Published online Aug 28, 2018. doi: 10.3748/wjg.v24.i32.3671
Peer-review started: July 2, 2018
First decision: July 11, 2018
Revised: July 17, 2018
Accepted: July 22, 2018
Article in press: July 21, 2018
Published online: August 28, 2018
Processing time: 61 Days and 22.7 Hours
To investigate the vascular anatomy of inferior mesenteric artery (IMA) in laparoscopic radical resection with the preservation of left colic artery (LCA) for rectal cancer.
A total of 110 patients with rectal cancer who underwent laparoscopic surgical resection with preservation of the LCA were retrospectively reviewed. A 3D vascular reconstruction was performed before each surgical procedure to assess the branches of the IMA. During surgery, the relationship among the IMA, LCA, sigmoid artery (SA) and superior rectal artery (SRA) was evaluated, and the length from the origin of the IMA to the point of branching into the LCA or common trunk of LCA and SA was measured. The relationship between inferior mesenteric vein (IMV) and LCA was also evaluated.
Three vascular types were identified in this study. In type A, LCA arose independently from IMA (46.4%, n = 51); in type B, LCA and SA branched from a common trunk of the IMA (23.6%, n = 26); and in type C, LCA, SA, and SRA branched at the same location (30.0%, n = 33). The difference in the length from the origin of IMA to LCA was not statistically significant among the three types. LCA was located under the IMV in 61 cases and above the IMV in 49 cases.
The vascular anatomy of the IMA and IMV is essential for laparoscopic radical resection with preservation of the LCA for rectal cancer. To recognize different branches of the IMA is necessary for the resection of lymph nodes and dissection of vessels.
Core tip: One hundred and ten patients who underwent laparoscopic surgical resection with preservation of left colic artery (LCA) for rectal cancer were retrospectively reviewed. The 3D reconstruction of the vasculature was performed before surgical procedures. The types of branch vessels of inferior mesenteric artery (IMA) were classified. Furthermore, in the operations, relationships between the IMA, sigmoid artery (SA), LCA and superior rectal artery (SRA) were evaluated. The relationship between LCA and inferior mesenteric vein (IMV) was also evaluated. To recognize different branches of the IMA is necessary for the resection of lymph nodes and dissection of vessels during laparoscopic radical resection of rectal cancer.
- Citation: Wang KX, Cheng ZQ, Liu Z, Wang XY, Bi DS. Vascular anatomy of inferior mesenteric artery in laparoscopic radical resection with the preservation of left colic artery for rectal cancer. World J Gastroenterol 2018; 24(32): 3671-3676
- URL: https://www.wjgnet.com/1007-9327/full/v24/i32/3671.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i32.3671
In laparoscopic radical resection for rectal cancer, high-tie of the inferior mesenteric artery (IMA) at its origin is essential for en bloc lymph node dissection. Some researchers have demonstrated the clinical significance of lymph node dissection from the origin of the IMA for postoperative staging and prognosis[1]. However, high tie at the origin of the IMA may lead to postoperative poor anastomotic perfusion, which increases the incidence of anastomotic leakage[2,3]. Many surgeons prefer a low-tie technique, which ligates the IMA while preserving the left colic artery (LCA) after lymph nodes around the IMA were dissected[4,5]. A clear understanding of the vascular anatomy of the IMA and inferior mesenteric vein (IMV) is essential for this low-tie procedure. However, there are multiple types of branch vessels originating from the IMA that makes this surgical procedure technically demanding[6]. We studied the vascular anatomy of the IMA to safely and effectively dissect the lymph nodes around the IMA while preserving the LCA in a laparoscopic procedure for rectal cancer.
Following approval of the Ethics Committee on Scientific Research of our hospital, the records of 110 patients, who underwent laparoscopic surgical resection with preservation of the LCA for rectal cancer from March 2016 to November 2017 were retrospectively analyzed. The research participants were recruited from the Department of General Surgery of Qilu Hospital, a teaching hospital of Shandong University in Shandong, China. The data of patient age, sex ratio, BMI, and histopathological stage were observed and compared.
The 3D reconstruction of the vascular anatomy was performed in all cases before surgery. The types of branch vessels of the IMA as well as the length from the origin of the IMA to the LCA were determined.
Laparoscopic surgery was performed by a single operating team consisting of two senior surgeons and three staff surgeons. During the operation, the patients were placed in lithotomy position. Multi-incision laparoscopic surgery was performed. That was, we placed five ports including the optical port. There were the first 10 mm trocar in the umbilicus as the optical port, another 12-mm trocar, and three 5-mm trocars. We established pneumoperitoneum and maintained abdominal pneumoperitoneum pressure at 12 mmHg. Sharp dissections were performed using a laparoscopic ultrasound knife. First, the small intestine was pulled on its cephalic side to allow for sufficient surgical space. Second, the sigmoid colon mesentery was mobilized with medial to lateral approach up to the origin of the IMA. Lymphous and adipic tissues were resected along the IMA down to the point of branching into the LCA or common trunk of LCA and sigmoid artery (SA). The dissection was then conducted from the LCA until the IMV could be identified. The IMV was exposed to the plane of the origin of the IMA. After the dissection, the vessels were ligated and cut with the preservation of the LCA. The superior hypogastric nerve and left ureter were carefully preserved during the procedure.
During surgery, the relationship among the IMA, LCA, SA, and superior rectal artery (SRA) was evaluated, and the length from the origin of the IMA to the point of branching into the LCA or common trunk of LCA and SA was measured. In addition, the relationship between LCA and IMV was also evaluated. The number of resected lymph nodes and the incidence of metastasis to station 253 nodes were recorded. Furthermore, the incidence of anastomotic bleeding and anastomotic leakage, and the length of postoperative hospital stay were investigated.
All experimental data were analyzed using the SPSS software version 17.0 (SPSS Inc., Chicago, IL, United States). There were three groups of samples in this study. The three groups were compared by single factor analysis of variance (single factor ANOVA) and homogeneity of variance. The comparison between the two groups was used on the LSD method. The count data were represented by the value/percentage (%), and the three groups were compared with the chi square test and Fisher accurate test. When the theoretical number T < 5, the Fisher test value was used, if not, the Pearson chi square test was used.
The data of patient age, sex ratio, BMI, and histopathological stage are shown in Table 1. There were no statistically significant differences among the three types.
| Factors | Type A (n = 51) | Type B (n = 26) | Type C (n = 33) | Statistical value | P value |
| Age (yr, mean ± SD) | 58.6 ± 14.1 | 60.4 ± 15.0 | 62.3 ± 12.9 | F = 2.881 | 0.06 |
| Male, n (%) | 31 (60.8) | 15 (57.7) | 18 (54.5) | Pearson χ2 = 0.324 | 0.85 |
| BMI (kg/m2) | 25.3 ± 5.4 | 24.8 ± 4.9 | 25.1 ± 4.6 | F = 0.331 | 0.72 |
| Stage (UICC 8th) | Fisher = 1.510 | 0.84 | |||
| I | 7 | 5 | 6 | ||
| II | 26 | 10 | 16 | ||
| III | 18 | 11 | 11 |
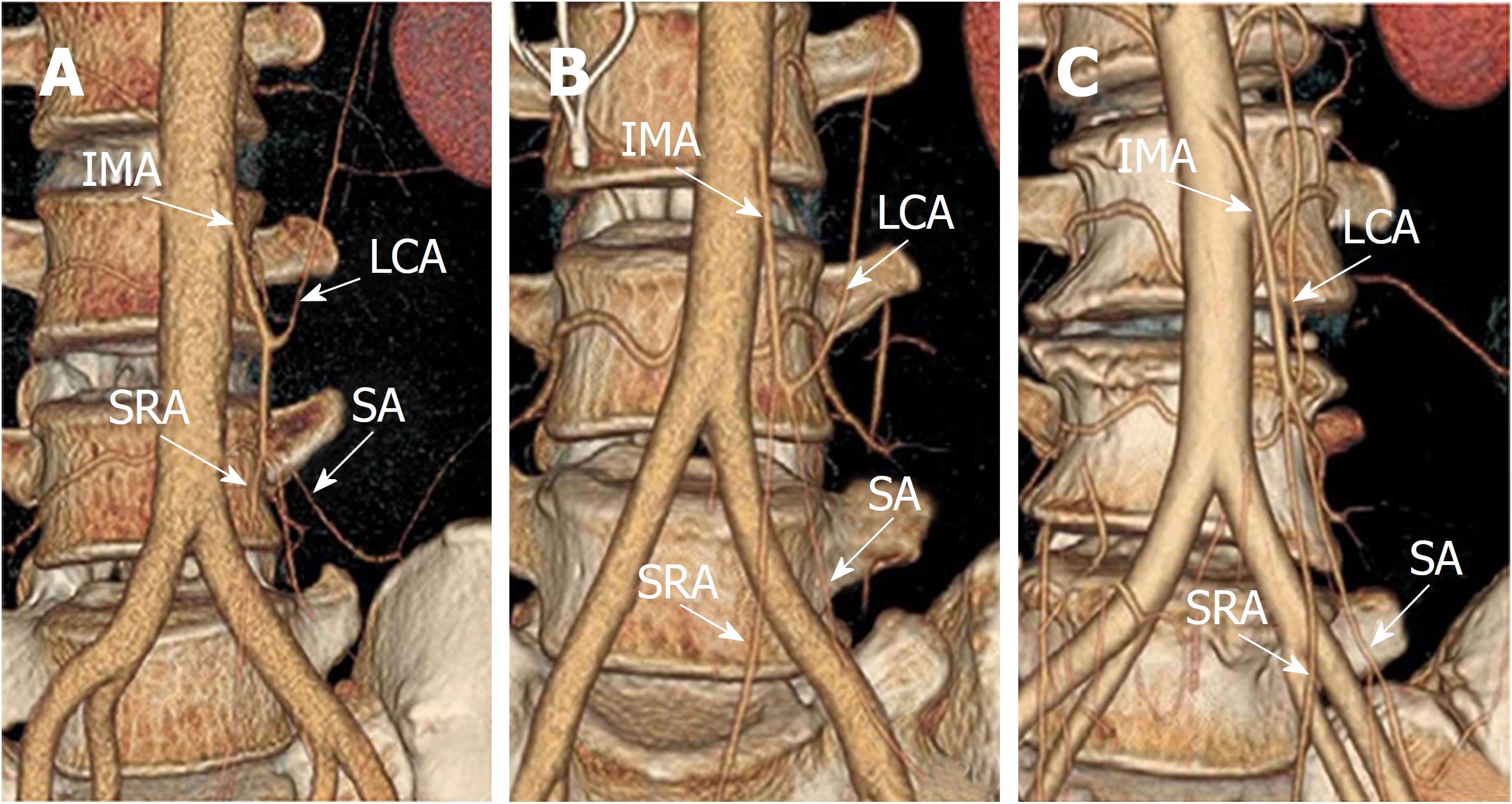
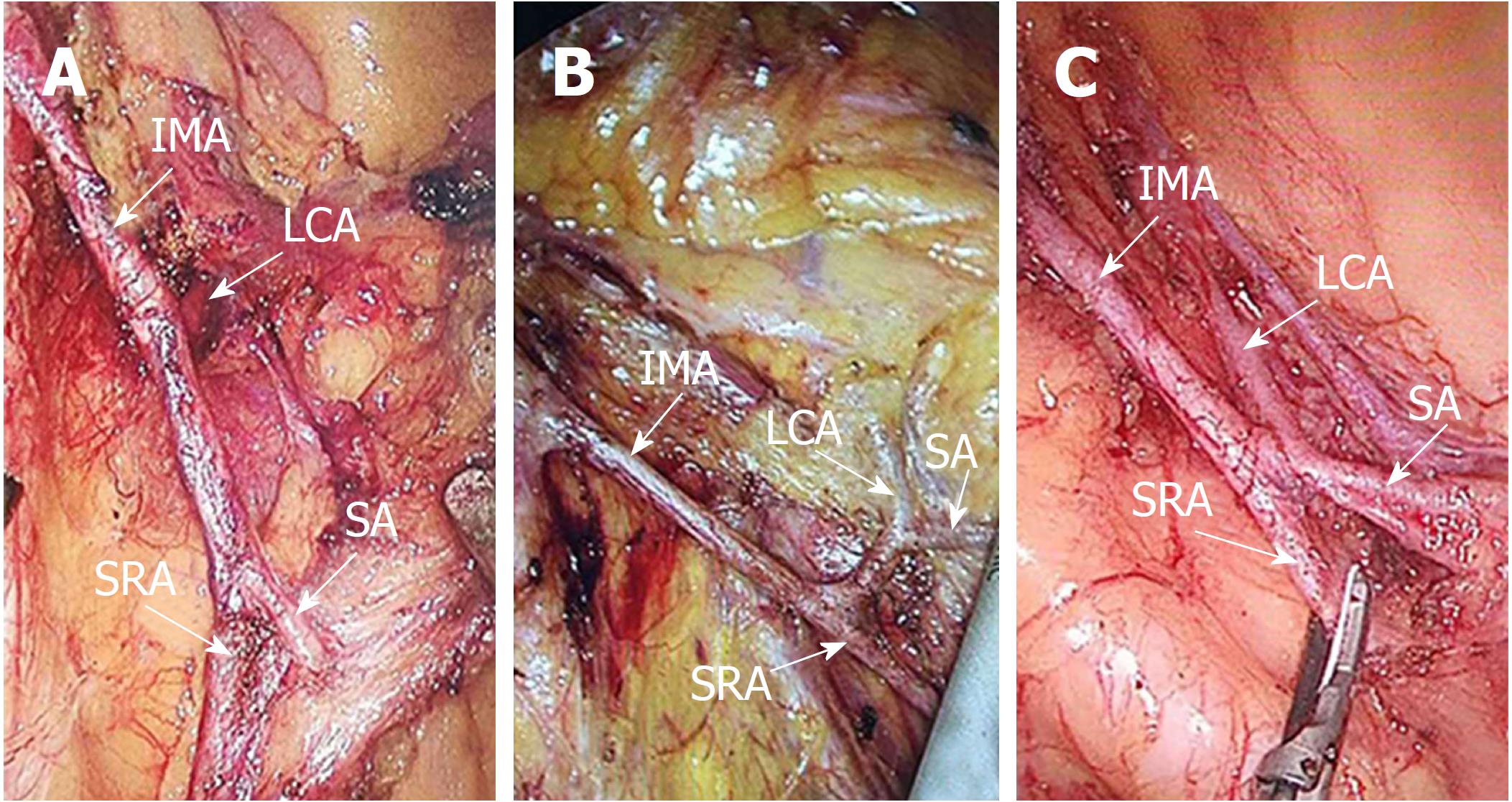
IMA, LCA, SA, and SRA were studied in 110 cases by preoperative 3D reconstruction of the vascular anatomy (Figure 1A-C) and laparoscopic surgery (Figure 2A-C). Three vascular types were identified in the study: type A (Figures 1A, 2A, and 3A), LCA arose independently from the IMA (46.4%, n = 51); type B (Figures 1B, 2B, and 3B), LCA and SA branched from a common trunk of the IMA (23.6%, n = 26); and type C (Figures 1C, 2C, and 3C), LCA, SA, and SRA branched at the same location (30.0%, n = 33). The length from the origin of the IMA to the LCA is displayed in Table 2. There was no statistically significant difference among the three types.
| Factors | Type A (n = 51) | Type B (n = 26) | Type C (n = 33) | Statistical value | P value |
| Length from the IMA to the LCA (mm) (mean ± SD) | 35.2 ± 8.7 | 37.8 ± 9.4 | 41.3 ± 11.5 | F = 1.976 | 0.144 |
| No. of LCA under IMV | 27 (52.9%) | 14 (53.8%) | 20 (60.6%) | Pearson χ2 = 0.512 | 0.802 |
In laparoscopic surgery, the relationship between the location of LCA and IMV was observed. The LCA was located under the IMV in 61 cases and above the IMV in 49 cases. The ratio regarding the location of the LCA under the IMV in the three types was similar (Table 2).
As shown in Table 3, the data of operating time, blood loss, and the length of postoperative hospital stay were not statistically significant among the three groups. Additionally, there were no statistically significant differences in the dissected lymph node numbers. The incidence of metastasis to station 253 nodes was 4.5% (5 of 110). The postoperative complications included anastomotic bleeding in two cases and anastomotic leakage in two cases. No statistically significant difference was observed among the three groups.
| Type A (n = 51) | Type B (n = 26) | Type C (n = 33) | Statistical value | P value | |
| Operation time (min) | 153.4 ± 26.8 | 168.7 ± 31.6 | 161.4 ± 25.8 | F = 1.618 | 0.20 |
| Blood loss (g) | 37.5 ± 18.4 | 42.1 ± 17.7 | 39.6 ± 20.1 | F = 1.383 | 0.26 |
| Lymph node numbers (n, mean ± SD) | 15.7 ± 8.3 | 17.2 ± 8.1 | 16.8 ± 9.0 | F = 0.620 | 0.54 |
| Metastasis to station 253 lymph nodes (n) | 2 | 1 | 1 | Fisher = 0.368 | 1.00 |
| Anastomotic bleeding | 1 | 1 | Fisher = 0.930 | 0.10 | |
| Anastomotic leakage | 1 | 1 | Fisher = 1.407 | 0.72 | |
| Postoperative hospitalized days | 9 (7-21) | 9 (6-18) | 9 (7-13) | χ2 = 0.863 | 0.65 |
In laparoscopic radical resection for rectal cancer, according to the location of the tie of the IMA, it is divided into the high-tie of the IMA at its origin and the low-tie of the IMA below the branch into the LCA with preservation of the LCA. Currently, there is still controversy regarding the indications for high-tie or low-tie approaches[7-9]. In traditional rectal cancer surgery, a high tie of the IMA is preferred. However, some anatomical studies suggest that anastomotic perfusion is diminished after the high-tie of the IMA[3]. Consequently, postoperative poor anastomotic perfusion increased the incidence of anastomotic leakage[10,11]. LCA can increase the blood supply of anastomotic and proximal colorectum. The Riolan artery arch is an anastomotic branch between ascending branches of the LCA and the left branches of the middle colonic artery. It is vital to the blood supply of the anastomotic and proximal colorectum. The Riolan arch exists in about 7.6% of the Chinese population[12]. In patients with absence of the Riolan arch, left hemicolon relies on blood supply from the IMA, and the high-tie technique causes ischemic changes of anastomotic stoma easily. Some Chinese surgeons have found that the absence of the Riolan arch is an independent risk factor for anastomotic leakage after laparoscopic radical resection of rectal cancer[13]. So the low-tie technique with preservation of the LCA to maintain the blood supply is recommended[14,15]. Furthermore, more and more research has indicated that the preservation of the LCA decreases the rate of anastomotic leakage[2,14,15].
A clear understanding of the vascular anatomy of the IMA and IMV is the essential knowledge required to conduct this surgical procedure. There are multiple types of branch vessels of the IMA that makes this surgery technically demanding. In our study, the branching patterns of the IMA can be divided into three groups by preoperative 3D vascular reconstruction and laparoscopic surgery (Figures 1 and 2). However, in other studies, there is a fourth pattern with the absence of the LCA[6,16]. Similarly, the relationship between the LCA and IMV was also observed. In 61 of the 110 cases, the LCA ran under the IMV. In these cases, during dissection of the LCA, extreme caution should be taken, and ligation of the SMV was performed first in order to avoid any damage to the IMV. Although there is still uncertainty with regard to the technical difficulty of the procedure, Sekimoto et al[17] have demonstrated that compared to the high-tie technique, the low-tie procedure did not prolong the operating time and did not increase the amount of intraoperative bleeding. In the present study, compared with other previous studies on high ligation, the operating time was not prolonged significantly[17,18]. In addition, the incidence of postoperative complications was relatively low owing to the familiarity with anatomy and meticulous operation. According to our results, low-tie of the IMA with preservation of the LCA was safe and feasible.
Lymph node metastasis plays a crucial role in the prognosis of rectal cancer[18]. It was demonstrated that lymph node dissection around the IMA prolonged the survival of patients with lymph node metastasis. Low-tie of the IMA with preservation of the LCA was suspected to hinder the lymph nodes resection surrounding the IMA. A prospective study showed that the low-tie group had a similar number of lymph nodes dissected compared to the high-tie group[19]. Other studies compared the prognosis between high-tie and low-tie, and found that the overall survival (OS) and recurrence free survival (RFS) were similar between the two treatments, even in those with lymph node metastases[5]. In the present study, the number of lymph nodes dissected with the low-tie technique for rectal cancer (Table 1) was similar to other studies[1,6]. Nonetheless, our study did not include a high-tie control group, which is a major limitation to the results and prevents an effective discussion to be established to address these problems.
In conclusion, knowledge of the anatomy of the branch vessels originating from the IMA and the relationship between the IMA and IMV are essential in order to conduct a laparoscopic radical resection with preservation of the LCA for rectal cancer. To recognize the different branches of the IMA is necessary for the resection of lymph nodes and dissection of vessels.
In laparoscopic radical resection for rectal cancer, according to the location of the tie of the inferior mesenteric artery (IMA), it is divided into the high-tie of the IMA at its origin and the low-tie of the IMA below the branch into the left colic artery (LCA) with preservation of the LCA. Currently, there is still controversy regarding the indications for high-tie or low-tie approaches.
In laparoscopic radical resection for rectal cancer, high-tie of the IMA at its origin is essential for en bloc lymph node dissection. We studied the vascular anatomy of the IMA to safely and effectively dissect the lymph nodes around the IMA while preserving the LCA in a laparoscopic procedure for rectal cancer.
We aimed to investigate the vascular anatomy of IMA in laparoscopic radical resection with the preservation of LCA for rectal cancer.
The records of 110 patients, who underwent laparoscopic surgical resection with preservation of the LCA for rectal cancer from March 2016 to November 2017 were retrospectively analyzed. The research participants were recruited from the Department of General Surgery of Qilu Hospital, a teaching hospital of Shandong University in Shandong, China. A 3D vascular reconstruction was performed before each surgical procedure to assess the branches of the IMA. During surgery, the relationship among the IMA, LCA, sigmoid artery (SA) and superior rectal artery (SRA) was evaluated.
IMA, LCA, SA, and SRA were studied in 110 cases by preoperative 3D reconstruction of the vascular anatomy and laparoscopic surgery. Three vascular types were identified in the study: type A, LCA arose independently from the IMA (46.4%, n = 51); type B, LCA and SA branched from a common trunk of the IMA (23.6%, n = 26); and type C, LCA, SA, and SRA branched at the same location (30.0%, n = 33). There was no statistically significant difference in the length from the origin of the IMA to the LCA among the three types. In laparoscopic surgery, the LCA was located under the IMV in 61 cases and above the IMV in 49 cases. The ratio regarding the location of the LCA under the IMV in the three types was similar. The data of operating time, blood loss, and the length of postoperative hospital stay were not statistically significant among the three types. Additionally, there were no statistically significant differences in the dissected lymph node numbers. The incidence of metastasis to station 253 nodes was 4.5% (5 of 110). The postoperative complications included anastomotic bleeding in two cases and anastomotic leakage in two cases.
Knowledge of the anatomy of the branch vessels originating from the IMA and the relationship between the IMA and IMV are essential in order to conduct a laparoscopic radical resection with preservation of the LCA for rectal cancer. To recognize the different branches of the IMA is necessary for the resection of lymph nodes and dissection of vessels.
We studied the vascular anatomy of the IMA to safely and effectively dissect the lymph nodes around the IMA while preserving the LCA in a laparoscopic procedure for rectal cancer. However, in the light of the limited evidence, the clinical benefit needs more high-quality RCT studies.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen Y, Ong J, Tsegmed U S- Editor: Gong ZM L- Editor: Filipodia E- Editor: Yin SY
| 1. | You X, Wang Y, Chen Z, Li W, Xu N, Liu G, Zhao X, Huang C. [Clinical study of preserving left colic artery during laparoscopic total mesorectal excision for the treatment of rectal cancer]. Zhonghua WeiChang WaiKe ZaZhi. 2017;20:1162-1167. [PubMed] |
| 2. | Hinoi T, Okajima M, Shimomura M, Egi H, Ohdan H, Konishi F, Sugihara K, Watanabe M. Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer. World J Surg. 2013;37:2935-2943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Komen N, Slieker J, de Kort P, de Wilt JH, van der Harst E, Coene PP, Gosselink MP, Tetteroo G, de Graaf E, van Beek T. High tie versus low tie in rectal surgery: comparison of anastomotic perfusion. Int J Colorectal Dis. 2011;26:1075-1078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Shen J, Li M, Du Y, Xie D, Qu H, Zhang Y. Long-term outcomes of laparoscopic low anterior resection of rectal carcinoma with preservation of the left colic artery. Zhonghua WeiChang WaiKe ZaZhi. 2017;20:660-664. [PubMed] |
| 5. | Yasuda K, Kawai K, Ishihara S, Murono K, Otani K, Nishikawa T, Tanaka T, Kiyomatsu T, Hata K, Nozawa H. Level of arterial ligation in sigmoid colon and rectal cancer surgery. World J Surg Oncol. 2016;14:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Miyamoto R, Nagai K, Kemmochi A, Inagawa S, Yamamoto M. Three-dimensional reconstruction of the vascular arrangement including the inferior mesenteric artery and left colic artery in laparoscope-assisted colorectal surgery. Surg Endosc. 2016;30:4400-4404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Cirocchi R, Trastulli S, Farinella E, Desiderio J, Vettoretto N, Parisi A, Boselli C, Noya G. High tie versus low tie of the inferior mesenteric artery in colorectal cancer: a RCT is needed. Surg Oncol. 2012;21:e111-e123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Hida J, Okuno K. High ligation of the inferior mesenteric artery in rectal cancer surgery. Surg Today. 2013;43:8-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Mari G, Maggioni D, Costanzi A, Miranda A, Rigamonti L, Crippa J, Magistro C, Di Lernia S, Forgione A, Carnevali P. “High or low Inferior Mesenteric Artery ligation in Laparoscopic low Anterior Resection: study protocol for a randomized controlled trial” (HIGHLOW trial). Trials. 2015;16:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Dworkin MJ, Allen-Mersh TG. Effect of inferior mesenteric artery ligation on blood flow in the marginal artery-dependent sigmoid colon. J Am Coll Surg. 1996;183:357-360. [PubMed] |
| 11. | Lim DR, Hur H, Min BS, Baik SH, Kim NK. Colon Stricture After Ischemia Following a Robot-Assisted Ultra-Low Anterior Resection With Coloanal Anastomosis. Ann Coloproctol. 2015;31:157-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Cheng BC, Chang S, Huang J, Mao ZF, Wang ZW, Lu SQ, Wang TS, Wu XJ, Hu H, Xia J. [Surgical anatomy of the colic vessels in Chinese and its influence on the operation of esophageal replacement with colon]. Zhonghua Yi Xue Za Zhi. 2006;86:1453-1456. [PubMed] |
| 13. | Huang J, Zhou J, Wan Y, Lin Y, Deng Y, Zhou Z, Qiu J, Wang J, Huang M. Influences of inferior mesenteric artery types and Riolan artery arcade absence on the incidence of anastomotic leakage after laparoscopic resection of rectal cancer. Zhonghua WeiChang WaiKe ZaZhi. 2016;19:1113-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Napolitano AM, Napolitano L, Costantini R, Ucchino S, Innocenti P. [Skeletization of the inferior mesenteric artery in colorectal surgery. Current considerations]. G Chir. 1996;17:185-189. [PubMed] |
| 15. | Messinetti S, Giacomelli L, Manno A, Finizio R, Fabrizio G, Granai AV, Busicchio P, Lauria V. Preservation and peeling of the inferior mesenteric artery in the anterior resection for complicated diverticular disease. Ann Ital Chir. 1998;69:479-482; discussion 482-483. [PubMed] |
| 16. | Kobayashi M, Morishita S, Okabayashi T, Miyatake K, Okamoto K, Namikawa T, Ogawa Y, Araki K. Preoperative assessment of vascular anatomy of inferior mesenteric artery by volume-rendered 3D-CT for laparoscopic lymph node dissection with left colic artery preservation in lower sigmoid and rectal cancer. World J Gastroenterol. 2006;12:553-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Patroni A, Bonnet S, Bourillon C, Bruzzi M, Zinzindohoué F, Chevallier JM, Douard R, Berger A. Technical difficulties of left colic artery preservation during left colectomy for colon cancer. Surg Radiol Anat. 2016;38:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Kanemitsu Y, Hirai T, Komori K, Kato T. Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg. 2006;93:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Sekimoto M, Takemasa I, Mizushima T, Ikeda M, Yamamoto H, Doki Y, Mori M. Laparoscopic lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery. Surg Endosc. 2011;25:861-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |