Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10415
Peer-review started: June 29, 2016
First decision: August 29, 2016
Revised: September 30, 2016
Accepted: October 31, 2016
Article in press: October 31, 2016
Published online: December 21, 2016
Processing time: 172 Days and 22.5 Hours
To retrospectively review patients with chronic pancreatitis (CP) treated with Frey’s procedures between January 2009 and January 2014.
A retrospective review was performed of patients with CP treated with Frey’s procedures between January 2009 and January 2014 in the Department of Pancreatic Surgery. A cross-sectional study of postoperative pain relief, quality of life (QoL), and alcohol and nicotine abuse was performed by clinical interview, letters and telephone interview in January 2016. QoL of patients was evaluated with the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30) version 3.0. The patients were requested to fill in the questionnaires by themselves via correspondence or clinical interview.
A total of 80 patients were enrolled for analysis, including 44 who underwent the original Frey’s procedure and 36 who underwent a modified Frey’s procedure. The mean age was 46 years in the original group and 48 years in the modified group. Thirty-five male patients (80%) were in the original group and 33 (92%) in the modified group. There were no differences in the operating time, blood loss, and postoperative morbidity and mortality between the two groups. The mean follow-up was 50.3 mo in the original group and 48.7 mo in the modified group. There were no differences in endocrine and exocrine function preservation between the two groups. The original Frey’s procedure resulted in significantly better pain relief, as shown by 5-year follow-up (P = 0.032), better emotional status (P = 0.047) and fewer fatigue symptoms (P = 0.028). When stratifying these patients by the M-ANNHEIM severity index, no impact was found on pain relief after the two types of surgery.
The original Frey’s procedure is as safe as the modified procedure, but the former yields better pain relief. The severity of CP does not affect postoperative pain relief.
Core tip: Surgical treatment is often required for chronic pancreatitis (CP) when conservative therapy cannot control the intractable pain. The Frey’s procedure is frequently applied for CP because of its safety and efficacy. However, there is no uniform standard for the amount of cored pancreatic head tissue. This study compared the original and modified Frey’s procedures with different depths of cored tissue and performance in a single clinical department. The original Frey’s procedure was advantageous in terms of pain relief in a 5-year follow-up.
- Citation: Tan CL, Zhang H, Yang M, Li SJ, Liu XB, Li KZ. Role of original and modified Frey's procedures in chronic pancreatitis. World J Gastroenterol 2016; 22(47): 10415-10423
- URL: https://www.wjgnet.com/1007-9327/full/v22/i47/10415.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i47.10415
Chronic pancreatitis (CP) is an inflammatory disease of the pancreas characterized by abdominal pain, repeated episodes of acute pancreatitis and fibrotic destruction of the organ, resulting in endocrine and exocrine insufficiency[1]. Alcohol consumption and biliary lithiasis are the main causes of CP, followed by autoimmune or individual genetic predisposition. High caloric intake of protein and fat, smoking, and lack of vitamins and trace elements have been described as additional predisposing risk factors[2]. Calcifying CP, characterized by intraductal calculi, protein plugs and parenchymal calcification, is most common. Additionally, irregular pancreatic duct, gland enlargement, heterogeneous parenchyma and small cavities can be found[3].
Persistent pain is the leading symptom of the disease, which reduces quality of life (QoL), leading to addiction to analgesics and unemployment or early retirement. Development of pain in the natural course of the disease is seen in 85% of patients[4]. In the initial stage of the disease, pain is intermittent and recurrent, while later it becomes persistent. The underlying mechanism for pain in CP is still poorly understood.
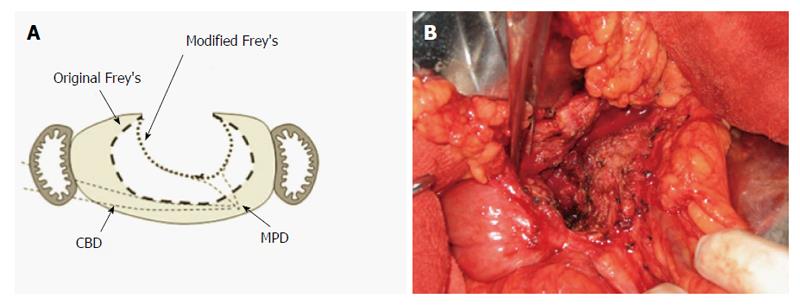
A general consensus exists that the primary therapy for CP should be a conservative symptom-related treatment. Surgery has to be considered in patients with failure of conservative and endoscopic interventions or suspicious malignancy. The two surgical procedures for CP are drainage of the main pancreatic duct (MPD) and resection of pancreatic parenchyma. The choice of surgical procedure should be determined by the degree and extent of MPD dilation and gland morphology. In 1987, Frey and Smith[5] described anterior resection of the head of the pancreas combined with MPD drainage using longitudinal pancreaticojejunostomy. To reduce the risk of penetrating the posterior capsule of the head, Frey and Amikura[6] later recommended that the posterior limit of resection should be the back wall of the opened duct of Wirsung and duct to the uncinate process. A few surgeons modified Frey’s procedure further by limiting the coring out of the pancreatic head to include only the area anterior to the MPD[7].
When Schneider et al[1] analyzed the predictive factors for hospital readmission for CP, they found that a severe form of the disease was associated with risk of readmission. The M-ANNHEIM is a simple, objective and noninvasive classification system for CP, which incorporates a severity index that refers to the different conditions of pancreatic morphology and function, and that includes clinical features of the disease such as patterns of pain and the impact of conservative, endoscopic and surgical treatment. However, the questions remained: When treating CP with Frey’s procedure, how much of the pancreatic head should be resected? Is the long-term effect after Frey’s procedure related to the different surgical procedures or to disease severity?
In this study, we aimed to analyze the role of different Frey’s procedures and the severity of disease according to the M-ANNHEIM severity index for predicting surgical treatment of CP.
This was a retrospective review of patients who underwent different Frey’s procedures in a single center between January 2009 and January 2014. Following Institutional Review Board approval, we performed a retrospective review of the patients with CP treated between January 2009 and January 2014 in our hospital. We enrolled patients who had undergone Frey’s procedures. Patients with Partington’s procedure, Whipple procedure, or distal or total pancreatectomy were excluded. Among duodenum-preserving pancreatic head resection procedures, the Beger and Berne procedures were also excluded. The Frey’s procedures were divided into two types: the original and modified procedures. Both types of Frey’s procedures are illustrated in Figure 1[7].
The M-ANNHEIM severity indexes were divided into two types. Grades A and B were classified as minor severity and Grades C-E were classified as major severity. The selected patients were analyzed regarding age, sex, body mass index (BMI), etiology, degree of pain, endocrine and exocrine function, morphological characteristics, organ complications, operating time, blood loss, morbidity, mortality and postoperative hospital stay. The mortality rate included all deaths within 30 d after surgery. The morbidity rate included all complications following surgery until discharge. Major postoperative morbidity was defined and graded using criteria recommended by the International Study Group of Pancreatic Surgery, including postoperative pancreatic fistula, delayed gastric emptying, and postpancreatectomy hemorrhage[8-10]. Enteric leaks were identified using radiographic contrast imaging. Fluid collection in intra-abdominal or pleural regions was performed via radiographic imaging, which was differentiated from abscesses by positive microbial cultures. Pneumonia was diagnosed based on chest X-ray changes following antibiotic therapy.
The cross-sectional study of postoperative pain relief, QoL, and alcohol and nicotine abuse was performed by outpatient interview, letter, and telephone interview in January 2016. QoL was evaluated using the European Organisation for Research and Treatment of Cancer Quality of life Questionnaire (EORTC QLQ-C30) version 3.0. The patients were requested to fill in the questionnaires by themselves via correspondence or clinical interview.
The original Frey’s procedure involved local resection of the pancreatic head combined with longitudinal pancreaticojejunostomy. The rim of pancreatic tissue of the entire head was preserved, and was used to sew to the opened jejunum. The ducts of Wirsung and Santorini were excised, and the excavation was created in continuity with the longitudinal dichotomy of the dorsal duct. The modified Frey’s procedure was recommended to reduce the risk of penetrating the posterior capsule of the pancreatic head. It was recommended that the posterior limit of resection should be the back wall of the opened duct of Wirsung and duct to the uncinate process.
Pearson’s χ2 test was used for categorical variables. Fisher’s exact test was used in cases with a variable count < 5. For continuous variables, Student’s t test was used for normally distributed variables and the Wilcoxon rank sum test was used for non-normally distributed variables. P < 0.05 was considered statistically significant. All analyses were performed using SPSS version 18.0 software on a personal computer (SPSS Inc., Chicago, IL, United States).
One hundred and fifty-six patients underwent surgical treatment for CP between January 2009 and January 2014. Twenty-eight patients had received the Whipple procedure or total pancreatectomy for adenocarcinoma. Twenty-five patients had received the Berney technique. Ten patients had received duodenum-preserving pancreatic head resection combined with distal pancreatectomy. Ninety-three patients had received Frey’s procedure. Eleven of these patients were lost to follow-up in this study. Two patients died from pancreatic cancer. Finally, 80 patients were enrolled for analysis, including 44 who underwent original Frey’s procedures and 36 who underwent modified Frey’s procedures. The indications for Frey’s procedures included intractable pain (66 cases), recurrent episodes of acute pancreatitis (4 cases), bile duct stenosis (2 cases) and risk of malignancy (8 cases).
The characteristics of the patients undergoing original and modified Frey’s procedures and the differences between the two groups are summarized in Table 1. The median age was 46 years in the original Frey’s group and 48 in the modified Frey’s group. Thirty-five male patients (80%) were in the original Frey’s group and 33 (92%) in the modified Frey’s group. The etiologies included alcohol (22 cases), nicotine (7 cases) and idiopathic (15 cases) in the original Frey’s group, and alcohol (21 cases), nicotine (4 cases) and idiopathic (11 cases) in the modified Frey’s group. Stone in the pancreatic duct and/or pancreatic calcification were identified in 39 (89%) patients in the original Frey’s group and 29 (81%) in the modified Frey’s group. Exocrine insufficiency was found in one patient in the original Frey’s group and none in the modified Frey’s group. Endocrine insufficiency was found in 14 (32%) patients in the original Frey’s group and 17 (37%) in the modified Frey’s group.
| Characteristic | O Frey(n = 44) | M Frey(n = 36) | P value |
| Age (yr) | 46 ± 12.5 | 48 ± 8.4 | 0.560 |
| Sex | 0.130 | ||
| Male | 35 | 33 | |
| Female | 9 | 3 | |
| Etiology | 0.720 | ||
| Alcohol | 22 | 21 | |
| Nicotine | 7 | 4 | |
| Idiopathic | 15 | 11 | |
| Pain severity index | 3.84 ± 1.14 | 2.92 ± 1.47 | 0.020 |
| Exocrine insufficiency | 3 | 0 | 0.580 |
| Endocrine insufficiency | 14 | 17 | 0.450 |
| Morphologic characters | |||
| Stone of calcification | 39 | 29 | 0.360 |
| Large cavities (> 10 mm) | 7 | 11 | 0.120 |
| Gland enlargement (> 2 × normal) | 7 | 9 | 0.310 |
| Severe organ complications | |||
| Obstruction of ductus choledochus | 0 | 2 | 0.200 |
| Ascites | 0 | 0 | |
| Weight loss | 13 | 9 | 0.650 |
| M-ANNHEIM severity index | 0.060 | ||
| A | 1 | 4 | |
| B | 29 | 17 | |
| C | 12 | 15 | |
| D | 2 | 0 | |
| E | 0 | 0 | |
| Indication for surgery | |||
| Intractable pain | 38 | 28 | 0.315 |
| Recurrent episodes | 2 | 2 | |
| Bile duct stenosis | 0 | 2 | |
| Risk of malignancy | 4 | 4 | |
| Follow-up time (mo) | 50.3 ± 17.3 | 48.7 ± 15.6 | 0.670 |
According to the M-ANNHEIM classification of CP, one (2%) patient had severity index A, 29 (66%) index B, 12 (27%) index C, and 2 (5%) index D in the original Frey’s group. Four (11%) patients had severity index A, 17 (47%) index B, 15 (42%) index C, and 2 (6%) index D in the modified Frey’s group. There was a significant difference in pain severity index between the two groups. A higher score was found in the original Frey’s group.
There were no differences in the short-term results between the two groups. The mean operating time was 230 min in the original Frey’s group and 258 min in the modified Frey’s group. The mean blood loss was 111 mL in the original Frey’s group and 98 mL in the modified Frey’s group. Only two patients had postoperative pancreatic fistula in the modified Frey’s group. There was one postoperative hemorrhage in each group. There was no significant difference in pulmonary and abdominal infections in the two groups. No mortality happened in either group. The mean length of postoperative hospital stay was 8.3 d in the original Frey’s group and 8.6 d in the modified Frey’s group (Table 2).
| O Frey | M Frey | P value | |
| Operating time (min) | 230 ± 79 | 258 ± 65 | 0.095 |
| Blood loss (mL) | 111 ± 79 | 98 ± 89 | 0.492 |
| Morbidity | |||
| Pancreatic fistula, B and C | 0 | 2 | 0.199 |
| Postoperative hemorrhage | 1 | 1 | 1 |
| Pulmonary infection | 2 | 1 | 1 |
| Abdominal infection | 4 | 4 | 1 |
| Mortality | 0 | 0 | \ |
| Postoperative hospital stay (d) | 8.3 ± 3.1 | 8.6 ± 4.7 | 0.698 |
The mean follow-up was 50.3 in the original Frey’s group and 48.7 mo in the modified Frey’s group. Among all the patients, three consumed alcohol and five were smokers after surgery in the original Frey’s group. In the modified Frey’s group, four patients consumed alcohol and two were smokers after surgery. In the original Frey’s group, eight patients had new-onset exocrine insufficiency and one had worsened exocrine insufficiency. Two patients had new-onset endocrine insufficiency and five had worsening endocrine insufficiency after surgery. In the modified Frey’s group, seven patients had new-onset exocrine insufficiency and one had worsening exocrine insufficiency. Three patients had new-onset endocrine insufficiency and three had worsening endocrine insufficiency (Table 3).
| Postoperative condition | O Frey(n = 44) | M Frey(n = 36) | P value |
| Alcohol abuse | 3 | 4 | 0.387 |
| Nicotine abuse | 5 | 2 | 0.307 |
| New-onset exocrine insufficiency | 8 | 7 | 0.886 |
| Worsen exocrine insufficiency | 1 | 1 | 1.000 |
| New-onset endocrine insufficiency | 2 | 3 | 0.404 |
| Worsen endocrine insufficiency | 5 | 3 | 0.475 |
Among the patients who had a history of surgery that was < 5 years, 33 received the original Frey’s procedure, while 28 had the modified Frey’s procedure. Eleven patients had positive pain symptoms when receiving survey in the original Frey’s group. Seventeen patients had positive pain symptoms when receiving survey in the modified Frey’s group. Among the patients who had a history of surgery < 5 years, there was a significant difference in positive pain symptoms between the two groups. Among the patients who had a history of surgery that was > 5 years, 11 were in the original Frey’s group and eight were in the modified Frey’s group. Six patients had positive pain symptoms when receiving survey in the original Frey’s group. Five patients had positive pain symptoms when receiving survey in the modified Frey’s group. There was no significant difference in positive pain symptoms in these patients (Table 4).
| History of surgery | Pain symptom | O Frey | M Frey | P value |
| < 5 yr | Positive | 11 | 17 | 0.032 |
| Negative | 22 | 11 | ||
| > 5 yr | Positive | 6 | 5 | 0.551 |
| Negative | 5 | 3 |
All patients completed the inquiry about EORTC QLQ-C30 during this study. QoL according to EORTC QLQQ-C30 is summarized in Table 5. A high score in the global health, physical, working ability, emotional, cognitive and social functioning represented a high QoL status. Regarding symptoms and financial impact of the disease, a low scale score indicated no important problems. It showed that patients who had the original Frey’s procedure may achieve better emotional status and fewer fatigue symptoms.
| Follow-up results of QoL assessment | O Frey | M Frey | P value |
| Functional scales | |||
| Physical | 95 | 91 | 0.113 |
| Role | 95 | 93 | 0.322 |
| Cognitive | 87 | 83 | 0.241 |
| Emotional | 69 | 58 | 0.047 |
| Social | 66 | 53 | 0.052 |
| Global QoL | 62 | 53 | 0.115 |
| Symptom scales | |||
| Fatigue | 28 | 39 | 0.028 |
| Nausea and vomiting | 0 | 0 | |
| Pain | 18 | 28 | 0.153 |
| Dyspnea | 0 | 0 | |
| Sleep disturbance | 4 | 1 | 0.294 |
| Appetite loss | 30 | 37 | 0.297 |
| Constipation | 3 | 1 | 0.683 |
| Diarrhea | 21 | 26 | 0.445 |
| Financial impact | 32 | 42 | 0.120 |
When dividing these patients by M-ANNHEIM severity index into two groups, we considered Grades A and B as minor severity and Grades C-E as major severity. There was no significant difference in the positive pain symptoms between the original and modified Frey’s groups (Table 6).
| History of surgery | Surgery | Pain symptom | M-ANNHEIM severity | P value | |
| A, B | C-E | ||||
| < 5 yr | O Frey | Positive | 7 | 4 | 0.794 |
| Negative | 15 | 7 | |||
| M Frey | Positive | 11 | 6 | 0.591 | |
| Negative | 6 | 5 | |||
| > 5 yr | O Frey | Positive | 4 | 2 | 0.576 |
| Negative | 4 | 1 | |||
| M Frey | Positive | 2 | 3 | 0.500 | |
| Negative | 2 | 1 | |||
Operative approaches to the treatment of CP have undergone a dramatic transformation over the past few decades. Two main surgical procedures have been performed in patients with CP: drainage and resection. It is evident that not all patients with CP are suitable for the Partington procedure. It is specifically not used as the procedure of choice for inflammatory disease of the pancreatic head[11]. The principal cause of failure of the Puestow operation is the lack of adequate decompression of the proximal duct of Wirsung, as well as the uncinated and tributary ducts in the head of the pancreas[6]. For these patients, pancreaticoduodenectomy has been performed for > 60 years. It has proven to be an effective means of managing pain and the complications of CP[12]. It is reported that pain relief at 4-6 years after the operation occurs in 71%-89% of patients[12-14]. Subsequently, surgeons have found that total pancreatectomy does not give better pain relief than pancreaticoduodenectomy. Moreover, the metabolic consequences of total pancreatectomy in the absence of islet cell transplantation are profound and life threatening.
In 1987, a new operation for the management of pain and the complications of CP was described by Frey and Smith[5]. This operation involves local resection of the pancreatic head combined with longitudinal pancreaticojejunostomy (LR-LPJ). The ducts of Wirsung and Santorini are excised, and the excavation is created in continuity with the longitudinal dichotomy of the dorsal duct. To reduce the risk of penetrating the posterior capsule of the pancreatic head, Frey and Amikura later recommended that the posterior limit of resection should be the back wall of the opened duct of Wirsung and duct to the uncinate process[6]. Subsequent to Frey’s own modification of the technique, other surgeons have described modifications of the extent or technique of LR-LPJ. Andersen and Topazian advocated performing LR-LPJ as it was originally described, but alternately excising the ducts of Wirsung and uncinate in the pancreatic head[15]. Izbicki et al[16] at the University of Hamburg also recommend a more extensive excavation of the pancreatic head, and use a technique that they refer to as the Hamburg modification of LR-LPJ.
To date, comparisons of pancreaticoduodenectomy and the Frey procedure have shown equivalent pain relief in initial and long-term results but better QoL with the Frey procedure[13,16,17]. For techniques of duodenum-preserving resection of the pancreatic head, one randomized trial comparing Frey and Beger procedures showed similar mortality but lower morbidity with the Frey procedure[17]. In the 8-year follow-up published by Strate et al[18] in 2005, there was no significant difference concerning QoL and pain score. No studies have compared the original and modified Frey’s procedures. Sakata et al[7] advocated a minimum Frey procedure with limited resection of the anterior part of the pancreatic head, with longitudinal pancreaticojejunostomy and found a similar outcome to the modified Frey’s procedure. We were not able to answer the question of how much of the pancreatic head should be resected in Frey’s procedure. In the present study, we compared the original Frey’s procedure with the modified Frey’s procedure using retrospective data in our department. We applied the M-ANNHEIM severity index to grade the disease. We focused on the role of severity of CP and the surgical techniques in the results of the Frey’s procedure.
The original Frey’s procedure is technically more complicated and risky than the modified Frey’s procedure in theory, because more pancreatic parenchyma needs to be resected in the original procedure. However, the difficulties in the original Frey’s procedure create few obstacles for experienced surgeons. There were no differences in operating time, loss of blood, morbidity, mortality and postoperative hospital stay between these two operations in the present study. There was penetration of the posterior capsule of the pancreatic head in the original Frey’s group. The mean operating time was 230 min in the original Frey’s group. The morbidity was 13.6% (6/44) in the original Frey’s group and 19.4% (7/36) in the modified Frey’s group. The results were similar to other reports about Frey’s procedure[6,19-21].
Pain symptoms related to exocrine and complications due to endocrine pancreatic insufficiency are a characteristic feature of CP. Pain is the most serious problem for the patient in terms of missing work, hospitalization, or addiction to analgesics. Alcohol and nicotine are the most important risk factors that affect pain relief after surgery. Although we repeatedly stressed the importance of stopping alcohol consumption and smoking, a few patients persisted. There were no significant differences in alcohol consumption and smoking after surgery between the two groups during follow-up. So, we still included these patients when we compared the long-term results of the two types of surgeries. When comparing pain relief, patients were divided into two subgroups according to whether the follow-up time was > 5 years. We found better pain relief at 5 years after surgery in the original Frey’s group. However, among the patients who had a history of surgery > 5 years, we did not find any difference between the two operations. The latter result could have been affected by the small number of patients. There were only 19 patients with a history of surgery > 5 years. However, 61 patients had a history of surgery < 5 years. So, we consider that a more accurate result may be achieved when more patients had a history of surgery > 5 years.
Success in the Frey’s procedure with complete decompression of the pancreatic ducts depends on maximal excision of the parenchyma in the pancreatic head. This may be the reason why the original Frey’s procedure achieved better pain relief in our study. Preservation of pancreatic function is another important result of Frey’s procedure. We found equal exocrine and endocrine insufficiency between the two Frey’s procedures. Patients with the original Frey’s procedure had better QoL on the emotional scale and fewer fatigue symptoms. We suggest that the better decompression with the original Frey’s procedure relieves pancreatic inflammation. Feeling relaxed would give greater confidence to patients for the original Frey’s procedure.
In current practice, patients with CP are managed by a conservative step-up practice. Surgical intervention is kept as an option of last resort when other treatments have failed and the severity of disease has increased substantially and pain becomes unmanageable[22]. As an alternative to the current conservative step-up practice, there is a new suggestion emerging that surgery early in the clinical course of CP is beneficial in terms of pain control and pancreatic function. This claim is based on some new evidence. In an experimental model of early vs late surgical drainage for CP in piglets, Lamme et al[23] found that early surgery resulted in less histological cell damage and better exocrine pancreatic function. From an observational study of 266 consecutive patients undergoing surgery, Ahmed Ali et al[24] observed that surgery at 3 years after onset of symptoms was independently associated with worsened pain outcome and increased rates of endocrine pancreatic insufficiency. Additionally, preoperative use of opioids was significantly associated with bad outcome of surgery in terms of pain control.
We found the original Frey’s procedure achieved significantly better pain relief at 5 years after surgery. However, the result may be interfered by the severity of CP. It is possible that surgeons had to choose the modified Frey’s procedure instead of the original procedure due to difficulty caused by severity of CP. So, it was necessary to identify the impact of severity of CP on the result of surgery. We applied the M-ANNHEIM severity index of CP to grade the severity of patients. The M-ANNHEIM is a simple, objective and noninvasive classification system of CP, which includes a severity index that refers to the different conditions of pancreatic morphology and pancreatic function, and clinical features of the disease, such as various patterns of pain and the impact of conservative, endoscopic and surgical treatment. It grades the severity of CP into five degrees according to its scoring system that involves reports of pain, pain control, surgical intervention, exocrine insufficiency, endocrine insufficiency, morphological status on imaging, and severe organ complications (Tables 7 and 8). In this study, we classified the severity of CP into two degrees. Grades A and B were classified as minor severity and Grades C-E were classified as major severity. The result was unexpected. The severity of CP had no impact on the pain relief after surgery in either group. This result supports the conservative step-up practice of CP.
| Clinical features | Points | |
| Patient report of pain | ||
| No pain without therapy | (patient reports requiring no pain medication) | 0 |
| Recurrent acute pancreatitis | (patient reports freedom from pain between attacks of acute pancreatitis) | 1 |
| No pain with therapy | (patient reports freedom from pain with pain medication or endoscopic intervention) | 2 |
| Intermittent pain | (patient reports intermittent pain-free episodes, either with or without therapy; possibly additional attacks of acute pancreatitis) | 3 |
| Continuous pain | (patient reports absence of pain-free episodes, either with or without therapy; possibly additional attacks of acute pancreatitis) | 4 |
| Pain control1 | ||
| No medication | 0 | |
| Use of non-opioid drugs or use of mild opioids (WHO step 1 or 2) | 1 | |
| Use of potent opioids (WHO step 3) or endoscopic intervention | 2 | |
| Surgical intervention12 | ||
| Pancreatic surgical intervention for any reason | 4 | |
| Exocrine insufficiency3 | ||
| Absence of exocrine insufficiency | 0 | |
| Presence of mild, moderate, or unproven exocrine insufficiency not requiring enzyme supplementation (including patient reports of intermittent diarrhea) | 1 | |
| Presence of proven exocrine insufficiency (according to exocrine function tests) or presence of marked exocrine insufficiency defined as steatorrhea (> 7 g fac/24 h), normalized or markedly reduced by enzyme supplementation | 2 | |
| Endocrine insufficiency | ||
| Absence of diabetes mellitus | 0 | |
| Presence of diabetes mellitus | 4 | |
| Morphologic status on pancreatic imaging (according to the Cambridge classification) | ||
| Normal | 0 | |
| Equivocal | 1 | |
| Mild | 2 | |
| Moderate | 3 | |
| Marked | 4 | |
| Severe organ complication2 (not included in the Cambridge classification) | ||
| Absence of complications | 0 | |
| Presence of possibly reversible complication4 | 2 | |
| Presence of irreversible complications4 | 4 | |
| Severity index | Severity level | Point range |
| M-ANNHEIM A | Minor | 0-5 |
| M-ANNHEIM B | Increased | 6-10 |
| M-ANNHEIM C | Advanced | 11-15 |
| M-ANNHEIM D | Marked | 16-20 |
| M-ANNHEIM E | Exacerbated | > 20 |
In conclusion, the original Frey’s procedure for CP was as safe as the modified Frey’s procedure. However, the original Frey’s procedure brings better pain relief and equal preservation of function to the modified Frey’s procedure. It may also bring better QoL. However, this should be supported by more evidence. The severity of CP does not affect postoperative pain relief.
In 1987, the original Frey’s procedure for management of pain and complications of chronic pancreatitis (CP) was described by Frey and Smith. To reduce the risk, Frey and Amikura later recommended the modified Frey’s procedure with a posterior limit of resection. The aim of this study was to compare the two Frey’s procedures, and to study the impact of the severity of CP on surgical outcome.
The Frey’s procedure can completely decompress the pancreatic ducts in the pancreatic head because it involves local resection of the pancreatic head. Some studies have suggested that a mean 60%-65% volume of pancreatic head mass resection allows better pain relief. Another study advocated a minimum Frey procedure with limited resection of the anterior part of the pancreatic head.
There is no uniform standard for the amount of cored pancreatic head tissue. This study compared the original and modified Frey’s procedures with different depth of cored tissue in a single department.
This study compared the original and modified Frey’s procedures with different depth of cored tissue in a single department. The results showed an advantage for the original Frey’s procedure in terms of pain relief at a 5-year follow-up.
The original Frey’s procedure involves coring out the anterior and posterior parenchyma of the main pancreatic duct. To reduce the risk of penetrating the posterior capsule of the pancreatic head, the modified Frey’s procedure recommends that the posterior limit of resection should be the back wall of the opened duct of Wirsung and duct to the uncinate process.
This is an interesting paper, regarding an item related to surgery and gastroenterology. The research is well performed, and discussion as well as conclusions adequate.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Manenti A, Sliwinska-Mosson M, Peng SY S- Editor: Qi Y L- Editor: Filipodia E- Editor: Wang CH
| 1. | Schneider A, Löhr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classifications of the disease. J Gastroenterol. 2007;42:101-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 311] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 2. | Strate T, Knoefel WT, Yekebas E, Izbicki JR. Chronic pancreatitis: etiology, pathogenesis, diagnosis, and treatment. Int J Colorectal Dis. 2003;18:97-106. [PubMed] |
| 3. | Axon AT, Classen M, Cotton PB, Cremer M, Freeny PC, Lees WR. Pancreatography in chronic pancreatitis: international definitions. Gut. 1984;25:1107-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 296] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Lankisch PG, Löhr-Happe A, Otto J, Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion. 1993;54:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 248] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2:701-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 267] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Frey CF, Amikura K. Local resection of the head of the pancreas combined with longitudinal pancreaticojejunostomy in the management of patients with chronic pancreatitis. Ann Surg. 1994;220:492-504; discussion 504-507. [PubMed] |
| 7. | Sakata N, Egawa S, Motoi F, Goto M, Matsuno S, Katayose Y, Unno M. How much of the pancreatic head should we resect in Frey’s procedure? Surg Today. 2009;39:120-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1771] [Cited by in RCA: 2320] [Article Influence: 128.9] [Reference Citation Analysis (0)] |
| 9. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3282] [Cited by in RCA: 3512] [Article Influence: 175.6] [Reference Citation Analysis (34)] |
| 10. | Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1411] [Cited by in RCA: 1937] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 11. | Isaji S. Has the Partington procedure for chronic pancreatitis become a thing of the past? A review of the evidence. J Hepatobiliary Pancreat Sci. 2010;17:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Sakorafas GH, Farnell MB, Nagorney DM, Sarr MG, Rowland CM. Pancreatoduodenectomy for chronic pancreatitis: long-term results in 105 patients. Arch Surg. 2000;135:517-23; discussion 523-4. [PubMed] |
| 13. | Bachmann K, Tomkoetter L, Kutup A, Erbes J, Vashist Y, Mann O, Bockhorn M, Izbicki JR. Is the Whipple procedure harmful for long-term outcome in treatment of chronic pancreatitis? 15-years follow-up comparing the outcome after pylorus-preserving pancreatoduodenectomy and Frey procedure in chronic pancreatitis. Ann Surg. 2013;258:815-820; discussion 820-811. |
| 14. | Jimenez RE, Fernandez-Del Castillo C, Rattner DW, Warshaw AL. Pylorus-preserving pancreaticoduodenectomy in the treatment of chronic pancreatitis. World J Surg. 2003;27:1211-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Andersen DK, Topazian MD. Pancreatic head excavation: a variation on the theme of duodenum-preserving pancreatic head resection. Arch Surg. 2004;139:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Izbicki JR, Bloechle C, Broering DC, Knoefel WT, Kuechler T, Broelsch CE. Extended drainage versus resection in surgery for chronic pancreatitis: a prospective randomized trial comparing the longitudinal pancreaticojejunostomy combined with local pancreatic head excision with the pylorus-preserving pancreatoduodenectomy. Ann Surg. 1998;228:771-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 228] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 17. | Izbicki JR, Bloechle C, Knoefel WT, Kuechler T, Binmoeller KF, Broelsch CE. Duodenum-preserving resection of the head of the pancreas in chronic pancreatitis. A prospective, randomized trial. Ann Surg. 1995;221:350-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 189] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Strate T, Taherpour Z, Bloechle C, Mann O, Bruhn JP, Schneider C, Kuechler T, Yekebas E, Izbicki JR. Long-term follow-up of a randomized trial comparing the beger and frey procedures for patients suffering from chronic pancreatitis. Ann Surg. 2005;241:591-598. [RCA] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 133] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 19. | Roch AM, Brachet D, Lermite E, Pessaux P, Arnaud JP. Frey procedure in patients with chronic pancreatitis: short and long-term outcome from a prospective study. J Gastrointest Surg. 2012;16:1362-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Keck T, Wellner UF, Riediger H, Adam U, Sick O, Hopt UT, Makowiec F. Long-term outcome after 92 duodenum-preserving pancreatic head resections for chronic pancreatitis: comparison of Beger and Frey procedures. J Gastrointest Surg. 2010;14:549-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Ueda J, Miyasaka Y, Ohtsuka T, Takahata S, Tanaka M. Short- and long-term results of the Frey procedure for chronic pancreatitis. J Hepatobiliary Pancreat Sci. 2015;22:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Bachmann K, Izbicki JR, Yekebas EF. Chronic pancreatitis: modern surgical management. Langenbecks Arch Surg. 2011;396:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Lamme B, Boermeester MA, Straatsburg IH, van Buijtenen JM, Boerma D, Offerhaus GJ, Gouma DJ, van Gulik TM. Early versus late surgical drainage for obstructive pancreatitis in an experimental model. Br J Surg. 2007;94:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |