Published online Apr 21, 2016. doi: 10.3748/wjg.v22.i15.4066
Peer-review started: December 13, 2015
First decision: December 21, 2015
Revised: December 25, 2015
Accepted: January 9, 2016
Article in press: January 11, 2016
Published online: April 21, 2016
Processing time: 112 Days and 21.1 Hours
Gastric inverted hyperplastic polyp (IHP) is a rare gastric polyp characterized by the downward growth of hyperplastic mucosal components into the submucosal layer. Macroscopically, a gastric IHP resembles a subepithelial tumor (SET); as a result, accurately diagnosing gastric IHP is difficult. This issue has clinical significance because gastric IHP can be misdiagnosed as SET or as malignant neoplasm In addition, adenocarcinoma can accompany benign gastric IHP. Although in most cases, gastric IHPs are asymptomatic and are found incidentally, these polyps may cause anemia secondary to chronic bleeding. Here, we report one case involving gastric IHP accompanied by chronic iron deficiency anemia that was successfully managed using endoscopic submucosal dissection.
Core tip: Gastric inverted hyperplastic polyp (IHP) is a rare gastric polyp characterized by the downward growth of hyperplastic mucosal components into the submucosal layer. It is difficult to diagnose accurately without endoscopic resection and pathological investigation because of its inverted grown into the submucosal layer and the paucity of case reports. In most cases, gastric IHPs are asymptomatic and are found incidentally. Rarely, it may manifest as anemia secondary to chronic bleeding and can be ignored by inexperienced endoscopist. Importantly, it is reported to be related with dysplasia and adenocarcinoma. So, en bloc resection using endoscopic submucosal dissection was recommended for diagnosis and treatment.
- Citation: Yun JT, Lee SW, Kim DP, Choi SH, Kim SH, Park JK, Jang SH, Park YJ, Sung YG, Sul HJ. Gastric inverted hyperplastic polyp: A rare cause of iron deficiency anemia. World J Gastroenterol 2016; 22(15): 4066-4070
- URL: https://www.wjgnet.com/1007-9327/full/v22/i15/4066.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i15.4066
Gastric inverted hyperplastic polyp (IHP) is a rare gastric polyp characterized by the downward growth of hyperplastic mucosal components into the submucosal layer[1]. In 1993, Kamata et al first referred to this type of lesion as an IHP[2]. This polyp has also been called a hamartomatous polyp and a solitary polypoid hamartoma[3]. Macroscopically, a gastric IHP resembles a subepithelial tumor (SET); as a result, accurately diagnosing gastric IHP is difficult. This issue has clinical significance because gastric IHP can be misdiagnosed as SET or as malignant neoplasm. In addition, adenocarcinoma can accompany benign gastric IHP[1]. Although most gastric IHPs are symptomatic and are identified incidentally, we encountered a case of gastric IHP that had the primary manifestation of chronic iron deficiency anemia (IDA) and was successfully managed using endoscopic submucosal dissection (ESD).
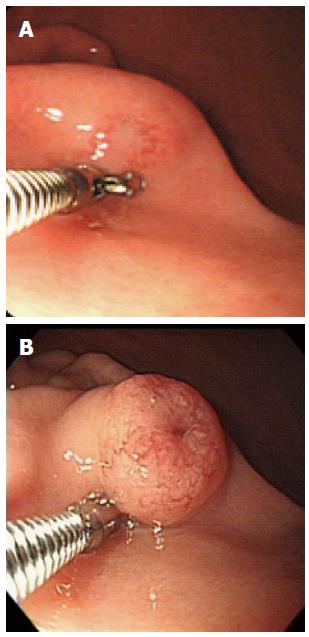
A 64-year-old woman presented with several year history of dizziness and general weakness that had recently become aggravated. Her medical history was otherwise unremarkable. Approximately 7 years prior to the events described here, the patient had been diagnosed with gastric SET (Figure 1A). A biopsy indicated the presence of chronic gastritis. Although the patient had undergone endoscopic examinations nearly every year, no treatment for her gastric SET had been considered.
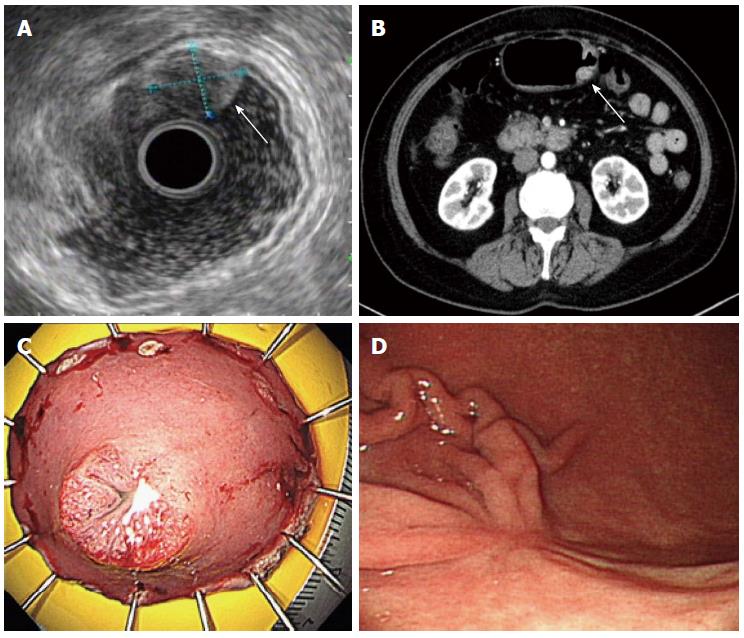
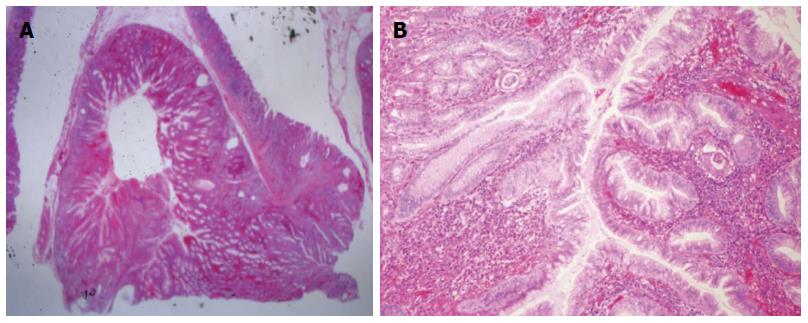
At admission, a physical examination produced unremarkable findings. Complete blood count results indicated a white blood cell count, hemoglobin level, and platelet count of 5900/mm3, 6.5 g/dL, and 497000/mm3, respectively. The patient’s anemia was diagnosed as IDA and her stool was negative for occult blood. Blood chemistry results were unremarkable. An endoscopic examination revealed a 1.5 cm SET on the greater curvature (GC) side of the lower body. This tumor, which had increased in size since the previous examination, was covered with normal mucosa exhibited irregular, hypervascular changes and a central orifice at its surface (Figure 1B). Endoscopic forceps biopsy results indicated chronic gastritis with intestinal metaplasia. A colonoscopic examination produced unremarkable findings. Endoscopic ultrasonography (EUS) revealed a 13.2 mm × 11.2 mm heterogeneous hypoechoic tumor in the submucosal layer of the gastric wall (Figure 2A). Abdominal contrast-enhanced computed tomography (CT) indicated the presence of a 1.5 cm, oval-shaped enhancing mass in the stomach, on the GC side of the lower body (Figure 2B). Because this lesion could have been a cause of the patient’s IDA and because we wished to obtain an appropriate diagnosis, we decided to respect the mass in question using ESD. Grossly, the resected specimen measured 5.0 cm × 3.0 cm and included a well-circumscribed 1.5 cm polypoid lesion (Figure 2C). Histologically, the lesion mainly consisted of inverted proliferating columnar cells and was primarily composed of hyperplastic foveolar-type glands; focal cystic dilatation, inflammatory cells, and smooth muscle bundles in the stroma were observed (Figure 3). The pathologic diagnosis was consistent with gastric IHP. No architectural or cytological atypia were detected.
The patient was discharged following endoscopic treatment of gastric IHP; 5 mo later, the patient’s hemoglobin had normalized to 12.4 g/dL, and anemic symptoms such as general weakness and dizziness had disappeared. A follow-up endoscopic examination revealed a post-ESD scar with a converging fold on the GC side of the lower body (Figure 2D).
Gastric polyps can be classified by morphology as either protruding or inverted. Most gastric polyps are protruding, whereas inverted gastric polyps are rare. Gastric IHP is characterized by the marked endophytic proliferation of foveolar-, pyloric-, or fundic-type glandular epithelium, which leads to a polypoid lesion[4]. Although the pathogenesis of IHP is not well understood, studies have suggested that inflammation and subsequent healing may promote epithelial displacement[4].
The connection between the inflamed overlying mucosa and hyperplastic components in combination with the presence of the slit-shaped cavity in the polyp’s center suggested that repeated mucosal inflammation caused a break in the muscularis mucosae that allowed for the downward herniation and submucosal trapping of mucosal glands[4].
Our literature review discovered 19 reported cases of gastric IHP[1-11]. Most of this gastric IHP were asymptomatic and were found incidentally. Rarely, gastric IHP may manifest as anemia secondary to chronic bleeding. Among the 19 previously reported IHP cases, only 1 case presented with mild anemia. Thus, our IHP case is the first report of symptomatic, severe anemia as a symptom of gastric IHP.
Gastric IHP is difficult to diagnose accurately without endoscopic resection and pathological investigation because of the polyp’s inverted growth into the submucosal layer and the existence of extremely few case reports. Gastric IHP is diagnosed based on the tumor’s pathological characteristics, including fibroblast cells, smooth muscle proliferation, nerve components, vasoformative tissue, glandular hyperplasia, and cystic gland dilatation[1]. The pathological finding of inverted ectopic gastric pseudopyloric glands in the submucosal layer is critical for diagnosing gastric IHP[1].
Gastric IHP is reportedly related to dysplasia and adenocarcinoma[3]. Although gastric IHPs are benign tumors, dysplastic or cancerous areas are found within a large lesion in approximately 20% of gastric IHP cases[5]. Kono et al[6] suggested that p53 dysregulation may play an important role in the malignant transformation of gastric IHPs. In addition, multifocal adenocarcinomas may be present and randomly distributed across the superficial and deep regions of a gastric IHP. Therefore, a negative biopsy cannot reliably exclude the presence of dysplasia or adenocarcinoma. As a result, a patient with gastric IHP should be subjected to complete resection with a negative margin and a thorough histological examination should be performed[4]. Several methods of diagnosing and treating gastric IHP have been used, including conventional polypectomy, endoscopic mucosal resection with piecemeal resection, ESD, and surgical approaches such as laparoscopic wedge resection. Recently, en bloc resection using ESD was recommended for the diagnosis and treatment of gastric IHP.
In conclusion, gastric IHP can cause symptoms such as anemia and can be ignored by an inexperienced endoscopist. Therefore, it is important to recognize the clinical significance of these lesions and consider treatment. We have reported a case of gastric IHP accompanied by chronic IDA that was successfully managed using ESD.
A 64-year-old woman presented with several year history of dizziness and general weakness that had recently become aggravated.
An endoscopic examination revealed a 1.5 cm subepithelial tumor on the greater curvature (GC) side of the lower body.
Carcinoid, Ectopic pancreas, Granular cell tumor, Leiomyoma, Lymphoma.
Hemoglobin level was 6.5 g/dL and all other labs were within normal limits.
Abdominal CT indicated the presence of a 1.5 cm, oval-shaped enhancing mass in the stomach, on the GC side of the lower body and endoscopic ultrasonography revealed a 13.2 mm × 11.2 mm heterogeneous hypoechoic tumor in the submucosal layer of the gastric wall.
Gastric inverted hyperplastic polyp (IHP).
Endoscopic submucosal dissection (ESD).
Gastric IHP is a rare gastric polyp characterized by the downward growth of hyperplastic mucosal components into the submucosal layer. It is difficult to diagnose accurately without endoscopic resection and pathological investigation. Rarely, it may manifest as anemia secondary to chronic bleeding and is related with dysplasia and adenocarcinoma.
ESD is a well-established technique of endoscopic resection that allows for en bloc removal of GI epithelial lesions.
Gastric IHP can cause symptoms such as anemia and can be ignored by an inexperienced endoscopist. Therefore, it is important to recognize the clinical significance of these lesions and consider treatment.
The manuscript is modern, well conceived and well written. The iconography is very comprehensive and discussion is exhaustive.
P- Reviewer: Geraci G, Reinehr R S- Editor: Qi Y L- Editor: A E- Editor: Ma S
| 1. | Mori H, Kobara H, Tsushimi T, Fujihara S, Nishiyama N, Matsunaga T, Ayaki M, Yachida T, Masaki T. Two rare gastric hamartomatous inverted polyp cases suggest the pathogenesis of growth. World J Gastroenterol. 2014;20:5918-5923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Lee SJ, Park JK, Seo HI, Han KH, Kim YD, Jeong WJ, Cheon GJ, Eom DW. A case of gastric inverted hyperplastic polyp found with gastritis cystica profunda and early gastric cancer. Clin Endosc. 2013;46:568-571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (111)] |
| 3. | Jung M, Min KW, Ryu YJ. Gastric inverted hyperplasic polyp composed only of pyloric glands: a rare case report and review of the literature. Int J Surg Pathol. 2015;23:313-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Kim HS, Hwang EJ, Jang JY, Lee J, Kim YW. Multifocal Adenocarcinomas Arising within a Gastric Inverted Hyperplastic Polyp. Korean J Pathol. 2012;46:387-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Odashima M, Otaka M, Nanjo H, Jin M, Horikawa Y, Matsuhashi T, Ohba R, Koizumi S, Kinoshita N, Takahashi T. Hamartomatous inverted polyp successfully treated by endoscopic submucosal dissection. Intern Med. 2008;47:259-262. [PubMed] |
| 6. | Kono T, Imai Y, Ichihara T, Miyagawa K, Kanemitsu K, Ajiki T, Kawasaki K, Kamigaki T, Ikuta H, Ohbayashi C. Adenocarcinoma arising in gastric inverted hyperplastic polyp: a case report and review of the literature. Pathol Res Pract. 2007;203:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Matsuoka J, Itaba S, Makihara Y, Murao H, Umeno N, Minoda Y, Kaku T, Kuniyoshi M, Hamada T, Nakamura K. [Three cases of pedunculated gastric hamartomatous inverted polyps resected endoscopically]. Nihon Shokakibyo Gakkai Zasshi. 2015;112:1030-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Aoki M, Yoshida M, Saikawa Y, Otani Y, Kubota T, Kumai K, Wakabayashi G, Omori T, Mukai M, Kitajima M. Diagnosis and treatment of a gastric hamartomatous inverted polyp: report of a case. Surg Today. 2004;34:532-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Yamashita M, Hirokawa M, Nakasono M, Kiyoku H, Sano N, Fujii M, Koyama T, Yoshida S, Sano T. Gastric inverted hyperplastic polyp. Report of four cases and relation to gastritis cystica profunda. APMIS. 2002;110:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Itoh K, Tsuchigame T, Matsukawa T, Takahashi M, Honma K, Ishimaru Y. Unusual gastric polyp showing submucosal proliferation of glands: case report and literature review. J Gastroenterol. 1998;33:720-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Miyamoto Y, Muguruma N, Okamura S, Okada Y, Kitamura S, Okamoto K, Yoneda A, Kagawa N, Takayama T. A pedunculated submucosal lesion in the stomach with inverted downgrowth. Intern Med. 2014;53:1625-1628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |