Published online Jun 7, 2017. doi: 10.3748/wjg.v23.i21.3900
Peer-review started: November 15, 2016
First decision: January 10, 2017
Revised: February 7, 2017
Accepted: March 31, 2017
Article in press: March 31, 2017
Published online: June 7, 2017
Processing time: 205 Days and 6.8 Hours
To assess the role of three-dimensional endoanal ultrasound (3D-EAUS) for morphological assessment of the anal sphincter of female patients with chronic proctalgia (CP).
In this unmatched case control study, 30 consecutive female patients with CP and 25 normal women (control group) were enrolled. 3D-EAUS was performed in all subjects. Thickness and length of internal anal sphincter (IAS), thickness of puborectalis muscle (PR), length of the external anal sphincter (EAS) plus PR, and puborectalis angle were measured and compared between the two groups.
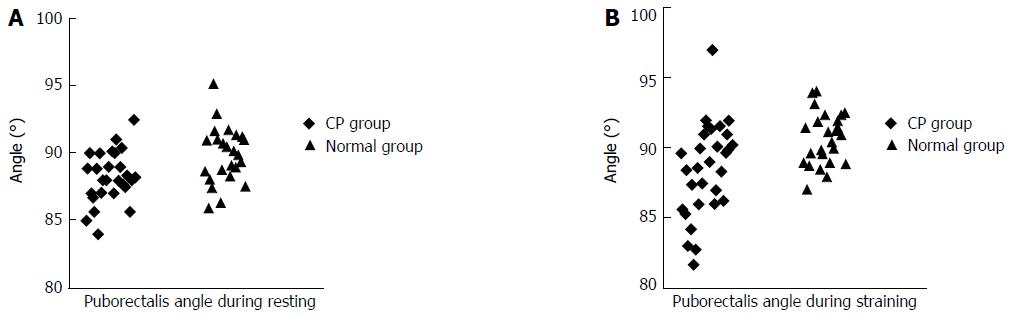
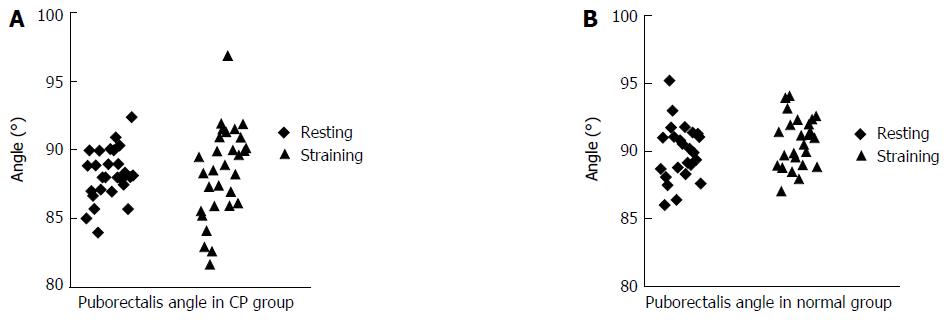
Patients with CP had significantly shorter IAS length and greater PR thickness, as compared to those in normal individuals (26.28 ± 3.59 mm vs 28.87 ± 4.84 mm, P < 0.05 and 9.67 ± 1.57 mm vs 8.85 ± 0.97 mm, P < 0.05, respectively). No significant between-group differences were observed with respect to IAS thickness and the EAS plus PR length (P > 0.05). Puborectalis angle in the CP group was significantly decreased, both in resting (88.23° ± 1.81° vs 89.94° ± 2.07° in control group, P < 0.05) and straining (88.47° ± 3.32° vs 90.72° ± 1.87° in control group, P < 0.05) phases, which suggest the presence of paradoxical contraction of PR in patients with CP. In the CP group, no significant difference in puborectalis angle was observed between the resting and straining phases (88.23° ± 1.81° vs 88.47° ± 3.32° respectively, P > 0.05).
The association of greater PR thickness and paradoxical contraction of PR with CP suggest their potential value as markers of CP.
Core tip: This study prospectively evaluated the anal sphincter morphology and function of chronic proctalgia (CP) in female patients by three-dimensional endoanal ultrasound. Here, we employed puborectalis angle to assess the paradoxical contraction of the puborectalis muscle (PR) in CP. The PR thickness and paradoxical contraction of PR are associated with CP, which may be promising diagnosis factors for CP.
- Citation: Xue YH, Ding SQ, Ding YJ, Pan LQ. Role of three-dimensional endoanal ultrasound in assessing the anal sphincter morphology of female patients with chronic proctalgia. World J Gastroenterol 2017; 23(21): 3900-3906
- URL: https://www.wjgnet.com/1007-9327/full/v23/i21/3900.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i21.3900
Chronic proctalgia (CP) is a type of functional anorectal disorder (FAD), which includes functional fecal incontinence, functional defecation disorders and functional anorectal pain (including CP and proctalgia fugax). According to the Rome III diagnostic criteria, CP refers to chronic or recurrent pain in the anal canal or rectum lasting at least 20 min, in the absence of any underlying organic disease (Table 1)[1-3]. CP can be further classified into levator ani syndrome and unspecified functional anorectal pain, based on the presence or absence of tenderness on posterior traction on the puborectalis[4]. CP has also been referred to as chronic idiopathic perineal pain, pyriformis syndrome, puborectalis syndrome, and levator spasm[5]. The epidemiology of CP is not well characterized, due to a relative paucity of research as well as the lack of standardized definition used in the published literature. An estimated 6.6% of the general population is affected by chronic or recurring pain in the anal region[2]. However, the morbidity burden from CP is not clear.
| 1 Presence of all of the following for at least 6 mo: (1) chronic or recurrent rectal pain or aching; (2) duration of episode: at least 20 minutes; and (3) exclusion of other causes of rectal pain (such as ischemia, abscess, fissure, coccygodynia and hemorrhoids) |
| 1.1 Levator ani syndrome: meet the diagnostic criteria for chronic proctalgia, and tenderness on posterior traction on puborectalis |
| 1.2 Unspecified functional anorectal pain: meet the diagnostic criteria for chronic proctalgia, and no tenderness on posterior traction on puborectalis |
Levator ani muscle spasm is believed to be the pathophysiological basis for levator ani syndrome[6]. However, the pathophysiology of CP is still far from clear. Diagnosis of CP is mainly based upon characteristic symptoms, physical findings and exclusion of organic disease[1]. Furthermore, the diagnosis of CP is not straightforward owing to the considerable overlap of symptoms with other causes of chronic pelvic pain. Therefore, investigation of the specific pathological and imaging characteristics is important for the diagnosis and treatment of CP.
Recent studies have employed use of modern diagnostic modalities such as endoanal ultrasound (EAUS), magnetic resonance imaging (MRI), and computerized tomography (CT) to explore the pathophysiology of FAD[7]. Compared with other imaging modalities, EAUS has several advantages, including the lack of exposure to ionizing radiation, minimal patient discomfort and its relative ease of use, short time requirement and low cost[8]. Three-dimensional (3D)-EAUS is a novel ultrasound technique, which provides for more reliable and accurate anatomical delineation of the anal canal than two-dimensional (2D)-EAUS[9]. 3D-EAUS is being increasingly used to diagnose pelvic floor disorders, such as anismus, rectocele and rectal intussusception[10-12]. For instance, Dietz et al[13] used 3D ultrasound for anatomical and functional assessment of levator ani muscles and the pelvic floor hiatus. However, the role and accuracy of 3D-EAUS in the diagnosis of CP is still unknown.
In the present study, we employed 3D-EAUS to assess the anal sphincter and puborectalis muscle (PR) in patients with CP. We observed significant differences in the morphology of anal sphincter and PR in patients with CP and normal individuals.
The study was approved by the hospital ethics committee. Written informed consent was obtained from all patients. Between February 2013 and December 2015, consecutive female patients with CP were prospectively enrolled in this study. The diagnosis of CP was based on the Rome III diagnostic criteria (Table 1). Exclusion criteria included any organic cause of pain, such as ischemia, abscess, fissure, hemorrhoid and so on. In addition, normal people were enrolled as a control group. All participants included in the study underwent 3D-EAUS examination. Data on clinical characteristics, physical examination, and ultrasound imaging were collected.
3D-EAUS was performed by a proctological surgeon experienced in EAUS and using the B-K 2050 transducer (B-K Medical, Herlev, Denmark) with a 360° rotating head and working frequency range of 9-16.0 MHz. The probe, on insertion into the anus, automatically scans the lower rectum and anal canal from proximal to distal directions in less than 1 min. 3D images were obtained without changing the position of the probe. All patients were evaluated in the left-lateral position without any prior bowel preparation. Examination was preceded by a digital rectal examination. After the patient had relaxed the anal sphincter, the probe (covered with a condom and adequate lubrication) was inserted through the anus into the lower rectum for approximately 6 cm, and the scans were obtained.
3D-EAUS can accurately delineate the anatomy of the anal canal at three levels. Three planes are generally distinguished in the anal canal: (1) the lower level includes the subcutaneous part of the external anal sphincter (EAS); (2) the mid level includes the superficial part of the EAS, the longitudinal muscle (LM) and the internal anal sphincter (IAS); and (3) the upper level includes the PR, the deep part of the EAS, and the IAS. Data on the following five parameters were obtained in a left lateral position and subjected to analysis.
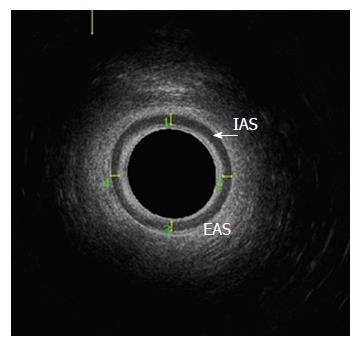
Thickness of IAS: Mean thicknesses of IAS at the 12, 3, 6 and 9 o’clock positions were calculated in the mid-axial plane (Figure 1).
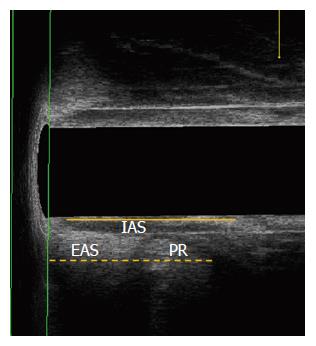
Length of IAS: Measured as the distance from the proximalis to the distalis of the IAS in the posterior anal canal, in the mid-sagittal plane (Figure 2).
Length of EAS plus PR: The distance from the edge of the subcutaneous portion of the EAS to the point of termination of the puborectalis muscle, in the mid-sagittal plane (Figure 2).
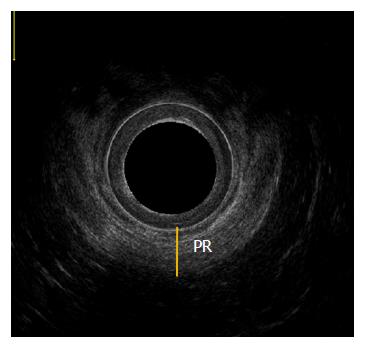
Thickness of puborectalis muscle: Measured as the distance from the inner edge to the outer edge of U-shaped puborectalis muscle at the 6 o’clock position, in the distal-axial plane (Figure 3).
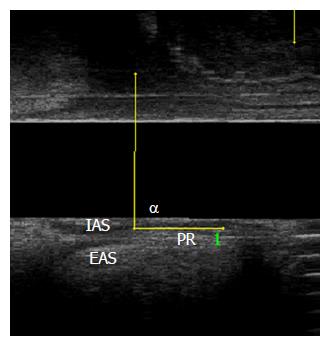
Puborectalis angle (α angle)[10]: The angle formed by the confluence of a line traced parallel to the internal edge of the puborectalis muscle (1.5 cm long) and another vertical line according to the anal canal axis calculated at rest and during straining (Figure 4). During the process of straining, all subjects were asked to relax during the first 15 s and to strain in the next 20 s. Finally, the subject was asked to relax again for 20 s and then images were obtained. The increase in puborectalis angle between the resting and straining is > 1° in normal individuals. Less than 1° increase indicates paradoxical contraction of PR, which is a clinically significant sign for the diagnosis of animus[14].
SPSS version 16.0 (SPSS Inc., Chicago, IL, United States) was used for data analysis. Data is expressed as mean ± SD. Between-group differences were assessed using t-test. P < 0.05 was considered indicative of a statistically significant difference.
Based on our diagnostic and exclusion criteria, a total of 30 female patients with CP (median age, 53.3 years; range, 33-77 years) were eventually included in this study. Meanwhile, 25 normal females (median age, 47.2 years; range, 21-72 years) were enrolled as a control group. Mean body mass index of patients and normal controls were 22.40 ± 2.92 kg/m2 (range, 18 to 29.1 kg/m2) and 22.21 ± 2.48 kg/m2 (range, 18.7 to 28.3 kg/m2) respectively. Among the patients, 7 (23.3%) had undergone Caesarian section and 23 (76.7%) had vaginal deliveries. In the control group, 4 (16%) were nulliparous, 7 (28%) had a Caesarian section and 14 (56%) had vaginal deliveries. In the CP group, the mean duration of symptoms at presentation was 52.8 (± 75.03) mo (range, 6-240 mo). Mean visual analog scale (VAS) score was 6.65 (± 2.11) (range, 3-10), including 2 mild cases (0 to 3 VAS), 12 moderate cases (4 to 6 VAS), and 16 severe cases (7 to 10 VAS). The types of pain were bearing-down pain (n = 22), persistent rough pain (n = 4), twitching pain (n = 2), and colicky pain (n = 2). The sites of pain included perianal region (n = 10), internal anal (n = 11), rectum (n = 7) and perineum (n = 2).
Out of the 30 patients, 10 (33.3%) had levator ani syndrome and 20 (66.7%) had unspecified functional anorectal pain based on the presence or absence of tenderness elicited by posterior traction on the puborectalis. Nine (30%) patients also had outlet obstructive constipation (OOC) and 5 patients (16.7%) had stress urinary incontinence.
Sphincter damage was not observed in any of the patients. The mean length of IAS in the CP group was significantly shorter than that in the control group (26.28 ± 3.59 mm vs 28.87 ± 4.84 mm, P < 0.05; Table 2). In addition, PR thickness in the CP group was significantly thicker than that in the control group (9.67 ± 1.57 mm vs 8.85 ± 0.97 mm, P < 0.05; Table 2). However, no significant between-group differences were observed with respect to the IAS thickness and EAS + PR thickness (P > 0.05). Compared with the control group, the puborectalis angles in the CP group were significantly smaller during the resting and straining phases (88.23° ± 1.81° vs 89.94° ± 2.07°, P < 0.05 and 88.47° ± 3.32° vs 90.72° ± 1.87°, P < 0.05 respectively) (Figure 5A and B). In the CP group, no significant difference in the puborectalis angle was observed between the resting position (88.23° ± 1.81°) and the straining position (88.47° ± 3.32°) (P > 0.05; Figure 6A). In the control group, the puborectalis angle in the resting position was significantly decreased as compared to that in the straining position (89.94° ± 2.07° vs 90.72° ± 1.87°, P < 0.05; Figure 6B)
| Parameter | CP in mm | Control in mm | P value |
| IAS length | 26.28 ± 3.59 | 28.87 ± 4.84 | < 0.05 |
| IAS thickness | 1.76 ± 0.43 | 1.63 ± 0.38 | NS |
| EAS + PR length | 30.71 ± 4.48 | 31.40 ± 4.43 | NS |
| PR thickness | 9.67 ± 1.57 | 8.85 ± 0.97 | < 0.05 |
CP is a common disease that belongs to the chronic pelvic pain conditions, and is a non-malignant persistent or recurrent pain perceived in structures related to the pelvis[15]. It has been reported that chronic or recurring pain in the anal region is a prevalent symptom that affects an estimated 6.6% of the population[2]. CP is common disease in females. About half of all patients included in this study suffered severe pain (VAS score 7-10). In most cases, pain was experienced in the perianal region and inner anus, which is consistent with data reported by Atkin and colleagues[4]. Unspecified functional anorectal pain is the most common type of CP; it accounted for 66.7% of all patients in the present study. Previous studies have reported an association of CP with OOC[3,16]. In the present study, 9 out of 30 female patients had OOC.
Some advances have been achieved in the diagnosis and treatment of CP[4,17,18]. However, the etiology and pathophysiology of CP is not well understood. In this study, we employed 3D-EAUS to assess the IAS, EAS and PR in the perianal area of female patients with CP.
Internal anal sphincter thickness correlates with resting anal pressure. Patients with proctalgia fugax were shown to have greater thickness of the internal anal sphincter, which may correlate with increased resting anal pressure[19]. It was reported that the patient with CP also has a high resting anal pressure[20]. Therefore, we supposed that the high resting anal pressure in CP may result in a high IAS thickness. To our knowledge, IAS thickness in patients with CP has not been reported. In this study, we measured the thickness and length of the IAS by 3D-EAUS[11,21]. Our data showed that the IAS thickness in patients with CP was not significantly different from that in normal individuals, which suggests that the thickness of IAS may not be associated with CP. We did not measure the EAS thickness because it is more difficult to define the borders of EAS with endoanal ultrasound owing to EAS showing low contrast with the surrounding hyperechoic fatty tissue[22,23].
Several studies have shown that IAS thickness is a more reliable and reproducible parameter than EAS thickness[24]. In addition, we also measured the length of IAS in the posterior portion of the anal canal in the mid-sagittal plane. Our data revealed shorter IAS length in patients with CP, as compared to that in normal individuals. The underlying reason for this is not clear. Some previous studies on normal female subjects did not show any association of IAS length with age and reproductive history[24,25]. However, the situation in CP is unclear. Since it is difficult to identify the demarcation between the edges of EAS and PR in the proximal portion of the anal canal, we measured the length of EAS plus PR, and did not measure the EAS length or PR length separately. However, no significant difference was observed in the length of EAS plus PR between the two groups. In addition, we also observed that the PR thickness of the CP patient was higher than that of the normal individuals. Increasing PR thickness may be a characteristic of CP, representing a promising diagnostic marker for CP.
Three-dimensional endosonography is also used to diagnose anismus by measuring puborectalis angle (α angle), which is a useful parameter to detect paradoxical contraction of PR[10,26]. Normally, the puborectalis angle will increase during straining by > 1°. It is consistent with our findings in the normal individuals in this study. However, no significant difference in puborectalis angle was observed between the straining and resting positions in the CP group. Additionally, the puborectalis angles, both in resting and straining positions, in the CP group were less than those in the control group. All these findings point towards paradoxical contraction of the PR in CP. We had earlier[27] detected paradoxical contraction of the PR in CP using pelvic floor surface electromyography, which is consistent with our findings based on 3D-EAUS. However, the relationship between high PR thickness and paradoxical contraction is not known and requires further study.
In this study, we, for the first time, employed 3D-EAUS to assess the perianal parameters (i.e., IAS, EAS and PR) of female patients with CP. We found increasing PR thickness and decreasing puborectalis angle in CP. However, our results are based on a small sample size of 30 female patients only, which is the main limitation along with sex bias. Therefore, it is necessary to conduct more studies with larger sample sizes and without sex selection in order to achieve a more objective and homogeneous assessment of CP.
In conclusion, our data suggests that high PR thickness and paradoxical PR contraction are associated with CP, and which may be potential diagnostic markers of CP.
Chronic proctalgia (CP) is pain located in the anal canal or rectum without any underlying organic disease, which is considered related to pelvic floor dysfunction, containing hypertonicity, hypotonicity and instability. In a previous study, we demonstrated that pelvic floor muscle dysfunction is the main feature of patients with CP by testing the characteristics of pelvic floor surface electromyography. Here, we used three-dimensional endoanal ultrasound (3D-EAUS) to explore its morphological characteristics and try to find some new features of CP.
3D-EAUS has been widely used in diagnosing anorectal diseases, like fistula, anal abscess and anorectal tumor, and also in functional diseases, such as constipation and fecal incontinence. In this study, these results displayed that greater puborectalis muscle (PR) thickness and paradoxical contraction of PR are the potential value as markers of CP.
In the present study, the authors employed 3D-EAUS to assess the morphology of the anal sphincter of female patients with CP. It was demonstrated that greater puborectalis muscle (PR) thickness and paradoxical contraction of PR are associated with CP, suggesting that they may be promising diagnosing factors for CP.
This study introduces a new evaluation method for CP. 3D-EAUS can not only exclude organic diseases of the anorectum, but also accurately measure length and thickness of the anal sphincter. It may be a promising technique to be used in diagnosing CP.
CP - Chronic or recurrent pain in the anal canal or rectum lasting at least 20 min, in the absence of any underlying organic disease. Puborectalis angle - The angle can be only measured under 3D-EAUS. In the sagittal plane, the angle formed by the confluence of a line traces parallel to the internal edge of the puborectalis muscle and another vertical line according to the anal canal axis, which can reflect the movement of puborectalis muscle at rest and during straining.
The authors have performed a good study, and only need to correct some writing issues.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Garcia-Olmo D, Guedea MA, Parellada CM S- Editor: Gong ZM L- Editor: Filipodia E- Editor: Zhang FF
| 1. | Thompson WG, Irvine EJ, Pare P, Ferrazzi S, Rance L. Functional gastrointestinal disorders in Canada: first population-based survey using Rome II criteria with suggestions for improving the questionnaire. Dig Dis Sci. 2002;47:225-235. [PubMed] |
| 2. | Boyce PM, Talley NJ, Burke C, Koloski NA. Epidemiology of the functional gastrointestinal disorders diagnosed according to Rome II criteria: an Australian population-based study. Intern Med J. 2006;36:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 3. | Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006;130:1510-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 340] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 4. | Atkin GK, Suliman A, Vaizey CJ. Patient characteristics and treatment outcome in functional anorectal pain. Dis Colon Rectum. 2011;54:870-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Chiarioni G, Asteria C, Whitehead WE. Chronic proctalgia and chronic pelvic pain syndromes: new etiologic insights and treatment options. World J Gastroenterol. 2011;17:4447-4455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 6. | Hull TL, Milsom JW, Church J, Oakley J, Lavery I, Fazio V. Electrogalvanic stimulation for levator syndrome: how effective is it in the long-term? Dis Colon Rectum. 1993;36:731-733. [PubMed] |
| 7. | West RL, Dwarkasing S, Briel JW, Hansen BE, Hussain SM, Schouten WR, Kuipers EJ. Can three-dimensional endoanal ultrasonography detect external anal sphincter atrophy? A comparison with endoanal magnetic resonance imaging. Int J Colorectal Dis. 2005;20:328-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Santoro GA, Wieczorek AP, Dietz HP, Mellgren A, Sultan AH, Shobeiri SA, Stankiewicz A, Bartram C. State of the art: an integrated approach to pelvic floor ultrasonography. Ultrasound Obstet Gynecol. 2011;37:381-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Garcés-Albir M, García-Botello SA, Espi A, Pla-Martí V, Martin-Arevalo J, Moro-Valdezate D, Ortega J. Three-dimensional endoanal ultrasound for diagnosis of perianal fistulas: Reliable and objective technique. World J Gastrointest Surg. 2016;8:513-520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Murad-Regadas SM, Regadas FS, Rodrigues LV, Souza MH, Lima DM, Silva FR, Filho FS. A novel procedure to assess anismus using three-dimensional dynamic anal ultrasonography. Colorectal Dis. 2007;9:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Regadas FS, Murad-Regadas SM, Lima DM, Silva FR, Barreto RG, Souza MH, Regadas Filho FS. Anal canal anatomy showed by three-dimensional anorectal ultrasonography. Surg Endosc. 2007;21:2207-2211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Vitton V, Vignally P, Barthet M, Cohen V, Durieux O, Bouvier M, Grimaud JC. Dynamic anal endosonography and MRI defecography in diagnosis of pelvic floor disorders: comparison with conventional defecography. Dis Colon Rectum. 2011;54:1398-1404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 372] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 14. | Murad-Regadas SM, Regadas FS, Barreto RG, Rodrigues LV, de Souza MH. A novel two-dimensional dynamic anal ultrasonography technique to assess anismus comparing with three-dimensional echodefecography. Colorectal Dis. 2009;11:872-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, Oberpenning F, de C Williams AC. EAU guidelines on chronic pelvic pain. Eur Urol. 2010;57:35-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 255] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 16. | Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. Functional Anorectal Disorders. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 324] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 17. | Chiarioni G, Nardo A, Vantini I, Romito A, Whitehead WE. Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology. 2010;138:1321-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Park DH, Yoon SG, Kim KU, Hwang DY, Kim HS, Lee JK, Kim KY. Comparison study between electrogalvanic stimulation and local injection therapy in levator ani syndrome. Int J Colorectal Dis. 2005;20:272-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Kamm MA, Hoyle CH, Burleigh DE, Law PJ, Swash M, Martin JE, Nicholls RJ, Northover JM. Hereditary internal anal sphincter myopathy causing proctalgia fugax and constipation. A newly identified condition. Gastroenterology. 1991;100:805-810. [PubMed] |
| 20. | Grimaud JC, Bouvier M, Naudy B, Guien C, Salducci J. Manometric and radiologic investigations and biofeedback treatment of chronic idiopathic anal pain. Dis Colon Rectum. 1991;34:690-695. [PubMed] |
| 21. | Knowles AM, Knowles CH, Scott SM, Lunniss PJ. Effects of age and gender on three-dimensional endoanal ultrasonography measurements: development of normal ranges. Tech Coloproctol. 2008;12:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Gold DM, Halligan S, Kmiot WA, Bartram CI. Intraobserver and interobserver agreement in anal endosonography. Br J Surg. 1999;86:371-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Beets-Tan RG, Morren GL, Beets GL, Kessels AG, el Naggar K, Lemaire E, Baeten CG, van Engelshoven JM. Measurement of anal sphincter muscles: endoanal US, endoanal MR imaging, or phased-array MR imaging? A study with healthy volunteers. Radiology. 2001;220:81-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Bollard RC, Gardiner A, Lindow S, Phillips K, Duthie GS. Normal female anal sphincter: difficulties in interpretation explained. Dis Colon Rectum. 2002;45:171-175. [PubMed] |
| 25. | Starck M, Bohe M, Fortling B, Valentin L. Endosonography of the anal sphincter in women of different ages and parity. Ultrasound Obstet Gynecol. 2005;25:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Murad-Regadas SM, Regadas FS, Rodrigues LV, Silva FR, Soares FA, Escalante RD. A novel three-dimensional dynamic anorectal ultrasonography technique (echodefecography) to assess obstructed defecation, a comparison with defecography. Surg Endosc. 2008;22:974-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 27. | Xue YH, Ding SQ, Ding YJ, Wang J, Li M, Cao JB, Zhou HF. Diagnostic value of pelvic floor surface electromyography in functional anorectal pain. Shijie Huaren Xiaohua Zazhi. 2014;10:1471-1474. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |