Published online Mar 21, 2016. doi: 10.3748/wjg.v22.i11.3285
Peer-review started: August 10, 2015
First decision: September 9, 2015
Revised: September 10, 2015
Accepted: October 23, 2015
Article in press: October 26, 2015
Published online: March 21, 2016
Processing time: 223 Days and 7.7 Hours
Complications of cecal retroflexion performed during colonoscopy have not previously been reported to occur. We report a case of contained colonic perforation secondary to using cecal retroflexion technique to examine the colon, and review available published reports of complications associated with this technique. We conclude that complications may rarely occur with use of cecal retroflexion, and that the clinical benefit of this technique is uncertain.
Core tip: Complications and benefits of cecal retroflexion have undergone limited study. This case report of a contained colonic perforation associated with cecal retroflexion suggests that cecal retroflexion may be associated with rare complications that should be considered in the differential diagnosis of patients exposed to the technique presenting with post-colonoscopy complications.
- Citation: Geng Z, Agrawal D, Singal AG, Kircher S, Gupta S. Contained colonic perforation due to cecal retroflexion. World J Gastroenterol 2016; 22(11): 3285-3288
- URL: https://www.wjgnet.com/1007-9327/full/v22/i11/3285.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i11.3285
Colorectal cancer (CRC) incidence and mortality can be reduced through screening[1-4]. Nonetheless, available evidence suggests risk reduction for CRC mortality is suboptimal, especially in the proximal colon, ranging from 0% to 50%[1-4]. Variable outcomes may be partially due to polyps and CRC that are prevalent but missed at the time of colonoscopic examination using standard examination techniques. Cecal retroflexion may reduce CRC risk by improving polyp and CRC detection in the proximal colon[5]. However, there are few reports on the benefits and potential risks associated with this technique. In this report we present the first case of cecal retroflexion related complication in literature, and review both published and our own experience with cecal retroflexion and associated complications.
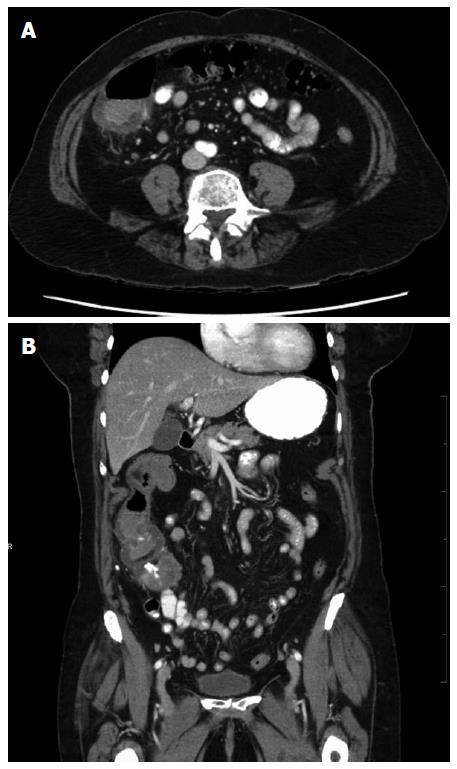
A 76-year-old female underwent colonoscopy for evaluation of painless hematochezia. Four polyps were removed without use of electrocautery (see Table 1), including a 3 mm ascending colonic polyp could only be visualized and removed via cecal retroflexion technique. Four hours post-colonoscopy, the patient presented with acute sharp right lower quadrant abdominal pain, exacerbated by movement, and associated with nausea. She was unable to pass flatus and had not had a bowel movement since the procedure. On exam, she was alert, afebrile, and normotensive. Her abdomen was non-distended, with localized tenderness and guarding in right lower quadrant, but no rebound pain. The white blood cell count was 15.5 × 109/L. Computed tomography abdomen/pelvis with contrast revealed fluid attenuation along the posterior half of the cecum and ascending colon over a 6 cm extent, beginning at the level of the ileocecal valve, but no free air was noted (Figure 1). The patient’s symptoms and imaging findings were felt to be most consistent with contained colonic perforation related to colonoscopy, with use of cecal retroflexion to examine the colon and remove the polyp. She was admitted for observation, kept nothing by mouth, and treated empirically with intravenous fluids and broad-spectrum antibiotics. On hospitalization day 3, she reported significant improvement in her abdominal pain. She was discharged home on a 14-d course of oral ciprofloxacin and metronidazole. She reported feeling well at 1-wk follow-up with resolution of abdominal pain, normal bowel movements, and full recovery of appetite.
| Location | Size (mm) | Removal technique | Pathology |
| Ascending colon | 3 | Cold biopsy forceps | Tubular adenoma1 |
| Transverse colon | 4 | Cold biopsy forceps | Hyperplastic polyp |
| Transverse colon | 5 | Cold snare | Hyperplastic polyp |
| Rectum | 15 | Cold snare | Tubulovillous adenoma with focal high grade dysplasia |
Complications of cecal retroflexion have undergone limited study, with prior work reporting no associated major complications[5-12]. To our knowledge, contained colonic perforation has not been reported as a potential complication of cecal retroflexion. In a review of 1127 colonoscopy reports for individuals who underwent colonoscopy by the senior author (S.G.) over a 6-year period with (n = 607) vs without (n = 520) exposure to cecal retroflexion, we found that that the incidence of major complications was similar (estimated to be 3.3 vs 7.7 complications per 1000 procedures for individuals exposed vs unexposed to cecal retroflexion, P > 0.05). Thus, in our own experience, and in the published literature, complications associated with cecal retroflexion appear to be rare.
We speculate that there are two potential explanations for the observed complication reported in this case. One is that the tip of the colonoscope may have torn the cecum wall when the endoscopist straightened the scope from the hairpin-shaped position. The other explanation is that the bending section of the colonoscope may have been pushed deep into the cecum wall while the endoscopist was trying to remove the adenoma located on the proximal side of the ascending colonic fold. We postulate that increased attention to careful control of the scope tip when straightening the scope after the retroflexion maneuver, and care in avoiding pushing the blunt end of the retroflexed scope into the cecal base might reduce future chances of retroflexion associated complications.
The benefit of cecal retroflexion has also undergone limited study. Two randomized control trails assigned patients underwent forward-view colonoscopy to a second examination of the proximal colon in either forward view or retroflexed view, but neither showed a benefit of cecal retroflexion over second forward-view examination[8,11]. In contrast, prospective cohort studies suggested a significant increase in adenoma detection rate when performing retroflexion in patients underwent initial forward-view examination[5,12].
Overall, we report that use of cecal retroflexion may be associated with rare complications, such as contained colonic perforation. This potential complication should be considered in the differential diagnosis of causes for post-colonoscopy complications among patients exposed to this technique. Given that cecal retroflexion does not appear to have a clear advantage over forward view inspection (especially repeat forward view exam) in detection of adenomas, future studies should focus on other approaches to improve right-sided colonic lesion detection, such as split dose bowel preparation[13,14], training in subtle polyp recognition, and novel endoscope technology.
A 76-year-old female with no significant medical history presented with acute sharp right lower quadrant abdominal pain 4 h post-colonoscopy, with cecal retroflexion performed and 4 colonic polys removed during procedure.
Upon physical examination, abdomen was non-distended, with localized tenderness and guarding in right lower quadrant, but no rebound pain, consistent with post colonoscopy abdominal pain.
Cecal retroflexion-caused perforation/microperforation, postpolypectomy syndrome, or polypectomy-caused perforation/microperforation.
White blood cell count was 15.5 × 109/L.
Computed tomography abdomen/pelvis with contrast revealed fluid attenuation along the posterior half of the cecum and ascending colon over a 6 cm extent, beginning at the level of the ileocecal valve, but no free air was noted.
She was managed with supportive care, kept nothing by mouth, and treated empirically with intravenous fluids and broad-spectrum antibiotics.
There are few reports on the benefits and potential risks associated with cecal retroflexion, and none has reported associated major complications.
Cecal retroflexion is a maneuver during scope withdrawal by making a U-turn with the bending section of the colonoscope in the cecum/proximal colon, so the viewing lens is looking backward and the insertion tube is visible to the endoscopist.
Cecal retroflexion associates with rare complications, and does not add proven benefit in cancer detection
This article could be interesting but they need to add more information about personal history of patient and diagnostic result.
P- Reviewer: Martinez O S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1153] [Article Influence: 96.1] [Reference Citation Analysis (0)] |
| 2. | Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1-8. [PubMed] |
| 3. | Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139:1128-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 373] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 4. | Boland BS, Rivera-Nieves J, Gupta S. Lower endoscopy and prevention of colon cancer. Gastroenterology. 2014;147:245-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011;74:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Rex DK. Accessing proximal aspects of folds and flexures during colonoscopy: impact of a pediatric colonoscope with a short bending section. Am J Gastroenterol. 2003;98:1504-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Rex DK, Khashab M. Colonoscopic polypectomy in retroflexion. Gastrointest Endosc. 2006;63:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Harrison M, Singh N, Rex DK. Impact of proximal colon retroflexion on adenoma miss rates. Am J Gastroenterol. 2004;99:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 116] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Kessler WR, Rex DK. Impact of bending section length on insertion and retroflexion properties of pediatric and adult colonoscopes. Am J Gastroenterol. 2005;100:1290-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Pishvaian AC, Al-Kawas FH. Retroflexion in the colon: a useful and safe technique in the evaluation and resection of sessile polyps during colonoscopy. Am J Gastroenterol. 2006;101:1479-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Kushnir VM, Oh YS, Hollander T, Chen CH, Sayuk GS, Davidson N, Mullady D, Murad FM, Sharabash NM, Ruettgers E. Impact of retroflexion vs. second forward view examination of the right colon on adenoma detection: a comparison study. Am J Gastroenterol. 2015;110:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Chandran S, Parker F, Vaughan R, Mitchell B, Fanning S, Brown G, Yu J, Efthymiou M. Right-sided adenoma detection with retroflexion versus forward-view colonoscopy. Gastrointest Endosc. 2015;81:608-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Kilgore TW, Abdinoor AA, Szary NM, Schowengerdt SW, Yust JB, Choudhary A, Matteson ML, Puli SR, Marshall JB, Bechtold ML. Bowel preparation with split-dose polyethylene glycol before colonoscopy: a meta-analysis of randomized controlled trials. Gastrointest Endosc. 2011;73:1240-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 205] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 14. | Gurudu SR, Ramirez FC, Harrison ME, Leighton JA, Crowell MD. Increased adenoma detection rate with system-wide implementation of a split-dose preparation for colonoscopy. Gastrointest Endosc. 2012;76:603-608.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 102] [Article Influence: 7.8] [Reference Citation Analysis (1)] |