Published online Feb 28, 2016. doi: 10.3748/wjg.v22.i8.2545
Peer-review started: July 30, 2015
First decision: October 15, 2015
Revised: November 4, 2015
Accepted: December 19, 2015
Article in press: December 19, 2015
Published online: February 28, 2016
Processing time: 211 Days and 1.8 Hours
AIM: To analyze the clinical and pathological parameters and expression of the neural cell adhesion molecule (CD56) in patients with biliary atresia (BA).
METHODS: Established clinical laboratory markers of hepatic function, including enzyme activity, protein synthesis, and bilirubin metabolism, were evaluated in patients with BA and compared with those in patients with choledochal cysts and neonatal hepatitis. Pathological changes in tissue morphology and fibrosis were examined by histological and tissue collagen staining. Immunohistochemical staining for the biliary epithelial cell markers CD56 and CK19 together with the Notch signaling related molecules Notch1 and Notch2 was performed in the context of alterations in the structure of intrahepatic biliary ducts.
RESULTS: Differences in some clinical laboratory parameters among the three diseases examined were observed, but they did not correlate with the pathological classification of fibrosis in BA. Immunohistochemical staining showed the presence of CD56-positive immature bile ducts in most patients (74.5%) with BA but not in patients with choledochal cysts or neonatal hepatitis. The number of CD56-expressing cells correlated with disease severity, with more positive cells present in the later stages of liver damage (81.8% vs 18.2%). Furthermore, bile plugs were mainly found in CD56-positive immature biliary ducts. Notch signaling was a key regulatory pathway in biliary duct formation and played a role in tissue fibrosis. Notch1 was co-expressed in CD56-positive cells, whereas Notch2 was found exclusively in blood vessels in the portal area of patients with BA.
CONCLUSION: The maturation of biliary epithelial cells and the expression of Notch may play a role in the pathogenesis of BA.
Core tip: Clinical laboratory parameters did not correlate with tissue fibrosis in patients with biliary atresia (BA). Immunohistochemical staining showed that CD56-positive immature bile ducts were present only in patients with BA but not in those with choledochal cyst or neonatal hepatitis. The number of CD56 expressing cells correlated with disease severity, with more positive cells present in the later stages of liver damage. Furthermore, the signaling molecule Notch1, but not Notch2, was co-expressed in CD56 positive cells. Our data provide new insights into the pathogenesis of BA in terms of biliary epithelial cell maturation and Notch expression.
- Citation: Zhang RZ, Yu JK, Peng J, Wang FH, Liu HY, Lui VC, Nicholls JM, Tam PK, Lamb JR, Chen Y, Xia HM. Role of CD56-expressing immature biliary epithelial cells in biliary atresia. World J Gastroenterol 2016; 22(8): 2545-2557
- URL: https://www.wjgnet.com/1007-9327/full/v22/i8/2545.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i8.2545
Biliary atresia (BA) is an infantile disorder that affects both intrahepatic and extrahepatic bile ducts, with progressive tissue fibrosis leading to irreversible liver cirrhosis[1]. With advances in clinical care and the availability of Kasai portoenterostomy to re-establish bile drainage, mortality has been significantly reduced; however, patients may still develop cirrhosis without liver transplantation[1,2]. The etiology of BA is still not fully understood, although a variety of pathological processes, such as viral infection[3], dysregulation of the immune system[4], and genetic defects, have been reported[5] in animal models and patients. It has also been proposed that the condition is multifactorial[6]. As transplantation is limited, advancing our knowledge on the pathological processes, such as inflammation and fibrosis, in BA may identify new therapeutic targets for treatment.
In patients with BA, an increase in bile ductules as the disease develops has been demonstrated, a process that is suggested to be associated with liver regeneration[7]. However, the function of these ductules is not fully understood, especially in liver fibrosis. Several markers have been used to differentiate biliary epithelial cells (BECs) from other hepatic cells and blood vessels. The most commonly used marker is cytokeratin 7 (CK7), which stains all BECs but also reacts with some progenitor hepatocytes[8]. Some investigators have used CD56 (neural cell adhesion molecule, NCAM) to identify immature BECs and epithelial cell adhesion molecule (EpCAM) as a marker of mature BECs, and antibodies specific for these molecules have been successfully used to isolate BECs from animal and human samples[9]. The expression of CD56 in patients with BA has been described in some studies[10,11], however, the function and relationship of this marker with the pathological changes that occur in BA have not been well studied.
Notch signaling plays a key role in the development of the biliary system[12]. Alagille syndrome is caused by mutations in Jagged1, which encodes a ligand for Notch1, resulting in a loss of bile duct structure in the portal tracts[13]. However, Notch signaling contributes to the pathology of carbon tetrachloride-induced liver fibrosis in an animal model, and use of the inhibitor γ-secretase reduces fibrosis[14]. In addition, in Alagille syndrome, although cholestasis is severe, progression to biliary cirrhosis is rare[15], further indicating that Notch1-mediated signaling contributes to tissue fibrosis. Notch2 functions in normal peri- and post-natal formation of the intrahepatic bile duct (IHBD), and low expression of this receptor causes malformation of the IHBD. Notch2 can also influence the development of blood vessels[16]. As the pathological processes in BA include the formation of neo-ductules and tissue fibrosis, the function of Notch signaling in BA warrants investigation.
In this study, we report differences in serum levels of markers of bile metabolism, i.e., total bilirubin (TBIL), direct bilirubin (DBIL), and total bile acid levels (TBA), in three cholestatic diseases: BA, neonatal hepatitis (NH), and choledochal cysts (CCs). Significantly higher levels of TBIL, DBIL, and TBA were found in patients with BA and NH compared to those with CC, which suggests that the liver, but not extra-hepatic structures, influences function. In addition, we noted that gamma-glutamyl transferase (γ-GT), which reflects involvement of BECs, was increased in BA, but was less pronounced in NH. Detailed analysis of the phenotype of BECs in the context of CD56, EpCAM, and CK7 expression was performed in order to determine the different stages of maturation. Biliary epithelial cells stained for CD56 were present in higher numbers in patients with BA compared to those with CC or NH, which implies that neo-BECs might contribute directly to liver fibrosis. As Notch signaling is related to tissue fibrosis, increased expression of Notch1 in these cells suggests that CD56-related Notch signaling may also be involved in the pathogenesis of BA.
The Trichrome Stain (Masson) Kit, Sirius Red, and other chemical reagents used were purchased from Sigma (Sigma-Aldrich Corporation, St Louis, MO, United States). Antibodies used were mouse anti-human CD56 (Dako Denmark, Glostrup, Denmark), mouse anti-human EpCAM, and mouse anti-human CK7 (Santa Cruz Biotechnology, Dallas, TX, United States), rabbit anti-human Notch1 (Cell Signaling Technology, Beverly, MA, United States), and rabbit anti-human Notch2 (Bethyl Laboratories, Montgomery, TX, United States).
Patients’ medical histories were obtained from the patient record system of Guangzhou Women and Children’s Medical Center, China. Clinical information relevant to this study is shown in Table 1. The age of patients with BA and NH was often less than 1 year, whereas the age of patients with CC varied from 4 months to 10 years, therefore, the latter group was further categorized by age (i.e., CC-AM < 1 year old) and then compared. The experimental protocols were approved by the Medical Ethics Committee of Guangzhou Women and Children’s Medical Center.
To compare differences in the biochemical parameters for BA, CC, and NH, the serum levels of 10 biochemical parameters were measured and analyzed. The serum samples were obtained from patients before surgery and were analyzed using a Hitachi Pre-Analytical Process Automation System with a 7600 Clinical Analyzer. The 10 parameters analyzed were alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ-GT, total protein (TP), albumin (ALB), globulin (GLO), TBIL, DBIL, indirect bilirubin (IBIL), and TBA.
Tissue fibrosis is one of the key pathophysiological changes in patients with BA and is often an indicator of an adverse clinical outcome. The deposition of tissue collagen was assessed as a clinical pathological parameter and classified according to the degree of tissue fibrosis by the pathology department. To confirm the clinical observations, sections were stained with Masson’s Trichrome Stain. In brief, the paraffin sections obtained from the pathology department were dewaxed and hydrated in xylene and descending concentrations of ethanol. The pathological changes were illustrated by Hematoxylin and Eosin staining. For Masson’s Trichrome staining, the sections were re-fixed in Bouin’s solution and then stained with Weigert’s iron hematoxylin solution before Biebrich scarlet-acid fuchsin solution was added. The color was differentiated in phosphomolybdic-phosphotungstic acid solution until the collagen was no longer red. The sections were then transferred to aniline blue solution and finally differentiated in 1% acetic acid solution. To confirm deposition of collagen, the adjacent sections were de-waxed and hydrated, and Sirius Red was applied for 1 h at room temperature; after counterstaining with hematoxylin, the sections were mounted and analyzed.
Tissue sections were dewaxed and hydrated as described above. Depending on the antibody, antigen retrieval was performed on the sections in 0.01 M citrate buffer (pH 6.0) for EpCAM, CK7, and Notch2, or tris-ethylenediaminetetraacetic acid (EDTA) buffer (pH 9.0) for CD56, Notch1, and CD31 in a microwave for 10 min at 95 °C. Endogenous peroxidase was quenched with 3% hydrogen peroxide (H2O2) for 10 min, and non-specific signals were blocked by the addition of 0.1% bovine serum albumin (BSA) and 0.1% goat serum for 30 min at room temperature. The antibodies (1:50-1:200 in dilution buffer, Dako) were added and incubated at 37 °C for 60 min or overnight at 4 °C. The signals were revealed by the Dako EnVision System (Dako Denmark, Glostrup, Denmark) with diaminobenzidine (DAB) or the Polink DS-MR-Hu C1 kit for double staining following the manufacturer’s instructions. The sections were observed using Nikon Eclipse Ci (Nikon Instruments (Shanghai) Co., Ltd., Shanghai, China) and photographed with NIS-Elements software (Nikon Instruments).
All clinical data are presented as mean ± standard deviation (SD). The statistical analysis was performed using GraphPad® Prism software (GraphPad Software, Inc., La Jolla, CA, United States). Student’s t test was used when comparing two sets of data and one way analysis of variance (ANOVA) was used when three sets or more were compared. The Tukey multiple comparison test was used for statistical analysis of each individual comparison within a group. P values < 0.05 were considered statistically significant.
Overall, none of the parameters was significantly different when the CC-AM group was compared with CC group using the Student’s t test (Table 2). However, when CC-AM patients were compared with CC patients excluding the CC-AM group (i.e., CC-AM patients vs CC patients aged > 1 year), the level of γ-GT was significantly different (786.9 ± 759.2 U/L vs 357.2 ± 408.4 U/L, respectively, P < 0.01), as was TBIL (130.7 ± 116.8 μmol/L vs 46.9 ± 58.2 μmol/L, respectively, P < 0.001). The difference in TBIL might have arisen due to increased levels of IBIL in the CC-AM patients (68.4 ± 88.1 μmol/L vs 14.9 ± 16.7 μmol/L, respectively, P < 0.01).
| Population | Average (SD) value | ||||||||||
| ALT (U/L) | AST (U/L) | γ-GT (U/L) | TP (g/L) | ALB (g/L) | GLO (g/L) | ALB GLO | TBIL (μmol/L) | DBIL (μmol/L) | IBIL (μmol/L) | TBA (μmol/L) | |
| Normal ranges | 9-50 | 5-60 | 10-60 | 65-85 | 40-55 | 20-40 | 1.2-2.4 | 2-17 | 0-7 | 2-13.7 | 0-15 |
| BA (n = 85) | 183.8 (167.9) | 284.8 (279.8) | 898.0 (724.0) | 57.7 (6.7) | 39.0 (5.6) | 21.4 (28.8) | 2.4 (0.9) | 184.8 (60.6) | 136.7 (45.7) | 48.1 (20.7) | 169.7 (79.5) |
| NH (n = 32) | 251.9 (391.2) | 372.7 (425.9) | 271.7d (297.6) | 61.3 (40.5) | 38.1 (6.2) | 39.4 (132.8) | (2.5 (0.8) | 199.0 (96.5) | 134.0 (86.7) | 64.7 (39.2) | 158.0 (96.0) |
| CC | |||||||||||
| All (n = 65) | 105.0b (115.3) | 208.9 (252.1) | 575.4c (644.8) | 62.1 (9.3) | 41.1 (5.6) | 24.3 (27.1) | 3.2 (8.8) | 88.8f (100.8) | 47.2h (61.0) | 41.6 (68.4) | 77.7jl (124.1) |
| Aged < 1 yr (n = 32) | 88.6a (104.3) | 245.6 (326.1) | 786.9e (759.2) | 57.9 (7.7) | 39.6 (5.0) | 18.3 (4.4) | 2.3 (0.5) | 130.7g (116.8) | 62.3i (71.4) | 68.4 (88.1) | 83.9km (91.1) |
| Aged > 1 yr (n = 33) | 117.3 (116.8) | 260.9 (264.2) | 357.2 (408.4) | 66.2 (9.2) | 42.6 (5.8) | 30.4 (37.4) | 4.1 (12.4) | 46.9 (58.2) | 32.0 (44.6) | 14.9 (16.7) | 71.8 (150.7) |
No differences in TP, ALB, GLO, or the ratio of ALB to GLO were observed between the three diseases compared with the normal ranges of expression of these biochemical markers. AST levels were higher than normal (> 3-fold) in all three patient groups, but there was no significant difference. Using one way ANOVA with regard to ALT, there were differences in the means of ALT in BA, NH, and CC patients [F (2, 180) = 5.702, P = 0.0040] and in BA, NH, and CC-AM patients [F (2, 148) = 4.048, P = 0.0194]. There was no statistically significant difference when the patients with BA were compared to those with CC or NH, although there were differences between patients with NH and both the overall CC group and the CC-AM subgroup (P < 0.01 and P < 0.05, respectively). There were differences in the means of γ-GT between BA, NH, and CC patients [F (2, 179) = 11.57, P < 0.0001] and between BA, NH, and CC-AM [F (2, 148) = 9.927, P < 0.0001]. Markedly higher levels of γ-GT were observed in patients with BA (898.0 ± 724.0 U/L), which were 3-fold higher than in the NH group (271.7 ± 297.6 U/L, P < 0.001) and 1.5-fold higher than in the CC group (575.4 ± 644.8 U/L, P < 0.05). There was no significant difference in γ-GT between BA and CC-AM groups, although the level in the CC-AM group was higher (786.9 ± 759.2 U/L). Furthermore, the high level of γ-GT in the CC-AM group reached significance compared with the NH group (P < 0.01).
Bilirubin metabolism is one of the most important indicators of liver function. Levels of all three bilirubin proteins (TBIL, DBIL, and IBIL) were higher than the upper limit of the normal ranges in the three diseases studied. In terms of TBIL, one way ANOVA showed differences in the means of these three proteins in BA, NH, and CC patients [F (2, 180) = 30.48, P < 0.0001], and in BA, NH and CC-AM patients [F (2, 148) = 6.469, P = 0.0020], when compared with the CC group (88.8 ± 100.8 μmol/L). The levels of TBIL were significantly higher in the BA and NH groups (184.8 ± 60.6 μmol/L and 199.0 ± 96.5 μmol/L, respectively; P < 0.001 for both) and the CC-AM group (130.7 ± 116.8 μmol/L, P < 0.01). Similarly, differences in the means of DBIL were observed in the three groups [CC; F (2, 180) = 46.06, P < 0.0001] and CC-AM; F (2, 148) = 17.92, P < 0.0001]. Increased levels of serum DBIL were observed in the BA and NH groups (136.7 ± 45.7 μmol/L and 134.0 ± 86.7 μmol/L, respectively) compared with the CC (47.2 ± 61.0 μmol/L) and CC-AM (62.3 ±7 1.4 μmol/L) subgroups (P < 0.001 for all comparisons). Total bile acid levels reflect liver function in terms of fatty acid metabolism, and the pattern of high levels detected in patients with BA and NH compared to those with CC was similar to that for bilirubin. The same phenomenon was observed for TBA in the three groups, BA, and NH with either CC or CC-AM, and the differences were significant [F (2, 172) = 14.79, P < 0.0001] and [F (2, 140) = 10.50, P < 0.0001]. Increased levels of TBA were observed in the BA and NH groups (169.7 ± 79.5 μmol/L and 158.0 ± 96.0 μmol/L, respectively) compared with the CC and CC-AM groups (71.8 ± 150.7 μmol/L, P < 0.001 and 83.9 ± 91.1 μmol/L, P < 0.01, respectively).
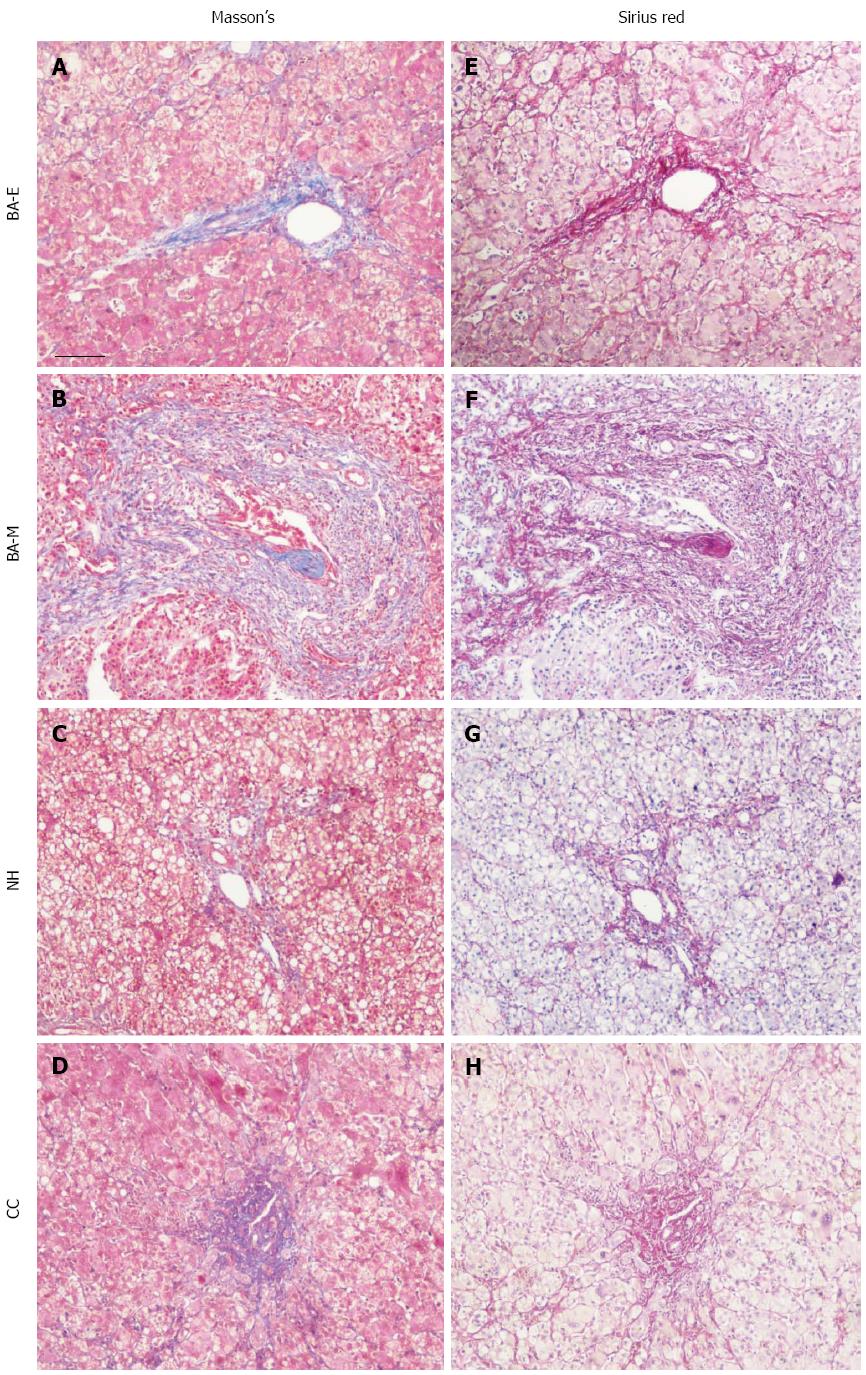
In order to determine whether clinical laboratory parameters had any relation to tissue fibrosis, the collagen content in tissue sections was examined with Masson’s Trichrome Stain. We observed that low levels of collagen were deposited in patients with early liver damage [early stage of biliary atresia (BA-E)], in which there was neither fibrosis nor mild portal fibrosis[17,18], and similar results were obtained for patients with NH and CC. However, collagen deposits were markedly increased in patients with moderate or late liver damage [middle or late stage of biliary atresia (BA-ML)], who were reported to have a high degree of fibrosis[17,18] (Figure 1 left panel). These results were confirmed by Sirius Red staining, which allowed more accurate quantification (Figure 1, right panel).
The levels of biochemical parameters, especially γ-GT, TBIL, and DBIL, were significantly different in the three different cholestatic diseases, and these were reanalyzed in the context of the degree of tissue fibrosis, using BA-E and BA-ML as the stages of disease progression. There were no statistically significant differences, although the trend in the BA-ML group suggested that there might be increases in all three parameters compared with the BA-E group.
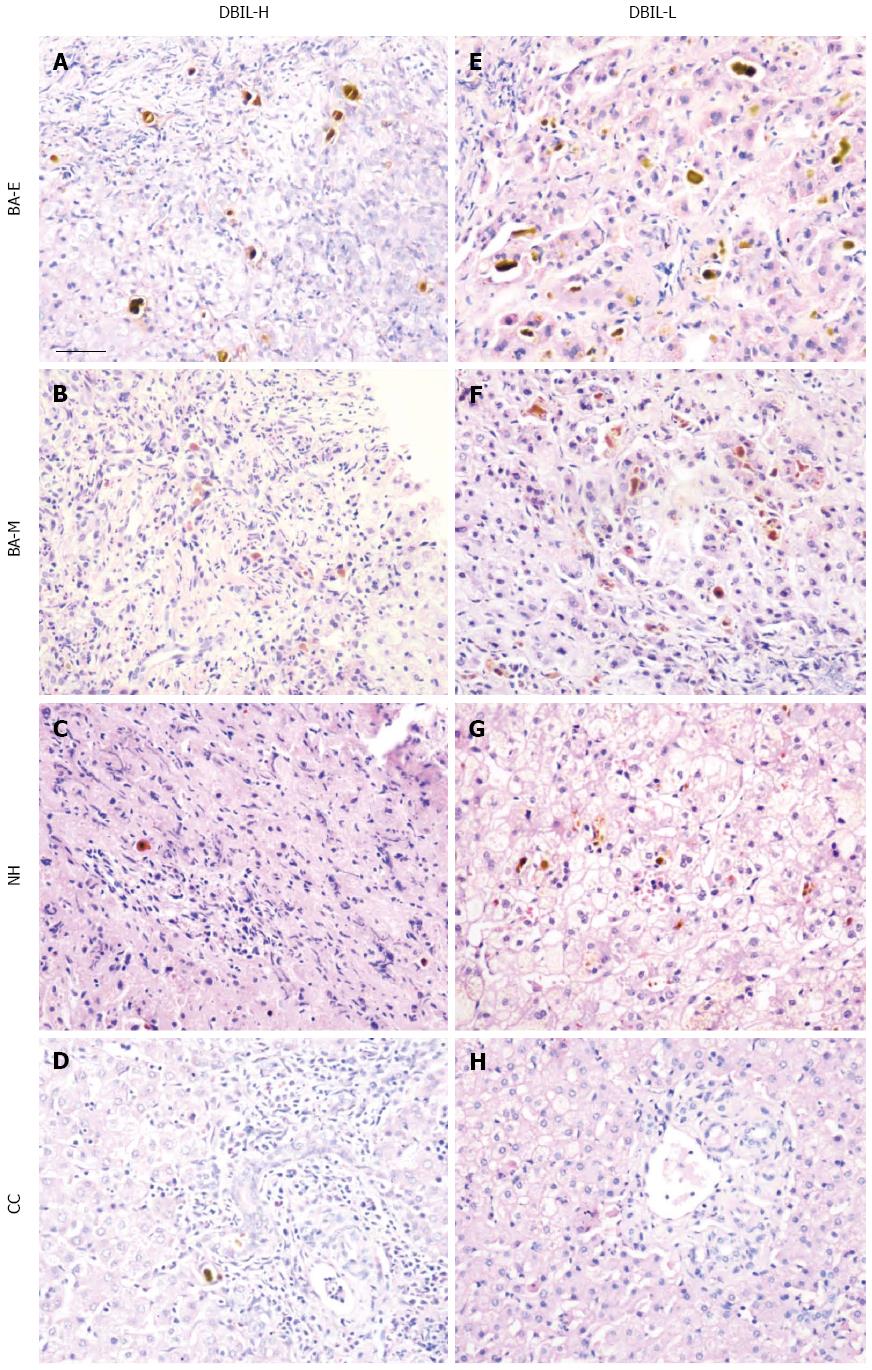
No significant differences in serum levels of the biochemical parameters of bilirubin metabolism were found between the BA-E and BA-ML groups, which suggested either a reduction in the expression of bilirubin-related molecules or impairment of the transport of these products. Accumulation of bile plugs is a hallmark of BA, and it can often be found in bile ducts or ductules (Figure 2A, B, E, and F). In contrast, the presence of bile plugs was much less marked in patients with NH and CC (Figure 2C and G; D and H). However, when using BA-E and BA-ML as the different stages of BA, no difference was found in the accumulation of bile plugs, which was extensive in both stages, and their presence in liver tissue was not evenly distributed.
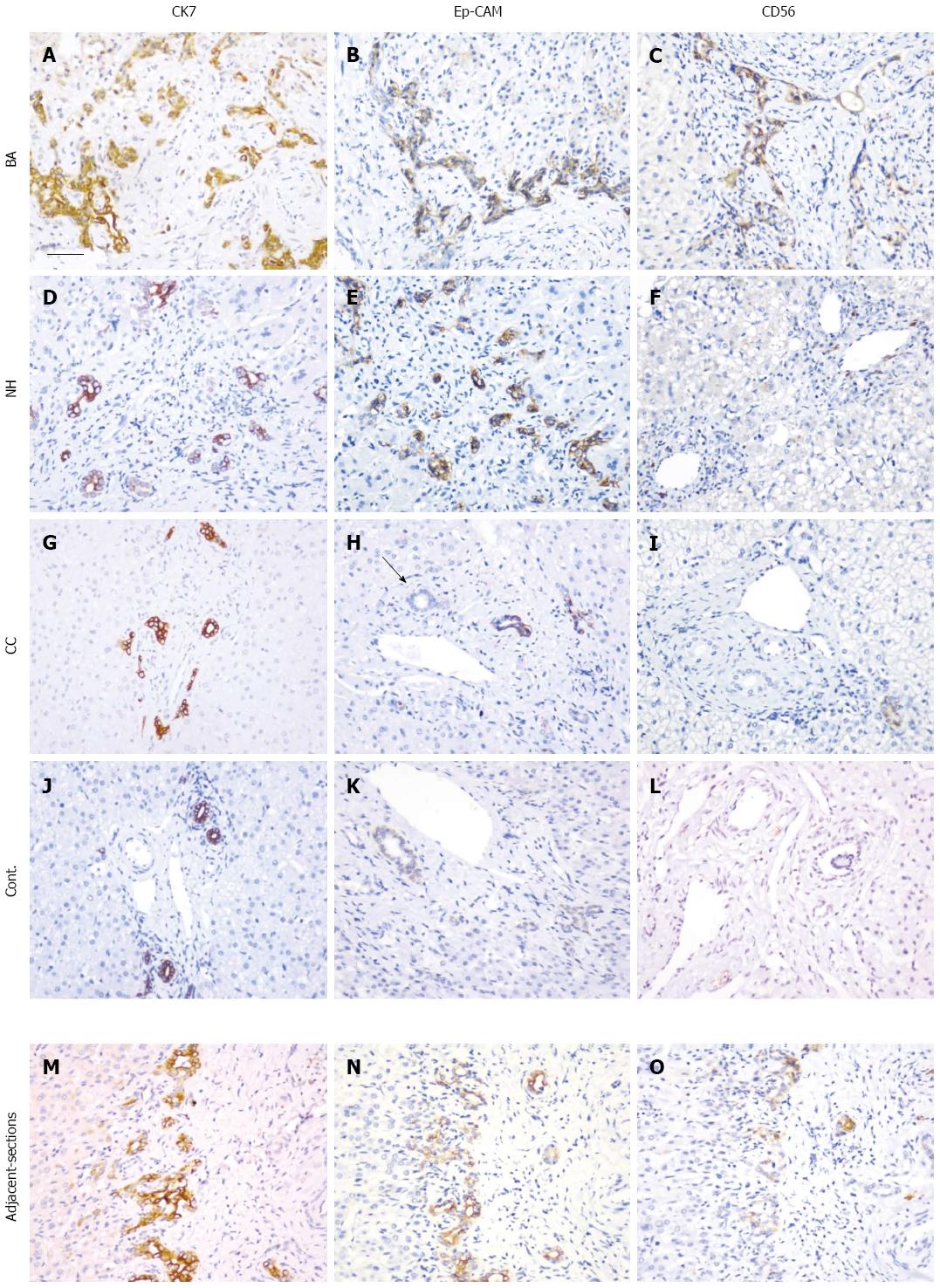
Changes in morphology of the IHBDs were further examined using different markers for BECs. CK7 has long been used as a marker for BECs and showed positive staining in all tissue sections examined in patients with BA, NH, and CC as well as the disease control (portal vein cavernous transformation, PVCT) (Figure 3A, D, G and J). However, CK7 staining was slightly weaker in BA, which may have been related to its immature status. Compared to the control, the number of CK7-positive cells was greatly increased in patients with BA, but less so in those with NH. In patients with CC, the number of cells was similar to that in the control.
EpCAM is a marker of mature BECs and was expressed in BA, NH, CC, and the disease control (Figure 3B, E, H and K). The pattern of EpCAM staining was similar to that of CK7, but the number of cells was less pronounced than that detected for CK7. In some tissue sections, bile ducts in the portal tract did not stain with EpCAM; and, therefore, the staining pattern was different from that of CK7 (Figure 3M and N).
CD56 is a marker of immature BECs. Marked expression of CD56-positive BECs was observed in patients with BA (Figure 3C), but not in those with NH, CC, or in normal control liver (Figure 3F, I and L). Using adjacent tissue sections from patients with BA, a partial co-localization of CD56 and CK7 was observed (Figure 3M and O).
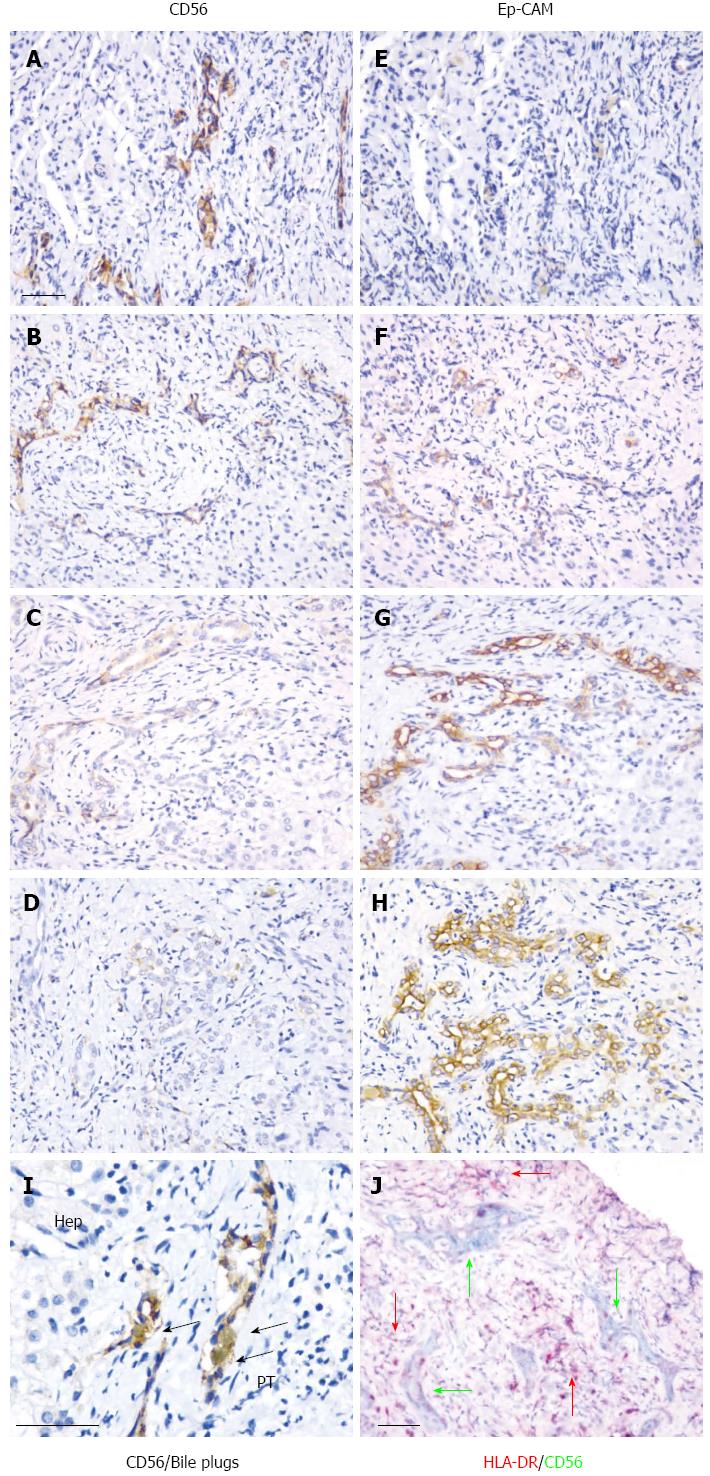
Using adjacent tissue sections, expression of CD56 was further analyzed and was observed to co-localize with EpCAM (Figure 4A-H). The CD56-positive immature bile ducts were mostly found in the periportal tract, where bile plugs were often observed (Figure 4I). Inflammatory cell infiltration is an important event in the development of BA, and expression of major histocompatibility complex class II [human leucocyte antigen (HLA)-DR] proteins was detected in tissue sections. The co-localization of CD56 and HLA-DR staining indicated the close relationship between these two sets of cells, and, in some instances, HLA-DR-positive cells were found in CD56-positive immature bile ducts (Figure 4J).
Three categories of CD56 expression were identified based on the intensity of staining: strong (++) (Figure 4A and B), weak (+) (Figure 4C), and no signal (-) (Figure 4D). In order to further understand the relationship between CD56, bile plugs and the pathological classification of BA-E and BA-ML, the percentage of each category was calculated for patients with BA (Table 3). Overall, the percentage of CD56++ was higher for BA-ML than for BA-E (57.1% vs 40.1%) and for sections with bile plugs than those without (51.2% vs 41.7%). Further analysis of the disease subcategories found that BA-E without bile plugs had a higher percentage of CD56- cells than CD56+ cells (50% vs 16.7%) and BA-ML with bile plugs had a higher percentage of CD56+ than CD56- cells (54.4% vs 18.2%). These data suggest a positive correlation between CD56+ cells and disease progression.
| Stage of BA | n | CD56++ | CD56+ | CD56- |
| All | 55 | 27 (49.1) | 14 (25.5) | 14 (25.5) |
| BA-E without bile plugs | 6 | 1 (16.7) | 2 (33.3) | 3 (50.0) |
| BA-E with bile plugs | 21 | 10 (47.6) | 5 (23.8) | 6 (28.6) |
| BA-ML without bile plugs | 6 | 4 (66.7) | 1 (16.7) | 1 (16.7) |
| BA-ML with bile plugs | 22 | 12 (54.5) | 6 (27.3) | 4 (18.2) |
| All BA-E | 27 | 11 (40.7) | 7 (25.9) | 9 (33.3) |
| All BA-ML | 28 | 16 (57.1) | 7 (25.0) | 5 (17.9) |
| All without bile plugs | 12 | 5 (41.7) | 3 (25.0) | 4 (33.3) |
| All with bile plugs | 43 | 22 (51.2) | 11 (25.6) | 10 (23.3) |
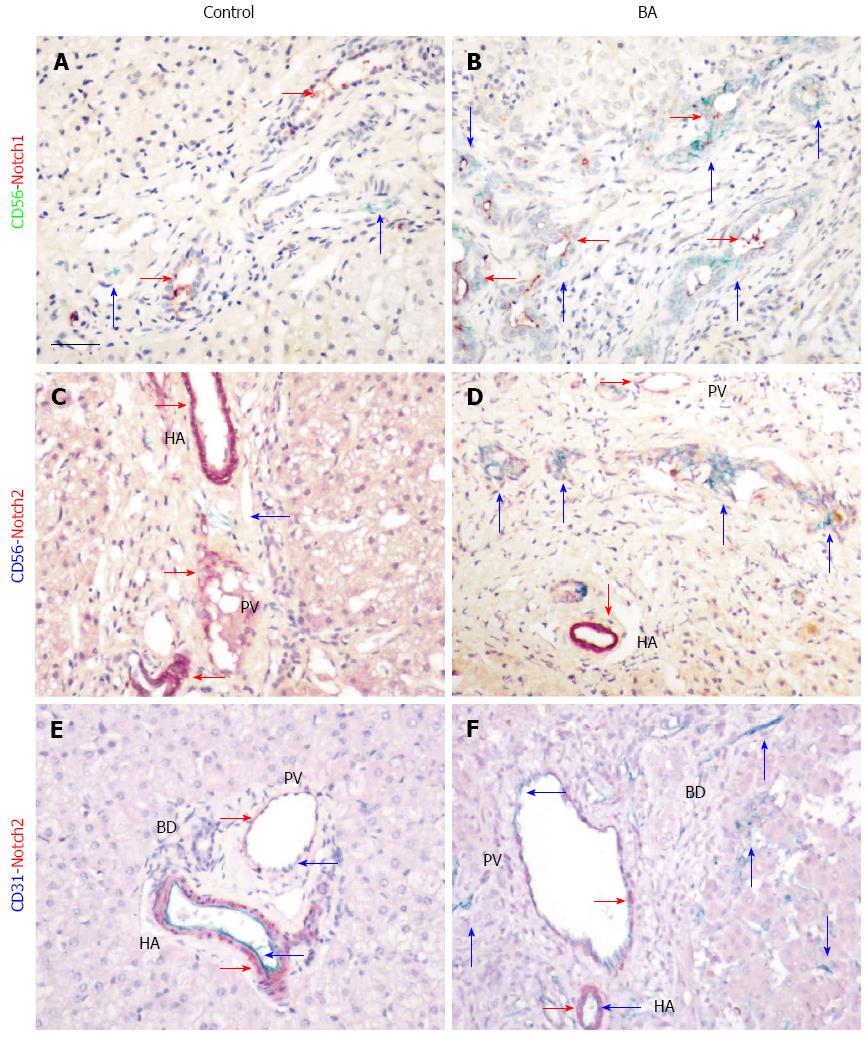
Notch signaling is involved in development of the bile duct system and also plays a role in tissue fibrosis. In order to study the relationship between CD56-positive BECs and the Notch signaling pathway, expression of the receptors Notch1 and Notch2 was investigated in patients with BA using immunohistochemistry and double staining. In age-matched liver tissue controls, Notch1 expression was detected in mature bile ducts in the portal area (Figure 5A). Expression of CD56 was rarely detected in normal liver tissue, but, when observed, it was not co-localized with Notch1. In contrast, increased expression of CD56 was found in immature bile ducts in patients with BA, and most of them also expressed Notch1 (Figure 5B). Expression of Notch1 was detected mainly in the lumen of the bile ducts in both normal tissue and tissue from patients with BA, which suggests the presence of the secreted form of the protein. Expression of Notch2 was mainly in the blood vessels, both the hepatic arteries and portal veins, which are situated inside the portal area in healthy subjects and those with BA (Figure 5C-F). No co-localization of CD56+ and Notch2+ cells was observed in the portal tract (Figure 5D). However, increased CD31, one of the endothelial cell markers, was found in tissue from patients with BA, and co-localization with Notch2 was observed. It is suggested that Notch signaling is increased in patients with BA, which may impact progression of tissue fibrosis.
In this study, we compared 10 clinical laboratory parameters in three neonatal cholestatic diseases and found similarities in most of the parameters examined. The levels of TP, ALB, and GLO, which reflect biosynthesis and storage of liver proteins, were similar to normal reference levels. Although there was variation between individual patients, it seems unlikely that these parameters are primarily responsible for severe liver damage. This is understandable, as blockade of bile transport in these three diseases is initially affected, while damage to the hepatocytes occurs only at the end stage of these conditions. Metabolism of bilirubin was the main feature that differentiated CC (including age-matched CC) from BA and NH, with the levels of DBIL being much lower in the CC group. This difference can be explained by the fact that CC mostly affects the extra-hepatic biliary ducts, but also damages the hepatocytes themselves and leakage of bile into the bloodstream is not severe. Similar results were obtained for TBIL and TBA, which indicates that metabolism of bilirubin was more severely impaired in patients with BA and NH than in those with CC. In terms of distinguishing BA and NH based on clinical laboratory parameters, only γ-GT showed different levels. In patients with NH, a 4-fold increase in γ-GT was observed compared to the upper limit of the normal range; however, γ-GT expression was increased 14-fold in patients with BA. Histological and immunohistochemical analyses showed more bile ducts and ductules in patients with BA than in those with NH. As γ-GT was expressed in both hepatocytes and BECs[19], higher numbers of BECs may be the source of increased levels of γ-GT. Our data validate an earlier report in which γ-GT was demonstrated to be a valuable indicator for distinguishing BA from NH[20]. However, as NH is a complex multi-factorial disease with variations in pathology, it is likely that some patients may develop BA in the later phase of the disease, and, therefore, the use of γ-GT as an exclusive clinical indicator requires caution.
The transition from inflammation to fibrosis is a pathological change that occurs in patients with BA, although the time frame for this has not been conclusively defined[2]. Infiltration of inflammatory cells, proliferation of neovascular and neo-biliary epithelial cells, and accumulation of bile play a role in this process, which complicates the understanding of the pathophysiology of the disease. In an attempt to simplify the analysis of the disease processes, we separated liver damage into two stages - BA-E and BA-ML - with tissue fibrosis as the main discriminator. We found that there was no difference in the number of bile plugs in early fibrosis compared to late stage fibrosis.
The number of bile plugs noted in bile ducts, which were occasionally found in hepatocytes, prompted us to study the morphology of the bile ducts. Using three different markers of BECs, we detected the presence of both CD56- and EpCAM-positive cells, which respectively reflect immature and mature BECs, and these two cell populations were a part of the cell population that stained with CK7. These results indicate that pathological changes develop in the biliary system of patients with BA. The expression of CD56 in bile ductules discriminated between BA and both NH and CC, confirming previous observations[10,11,21]. We failed to detect CD56-positive cells in some tissue sections from patients with BA, but the presence of the mature BEC markers may indicate heterogeneity of the maturation process. Whether this reflects the early phase of “ductal reaction” warrants further study. Nevertheless, even in the absence of CD56-positive cells, the possibility of BA cannot be excluded. Our observation that progression of BEC maturation reduced the expression of CD56 also suggests that analyzing the expression of EpCAM might help to clarify further events in the development of BA. As CK7 also stains ductal hepatocytes, or oval cells[22], which are progenitors of BECs, it may aid in understanding the origin of CD56-positive cells. The combined use of these three markers for BECs will extend our understanding of the function of BECs in the BA disease process.
Liver tissue regeneration offers some compensation for lost organ function arising from these diseases, and it has been suggested that the presence of CD56 positivity is a sign of tissue repair[21]. However, in this study, we found that newly formed bile ductules often co-localized with bile plugs. Analysis of the morphology of the ductules with CD56-positive staining often showed no lumen, and as maturation progressed, we noted that the CD56 signal reduced, but increased for EpCAM, which resulted in an increase in the lumen area. However, the high expression of CD56 in BA suggests that there is inhibition of the maturation process. Furthermore, bile accumulation contributes to liver fibrosis, as demonstrated by the finding that ligation of the bile duct can directly induce liver fibrosis[23]. The presence of CD56 implies the progression of BA to liver fibrosis. This, together with evidence for Notch signaling in CD56-positive cells, further increases the possibility of liver fibrosis, as this signaling pathway plays a key role in the development of fibrosis directly within tissues[24] and by the infiltration of inflammatory cells[25]. Our data suggest that the presence of CD56-positive BECs might promote deleterious outcomes in the progression of BA. We also demonstrated that CD56-positive cells are often surrounded by HLA-DR expressing cells, which is in agreement with previous studies[26,27]. Therefore, it is possible that CD56-positive BECs from ductal hepatocytes may interact with the inflammatory cell infiltrate. Our results are compatible with extrahepatic bile duct blockade and inflammatory cellular infiltration acting together to promote the pathogenesis of BA. The presence of CD56-positive cells does not ameliorate the pathological condition but, in contrast, accelerates the development of tissue fibrosis.
In conclusion, our study shows that levels of bilirubin-related parameters, such as TBIL, DBIL, and TBA, are higher in patients with BA and NH and moderately high in patients with CC. Furthermore, γ-GT was significantly increased in patients with BA as compared to those with NH. This change might be related to the increased levels of CD56-positive immature BECs in patients with BA. However, newly formed immature bile ducts or ductules have no bile transport function and bile may accumulate to form bile plugs. Enhanced expression of Notch signaling in CD56-positive cells further increases the possibility of progression to liver cirrhosis. Inhibition of the formation of CD56-positive BECs or the promotion of maturation of these cells may help to reduce BA progression to cirrhosis.
The authors would like to thank Dr. Stacey Cherny (Department of Psychiatry, the University of Hong Kong) for assistance with statistical analysis.
Clinical laboratory parameters do not correspond fully with the pathological processes in biliary atresia (BA). Therefore, it is necessary to define biliary ductular structure in order to assess the development of fibrotic changes.
Clinical laboratory parameters, tissue fibrosis, and bile plugs have been examined in many studies, but the different stages of maturation of biliary epithelial cells (BECs) in BA are not well defined and their relationship with fibrosis is unclear.
The expression of CD56+ immature epithelial cells in BA, which was correlated with liver fibrosis, and their expression of fibrogenesis signaling molecule Notch 1 are novel findings in this study.
CD56+ immunohistochemistry might have additive value in the diagnosis of BA, and studies on the mechanisms of maturation of BECs may provide new insights into the treatment of BA.
CD56 is a marker of immature BECs, whereas epithelial cell adhesion molecule (EpCAM) expression is representative of more mature BECs. CK7 labels all BECs.
The authors analyzed the clinical and pathological parameters together with the expression of the neural cell adhesion molecule (CD56) in BA patients. They found that the maturation of biliary epithelial cells and the expression of Notch might play a role in the pathogenesis of BA.
P- Reviewer: de Silva AP, Dong R, Moralioglu S S- Editor: Gong ZM L- Editor: Filipodia E- Editor: Zhang DN
| 1. | Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009;374:1704-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 638] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 2. | Bessho K, Bezerra JA. Biliary atresia: will blocking inflammation tame the disease? Annu Rev Med. 2011;62:171-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Lu BR, Brindley SM, Tucker RM, Lambert CL, Mack CL. α-enolase autoantibodies cross-reactive to viral proteins in a mouse model of biliary atresia. Gastroenterology. 2010;139:1753-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Shivakumar P, Sabla G, Mohanty S, McNeal M, Ward R, Stringer K, Caldwell C, Chougnet C, Bezerra JA. Effector role of neonatal hepatic CD8+ lymphocytes in epithelial injury and autoimmunity in experimental biliary atresia. Gastroenterology. 2007;133:268-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Bezerra JA, Tiao G, Ryckman FC, Alonso M, Sabla GE, Shneider B, Sokol RJ, Aronow BJ. Genetic induction of proinflammatory immunity in children with biliary atresia. Lancet. 2002;360:1653-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 144] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Mack CL. The pathogenesis of biliary atresia: evidence for a virus-induced autoimmune disease. Semin Liver Dis. 2007;27:233-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 134] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Cocjin J, Rosenthal P, Buslon V, Luk L, Barajas L, Geller SA, Ruebner B, French S. Bile ductule formation in fetal, neonatal, and infant livers compared with extrahepatic biliary atresia. Hepatology. 1996;24:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Bellizzi AM, LeGallo RD, Boyd JC, Iezzoni JC. Hepatocyte cytokeratin 7 expression in chronic allograft rejection. Am J Clin Pathol. 2011;135:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Joplin R, Kachilele S. Human intrahepatic biliary epithelial cell lineages: studies in vitro. Methods Mol Biol. 2009;481:193-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Sira MM, El-Guindi MA, Saber MA, Ehsan NA, Rizk MS. Differential hepatic expression of CD56 can discriminate biliary atresia from other neonatal cholestatic disorders. Eur J Gastroenterol Hepatol. 2012;24:1227-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Torbenson M, Wang J, Abraham S, Maitra A, Boitnott J. Bile ducts and ductules are positive for CD56 (N-CAM) in most cases of extrahepatic biliary atresia. Am J Surg Pathol. 2003;27:1454-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Kodama Y, Hijikata M, Kageyama R, Shimotohno K, Chiba T. The role of notch signaling in the development of intrahepatic bile ducts. Gastroenterology. 2004;127:1775-1786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 170] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 13. | Li L, Krantz ID, Deng Y, Genin A, Banta AB, Collins CC, Qi M, Trask BJ, Kuo WL, Cochran J. Alagille syndrome is caused by mutations in human Jagged1, which encodes a ligand for Notch1. Nat Genet. 1997;16:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 932] [Cited by in RCA: 877] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 14. | Chen Y, Zheng S, Qi D, Zheng S, Guo J, Zhang S, Weng Z. Inhibition of Notch signaling by a γ-secretase inhibitor attenuates hepatic fibrosis in rats. PLoS One. 2012;7:e46512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Fabris L, Cadamuro M, Guido M, Spirli C, Fiorotto R, Colledan M, Torre G, Alberti D, Sonzogni A, Okolicsanyi L. Analysis of liver repair mechanisms in Alagille syndrome and biliary atresia reveals a role for notch signaling. Am J Pathol. 2007;171:641-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Hofmann JJ, Iruela-Arispe ML. Notch signaling in blood vessels: who is talking to whom about what? Circ Res. 2007;100:1556-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 180] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 17. | Moyer K, Kaimal V, Pacheco C, Mourya R, Xu H, Shivakumar P, Chakraborty R, Rao M, Magee JC, Bove K. Staging of biliary atresia at diagnosis by molecular profiling of the liver. Genome Med. 2010;2:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Weerasooriya VS, White FV, Shepherd RW. Hepatic fibrosis and survival in biliary atresia. J Pediatr. 2004;144:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 88] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Nemesánszky E, Lott JA. Gamma-glutamyltransferase and its isoenzymes: progress and problems. Clin Chem. 1985;31:797-803. [PubMed] |
| 20. | Rendón-Macías ME, Villasís-Keever MA, Castañeda-Muciño G, Sandoval-Mex AM. Improvement in accuracy of gamma-glutamyl transferase for differential diagnosis of biliary atresia by correlation with age. Turk J Pediatr. 2008;50:253-259. [PubMed] |
| 21. | Okada T, Itoh T, Sasaki F, Honda S, Naito S, Todo S. CD56-immunostaining of the extrahepatic biliary tree as an indicator of clinical outcome in biliary atresia: a preliminary report. Turk J Pediatr. 2008;50:542-548. [PubMed] |
| 22. | Paku S, Dezso K, Kopper L, Nagy P. Immunohistochemical analysis of cytokeratin 7 expression in resting and proliferating biliary structures of rat liver. Hepatology. 2005;42:863-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Xia JL, Dai C, Michalopoulos GK, Liu Y. Hepatocyte growth factor attenuates liver fibrosis induced by bile duct ligation. Am J Pathol. 2006;168:1500-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 24. | Henderson NC, Arnold TD, Katamura Y, Giacomini MM, Rodriguez JD, McCarty JH, Pellicoro A, Raschperger E, Betsholtz C, Ruminski PG. Targeting of αv integrin identifies a core molecular pathway that regulates fibrosis in several organs. Nat Med. 2013;19:1617-1624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 684] [Cited by in RCA: 691] [Article Influence: 57.6] [Reference Citation Analysis (0)] |
| 25. | Dees C, Tomcik M, Zerr P, Akhmetshina A, Horn A, Palumbo K, Beyer C, Zwerina J, Distler O, Schett G. Notch signalling regulates fibroblast activation and collagen release in systemic sclerosis. Ann Rheum Dis. 2011;70:1304-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 26. | Kobayashi H, Puri P, O’Briain DS, Surana R, Miyano T. Hepatic overexpression of MHC class II antigens and macrophage-associated antigens (CD68) in patients with biliary atresia of poor prognosis. J Pediatr Surg. 1997;32:590-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Gong ZH, Xiao X, Chen L. Hepatic fibrosis with choledochal cyst in infants and children - an immunohistochemical assessment. Eur J Pediatr Surg. 2007;17:12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |