Published online Sep 7, 2017. doi: 10.3748/wjg.v23.i33.6181
Peer-review started: January 10, 2017
First decision: April 21, 2017
Revised: May 23, 2017
Accepted: June 9, 2017
Article in press: June 12, 2017
Published online: September 7, 2017
Processing time: 243 Days and 2.7 Hours
The prognosis of pancreatic cancer remains poor, even after initial surgical therapy. Local recurrence after Whipple’s pancreatico-duodenectomy may lead to intestinal obstruction at the level of the afferent limb or the alimentary limb. Endoscopic insertion of a self-expandable metal stent (SEMS) into the intestinal malignant stricture is the preferred method of choice for palliation. We describe two new endoscopic techniques to treat a malignant intestinal obstruction with the insertion of a SEMS into the afferent limb and the alimentary limb. A case of malignant gastric outlet obstruction after a Whipple’s resection was treated by the creation of an endoscopic gastrojejunostomy by the insertion of a lumen apposing HotAxios stent in between the stomach and the alimentary limb under fluoroscopic and endoscopic ultrasound control. Biliary obstruction and jaundice caused by a malignant stricture of the afferent limb after a Roux-en-Y Whipple’s resection was treated by the insertion of a SEMS by means of the single-balloon overtube-assisted technique under fluoroscopic control. Feasibility and advantages of both techniques are discussed.
Core tip: Malignant recurrence after Whipple’s pancreatico-duodenectomy is frequent and may lead to intestinal obstruction. Endoscopic palliation of the intestinal obstruction is challenging. We present 2 endoscopic techniques: Endoscopic ultrasound-guided creation of a gastrojejunostomy using a fully covered lumen apposing metal stent, and insertion of a self-expandable metal stent by means of the single-balloon overtube-assisted technique under fluoroscopic control.
- Citation: Mouradides C, Taha A, Borbath I, Deprez PH, Moreels TG. How to treat intestinal obstruction due to malignant recurrence after Whipple’s resection for pancreatic head cancer: Description of 2 new endoscopic techniques. World J Gastroenterol 2017; 23(33): 6181-6186
- URL: https://www.wjgnet.com/1007-9327/full/v23/i33/6181.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i33.6181
Whipple’s pancreatico-duodenectomy was named after Alan Oldfather Whipple who described the technique in 1935[1]. It still is the surgical treatment of choice to cure pancreatic head cancer[2]. Modifications of the technique have emerged, including pylorus-preserving Whipple’s resection and Roux-en-Y intestinal reconstruction[3]. After resection of the pancreatic head, both the remnant bile duct and pancreatic duct have to be anastomosed to the afferent limb (hepaticojejunostomy/pancreaticojejunostomy) and food passes through the alimentary limb. Despite the different surgical Whipple’s variations, the risk of local tumor recurrence after Whipple’s resection for pancreatic head cancer remains more than 50%[4]. Few cases present with malignant intestinal obstruction at the level of the afferent or the alimentary limb. Endoscopic palliative therapy by means of insertion of self-expandable metal stents (SEMS) is the preferred method of choice to treat malignant intestinal obstruction in case of pancreatic cancer[2]. However, endoscopic SEMS placement in the afferent or the alimentary limb remains a challenging procedure[5]. We report on the endoscopic treatment modalities of two cases of malignant intestinal obstruction due to tumor recurrence after Whipple’s pancreatico-duodenectomy.
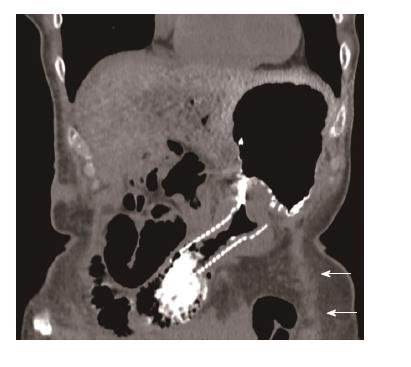
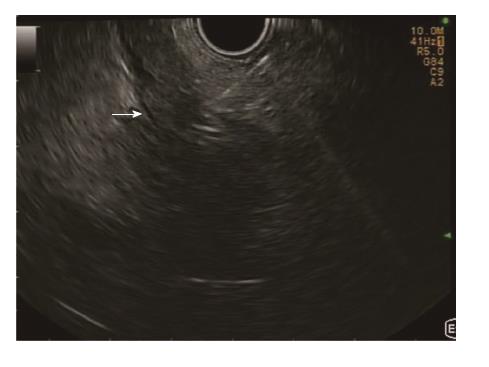
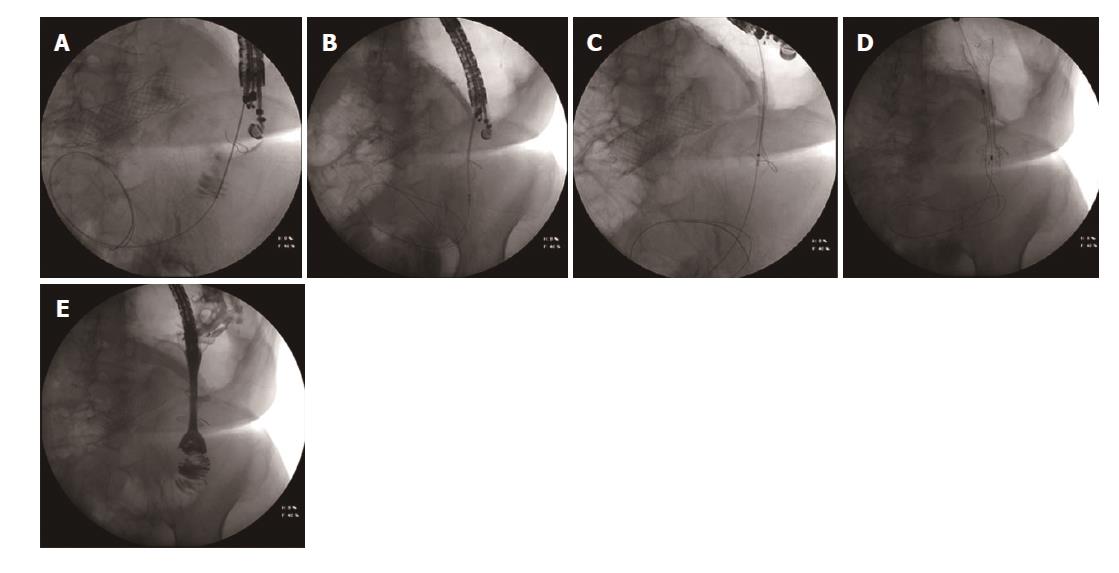
A 71 year-old woman was referred with symptoms of upper gastrointestinal obstruction because of local tumor recurrence at the level of the gastrojejunal anastomosis with peritoneal carcinomatosis. She underwent Whipple’s resection for pancreatic head cancer two years earlier. Initially, an uncovered enteral SEMS (Wallflex 60 x 22 mm, Boston Scientific) was inserted and ended up in the afferent limb, eventually obstructing the alimentary limb worsening the gastric outlet syndrome. CT scan confirmed the dilated afferent limb towards the hepaticojejunostomy, with food remnants and the empty alimentary limb underneath the stomach (Figure 1). Since the uncovered SEMS could not be removed from the afferent limb because of tumor ingrowth obstructing the entrance to the alimentary limb, we decided to create an endoscopic gastrojejunostomy, using the HotAxios device (XLumina Axios 10 mm x 15 mm, Boston Scientific), under endoscopic ultrasound (EUS) guidance (linear-array echoendoscope GF-UCT 180, Olympus) and fluoroscopy. The HotAxios device is a cystotome catheter with a preloaded covered lumen apposing metal stent. It is developed to drain pancreatic pseudocysts with an all-in-one device[6]. Here we used it to create an endoscopic gastrojejunostomy. The empty alimentary limb was identified by transgastric EUS, accessed with a 19 gauche needle (Figure 2), and confirmed fluoroscopically by intraluminal contrast dye injection. Next, a 0.035 inch guidewire was placed (Figure 3A), allowing smooth introduction of the HotAxios stent deployment system into the alimentary limb using electrocautery. The fully covered 10 mm HotAxios lumen apposing stent was deployed under fluoroscopic and endoscopic guidance, with the distal flange in the intestinal lumen, and the proximal flange in the stomach (Figure 3B). However, upon release, it immediately migrated outside the stomach because of the distance between the alimentary limb and the stomach (Figure 3C). A fully covered metal esophageal stent (Taewoong Medical Niti, 80 mm x 22 mm) was introduced over the guidewire and deployed inside the HotAxios stent, with the proximal part protruding into the gastric lumen (Figures 3D and E). After the procedure, the patient quickly resumed oral feeding.
Three months later, she was readmitted for vomiting due to intragastric migration of the esophageal stent. The HotAxios stent was still in place. A fully covered Nagi stent (Taewoong Medical, 20 mm x 16 mm) was placed inside the HotAxios stent, and the patient resumed oral feeding. Seven months after the initial presentation, she died due to malignant progression of the disease.
This case illustrates the feasibility of the HotAxios system in creating an EUS-guided gastrojejunostomy to treat malignant gastric outlet syndrome. This technique has recently emerged as an alternative to surgical gastrojejunostomy treating benign and malignant gastric outlet syndrome, with technical success rate of 92% and 85% clinical success[7-9]. Serious adverse events of this endoscopic ultrasound technique were reported in 11.5%, and encompass gastrointestinal perforation, peritonitis and bleeding[9]. We encountered another complication. After deployment of the HotAxios lumen apposing stent to create the gastrojejunostomy, the gastric flange migrated outside the stomach without the possibility to reposition it into the stomach. Since the guidewire was still in place, we were able to save the gastrojejunostomy by inserting a second fully covered oesophageal SEMS inside the HotAxios stent.
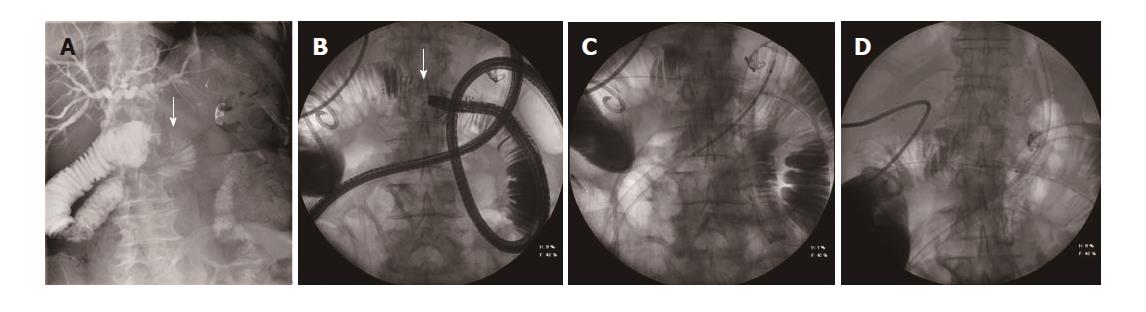
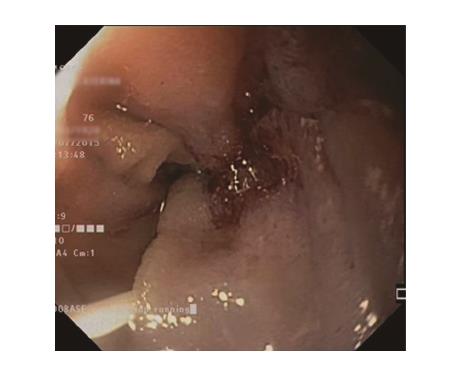
A 76-year-old woman who underwent Roux-en-Y Whipple’s resection two years earlier for pancreatic head cancer, was referred because of obstructive jaundice and dilated intrahepatic bile ducts. Percutaneous transhepatic cholangiography and biliary drainage excluded an obstruction at the level of the bilioenteric anastomosis. However, afferent limb syndrome was diagnosed based on the obstruction of the afferent limb 20 cm distally from the hepaticojejunostomy with a dilated intestinal segment between the hepaticojejunostomy and the enteral stricture of the afferent limb (Figure 4A). Next, we performed a single-balloon enteroscopy (SBE) through the Roux-en-Y anastomosis into the afferent limb under fluoroscopic guidance, and reached the jejunal stenosis, with endoscopic characteristics of a malignant stricture (Figure 5). The length of the stricture was estimated by means of the injection of water soluble contrast. A 0.035 inch guidewire was inserted into the stricture under endoscopic and fluoroscopic control, and a CRE dilation balloon (8-10 mm) was inserted over the guide wire to dilate the stricture. Biopsies confirmed the intestinal recurrence of a pancreas adenocarcinoma. After a multidisciplinary oncology discussion, a non-surgical endoscopic approach was suggested. One week later, a second SBE was performed in order to place a SEMS into the malignant stricture. Again, the length of the stricture was estimated by contrast injection under fluoroscopic control (Figure 4B). A 0.035 inch stiff guidewire (VisiGlide 450 cm, Olympus) was inserted into the dilated jejunal segment proximal of the stricture. The overtube of the SBE was anchored as close as possible near the malignant stricture with the balloon inflated. Next, the enteroscope was removed under fluoroscopic guidance, leaving the guidewire and the overtube in place. An uncovered SEMS (Wallflex 60 mm x 22 mm, Boston Scientific) was inserted over the guidewire through the overtube into the stricture, located by means of the previously injected contrast (Figure 4C). The stent was deployed under fluoroscopic guidance (Figure 4D). Afterwards, the enteroscope was reintroduced through the overtube to control for the correct positioning of the SEMS. The percutaneous biliary drain was removed and the patient was discharged two days later with normal oral food intake. Gemcitabine-based chemotherapy was started.
Three months later, she presented again with obstructive jaundice and afferent limb syndrome suggestive of tumor invasion of the uncovered SEMS. A third SBE procedure was performed, confirming the diagnosis of SEMS obstruction. We used the same single-balloon overtube-assisted technique to insert a new partially covered SEMS (ComVi Enteral Colonic Stent 100 mm x 22 mm, Taewoong) inside the uncovered SEMS. No complications were encountered. Ten months after the second SEMS insertion, she died due to malignant progression of the disease.
This case emphasizes the usefulness, feasibility and reproducibility of the single-balloon overtube-assisted technique for SEMS insertion in malignant strictures of the small intestine, especially in patients with altered anatomy such as Roux-en-Y anastomosis where conventional endoscopes cannot reach. Since the currently available enteral SEMS deployment catheters cannot be used through the working channel (2.8 or 3.2 mm) of the 200 cm long enteroscope, the SEMS is introduced over a long stiff guidewire through the balloon-anchored overtube under fluoroscopic control. This balloon-assisted overtube technique enables to relieve intestinal obstruction without surgical intervention by a combined endoscopic and fluoroscopic approach [10,11].
Malignant recurrence after (modified) Whipple’s
pancreatico-duodenectomy for pancreatic head adenocarcinoma remains high[4]. Sometimes, local recurrence may lead to the afferent limb syndrome (stricture of the afferent limb) or a gastric outlet-like syndrome (stricture of the alimentary limb) because of intestinal tumor infiltration. In the case of malignant intestinal obstruction following Whipple’s resection, palliative surgery is generally indicated to obtain symptom relief (resection of an intestinal segment, enterostomy or intestinal bypass)[12]. Case reports have shown that endoscopic enteral SEMS placement has become feasible, either by the creation of an EUS-guided gastrojejunostomy or by insertion of a SEMS by means of the balloon-assisted overtube technique[7-11]. We illustrated both procedures in two cases of malignant intestinal obstruction (afferent and alimentary limb obstruction) after Whipple’s resection.
Both patients underwent Whipple’s pancreatico-duodenectomy as a curative treatment of pancreatic head cancer. However, local tumor recurrence in the alimentary limb resulted in the gastric outlet syndrome (case 1) and local tumor recurrence in the afferent limb resulted in obstructive jaundice (case 2).
The patient with the gastric outlet syndrome presented with recurrent vomiting and weight loss (case 1). The patient with the afferent limb syndrome presented with fever, abdominal pain and jaundice.
Vomiting may be a side-effect of chemotherapy (gemcitabine) or may be caused by peptic ulcer disease (case 1). Obstructive jaundice may be the clinical sign of a postoperative stricture at the level of the hepaticojejunostomy (case 2).
The patient with the gastric outlet syndrome presented a slight increase in CA19.9 tumor marker (case 1). The patient with the afferent limb syndrome presented with elevated CRP and liver function tests (case 2).
Abdominal CT scan of the patient with the gastric outlet syndrome suspected peritoneal carcinomatosis (case 1). MRI-MRPC of the patient with the afferent limb syndrome suspected a postoperative stenosis at the level of the hepaticojejunostomy (case 2).
No histological biopsies were taken during the endoscopic ultrasound (EUS)-guided gastrojejunostomy procedure to confirm local tumor recurrence (case 1). During the first single-balloon enteroscopy biopsies were taken at the level of the afferent limb stricture, confirming the presence of a well-differentiated pancreatic adenocarcinoma (case 2).
Both patients were treated endoscopically in a palliative setting. The first patient underwent EUS-guided gastrojejunostomy followed by chemotherapy (Oxaliplatine) (case 1). The second patient underwent self-expandable metal stent (SEMS) insertion into the afferent limb followed by chemotherapy (Gemcitabine) (case 2).
The two endoscopic techniques presented here have been described previously under the form a case reports.
Whipple’s resection is the surgical curative treatment for pancreatic head cancer, with resection of the pancreatic head and the duodenum and the creation of a hepaticojejunostomy and a pancreaticojejunostomy on to the afferent jejunal limb. The afferent limb syndrome is caused by an obstruction at the level of the afferent limb after Whipple’s resection. The gastric outlet syndrome is caused by an obstruction at the level of the alimentary limb after Whipple’s resection.
Local tumor recurrence remains high after initial curative Whipple’s pancreatico-duodenectomy for pancreatic head cancer. The clinical presentation as the gastric outlet syndrome or the afferent limb syndrome is rare. New endoscopic techniques may allow to overcome these clinical syndromes by creating an EUS-guided gastrojejunostomy or by SEMS insertion into the afferent limb.
This is a well-written and illustrated overview of two endoscopic techniques for the palliation of intestinal obstruction due to local tumor recurrence after Whipple’s pancreatico-duodenectomy for pancreatic head cancer.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Belgium
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Przemioslo R S- Editor: Gong ZM L- Editor: A E- Editor: Huang Y
| 1. | Haubrich WS. Whipple of the Whipple operation. Gastroenterology. 2007;132:1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goéré D, Seufferlein T, Haustermans K, Van Laethem JL, Conroy T. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 Suppl 5:v56-v68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 905] [Cited by in RCA: 927] [Article Influence: 92.7] [Reference Citation Analysis (0)] |
| 3. | Griffin JF, Poruk KE, Wolfgang CL. Pancreatic cancer surgery: past, present, and future. Chin J Cancer Res. 2015;27:332-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 63] [Reference Citation Analysis (0)] |
| 4. | Mu DQ, Peng SY, Wang GF. Risk factors influencing recurrence following resection of pancreatic head cancer. World J Gastroenterol. 2004;10:906-909. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Johnsson E, Delle M, Lundell L, Liedman B. Transhepatic placement of an enteral stent to treat jaundice in a tumor recurrence obstructed afferent loop after a whipple procedure. Dig Surg. 2003;20:329-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Patil R, Ona MA, Papafragkakis C, Anand S, Duddempudi S. Endoscopic ultrasound-guided placement of AXIOS stent for drainage of pancreatic fluid collections. Ann Gastroenterol. 2016;29:168-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Binmoeller KF, Shah JN. Endoscopic ultrasound-guided gastroenterostomy using novel tools designed for transluminal therapy: a porcine study. Endoscopy. 2012;44:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (16)] |
| 8. | Shah A, Khanna L, Sethi A. Treatment of afferent limb syndrome: novel approach with endoscopic ultrasound-guided creation of a gastrojejunostomy fistula and placement of lumen-apposing stent. Endoscopy. 2015;47 Suppl 1 UCTN:E309-E310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, Peñas I, de la Serna C, Shah J, Binmoeller K, Gaidhane M, Grimm I, Baron T. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016;4:E276-E281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 174] [Cited by in RCA: 179] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 10. | Popa D, Ramesh J, Peter S, Wilcox CM, Mönkemüller K. Small Bowel Stent-in-Stent Placement for Malignant Small Bowel Obstruction Using a Balloon-Assisted Overtube Technique. Clin Endosc. 2014;47:108-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Nakahara K, Okuse C, Matsumoto N, Suetani K, Morita R, Michikawa Y, Ozawa S, Hosoya K, Kobayashi S, Otsubo T. Enteral metallic stenting by balloon enteroscopy for obstruction of surgically reconstructed intestine. World J Gastroenterol. 2015;21:7589-7593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Kofokotsios A, Papazisis K, Andronikidis I, Ntinas A, Kardassis D, Vrochides D. Palliation With Endoscopic Metal Stents May Be Preferable to Surgical Intervention for Patients With Obstructive Pancreatic Head Adenocarcinoma. Int Surg. 2015;100:1104-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |