Published online Feb 21, 2017. doi: 10.3748/wjg.v23.i7.1180
Peer-review started: July 1, 2016
First decision: August 29, 2016
Revised: September 13, 2016
Accepted: October 10, 2016
Article in press: October 10, 2016
Published online: February 21, 2017
Processing time: 235 Days and 0.5 Hours
To investigate the therapeutic effect of Jianpi Qingchang decoction (JPQCD) on dextran sulfate sodium (DSS)-induced ulcerative colitis (UC) in mice.
C57BL/c mice were injected intragastrically with 5% DSS instead of drinking water for 7 d, and their body weight, diarrhea severity and fecal bleeding were monitored, while the mice in the control group were treated with standard drinking water, without DSS. After 7 d, the DSS drinking water was changed to normal water and the DSS group continued with DSS water. The control and DSS groups were given normal saline by intragastric injection. The 5-aminosalicylic acid (5-ASA) group was treated orally with 5-ASA at a dose of 100 mg/kg daily. The JPQCD group was treated orally with JPQCD at a dose of 17.1 g/kg daily. On day 14, the colon length was measured, the colorectal histopathological damage score was assessed, and protein levels of interleukin (IL)-1β, IL-8 and tumor necrosis factor-alpha (TNF-α) in colon supernatants were measured by enzyme-linked immunosorbent assay. mRNA expression of IL-1β, IL-8, TNF-α and nuclear factor-kappa B (NF-κB) was detected by real-time quantitative polymerase chain reaction. Western blotting was used to detect the protein expression of NF-κB and inhibitor of kappa B.
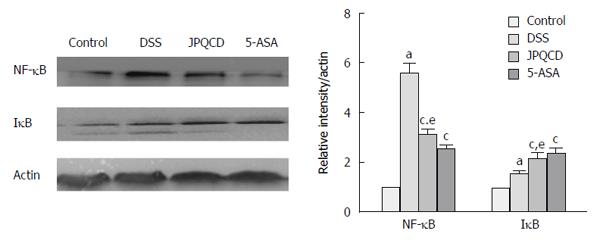
Acute inflammation occurred in the mice administered DSS, including the symptoms of losing body weight, loose feces/watery diarrhea and presence of fecal blood; all these symptoms worsened at 7 d. The colons of mice treated with DSS were assessed by histological examination, and the results confirmed that acute inflammation had occurred, as evidenced by loss of colonic mucosa and chronic inflammatory cell infiltration, and these features extended into the deeper layer of the colon walls. The expression levels of IL-1β, IL-8 and TNF-α in the DSS group were higher than those in the control group (P < 0.05), and the expression levels of IL-1β, IL-8 and TNF-α in the JPQCD and 5-ASA groups were lower than those in the DSS group after treating with JPQCD and 5-ASA. Comparing with the DSS group, the mRNA level of IL-1β, IL-8, TNF-α and NF-κB was significantly reduced by 5-ASA and JPQCD. The difference between JPQCD and 5-ASA groups was not statistically significant (P > 0.05). Comparing with the DSS group, due to using JPQCD and 5-ASA, significant suppression of activation in DSS-induced NF-κB and increased phosphorylation of IκB in mice with experimental colitis occurred (P < 0.05). The difference between the JPQCD group and the 5-ASA group was not statistically significant (P > 0.05).
Activation of the NF-κB signaling pathway is inhibited by JPQCD, which shows the potential mechanism by which JPQCD treats UC.
Core tip: Nuclear factor-kappa B (NF-κB) is a major transcription factor inducing the expression of inflammatory mediators, which plays a crucial role in the transcription in diverse immune responses, and its signaling has been confirmed to be a major pathway for ulcerative colitis. It is demonstrated in the current study that Jianpi Qingchang decoction (JPQCD), which can decrease levels of proinflammatory cytokines, plays a role in inhibiting nuclear translocation of NF-κB and phosphorylation of inhibitor of kappa B, thus indicating that JPQCD can suppress the activation of NF-κB signaling pathway.
- Citation: Zheng L, Zhang YL, Dai YC, Chen X, Chen DL, Dai YT, Tang ZP. Jianpi Qingchang decoction alleviates ulcerative colitis by inhibiting nuclear factor-κB activation. World J Gastroenterol 2017; 23(7): 1180-1188
- URL: https://www.wjgnet.com/1007-9327/full/v23/i7/1180.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i7.1180
Ulcerative colitis (UC) is a chronic gastrointestinal disorder characterized by inflammation and mucosal damage in colon, the pathophysiology of which is multifactorial, with environmental, genetic and immunological factors being involved[1]. Chronic colonic inflammation in patients with UC may be attributed to activation of the immune system through intestinal flora. The main clinical manifestations of UC include recurrent abdominal pain and diarrhea, as well as mucous, bloody or purulent stools[2]. Currently, disease severity is an important factor in selecting treatment strategies, most of which concentrate on alleviation of disease symptoms, rather than disease treatment. In addition, a large number of ways for treating UC may result in systemic immunosuppression, thus leading to limited long-term application and an urgent need to develop a novel therapeutic. At present, many researchers are interested in traditional Chinese medicine (TCM), such as herbal therapy, because these complementary and alternative agents have few side effects in treating various diseases, including UC[3-6]. Multiple cellular signal transduction pathways highly regulate inflammatory responses, including the nuclear factor-kappa B (NF-κB) pathway, a nuclear factor that can be activated by a variety of pathogens.
NF-κB, a major transcription factor, which induces expression of a large array of inflammatory mediators, is crucial in transcription related to diverse immune responses, and the NF-κB signaling pathway is regarded as a major pathway for UC[7]. Abnormal expression of NF-κB leads to release of proinflammatory cytokines, for instance, interleukin (IL)-1β, IL-8, tumor necrosis factor-alpha (TNF-α) and adhesion molecules.
Jianpi Qingchang decoction (JPQCD) is a TCM prescription that consists of nine Chinese herbs, namely, Astragalus, Codonopsis pilosula, Portulaca oleracea, Sanguisorba officinalis, Notoginseng, Bletilla striata, Radix Aucklandiae, and Licorice. JPQCD can clear away heat and dampness, and strengthen the spleen to produce vitality, thanks to effects of these components. In the TCM system, pathogenesis of UC is formed in the case of accumulation of toxic dampness and heat, therefore the basic principle for JPQCD to treat inflammatory diseases is to clear away heat and eliminate dampness. In China, JPQCD has long been applied in the treatment of UC in clinic; however, its precise mechanism of action of anti-inflammatory activities remains unknown. In this study, C57BL mice with dextran sodium sulfate (DSS)-induced UC were used as models of human intestinal epithelium, so as to evaluate the anti-inflammatory effects of JPQCD and to investigate its molecular mechanism.
C57BL/6 male mice weighing 18-22 g were purchased from the Laboratory Animal Center of Shanghai University of Traditional Chinese Medicine, and they were raised under the following conditions: a standard cycle of 12-h light/12-h dark, with the room temperature at 24 ± 2 °C and the relative humidity at 50% to 60%. Forty mice were randomly divided into four groups after 1 wk of acclimation, which were control group, DSS group, JPQCD group and 5-aminosalicylic acid (5-ASA) group, with 10 mice in each group.
After acclimation, mice were fed with 5% (w/v) DSS (MW 36000-50000; MP Biomedicals, Santa Ana, CA, United States)[8] dissolved in sterile distilled water ad libitum for 7 d to induce acute UC. When DSS-induced acute UC models were successfully established 7 d later, the DSS drinking water was replaced by normal water but the DSS group continued to be fed with DSS drinking water. Control and DSS groups were given 0.3 mL normal saline by intragastric administration. The 5-ASA group was offered oral administration of 5-ASA at a dose of 100 mg/kg daily. The JPQCD group was treated orally with JPQCD at a dose of 17.1 g/kg daily. Body weights were monitored daily, and daily weight changes were calculated as the percentage of initial weights.
Parameters shown below were adopted to calculate the disease activity index (DAI) in combination with a scale involving the grading from 0-4: weight loss (0: normal; 1: 0%-5%; 2: 5%-10%; 3: 10%-15%; and 4: > 15%); stool consistency (0: normal; 2: loose stools; and 4: watery diarrhea); and fecal occult blood (0: negative; 2: positive; and 4: gross bleeding)[9,10]. Mice were sacrificed under anesthesia 14 d later. Colons were removed, cut open longitudinally along the main axis, and washed with phosphate-buffered saline (pH 7.4). After gross examination, colons were fixed in 10% neutral-buffered formalin for histological examination, and the remaining colons were used for enzyme-linked immunosorbent assay (ELISA), mRNA and western blot analyses.
Protein expressions of IL-1β, IL-8 and TNF-α (BioLegend, San Diego, CA, United States) in supernatants from the colon were measured by commercially available ELISA kits.
Paraffin-embedded samples were cut into 5-μm sections and examined under light microscope after being stained with hematoxylin and eosin (HE). Samples were analyzed and scored as described previously[11,12].
The tissue samples were frozen and dissociated mechanically in RNA buffer, and total RNA was extracted using RNAprep Pure Tissue Kit (Tiangen, Shanghai, China). Real-time (RT)-PCR was carried out with the help of an Eppendorf PCR system; meanwhile, QuantiFast SYBR Green PCR Master Mix (TOYOBO, Osaka, Japan), 1 mmol/L primers (Table 1), and 1 μL cDNA in 20 μL reaction mixture were also used. Activation was performed for 30 s at 95 °C to initiate the thermal cycling, followed by 40 cycles of 10 min at 95 °C, 15 s at 95 °C and 1 min at 60 °C. Immediately after amplification, melt curve protocol was utilized to guarantee minimization in primer dimers and other non-specific products. Expression of target genes was analyzed by the ΔΔCt method.
| Gene | Primer sequence | Primer length (bp) | |
| IL-1β | Forward | 5’-TAGACAACTGCACTACAGGCTCCGA-3’ | 25 |
| Reverse | 5’-GGGTCCGACAGCACGAGGCT-3’ | 20 | |
| IL-8 | Forward | 5’-ATGCTGGTGACAACCACGGCC-3’ | 21 |
| Reverse | 5’-CCTCTGTGAAGTCTCCTCTCCGGAC-3’ | 25 | |
| TNF-α | Forward | 5’-TGGTGACCAGGCTGTCGCTACA-3’ | 22 |
| Reverse | 5’-TACAGTCACGGCTCCCGTGGG-3’ | 21 | |
| NF-κB | Forward | 5’-GTGGAGGCATGTTCGGTAGTG-3’ | 21 |
| Reverse | 5’-TCTTGGCACAATCTTTAGGGC-3’ | 21 | |
| Actin | Forward | 5’-GTGCCGCCTGGAGAAACC-3’ | 18 |
| Reverse | 5’-GGTGGAAGAGTGGGAGTTGC-3’ | 20 |
Western blot analysis described in previous studies was used[13]. Colonic tissue was cut into pieces and homogenized in 5-fold volumes of ice-cold homogenizing buffer (0.1 mmol/L NaCl, 0.1 mol/L Tris-HCl, and 0.001 mol/L EDTA) containing 1 mmol/L phenylmethylsulfonyl fluoride, 1 mg/mL aprotinin, and 0.1 mmol/L leupeptin at 3000 g and 4 °C for 1 h. Bovine serum albumin was used to estimate the protein content in supernatants. The protein samples (40 µg in each sample) were subjected to SDS-PAGE and transferred to polyvinylidene fluoride membranes using a transfer apparatus (Bio-Rad, Hercules, CA, United States). The membranes were blocked for 1 h before NF-κB and inhibitor of kappa B (IκB) (Cell Signaling Technology, Danvers, MA, United States) were adopted as the primary antibodies to incubate under the proper dilution at 4 °C overnight, and the corresponding horseradish-peroxidase-conjugated secondary antibody (Cell Signaling Technology) was used to incubate for another 1 h. Protein–antibody complexes were detected by Clarity Western ECL Substrate (Bio-Rad), and results were qualified with the ImageJ software (Gene Company Limited, China).
Research results were analyzed by SPSS 21.0 (SPSS, Chicago, IL, United States); analyses were performed by adopting statistical methods, such as student’s t-test and one-way analysis of variance (ANOVA), and histograms were generated by GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, United States). Difference with the P value < 0.05 was deemed as statistically significant.
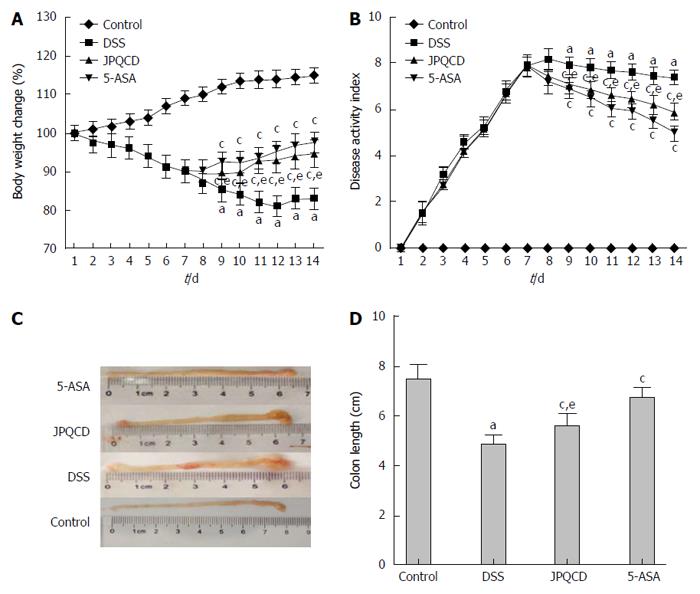
Compared with the control group, the characteristic weight loss in mice with DSS-induced acute colitis developed on day 3 (Figure 1A), and significant differences (P < 0.05) could be seen from day 4. However, administration of JPQCD and 5-ASA resulted in increased body weights, with significant difference (P < 0.05) being seen on day 9. Results in previous studies had indicated that length of colon was negatively correlated with severity of experimental colitis[14,15]. Observation results in the DSS-treated mice showed that colon was significantly shortened, and the suppressed results derived from treatment with JPQCD and 5-ASA (Figure 1B-D).
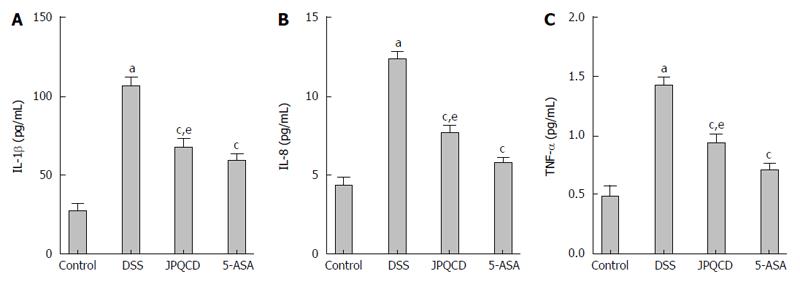
Secretion of IL-1β, IL-8 and TNF-α was measured to evaluate effects of JPQCD on DSS-induced experimental mice with acute colitis. Cytokines were released, which was regarded as an indicator of inflammatory response. JPQCD and 5-ASA groups were administered gavage once daily for 1 wk, and levels of IL-1β, IL-8 and TNF-α in supernatants from colonic tissue were assessed by ELISA, the results of which indicated that JPQCD and 5-ASA significantly decreased the release of IL-1β, IL-8 and TNF-α in mice with experimental colitis (Figure 2).
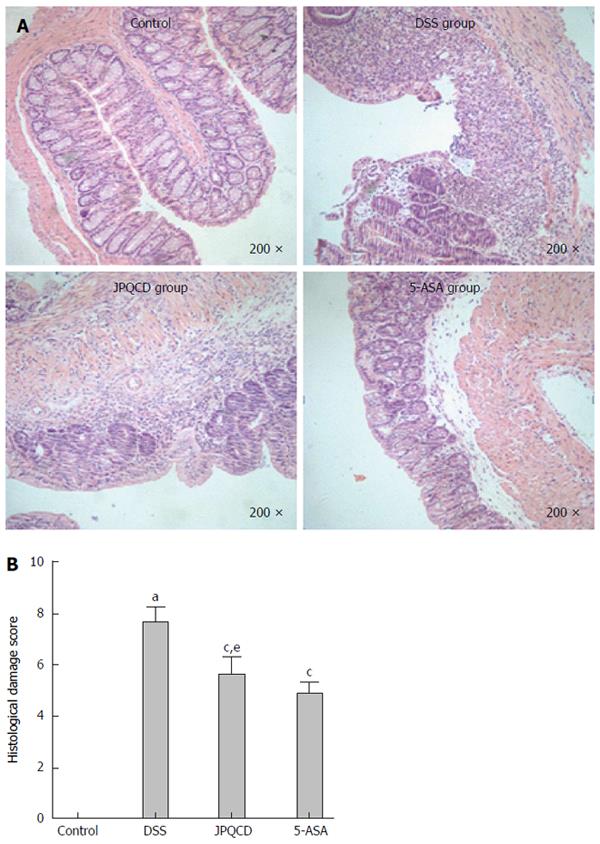
Histological and morphological characteristics of colon were assessed after HE staining, and representative results as well as the microscopic scores are shown in Figure 3A and B. Colons in the control group presented with normal crypt morphology, abundant goblet cells, no signs of mucosal thickening, and complete absence of ulceration. However, severe epithelial damage occurred in mice with induced colitis, giving rise to a higher score for microscopic damage (Figure 2A). On the contrary, scores for microscopic damage were lower in mice treated with JPQCD and 5-ASA than those in mice treated with DSS.
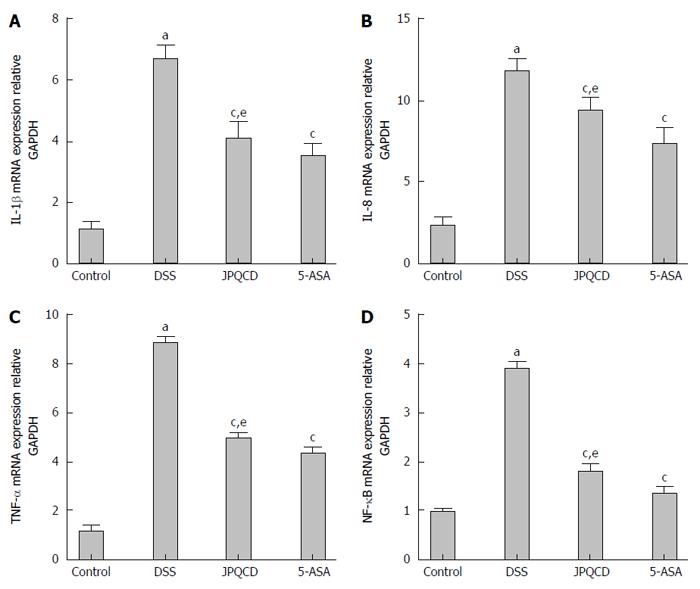
Expression levels of IL-1β, IL-8, TNF-α and NF-κB in control and experimental mice were measured by RT-PCR (Figure 4). Expression of IL-1β, IL-8, TNF-α and NF-κB was elevated during UC[16], as had been shown in numerous studies. Compared with control mice, increased expression of IL-1β, IL-8, TNF-α and NF-κB could be detected in experimental mice in this study, which was consistent with previous findings. However, oral administration of JPQCD and 5-ASA contributed to reducing expression levels of IL-1β, IL-8, TNF-α and NF-κB (P < 0.05).
As one of the core transcription factors in inflammation, activation of the NF-κB pathway involved several key processes, such as phosphorylation, IκB depredating and nuclear translocation of NF-κB. Effects of JPQCD on DSS-induced activation of NF-κB pathway in mice with experimental colitis were studied, with an aim to examine the mechanism of anti-inflammatory activity. Mice in the JPQCD group were pretreated with JPQCD once daily for 1 wk, and IκB was detected by western blot. Expression of IκB was significantly increased after treatment with JPQCD, and such increase was markedly alleviated by JPQCD (Figure 5).
UC, a major form of inflammatory bowel disease (IBD), results from chronic intestinal inflammatory response[17,18], the exact cause of which remains undiscovered, thus giving rise to ineffective treatment results. Additionally, a majority of treatments applied at present are associated with occurrence of systemic immunosuppression. As a consequence, there is in an urgent need to develop new medicines targeting UC. Natural products with few side effects[19], such as in TCM, have been studied and applied in treating various diseases and for replacing some remedies. It has been revealed in previous studies that the NF-κB pathway regulates UC in a close way, so it may be an efficient strategy for treating UC. JPQCD, a TCM prescription, has been applied in treating UC in clinic for many years; nevertheless, its anti-inflammatory properties remain unknown. In the current study, effects of JPQCD and its molecular mechanism were evaluated in C57BL mice with DSS-induced UC, which were treated as experimental models of colitis[20-22].
It was successfully demonstrated in this study that clinical features of UC reoccur in models of acute colitis. Typical features of UC, such as diarrhea, bloody feces, and weight loss occur on d 3 and are markedly expressed by day 7. Results in mice could also be seen in human, suggesting that weight loss and colon shortening, the stable markers of colitis, are correlated with histopathological changes.
It is noted in our research that body weight and colon length are outstandingly increased, while DAI is reduced after treating with JPQCD and 5-ASA for 7 d. Day 9 (2 d after completing the treatment) witnesses the beginning of inflammation reduction, which is consistent with results of research indicating that it takes a long time for the human body to respond to treatment. As an important nuclear transcription factor, NF-κB controls several important physiological processes, as well as immune and inflammatory responses. IκB kinase will phosphorylate IκB protein in the presence of pathologically stimulated cells. IκB proteins promote ubiquitination and degradation as a result of its phosphorylation, which leads to subsequent release of sequestered NF-κB, and further renders nuclear translocation, thus inducing expression of a variety of proinflammatory cytokines[23-25].
In the intestine, proinflammatory cytokines are produced, which play vital roles in pathogenesis of IBD. Hence, it is considered that release of proinflammatory cytokines is an indicator of inflammatory response[26]. TNF-α is crucial in recruiting immune cells at the sites of damaged tissues and in the pathogenesis of IBD. As a result, anti-TNF-α antibodies, including infliximab, are applied in treating UC and skin rash, extra-intestinal manifestations. However, it is indicated in the current study that anti-TNF antibodies, effective medicine in treating psoriasis, can result in psoriasiform skin lesion in IBD patients[27,28]. Furthermore, elevated levels of cytokines in UC, such as IL-8, IL-17 and IL-21 are reported[29,30].
It is observed that JPQCD has a remarkable effect on reducing DSS-induced secretion of proinflammatory cytokines in mice with colitis, so as to inhibit inflammatory responses in intestinal epithelial cells. It can be seen from our findings that mRNA levels of IL-1β, IL-8, TNF-α and NF-κB in mice with DSS-induced colitis are increased, while those are decreased in the presence of oral administration of JPQCD and 5-ASA, suggesting that JPQCD and 5-ASA have similar effects, but there is no significant difference between them. Consequently, JPQCD contributes to decreasing levels of proinflammatory cytokines.
Furthermore, NF-κB is considered to be an important factor to activate IBD in human and colitis in animals[31-33]. Actually, antisense oligonucleotides can inhibit disease activity in mice with colitis, indicating that NF-κB plays a key role in mediating inflammatory response[34]. Results in our current study reveal that compared with mice in the control group, expression of NF-κB is increased, while that of IκB is decreased. In the acute colitis model[35], mucosal inflammation can be controlled by using an agent to block the NF-κB pathway, which marks a successful attempt. Similar experimental results can also be obtained, which are that JPQCD treatment can inhibit phosphorylation of IκB and nuclear translocation of NF-κB, demonstrating that JPQCD inhibits the NF-κB signal pathway. In summary, results in our study show that JPQCD is promising in treating UC.
We would like to thank our colleagues in the Institute of Digestive Disease affiliated to Shanghai University of Traditional Chinese Medicine for their help and support in this research.
Multiple cellular signal transduction pathways, including the nuclear factor-kappa B (NF-κB) pathway, regulate the inflammatory response. A variety of pathogens can activate the NF-κB pathway, while the treatment is not effective in the long term. Currently, disease severity is an important factor when considering treatment strategies, and the attenuation of illness symptoms, rather than the treatment of illness is the focus in most of the strategies. As a result, development of a new treatment agent is urgently needed. Now, many researchers are interested in traditional Chinese medicine (TCM), such as herbal therapy, because these complementary and alternative agents have few side effects in treating various illnesses, including ulcerative colitis (UC).
The NF-κB signaling pathway plays a pivotal role in experimental UC in mice. This pathway is currently a hot topic in UC studies.
NF-κB is thought to be vital in the activation and progression of inflammatory bowel disease in humans and colitis in animals. Abnormal expression of NF-κB leads to release of proinflammatory cytokines, adhesion molecules and growth factors, and overexpression of cell proliferation-related genes and survival-related genes. The present study demonstrated that Jianpi Qingchang decoction (JPQCD) can decrease the levels of proinflammatory cytokines, and inhibit phosphorylation of inhibitor of kappa B and nuclear translocation of NF-κB in experimental colitis, which indicates that JPQCD suppresses activation of the NF-κB signaling pathway.
The present study provides evidence that JPQCD, a TCM decoction, inhibits activation of the NF-κB signaling pathway, suggesting that the potential mechanism by which JPQCD ameliorates dextran sulfate sodium (DSS)-induced UC is associated with this pathway. Thus, the findings of this study indicate a new potential mechanism by which JPQCD treats UC.
NF-κB is a transcription factor that can induce the expression of a large array of inflammatory mediators and plays a role as a core transcription factor in diverse immune responses.
The authors demonstrated that JPQCD has potential therapeutic effect on the treatment of UC through the inhibition of NF-κB activation. This is an important mechanistic advancement in our understanding of the herbal product JPQCD and its role in preventing UC. The anti-inflammatory effects of JPQCD and its underlying molecular mechanisms have been correlated with the reduction in the level of pro-inflammatory cytokines (IL-1β, IL-8 and TNF-α). Using real-time PCR, ELISA and H&E staining of the colon tissue clearly shows that JPQCD has protective effects against DSS-induced colon damage in mice.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Nihalani D S- Editor: Qi Y L- Editor: Filipodia E- Editor: Wang CH
| 1. | Niu X, Fan T, Li W, Huang H, Zhang Y, Xing W. Protective effect of sanguinarine against acetic acid-induced ulcerative colitis in mice. Toxicol Appl Pharmacol. 2013;267:256-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 2. | Bressler B, Marshall JK, Bernstein CN, Bitton A, Jones J, Leontiadis GI, Panaccione R, Steinhart AH, Tse F, Feagan B. Clinical practice guidelines for the medical management of nonhospitalized ulcerative colitis: the Toronto consensus. Gastroenterology. 2015;148:1035-1058.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 300] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 3. | Yang H, Li Y, Wu W, Sun Q, Zhang Y, Zhao W, Lv H, Xia Q, Hu P, Li H. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014;9:e101296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Ahn BM. [Herbal preparation-induced liver injury]. Korean J Gastroenterol. 2004;44:113-125. [PubMed] |
| 5. | Langmead L, Rampton DS: Review article: complementary and alternative therapies for inflammatory bowel disease. Aliment Pharmacol Ther. 2006;23:341-349. |
| 6. | Bensoussan M, Jovenin N, Garcia B, Vandromme L, Jolly D, Bouché O, Thiéfin G, Cadiot G. Complementary and alternative medicine use by patients with inflammatory bowel disease: results from a postal survey. Gastroenterol Clin Biol. 2006;30:14-23. [PubMed] |
| 7. | Shin EK, Kwon HS, Kim YH, Shin HK, Kim JK. Chrysin, a natural flavone, improves murine inflammatory bowel diseases. Biochem Biophys Res Commun. 2009;381:502-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Wirtz S, Neufert C, Weigmann B, Neurath MF. Chemically induced mouse models of intestinal inflammation. Nat Protoc. 2007;2:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1063] [Cited by in RCA: 1255] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 9. | Goto H, Takemura N, Ogasawara T, Sasajima N, Watanabe J, Ito H, Morita T, Sonoyama K. Effects of fructo-oligosaccharide on DSS-induced colitis differ in mice fed nonpurified and purified diets. J Nutr. 2010;140:2121-2127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Agollah GD, Wu G, Peng HL, Kwon S. Dextran sulfate sodium-induced acute colitis impairs dermal lymphatic function in mice. World J Gastroenterol. 2015;21:12767-12777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Rath HC, Herfarth H, Ikeda JS, Grenther WB, Hamm TE, Jr , Balish E, Taurog JD, Hammer RE, Wilson KH. “Normal luminal bacteria, especially bacteroides species, mediate chronic colitis, gastritis, and arthritis in HLA-B27/humanβ 2 microglobulin transgenic rats,”. J Clin Invest. 1996;4:945-953. |
| 12. | Van der Sluis M, De Koning BA, De Bruijn AC, Velcich A, Meijerink JP, Van Goudoever JB, Büller HA, Dekker J, Van Seuningen I, Renes IB. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology. 2006;131:117-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 1219] [Article Influence: 64.2] [Reference Citation Analysis (1)] |
| 13. | Pandurangan AK, Saadatdoust Z, Esa NM, Hamzah H, Ismail A. Dietary cocoa protects against colitis-associated cancer by activating the Nrf2/Keap1 pathway. Biofactors. 2015;41:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Bento AF, Marcon R, Dutra RC, Claudino RF, Cola M, Leite DF, Calixto JB. β-Caryophyllene inhibits dextran sulfate sodium-induced colitis in mice through CB2 receptor activation and PPARγ pathway. Am J Pathol. 2011;178:1153-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 186] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 15. | Pandurangan AK, Ismail S, Saadatdoust Z, Esa NM. Allicin Alleviates Dextran Sodium Sulfate- (DSS-) Induced Ulcerative Colitis in BALB/c Mice. Oxid Med Cell Longev. 2015;2015:605208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 16. | Sanchez-Munoz F, Dominguez-Lopez A, Yamamoto-Furusho JK. Role of cytokines in inflammatory bowel disease. World J Gastroenterol. 2008;14:4280-4288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 440] [Cited by in RCA: 517] [Article Influence: 30.4] [Reference Citation Analysis (2)] |
| 17. | Nielsen OH. New strategies for treatment of inflammatory bowel disease. Front Med (Lausanne). 2014;1:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12:205-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 930] [Cited by in RCA: 1238] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 19. | Amiot A, Peyrin-Biroulet L. Current, new and future biological agents on the horizon for the treatment of inflammatory bowel diseases. Therap Adv Gastroenterol. 2015;8:66-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 103] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 20. | Stickel F, Schuppan D. Herbal medicine in the treatment of liver diseases. Dig Liver Dis. 2007;39:293-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 218] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 21. | Langmead L, Rampton DS. Review article: complementary and alternative therapies for inflammatory bowel disease. Aliment Pharmacol Ther. 2006;23:341-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 118] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Hilsden RJ, Verhoef MJ, Best A, Pocobelli G. Complementary and alternative medicine use by Canadian patients with inflammatory bowel disease: results from a national survey. Am J Gastroenterol. 2003;98:1563-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Neuman MG. Immune dysfunction in inflammatory bowel disease. Transl Res. 2007;149:173-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 177] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 24. | Wang D, Dubois RN, Richmond A. The role of chemokines in intestinal inflammation and cancer. Curr Opin Pharmacol. 2009;9:688-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Brynskov J, Foegh P, Pedersen G, Ellervik C, Kirkegaard T, Bingham A, Saermark T. Tumour necrosis factor alpha converting enzyme (TACE) activity in the colonic mucosa of patients with inflammatory bowel disease. Gut. 2002;51:37-43. [PubMed] |
| 26. | Strober W, Fuss IJ. Proinflammatory cytokines in the pathogenesis of inflammatory bowel diseases. Gastroenterology. 2011;140:1756-1767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 887] [Cited by in RCA: 852] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 27. | Tillack C, Ehmann LM, Friedrich M, Laubender RP, Papay P, Vogelsang H, Stallhofer J, Beigel F, Bedynek A, Wetzke M. Anti-TNF antibody-induced psoriasiform skin lesions in patients with inflammatory bowel disease are characterised by interferon-γ-expressing Th1 cells and IL-17A/IL-22-expressing Th17 cells and respond to anti-IL-12/IL-23 antibody treatment. Gut. 2014;63:567-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 220] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 28. | Aldrich MB, Sevick-Muraca EM. Cytokines are systemic effectors of lymphatic function in acute inflammation. Cytokine. 2013;64:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 29. | Araki A, Nara H, Rahman M, Onoda T, Li J, Juliana FM, Jin L, Murata K, Takeda Y, Asao H. Role of interleukin-21 isoform in dextran sulfate sodium (DSS)-induced colitis. Cytokine. 2013;62:262-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Shin JH, Ryu JH, Kang MJ, Hwang CR, Han J, Kang D. Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts on the LPS-induced production of NO and pro-inflammatory cytokines by downregulating allicin activity in RAW 264.7 macrophages. Food Chem Toxicol. 2013;58:545-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Atreya I, Atreya R, Neurath MF. NF-kappaB in inflammatory bowel disease. J Intern Med. 2008;263:591-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 644] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 32. | Wang KP, Zhang C, Zhang SG, Liu ED, Dong L, Kong XZ, Cao P, Hu CP, Zhao K, Zhan YQ. 3-(3-pyridylmethylidene)-2-indolinone reduces the severity of colonic injury in a murine model of experimental colitis. Oxid Med Cell Longev. 2015;2015:959253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Spiik AK, Ridderstad A, Axelsson LG, Midtvedt T, Björk L, Pettersson S. Abrogated lymphocyte infiltration and lowered CD14 in dextran sulfate induced colitis in mice treated with p65 antisense oligonucleotides. Int J Colorectal Dis. 2002;17:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Islam MS, Murata T, Fujisawa M, Nagasaka R, Ushio H, Bari AM, Hori M, Ozaki H. Anti-inflammatory effects of phytosteryl ferulates in colitis induced by dextran sulphate sodium in mice. Br J Pharmacol. 2008;154:812-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 155] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 35. | Bruck R, Aeed H, Brazovsky E, Noor T, Hershkoviz R. Allicin, the active component of garlic, prevents immune-mediated, concanavalin A-induced hepatic injury in mice. Liver Int. 2005;25:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |