their disease prevented them from pursuing intimate relationships[1]. Indeed, sexual dysfunction rates are higher in patients with IBD than in the general population[16]; it is indeed by reported 45%-60% of IBD women and 15-25% of IBD men[3,16,17], compared with 30% of women and 5% of men in the general population[16]. Around 40% of IBD men suffer from erectile dysfunction versus 15% of men of the same age in the general population[3,16,18]. A study based on the Danish medical register and that included 31498 IBD and 314980 non-IBD men showed that erectile dysfunction treatments were more often used by IBD patients [12% vs 10%, HR 1.22 (1.18-1.27)][18]. In IBD men, a reduction of sexual desire is also more frequent than in the general population[16]. Body image is lower in 70% of patients, especially in women who have had a surgery[19]. The sexual activity rate of IBD patients appears similar to healthy individuals, indicating that IBD patients engage in sexual relationships but that their satisfaction is below that of the general population[16,21].
Receptive anal sexuality (RAS) is not an exceptional practice but is still a taboo topic in health care. General population studies in North America and Europe show that around 10% of women engage in frequent RAS and 35% have experienced it[22,23]. Around 5%-15% of men report regular RAS and 10%-45% lifetime RAS[23,24]. The consequences of RAS in IBD patients when it comes to rectal symptoms and lesions, susceptibility of inflamed mucosa to sexually transmitted infectious agents, anal dysplasia, and anal carcinoma risks have been poorly studied[25]. Anal carcinoma prevalence is increased in patients with anoperineal CD[26] and is associated with human papilloma virus (HPV) infection and immunosuppressive therapy[27]. Currently, there are no guidelines on screening for sexually transmitted infections or proposing HPV vaccinations for IBD patients[28]. Dibley et al[29] showed that IBD men having sexual relationships with other men are reluctant to disclose their sexual practices because of fear of medical judgment. However, patients would benefit from an open discussion with medical staff and information about their ability to engage in RAS.
Sexual health is multidimensional. In patients with IBD, sexual dysfunction in IBD is associated with anxiety, depression, impaired QoL, and fatigue but not with disease activity[3,16-18,30,31]. In a study by Bel et al[3], the univariate association of IBD activity on sexual function was totally explained by depression. This is consistent with other observations showing that in IBD patients psychosocial factors are more significant predictors of overall QoL than disease activity[9,32]. Depression and anxiety are frequent psychological comorbidities in IBD and are the major drivers of sexual dysfunction[3,16,17]. Depression is found in as many as 20%-30% of IBD patients in remission and anxiety in 10%-30%[32]. Psychological burden may be not only a cause, but also aggravated by sexual dysfunction.
Little data exist on the impact of surgery on sexual function in IBD men. In a French study on 166 IBD men, a history of abdominal surgery was an independent predictor of erectile dysfunction with an odds ratio of 2.24 (95% confidence interval 1.04-4.92, P = 0.04)[16]. Studies on the impact of ileal pouch anal anastomosis (IPAA) in UC patients provided conflicting results. Postoperative screening found the frequency of sexual dysfunction in men after IPAA as varying from 4%-30%[33,34]. Prospective studies comparing pre- and postoperative scores showed an improvement in the overall QoL and sexual function[35,36]. Prospective and follow-up data are needed to evaluate the risk of erectile dysfunction and retrograde ejaculation after pelvic surgery and abdominal surgery in IBD men. For the moment, the ECCO guidelines recommend discussing sperm banking with the patient before IPAA[37]. In women, surgery has been found to be associated with a poorer body image[19] and dyspareunia[38].
In the literature, the majority of IBD drugs appear to have very limited influence on sexual dysfunction whereas other medications like psychotropic drugs are known to induce sexual dysfunction[39,40]. However, the statistical power of previous studies is limited, and rare side effects could not be properly evaluated. In a study by Marín et al[17] on 202 IBD women, corticosteroids were independently associated with sexual dysfunction, which may be because of their impact on body image. Hypogonadism and decreased levels of testosterone have also been shown in IBD men[41] and could be responsible of sexual dysfunction. Methotrexate has been reported to be associated with erectile dysfunction in a few cas reports with a very low level of evidence[42,43]. Concerning the use of biological agents, the study by Marín et al[17] showed its use was an independent factor of sexual dysfunction on 153 IBD men. However, no data on sexual dysfunction were reported in the systematic literature review by Semet et al[44] (Table 1).
| Factors associated | Factors not associated |
| Anxiety | Disease activity |
| Depression | Immunosuppressants |
| Impaired overall quality of life | Biological therapies |
| Fatigue | |
| Corticosteroids and psychotropic drugs |
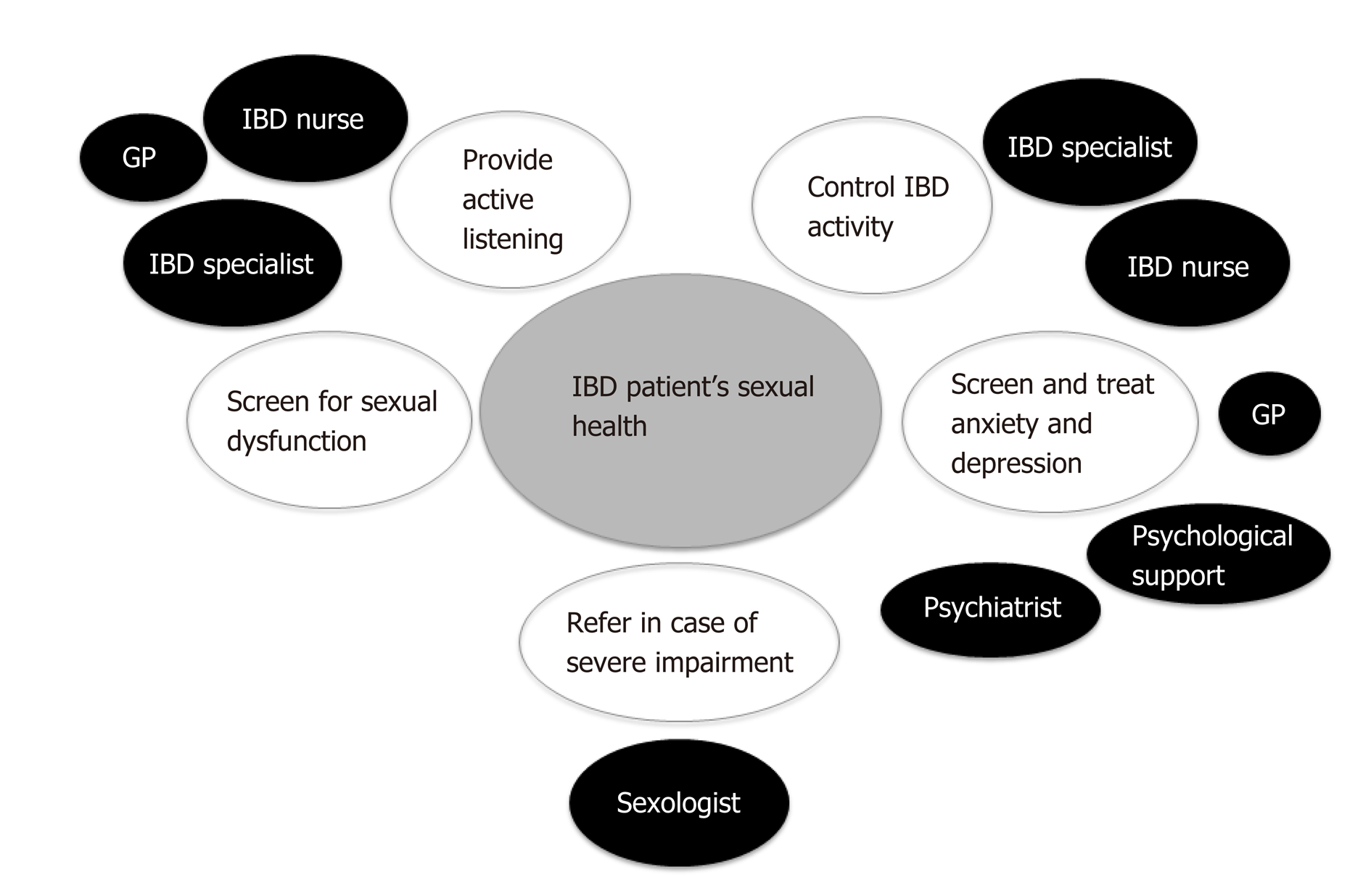
The management of sexual dysfunction is a complex bio-psycho-social process (Figure 1). Most IBD patients expect their gastroenterologist to provide information about the disease of their impact on their sexuality as early as diagnosis[17] and to ask them regularly about their sexual health[16]. However, it seems that this topic is rarely addressed in daily practice. One study found that only 8% of patients had been asked about their sexual health in the past[29]. Among 69 gastroenterologists participating in a recent French survey, only 16% addressed the topic, even though 93% considered it would be a good thing to do so[45]. The main reason not to tackle the subject was the feeling of a lack of knowledge regarding sexual dysfunction management (45%), reluctance to shame patients (29%), discomfort from the doctor (19%) and, finally, lack of time (9%). Proctologic surgeons addressed the subject more often (55% vs 9%, P < 0.001).
The first step would be to screen patients for impaired sexual function. Questionnaires such as the IIEF and FSFI are rarely used in daily practice. A specific index for IBD patients could be an interesting tool and should also evaluate psychological comorbidities such as depression and anxiety.
The benefit of psychoeducational sessions on sexual health has never been evaluated in IBD patients. However, this approach has proven to be effective in patients suffering from irritable bowel syndrome or those who have been treated for a nongastroenterological disease[46]. Regarding medications, a randomized controlled study in patients with erectile dysfunction after IPAA showed a 79% response rate for the patients treated with sildenafil vs 17% for those in the placebo group[47].
Referral to a sexologist should be considered in several situations. The first is when a problem is discovered by the screening questions and when the gastroenterologist is reluctant to tackle the subject. Patients should also be referred in the case of the failure of a first-line management (to a sexologist helping to inform and prescribe erectile dysfunction medication), in persistent sexual dysfunction, and/or couple suffering. The referral process represents a strong signal for the patient that his/her suffering has been heard.
Fertility is the capacity to produce a child[48], differing from fecundability, which is the probability of pregnancy per month with unprotected intercourse. Approximately 80% of couples will conceive in the first 6 months of attempting pregnancy[49]. Infertility is defined as the failure to achieve a pregnancy after 12 months of unprotected intercourse. Table 2 shows the main causes of infertility in the general population and a few IBD-specific situations. What the gastroenterologist should do in this context is summarized in Table 3. Pregnancy outcomes in the general population compared with IBD patients are shown in Table 4. IBD typically affects young patients during their reproductive years. Thus, fertility is a major concern for IBD patients. Patients with quiescent IBD have similar fertility rates compared with the general population. However, because of voluntary childlessness, IBD patients have fewer children than the general population[7]. Apprehension about fertility, potentially adverse pregnancy outcomes, risk of IBD in the offspring, and medication safety may be the causes for the fear and doubts during preconception. Moreover, in cases of IBD, patients’ perceptions about fertility are often associated with negative views[50].
| Women | Men |
| General risk factors: | |
| Age: High fertility rate around 25 yr, then gradually reduce and more quickly after 35 yr | General risk factors: |
| High age | |
| Tobacco | |
| Addiction and lead poisoning | |
| Tobacco | |
| Ovulation disorders: Obesity or thinness/hyperprolactinaemia/polycystic ovary syndrome/hypothalamic amenorrhoea, etc | Oligoasthenoteratospermia (the most common cause for male infertility) |
| Sulfasalazine | |
| Azoospermia (hypogonadism induced or blockages) | |
| Diseases with chronic inflammation | |
| Sulfasalazine | |
| Mechanical obstruction: | |
| Tubal obstruction (frequent cause after a salpingitis or endometriosis) | |
| Ileal pouch-anal anastomosis by laparotomy, Crohn’s disease with severe pelvic inflammation with or without prior surgery | |
| Uterine malformation, uterine synechiae or endometriosis | |
| Cervical stenosis |
| Consider | Causes/mechanisms | What the gastroenterologist should do |
| Voluntary childlessness | Apprehension about fertility/potentially adverse pregnancy outcomes/medication safety | Information and accurate counseling on medications/risk of transmission/pregnancy outcomes |
| Correcting misconceptions | ||
| Misconceptions | Provide preconceptual cares | |
| Risk of IBD in the offspring | Information about genetics | |
| Involuntary childlessness | Sexual dysfunction | Psychological support |
| Refer to sexologist | ||
| Sildenafil therapy for post surgery erectile dysfunction | ||
| Surgery | Informations before surgery | |
| IPAA laparoscopy access | ||
| Disease activity | Control disease activity | |
| Psychological factors | Counseling and psychological support | |
| Medications | Stop sulfasalazine and switch to mesalazine | |
| Stop methotrexate | ||
| Sperm banking before surgery |
| General population | IBD patients | |
| Infertility (1 yr) | 10%-20% | Idem except after IPAA with laparotomy access |
| Spontaneous miscarriage of 1st quarter | 15% | Idem |
| Ectopic pregnancy | 2% | Idem except in case of prior surgery[80] |
| Stillbirth | 0.1% | Idem |
| Prematurity | 7% | 10% |
| Malformations | 2.7% | Idem |
| Risk of developing IBD for the offspring | 0.5% | UC 2%-CD 5% IBD both parents: 30% |
| Pregnancy with no events | 75% | Idem |
Many series assessed the impact of disease activity on fertility in females and males, and there is no evidence that UC or inactive CD affect fertility[51]. Tavernier et al[6] showed that the infertility rates are similar between women with quiescent IBD and no prior pelvic surgery (5%-14%) and the general population. Nevertheless, in cases of active disease, peritoneal inflammation might be responsible for intra-abdominal adherences and hence a decrease in the fertility rate. Moreover, decreased libido, dyspareunia, chronic abdominal pain, and anxiety/depression disorders can lead to increased infertility for IBD patients[30].
The disease activity at conception or during pregnancy is considered one of the most significant risk factors for adverse pregnancy outcomes[52]. Moreover, women affected by IBD and who are considering pregnancy often stop their treatment without informing their doctors[53]. Studies from the Netherlands have demonstrated that a systematized preadvisory information program[54] improved the birth rate and reduced the risk of relapse of IBD during pregnancy. These positive effects can be attributed to the beneficial impacts of preconceptual care on pregnancy planification during remission, to the IBD treatment adherence, and to smoking cessation during pregnancy. Thus, counseling should be considered a crucial aspect in the management of all IBD patients and should be implemented in IBD centers.
Most medical treatments for IBD have no effect on the patient’s ability to conceive[55]. Sulfasalazine is an exception, though, because it increases the risk of subfertility in men by altering the spermogram[44]; it reduces sperm motility and increases the proportion of abnormal forms[56]. Birnie et al[57] performed a sperm analysis in 21 patients receiving sulfasalazine treatment for IBD and reported that 86% and 72% of the patients had abnormal semen and oligospermia, respectively. A switch to 5-aminosalicylic acid (mesalazine) generally restores fertility and spermogram anomalies. There is still some debate regarding the effects of thiopurines on fertility. Dejaco et al[58] showed that the sperm quality of 18 IBD patients was not altered after 3 months of using azathioprine. In a cohort of 40 IBD men[59], thiopurines did not decrease sperm quality but was sometimes associated with the impairment of sperm motility. Methotrexate (MTX) can be responsible for oligospermia and is reversible after stopping usage; this drug is contraindicated for both women and men because it is embryotoxic[60]. Corticosteroids and cyclosporine seem to have no effects on fertility. However, there is some debate about the effect of infliximab on fertility. In studying a small series of 10 IBD patients, Mahadevan et al[61] reported a trend toward decreased sperm motility with infliximab therapy. However, Villiger et al[62] reported that the sperm quality of 26 men treated with infliximab for spondylarthritis was similar to that of healthy controls. Data on the impact of adalimumab, vedolizumab, and ustekinumab on human fertility are insufficient.
Surgery-related problems can alter fertility, and patients should be informed prior to all surgical procedures. A meta-analysis showed that IPAA increases the risk of infertility in women with UC by approximately threefold[63]. The mechanisms likely responsible for this important increase of the subfertility rate have been related to postsurgical abdominal adhesions and also to tubal obstructions[64]. However, Beyer-Berjot et al[65] demonstrated that infertility rates after laparoscopic IPAA surgery appears to be lower than after open surgery.
In CD, perineal disease and fallopian tube inflammation may occur and, in rare cases, may induce a reduction in the fertility rate. A systematic review by Tavernier et al[6] showed a decrease in Crohn’s women fertility rates between 17% and 44% when compared with controls; however, most of these studies did not distinguish voluntary childlessness from involuntary infertility. Thus, regarding involuntary infertility, women with CD tend to have similar rates compared with control patients. Concerning women with UC, most studies have not found any difference in the fertility rates compared with the general population[66,67].
A few studies have assessed the anti-Mullerian hormone (AMH), which is considered an accurate hormonal marker of ovarian reserve. In a retrospective case control study including 50 women with CD, Fréour et al[68] showed that women older than 30 years of age and with a colonic location could present an accelerated alteration of the ovarian reserve when compared with control healthy women. The authors hypothesized that the proximity between the colon and the ovaries may be responsible for the higher level of chronic inflammation and, thus, an alteration of the ovarian reserve. Another case control study showed that 35 patients with CD had significantly lower levels of serum AMH than the matched controls and that disease activity was inversely correlated to the AMH levels[69].
The medical literature has shown that advanced age, consumption of tobacco and alcohol, and psychological stress are risk factors for male infertility[70]. Moreover, a large meta-analysis from Sermondade et al[71] indicated that there was a correlation between body mass index and the prevalence of azoospermia or oligozoospermia. However, there is some controversy about the impact of IBD in men’s fertility. Two population-based studies on men with UC did not show any reduction in fertility rate, whereas a recent medical literature overview indicated that active inflammation, poor nutrition, alcohol use, smoking, medications, and surgery may cause infertility in men with IBD[72]. There is no evidence of any impact of IBD surgery on male fertility, except from the debated risk of erectile dysfunction (see the section titled “Associated factors to sexual dysfunction”).
Voluntary childlessness and psychological factors: Voluntary childlessness is more frequent in IBD patients than in the general population; it was estimated in two studies in the United States and Great Britain to be at 14% to 18% vs 6% in the general population[73,74]. This situation is thought to be mostly because of fears of the potential negative impact of pregnancy on the disease activity and also on transmitting IBD to the patient’s child[66,74]. Moller et al[75] studied the estimation of the familial risk of IBD in the entire Danish population from 1977 to 2011. The risk of CD and UC in the first-degree relatives of a CD and UC case was eightfold and fourfold increased, respectively, compared with families without IBD history. Laharie et al[76] reported that when the two parents were affected by IBD, the children had a 30% risk of developing IBD. Several studies have shown a significant association between voluntary childlessness and a low level of knowledge about IBD compared with controls, indicating that education could reassure some patients and allow them to consider pregnancy by correcting misconceptions[74]. This again stresses the importance of patient counseling before pregnancy. However, Nørgård et al[77] suggested that women with IBD were not so worried about their disease as they reported similar elective abortion rates compared with healthy women.
The first step to treat infertility is to provide accurate counseling to positively impact preconceptual care. The optimization of nutritional status, vitamins supplementation (vitamin D and zinc) and the cessation of tobacco and alcohol are necessary. Overall, how to control the disease activity must be obtained and maintained. IBD couples facing infertility should be referred to specialized gynecology centers. However, the medical literature is scarce on infertility treatment in IBD patients. Assisted reproductive technology (ART) such as in vitro fertilization, intracytoplasmic sperm injection, and frozen embryo replacement can be proposed to infertile IBD couples. Friedman et al[78] showed a significant decrease of the live birth rate within 18 mo after the beginning of ART for women with prior CD surgery compared with non-IBD women. Moreover, in the case of women affected by UC, prior surgery before ART did not affect the chance of a live birth[79]. In cases of persistent infertility for IBD patients, an overall recommendation could be to consider ART earlier than in the general population (for example after 6 mo) because it might be more tedious to succeed.
In IBD patients, more than 50% of women suffer from sexual dysfunction and 45% of men from erectile dysfunction. Psychological comorbidities, body image, and disease perception are strongly associated with poor sexual health in IBD patients. Because of this, patients are calling for more information on IBD and sexuality from their care providers. Open discussions, psychoeducational sessions, and referrals to a sexologist when needed would improve the QoL of patients. Fertility is another major concern among IBD patients. Inactive IBD has little to no impact on fertility rates, but psychological comorbidities and misconceptions about the disease lead to voluntary childlessness among IBD patients. Finally, patient counseling before and during pregnancy could be helpful in the patient’s reproductive years.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: France
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de'Angelis GL, M'Koma AE, Sitkin S, Wittmann T S-Editor: Ma RY L-Editor: A E-Editor: Zhang YL
| 1. | Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: Results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1:10-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 239] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 2. | Peyrin-Biroulet L. What is the patient's perspective: How important are patient-reported outcomes, quality of life and disability? Dig Dis. 2010;28:463-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Bel LG, Vollebregt AM, Van der Meulen-de Jong AE, Fidder HH, Ten Hove WR, Vliet-Vlieland CW, Ter Kuile MM, de Groot HE, Both S. Sexual Dysfunctions in Men and Women with Inflammatory Bowel Disease: The Influence of IBD-Related Clinical Factors and Depression on Sexual Function. J Sex Med. 2015;12:1557-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Zhao S, Wang J, Liu Y, Luo L, Zhu Z, Li E, Luo J, Zhao Z. Inflammatory Bowel Diseases Were Associated With Risk of Sexual Dysfunction in Both Sexes: A Meta-analysis. Inflamm Bowel Dis. 2019;25:699-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Maunder R, Toner B, de Rooy E, Moskovitz D. Influence of sex and disease on illness-related concerns in inflammatory bowel disease. Can J Gastroenterol. 1999;13:728-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Tavernier N, Fumery M, Peyrin-Biroulet L, Colombel JF, Gower-Rousseau C. Systematic review: fertility in non-surgically treated inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38:847-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Mañosa M, Navarro-Llavat M, Marín L, Zabana Y, Cabré E, Domènech E. Fecundity, pregnancy outcomes, and breastfeeding in patients with inflammatory bowel disease: a large cohort survey. Scand J Gastroenterol. 2013;48:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | WHO Sexual health [Internet]. [cited 2018 Sep 19]. Available from: http://www.who.int/topics/sexual_health/en/. |
| 9. | Knowles SR, Gass C, Macrae F. Illness perceptions in IBD influence psychological status, sexual health and satisfaction, body image and relational functioning: A preliminary exploration using Structural Equation Modeling. J Crohns Colitis. 2013;7:e344-e350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3880] [Cited by in RCA: 4342] [Article Influence: 173.7] [Reference Citation Analysis (0)] |
| 11. | Rosen RC, Cappelleri JC, Gendrano N. The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14:226-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 699] [Cited by in RCA: 731] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 12. | Peyrin-Biroulet L, Cieza A, Sandborn WJ, Coenen M, Chowers Y, Hibi T, Kostanjsek N, Stucki G, Colombel JF; International Programme to Develop New Indexes for Crohn's Disease (IPNIC) group. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut. 2012;61:241-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 277] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 13. | Ghosh S, Louis E, Beaugerie L, Bossuyt P, Bouguen G, Bourreille A, Ferrante M, Franchimont D, Frost K, Hebuterne X, Marshall JK, OʼShea C, Rosenfeld G, Williams C, Peyrin-Biroulet L. Development of the IBD Disk: A Visual Self-administered Tool for Assessing Disability in Inflammatory Bowel Diseases. Inflamm Bowel Dis. 2017;23:333-340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 14. | Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804-810. [PubMed] |
| 15. | de Rooy EC, Toner BB, Maunder RG, Greenberg GR, Baron D, Steinhart AH, McLeod R, Cohen Z. Concerns of patients with inflammatory bowel disease: results from a clinical population. Am J Gastroenterol. 2001;96:1816-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Rivière P, Zallot C, Desobry P, Sabaté JM, Vergniol J, Zerbib F, Peyrin-Biroulet L, Laharie D, Poullenot F. Frequency of and Factors Associated With Sexual Dysfunction in Patients With Inflammatory Bowel Disease. J Crohns Colitis. 2017;11:1347-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 17. | Marín L, Mañosa M, Garcia-Planella E, Gordillo J, Zabana Y, Cabré E, Domènech E. Sexual function and patients' perceptions in inflammatory bowel disease: a case-control survey. J Gastroenterol. 2013;48:713-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Friedman S, Magnussen B, OʼToole A, Fedder J, Larsen MD, Nørgård BM. Increased Use of Medications for Erectile Dysfunction in Men With Ulcerative Colitis and Crohn's Disease Compared to Men Without Inflammatory Bowel Disease: A Nationwide Cohort Study. Am J Gastroenterol. 2018;113:1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Muller KR, Prosser R, Bampton P, Mountifield R, Andrews JM. Female gender and surgery impair relationships, body image, and sexuality in inflammatory bowel disease: patient perceptions. Inflamm Bowel Dis. 2010;16:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 138] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 20. | Eluri S, Cross RK, Martin C, Weinfurt KP, Flynn KE, Long MD, Chen W, Anton K, Sandler RS, Kappelman MD. Inflammatory Bowel Diseases Can Adversely Impact Domains of Sexual Function Such as Satisfaction with Sex Life. Dig Dis Sci. 2018;63:1572-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Benson LS, Martins SL, Whitaker AK. Correlates of Heterosexual Anal Intercourse among Women in the 2006-2010 National Survey of Family Growth. J Sex Med. 2015;12:1746-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Enquête sur la sexualité en France [Internet]. Ined - Inst. Natl. D’études Démographiques [cited 2018 Sep 19] Available from: https://www.ined.fr/fr/publications/coeditions/enquete-sur-la-sexualite-en-france/. |
| 23. | Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14-94. J Sex Med. 2010;7 Suppl 5:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 352] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 24. | Martin T, Smukalla SM, Kane S, Hudesman DP, Greene R, Malter LB. Receptive Anal Intercourse in Patients with Inflammatory Bowel Disease: A Clinical Review. Inflamm Bowel Dis. 2017;23:1285-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Beaugerie L, Carrat F, Nahon S, Zeitoun JD, Sabaté JM, Peyrin-Biroulet L, Colombel JF, Allez M, Fléjou JF, Kirchgesner J, Svrcek M; Cancers et Surrisque Associé aux Maladies Inflammatoires Intestinales En France Study Group. High Risk of Anal and Rectal Cancer in Patients With Anal and/or Perianal Crohn's Disease. Clin Gastroenterol Hepatol. 2018;16:892-899.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 26. | Roberts JR, Siekas LL, Kaz AM. Anal intraepithelial neoplasia: A review of diagnosis and management. World J Gastrointest Oncol. 2017;9:50-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 80] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (1)] |
| 27. | Tack GJ, de Boer NKH. Let Us Not Forget HPV Vaccination in Women and Men in IBD. Inflamm Bowel Dis. 2019;25:e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Dibley L, Norton C. Experiences of fecal incontinence in people with inflammatory bowel disease: self-reported experiences among a community sample. Inflamm Bowel Dis. 2013;19:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Mahmood S, Nusrat S, Crosby A, Zhao YD, Ali T. Assessment of sexual function among inflammatory bowel disease patients. Am J Gastroenterol. 2015;110:601-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Timmer A, Bauer A, Dignass A, Rogler G. Sexual function in persons with inflammatory bowel disease: a survey with matched controls. Clin Gastroenterol Hepatol. 2007;5:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Timmer A, Bauer A, Kemptner D, Fürst A, Rogler G. Determinants of male sexual function in inflammatory bowel disease: a survey-based cross-sectional analysis in 280 men. Inflamm Bowel Dis. 2007;13:1236-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 32. | Iglesias-Rey M, Barreiro-de Acosta M, Caamaño-Isorna F, Rodríguez IV, Ferreiro R, Lindkvist B, González AL, Dominguez-Munoz JE. Psychological factors are associated with changes in the health-related quality of life in inflammatory bowel disease. Inflamm Bowel Dis. 2014;20:92-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 33. | Lindsey I, George BD, Kettlewell MG, Mortensen NJ. Impotence after mesorectal and close rectal dissection for inflammatory bowel disease. Dis Colon Rectum. 2001;44:831-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Yoshida K, Araki T, Uchida K, Okita Y, Fujikawa H, Inoue M, Tanaka K, Inoue Y, Mohri Y, Kusunoki M. Sexual activity after ileal pouch-anal anastomosis in Japanese patients with ulcerative colitis. Surg Today. 2014;44:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Gorgun E, Remzi FH, Montague DK, Connor JT, O'Brien K, Loparo B, Fazio VW. Male sexual function improves after ileal pouch anal anastomosis. Colorectal Dis. 2005;7:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Cornish JA, Tan E, Teare J, Teoh TG, Rai R, Darzi AW, Paraskevas P, Clark SK, Tekkis PP. The effect of restorative proctocolectomy on sexual function, urinary function, fertility, pregnancy and delivery: a systematic review. Dis Colon Rectum. 2007;50:1128-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 143] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 37. | Øresland T, Bemelman WA, Sampietro GM, Spinelli A, Windsor A, Ferrante M, Marteau P, Zmora O, Kotze PG, Espin-Basany E, Tiret E, Sica G, Panis Y, Faerden AE, Biancone L, Angriman I, Serclova Z, de Buck van Overstraeten A, Gionchetti P, Stassen L, Warusavitarne J, Adamina M, Dignass A, Eliakim R, Magro F, D'Hoore A; European Crohn's and Colitis Organisation (ECCO). European evidence based consensus on surgery for ulcerative colitis. J Crohns Colitis. 2015;9:4-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 248] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 38. | Berndtsson I, Oresland T, Hultén L. Sexuality in patients with ulcerative colitis before and after restorative proctocolectomy: a prospective study. Scand J Gastroenterol. 2004;39:374-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 39. | Allocca M, Gilardi D, Fiorino G, Furfaro F, Peyrin-Biroulet L, Danese S. Sexual and reproductive issues and inflammatory bowel disease: a neglected topic in men. Eur J Gastroenterol Hepatol. 2018;30:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 40. | O'Toole A, Winter D, Friedman S. Review article: the psychosexual impact of inflammatory bowel disease in male patients. Aliment Pharmacol Ther. 2014;39:1085-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Szathmári M, Vásárhelyi B, Treszl A, Tulassay T, Tulassay Z. Association of dehydroepiandrosterone sulfate and testosterone deficiency with bone turnover in men with inflammatory bowel disease. Int J Colorectal Dis. 2002;17:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Aguirre MA, Vélez A, Romero M, Collantes E. Gynecomastia and sexual impotence associated with methotrexate treatment. J Rheumatol. 2002;29:1793-1794. [PubMed] |
| 43. | Blackburn WD, Alarcón GS. Impotence in three rheumatoid arthritis patients treated with methotrexate. Arthritis Rheum. 1989;32:1341-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 44. | Semet M, Paci M, Saïas-Magnan J, Metzler-Guillemain C, Boissier R, Lejeune H, Perrin J. The impact of drugs on male fertility: a review. Andrology. 2017;5:640-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 161] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 45. | Rivière P, Poullenot F, Zerbib F, Laharie D. Quality of Sex Life in Patients with Inflammatory Bowel Disease: The Gastroenterologists' Perspective. Inflamm Bowel Dis. 2017;23:E51-E52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 46. | Eugenio MD, Jun SE, Cain KC, Jarrett ME, Heitkemper MM. Comprehensive self-management reduces the negative impact of irritable bowel syndrome symptoms on sexual functioning. Dig Dis Sci. 2012;57:1636-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 47. | Lindsey I, George B, Kettlewell M, Mortensen N. Randomized, double-blind, placebo-controlled trial of sildenafil (Viagra) for erectile dysfunction after rectal excision for cancer and inflammatory bowel disease. Dis Colon Rectum. 2002;45:727-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 48. | Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: a committee opinion. Fertil Steril. 2017;107:52-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 49. | Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. 2003;18:1959-1966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 50. | Selinger CP, Eaden J, Selby W, Jones DB, Katelaris P, Chapman G, McDondald C, McLaughlin J, Leong RW, Lal S. Inflammatory bowel disease and pregnancy: lack of knowledge is associated with negative views. J Crohns Colitis. 2013;7:e206-e213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 51. | van der Woude CJ, Ardizzone S, Bengtson MB, Fiorino G, Fraser G, Katsanos K, Kolacek S, Juillerat P, Mulders AG, Pedersen N, Selinger C, Sebastian S, Sturm A, Zelinkova Z, Magro F; European Crohn’s and Colitis Organization. The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis. 2015;9:107-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 335] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 52. | Cornish J, Tan E, Teare J, Teoh TG, Rai R, Clark SK, Tekkis PP. A meta-analysis on the influence of inflammatory bowel disease on pregnancy. Gut. 2007;56:830-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 325] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 53. | Nguyen GC, Seow CH, Maxwell C, Huang V, Leung Y, Jones J, Leontiadis GI, Tse F, Mahadevan U, van der Woude CJ; IBD in Pregnancy Consensus Group; Canadian Association of Gastroenterology. The Toronto Consensus Statements for the Management of Inflammatory Bowel Disease in Pregnancy. Gastroenterology. 2016;150:734-757.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 340] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 54. | de Lima A, Zelinkova Z, Mulders AG, van der Woude CJ. Preconception Care Reduces Relapse of Inflammatory Bowel Disease During Pregnancy. Clin Gastroenterol Hepatol. 2016;14:1285-1292.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 55. | Martin J, Kane SV, Feagins LA. Fertility and Contraception in Women With Inflammatory Bowel Disease. Gastroenterol Hepatol (NY). 2016;12:101-109. [PubMed] |
| 56. | Sands K, Jansen R, Zaslau S, Greenwald D. Review article: the safety of therapeutic drugs in male inflammatory bowel disease patients wishing to conceive. Aliment Pharmacol Ther. 2015;41:821-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 57. | Birnie GG, McLeod TI, Watkinson G. Incidence of sulphasalazine-induced male infertility. Gut. 1981;22:452-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 120] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 58. | Dejaco C, Mittermaier C, Reinisch W, Gasche C, Waldhoer T, Strohmer H, Moser G. Azathioprine treatment and male fertility in inflammatory bowel disease. Gastroenterology. 2001;121:1048-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 59. | Grosen A, Nersting J, Bungum M, Christensen LA, Schmiegelow K, Spanò M, Julsgaard M, Cordelli E, Leter G, Larsen PB, Hvas CL, Kelsen J. Sperm DNA Integrity is Unaffected by Thiopurine Treatment in Men With Inflammatory Bowel Disease. J Crohns Colitis. 2019;13:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Mahadevan U. Fertility and pregnancy in the patient with inflammatory bowel disease. Gut. 2006;55:1198-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 61. | Mahadevan U, Terdiman JP, Aron J, Jacobsohn S, Turek P. Infliximab and semen quality in men with inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 93] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 62. | Villiger PM, Caliezi G, Cottin V, Förger F, Senn A, Østensen M. Effects of TNF antagonists on sperm characteristics in patients with spondyloarthritis. Ann Rheum Dis. 2010;69:1842-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 63. | Waljee A, Waljee J, Morris AM, Higgins PD. Threefold increased risk of infertility: a meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut. 2006;55:1575-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 246] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 64. | Rajaratnam SG, Eglinton TW, Hider P, Fearnhead NS. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011;26:1365-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 65. | Beyer-Berjot L, Maggiori L, Birnbaum D, Lefevre JH, Berdah S, Panis Y. A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg. 2013;258:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 66. | Mountifield R, Bampton P, Prosser R, Muller K, Andrews JM. Fear and fertility in inflammatory bowel disease: a mismatch of perception and reality affects family planning decisions. Inflamm Bowel Dis. 2009;15:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 176] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 67. | Ørding Olsen K, Juul S, Berndtsson I, Oresland T, Laurberg S. Ulcerative colitis: female fecundity before diagnosis, during disease, and after surgery compared with a population sample. Gastroenterology. 2002;122:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 220] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 68. | Fréour T, Miossec C, Bach-Ngohou K, Dejoie T, Flamant M, Maillard O, Denis MG, Barriere P, Bruley des Varannes S, Bourreille A, Masson D. Ovarian reserve in young women of reproductive age with Crohn's disease. Inflamm Bowel Dis. 2012;18:1515-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 69. | Şenateş E, Çolak Y, Erdem ED, Yeşil A, Coşkunpınar E, Şahin Ö, Altunöz ME, Tuncer I, Kurdaş Övünç AO. Serum anti-Müllerian hormone levels are lower in reproductive-age women with Crohn's disease compared to healthy control women. J Crohns Colitis. 2013;7:e29-e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 70. | Li Y, Lin H, Li Y, Cao J. Association between socio-psycho-behavioral factors and male semen quality: systematic review and meta-analyses. Fertil Steril. 2011;95:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 206] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 71. | Sermondade N, Faure C, Fezeu L, Shayeb AG, Bonde JP, Jensen TK, Van Wely M, Cao J, Martini AC, Eskandar M, Chavarro JE, Koloszar S, Twigt JM, Ramlau-Hansen CH, Borges E, Lotti F, Steegers-Theunissen RP, Zorn B, Polotsky AJ, La Vignera S, Eskenazi B, Tremellen K, Magnusdottir EV, Fejes I, Hercberg S, Lévy R, Czernichow S. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update. 2013;19:221-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 497] [Cited by in RCA: 406] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 72. | Shin T, Okada H. Infertility in men with inflammatory bowel disease. World J Gastrointest Pharmacol Ther. 2016;7:361-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 73. | Marri SR, Ahn C, Buchman AL. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:591-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 145] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 74. | Selinger CP, Ghorayeb J, Madill A. What Factors Might Drive Voluntary Childlessness (VC) in Women with IBD? Does IBD-specific Pregnancy-related Knowledge Matter? J Crohns Colitis. 2016;10:1151-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 75. | Moller FT, Andersen V, Wohlfahrt J, Jess T. Familial risk of inflammatory bowel disease: a population-based cohort study 1977-2011. Am J Gastroenterol. 2015;110:564-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 162] [Article Influence: 16.2] [Reference Citation Analysis (1)] |
| 76. | Laharie D, Debeugny S, Peeters M, Van Gossum A, Gower-Rousseau C, Bélaïche J, Fiasse R, Dupas JL, Lerebours E, Piotte S, Cortot A, Vermeire S, Grandbastien B, Colombel JF. Inflammatory bowel disease in spouses and their offspring. Gastroenterology. 2001;120:816-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 77. | Nørgård BM, Magnussen B, Fedder J, de Silva PS, Wehberg S, Friedman S. The Risk of Elective Abortion in Women With Crohn's Disease and Ulcerative Colitis: A Nationwide Cohort Study. Inflamm Bowel Dis. 2019;25:561-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 78. | Friedman S, Larsen PV, Fedder J, Nørgård BM. The Efficacy of Assisted Reproduction in Women with Inflammatory Bowel Disease and the Impact of Surgery-A Nationwide Cohort Study. Inflamm Bowel Dis. 2017;23:208-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 79. | Nørgård BM, Larsen PV, Fedder J, de Silva PS, Larsen MD, Friedman S. Live birth and adverse birth outcomes in women with ulcerative colitis and Crohn's disease receiving assisted reproduction: a 20-year nationwide cohort study. Gut. 2016;65:767-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 80. | de Silva PS, Hansen HH, Wehberg S, Friedman S, Nørgård BM. Risk of Ectopic Pregnancy in Women With Inflammatory Bowel Disease: A 22-Year Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2018;16:83-89.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |